Serum Gamma Glutamyltransferase Is Associated with 25-Hydroxyvitamin D Status in Elderly Patients with Stable Coronary Artery Disease
Abstract
1. Introduction
2. Materials and Methods
3. Statistical Analysis
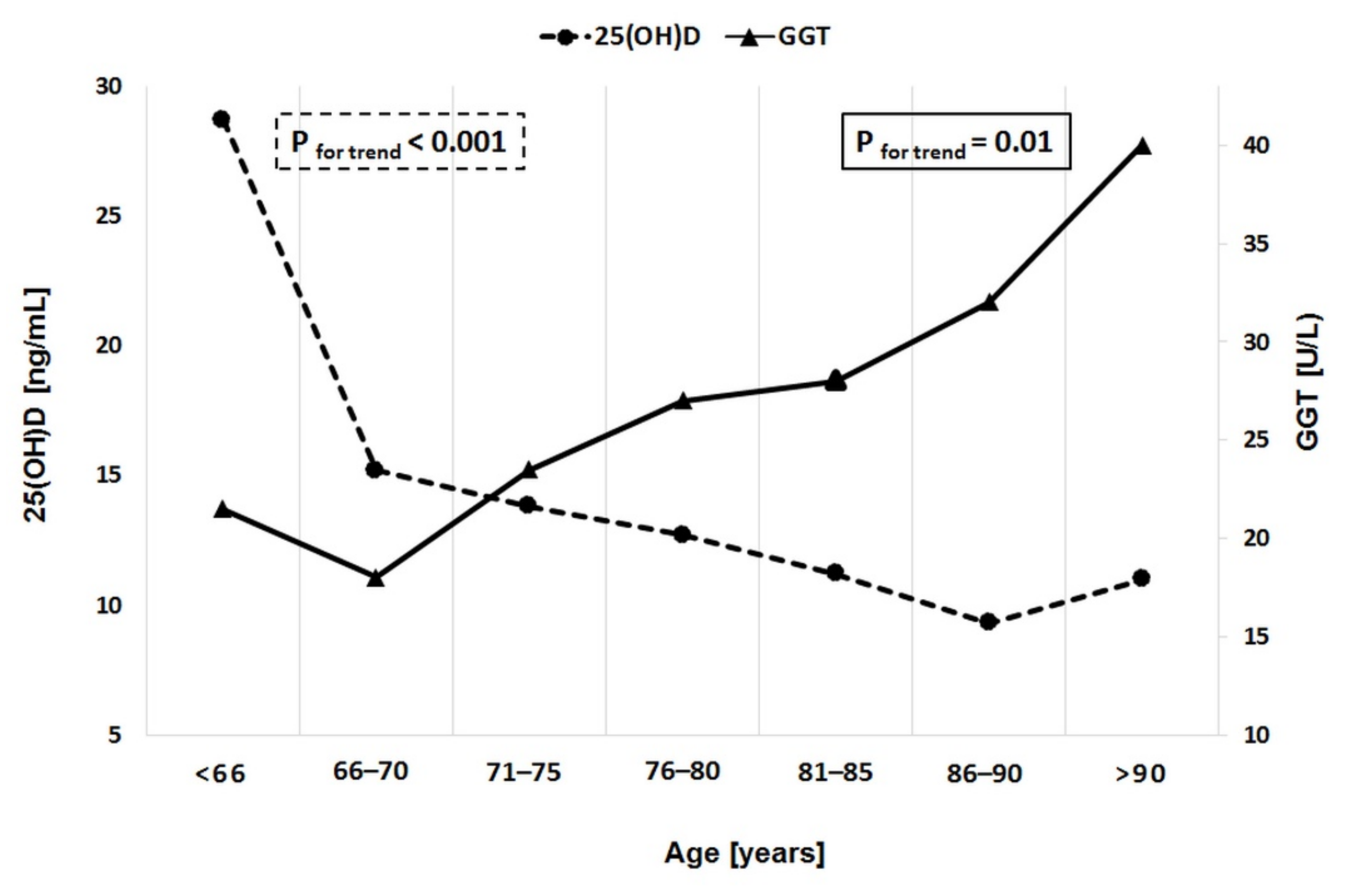
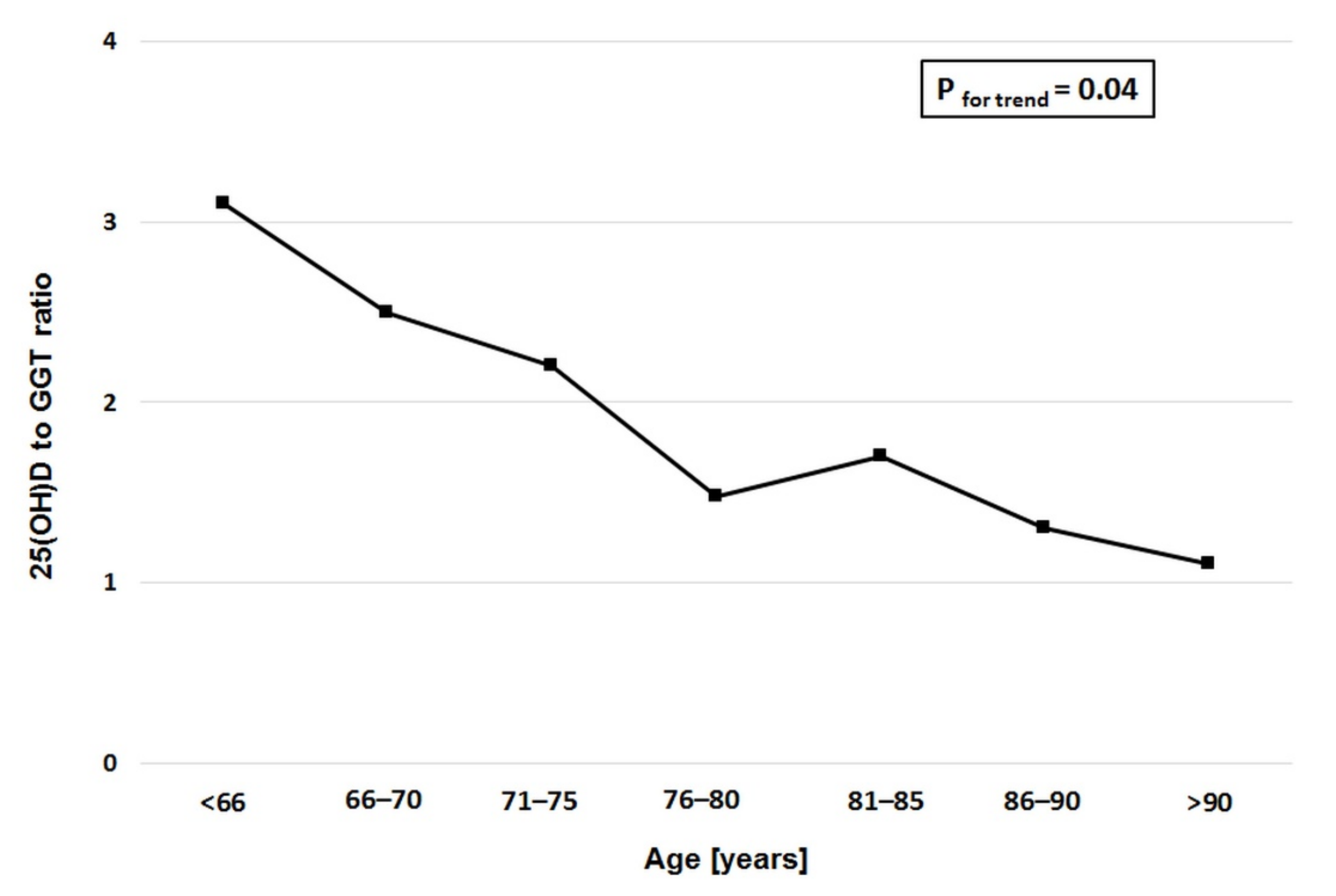
4. Results
5. Discussion
6. Conclusions
Limitations
Author Contributions
Funding
Conflicts of Interest
References
- Libby, P. Inflammation in atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 2045–2051. [Google Scholar] [CrossRef] [PubMed]
- Kattoor, A.J.; Pothineni, N.V.K.; Palagiri, D.; Mehta, J.L. Oxidative Stress in Atherosclerosis. Curr. Atheroscler. Rep. 2017, 19, 42. [Google Scholar] [CrossRef]
- Lonn, M.E.; Dennis, J.M.; Stocker, R. Actions of “antioxidants” in the protection against atherosclerosis. Free Radic. Biol. Med. 2012, 53, 863–884. [Google Scholar] [CrossRef]
- Schutte, R.; Schutte, A.E.; Huisman, H.W.; van Rooyen, J.M.; Malan, N.T.; Péter, S.; Fourie, C.M.T.; van der Westhuizen, F.H.; Louw, R.; Botha, C.A.; et al. Blood glutathione and subclinical atherosclerosis in African men: The SABPA Study. Am. J. Hypertens. 2009, 22, 1154–1159. [Google Scholar] [CrossRef][Green Version]
- Ndrepepa, G.; Colleran, R.; Kastrati, A. Gamma-glutamyl transferase and the risk of atherosclerosis and coronary heart disease. Clin. Chim. Acta 2018, 476, 130–138. [Google Scholar] [CrossRef]
- Mao, Y.; Qi, X.; Xu, W.; Song, H.; Xu, M.; Ma, W.; Zhou, L. Serum gamma-glutamyl transferase: A novel biomarker for coronary artery disease. Med. Sci. Monit. 2014, 20, 706–710. [Google Scholar]
- Sheikh, M.; Tajdini, M.; Shafiee, A.; Anvari, M.S.; Jalali, A.; Poorhosseini, H.; Amirzadegan, A. Association of serum gamma-glutamyltransferase and premature coronary artery disease. Neth. Heart J. 2017, 25, 439–445. [Google Scholar] [CrossRef]
- Celik, O.; Cakmak, H.A.; Satilmis, S.; Gungor, B.; Akin, F.; Ozturk, D.; Yalcin, A.A.; Ayca, B.; Erturk, M.; Atasoy, M.M.; et al. The relationship between gamma-glutamyl transferase levels and coronary plaque burdens and plaque structures in young adults with coronary atherosclerosis. Clin. Cardiol. 2014, 37, 552–557. [Google Scholar]
- Pucci, A.; Franzini, M.; Matteucci, M.; Ceragioli, S.; Marconi, M.; Ferrari, M.; Passino, C.; Basolo, F.; Emdin, M.; Paolicchi, A. b-Gamma-glutamyltransferase activity in human vulnerable carotid plaques. Atherosclerosis 2014, 237, 307–313. [Google Scholar] [CrossRef]
- Holick, M.F. The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev. Endocr. Metab. Disord. 2017, 18, 153–165. [Google Scholar] [CrossRef]
- Pike, J.W.; Christakos, S. Biology and Mechanisms of Action of the Vitamin D Hormone. Endocrinol. Metab. Clin. N. Am. 2017, 46, 815–843. [Google Scholar] [CrossRef] [PubMed]
- Siasos, G.; Tousoulis, D.; Oikonomou, E.; Maniatis, K.; Kioufis, S.; Kokkou, E.; Miliou, A.; Zaromitidou, M.; Kassi, E.; Stefenadis, C. Vitamin D serum levels are associated with cardiovascular outcome in coronary artery disease. Int. J. Cardiol. 2013, 168, 4445–4447. [Google Scholar] [CrossRef] [PubMed]
- Tousoulis, D. Vitamin D deficiency and cardiovascular disease: Fact or fiction? Hell. J. Cardiol. 2018, 59, 69–71. [Google Scholar] [CrossRef]
- Lavie, C.J.; Lee, J.H.; Milani, R.V. Vitamin D and cardiovascular disease will it live up to its hype? J. Am. Coll. Cardiol. 2011, 58, 1547–1556. [Google Scholar] [CrossRef]
- O’Keefe, J.H.; Lavie, C.J.; Holick, M.F. Vitamin D supplementation for cardiovascular disease prevention. JAMA 2011, 306, 1546–1547. [Google Scholar] [CrossRef]
- Elangovan, H.; Chahal, S.; Gunton, J.E. Vitamin D in liver disease: Current evidence and potential directions. Biochim. Biophys. Acta Mol. Basis Dis. 2017, 4, 907–916. [Google Scholar] [CrossRef]
- Korzonek-Szlacheta, I.; Hudzik, B.; Nowak, J.; Szkodziński, J.; Nowak, J.; Gąsior, M.; Zubelewicz-Szkodzińska, B. Mean platelet volume is associated with serum 25-hydroxyvitamin D concentrations in patients with stable coronary artery disease. Heart Vessel. 2018, 33, 1275–1281. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgatdo, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef]
- Boettger, S.F.; Angersbach, B.; Klimek, C.N.; Wanderley, A.L.M.; Shaibekov, A.; Sieske, L.; Wang, B.; Zuchowski, M.; Wirth, R.; Pourhassan, M. Prevalence and predictors of vitamin D-deficiency in frail older hospitalized patients. BMC Geriatr. 2018, 18, 219. [Google Scholar] [CrossRef]
- Spoto, B.; Mattace-Raso, F.; Sijbrands, E.J.; D’Arrigo, G.; Tripepi, G.; Volpato, S.; Bandinelli, S.; Ferrucci, L.; Zoccali, C. Oxidized LDL, Gamma-Glutamyltransferase and Adverse Outcomes in Older Adults. J. Am. Geriatr Soc. 2017, 65, e77–e82. [Google Scholar] [CrossRef]
- Cumhur Cure, M.; Cure, E.; Yuce, S.; Yazici, T.; Karakoyun, I.; Efe, H. Mean platelet volume and vitamin D level. Ann. Lab. Med. 2014, 34, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Paolicchi, A.; Emdin, M.; Ghliozeni, E.; Ciancia, E.; Passino, C.; Popoff, G.; Pompella, A. Images in cardiovascular medicine. Human atherosclerotic plaques contain gamma-glutamyl transpeptidase enzyme activity. Circulation 2004, 109, 1440. [Google Scholar] [CrossRef]
- Whitfield, J.B. Gamma glutamyl transferase. Crit. Rev. Clin. Lab. Sci. 2001, 38, 263–355. [Google Scholar] [CrossRef]
- Bo, S.; Gambino, R.; Durazzo, M.; Guidi, S.; Tiozzo, E.; Ghione, F.; Gentile, L.; Cassader, M.; Pagano, G.F. Associations between gamma-glutamyl transferase, metabolic abnormalities and inflammation in healthy subjects from a population-based cohort: A possible implication for oxidative stress. World J. Gastroenterol. 2005, 11, 7109–7117. [Google Scholar] [CrossRef]
- Emdin, M.; Pompella, A.; Paolicchi, A. Gamma-glutamyltransferase, atherosclerosis, and cardiovascular disease: Triggering oxidative stress within the plaque. Circulation 2005, 112, 2078–2080. [Google Scholar] [CrossRef]
- Wannamethee, G.; Ebrahim, S.; Shaper, A.G. Gamma-glutamyltransferase: Determinants and association with mortality from ischemic heart disease and all causes. Am. J. Epidemiol. 1995, 142, 699–708. [Google Scholar] [CrossRef]
- Karp, D.R.; Shimooku, K.; Lipsky, P.E. Expression of gamma-glutamyl transpeptidase protects ramos B cells from oxidation-induced cell death. J. Biol. Chem. 2001, 276, 3798–3804. [Google Scholar] [CrossRef]
- Demircan, S.; Yazici, M.; Durna, K.; Kilicaslan, F.; Demir, S.; Pinar, M.; Gulel, O. The importance of gamma-glutamyltransferase activity in patients with coronary artery disease. Clin. Cardiol. 2009, 32, 220–225. [Google Scholar] [CrossRef]
- Emdin, M.; Passino, C.; Michelassi, C.; Titta, F.; L’abbate, A.; Donato, L.; Pompella, A.; Paolicchi, A. Prognostic value of serum gamma-glutamyl transferase activity after myocardial infarction. Eur. Heart J. 2001, 22, 1802–1807. [Google Scholar] [CrossRef]
- Akpek, M.; Elcik, D.; Kalay, N.; Yarlioglues, M.; Dogdu, O.; Sahin, O.; Ardic, I.; Oguzhan, A.; Ergin, A.; Kaya, M.K. The prognostic value of serum gamma glutamyl transferase activity on admission in patients with STEMI undergoing primary PCI. Angiology 2012, 63, 579–585. [Google Scholar] [CrossRef]
- Dogan, A.; Icli, A.; Aksoy, F.; Varol, E.; Erdogan, D.; Ozaydin, M.; Kocyigit, S. Gamma-glutamyltransferase in acute coronary syndrome patients without ST elevation and its association with stenotic lesion and cardiac events. Coron. Artery Dis. 2012, 23, 39–44. [Google Scholar] [CrossRef]
- Huang, Y.; Luo, J.; Liu, X.; Wu, Y.; Yang, Y.; Li, W.; Lv, W.; Hu, Y. Gamma-Glutamyltransferase and Risk of Acute Coronary Syndrome in Young Chinese Patients: A Case-Control Study. Dis. Markers 2018, 2018, 2429160. [Google Scholar] [CrossRef]
- Carvalho, L.S.; Sposito, A.C. Vitamin D for the prevention of cardiovascular disease: Are we ready for that? Atherosclerosis 2015, 241, 729–740. [Google Scholar] [CrossRef]
- Pilz, S.; Verheyen, N.; Grubler, M.R.; Tomaschitz, A.; Marz, W. Vitamin D and cardiovascular disease prevention. Nat. Rev. Cardiol. 2016, 13, 404–417. [Google Scholar] [CrossRef]
- Manson, J.E.; Cook, N.R.; Lee, I.M.; Christen, W.; Bassuk, S.S.; Mora, S.; Gibson, H.; Gordon, D.; Copeland, T.; D’Agostino, D.; et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N. Engl. J. Med. 2019, 380, 33–44. [Google Scholar] [CrossRef]
- Scragg, R.; Stewart, A.W.; Waayer, D.; Lawes, C.M.M.; Toop, L.; Sluyter, J.; Murphy, J.; Khaw, K.T.; Camargo, C.A., Jr. Effect of Monthly High-Dose Vitamin D Supplementation on Cardiovascular Disease in the Vitamin D Assessment Study: A Randomized Clinical Trial. JAMA Cardiol. 2017, 2, 608–616. [Google Scholar] [CrossRef]
- Barchetta, I.; Angelico, F.; Del Ben, M.; Baroni, M.G.; Pozzilli, P.; Morini, S.; Cavallo, M.G. Strong association between non alcoholic fatty liver disease (NAFLD) and low 25(OH) vitamin D levels in an adult population with normal serum liver enzymes. BMC Med. 2011, 9, 85. [Google Scholar] [CrossRef]
- He, X.; Xu, C.; Lu, Z.H.; Fang, X.Z.; Tan, J.; Song, Y. Low serum 25-hydroxyvitamin D levels are associated with liver injury markers in the US adult population. Public Health Nutr. 2020, 23, 2915–2922. [Google Scholar] [CrossRef]
- Barchetta, I.; Cimini, F.A.; Cavallo, M.G. Vitamin D Supplementation and Non-Alcoholic Fatty Liver Disease: Present and Future. Nutrients 2017, 9, 1015. [Google Scholar] [CrossRef]
- Barchetta, I.; Del Ben, M.; Angelico, F.; Martino, M.D.; Fraioli, A.; Torre, G.L.; Saulle, R.; Perri, L.; Morini, S.; Tiberti, C.; et al. No effects of oral vitamin D supplementation on non-alcoholic fatty liver disease in patients with type 2 diabetes: A randomized, double-blind, placebo-controlled trial. BMC Med. 2016, 14, 92. [Google Scholar] [CrossRef]
- Naderpoor, N.; Mousa, A.; de Courten, M.; Scradd, R.; de Courten, B. The relationship between 25-hydroxyvitamin D concentration and liver enzymes in overweight or obese adults: Cross-sectional and interventional outcomes. J. Steroid Biochem. Mol. Biol. 2018, 177, 193–199. [Google Scholar] [CrossRef]
- Dabbaghmanesh, M.H.; Danafar, F.; Eshraghian, A.; Omrani, G.R. Vitamin D supplementation for the treatment of non-alcoholic fatty liver disease: A randomized double blind placebo controlled trial. Diabetes Metab. Syndr. 2018, 12, 513–517. [Google Scholar] [CrossRef]
- Barchetta, I.; Cimini, F.A.; Cavallo, M.G. Vitamin D and Metabolic Dysfunction-Associated Fatty Liver Disease (MAFLD): An Update. Nutrients 2020, 12, 3302. [Google Scholar] [CrossRef]
- Asrih, M.; Jornayvaz, F.R. Inflammation as a potential link between nonalcoholic fatty liver disease and insulin resistance. J. Endocrinol. 2013, 218, R25–R36. [Google Scholar] [CrossRef]
- Braunersreuther, V.; Viviani, G.L.; Mach, F.; Montecucco, F. Role of cytokines and chemokines in non-alcoholic fatty liver disease. World J. Gastroenterol. 2012, 18, 727–735. [Google Scholar] [CrossRef]
- Cannell, J.J.; Grant, W.B.; Holick, M.F. Vitamin D and inflammation. Dermatoendocrinology 2014, 6, e983401. [Google Scholar] [CrossRef]
- Mangin, M.; Sinha, R.; Fincher, K. Inflammation and vitamin D: The infection connection. Inflamm. Res. 2014, 63, 803–819. [Google Scholar] [CrossRef]
| Group 1 25(OH)D < 10 ng/mL n = 59 | Group 2 25(OH)D 10–20 ng/mL n = 82 | Group 3 25(OH)D > 20 ng/mL n = 28 | p | |
|---|---|---|---|---|
| Age, years | 77 (68–85) | 76 (67–87) | 75 (70–80) | 0.1 |
| Sex, men n (%) | 13 (22.0) | 35 (42.7) | 10 (35.7) | 0.0001 |
| Arterial hypertension n (%) | 42 (71.2) | 69 (84.1) | 24 (86.0) | 0.6 |
| Hyperlipidemia n (%) | 37 (63.0) | 48 (58.5) | 16 (57.1) | 0.8 |
| Diabetes mellitus n (%) | 16 (27.1) | 23 (28.0) | 11 (63.3) | 0.4 |
| Prior myocardial infarction n (%) | 3 (5.1) | 15 (18.3) | 8 (39.2) | 0.5 |
| BMI | 25 (23–28) | 29 (24–31) | 27 (24–30) | 0.1 |
| Group 1 25(OH)D < 10 ng/mL n = 59 | Group 2 25(OH)D 10–20 ng/mL n = 82 | Group 3 25(OH)D > 20 ng/mL n = 28 | p | |
|---|---|---|---|---|
| Leucocytes (103/mm3) | 6.4 (4.8–8.6) | 6.8 (5.5–8.4) | 6.1 (4.7–6.7) | 0.1 |
| Erythrocytes (106/mm3) | 4.1 (3.8–4.6) | 4.3 (3.9–4.5) | 4.1 (3.9–4.3) | 0.5 |
| Lymphocytes (103/mm3) | 2.0 (1.5–3.0) | 2.3 (2.0–3.1) | 2.0 (1.9–2.4) | 0.7 |
| Neutrophils (103/mm3) | 4.0 (2.6–5.3) | 3.8 (3.0–4.8) | 2.7 (2.2–3.9) | 0.04 |
| Hemoglobin (g/dL) | 12.6 (12.1–13.8) | 12.7 (11.7–13.4) | 12.4 (11.3–13.1) | 0.2 |
| Hematocrit (%) | 38 (36–42) | 39 (36–41) | 38 (37–39) | 0.3 |
| Platelets (103/mm3) | 220 (173–262) | 205 (168–248) | 225 (204–277) | 0.1 |
| Total cholesterol (mmol/L) | 4.3 (3.8–5.5) | 4.4 (3.5–5.3) | 4.3 (3.7–5.1) | 0.7 |
| HDL cholesterol (mmol/L) | 1.5 (1.0–1.9) | 1.5 (1.2–1.7) | 1.2 (1.1–1.3) | 0.1 |
| LDL cholesterol (mmol/L) | 2.3 (1.3–3.6) | 2.6 (1.7–3.3) | 2.5 (1.8–3.2) | 0.8 |
| Triglycerides (mmol/L) | 1.0 (0.9–1.4) | 1.1 (0.9–1.4) | 1.1 (0.9–1.9) | 0.8 |
| Serum creatinine (μmol/L) | 70 (60–90) | 76 (66–100) | 75 (66–88) | 0.1 |
| Aspartate aminotransferase (AST) (U/L) | 18 (15–20) | 18 (16–26) | 16 (14–19) | 0.1 |
| Alanine aminotransferase (ALT) (U/L) | 16 (10–22) | 15 (11–20) | 13 (11–17) | 0.4 |
| Bilirubin (mmol/L) | 12.3 (9.5–18.1) | 9.7 (8.4–12.0) | 10.1 (8.2–13.5) | 0.08 |
| GGT (U/L) | 27 (23–42) | 20 (17–40) | 16 (11–25) | 0.04 |
| Total protein (g/L) | 60.9 (57.2–62.5) | 64.5 (56.0–67.3) | 62.1 (58.0–64.7) | 0.07 |
| Albumin (mg/mL) | 36 (32–38) | 37 (31–39) | 42 (38–46) | 0.04 |
| 25(OH)D (ng/mL) | 8.4 (7.1–9.3) | 13.4 (12.1–15.8) | 23.4 (21.3–25.2) | <0.001 |
| Gamma Glutamyltransferase | ||
|---|---|---|
| Spearman R | p | |
| Weight | 0.20 | 0.008 |
| Waist-to-hip ratio | 0.20 | 0.008 |
| Waist-to-height ratio | 0.15 | 0.04 |
| 25(OH)D | −0.23 | 0.002 |
| HDL cholesterol | −0.24 | 0.002 |
| Alanine aminotransferase (ALT) | 0.26 | 0.0005 |
| Bilirubin | 0.25 | 0.0002 |
| Hemoglobin | 0.20 | 0.01 |
| Leukocytes | 0.23 | 0.003 |
| Neutrophils | 0.22 | 0.004 |
| Lymphocytes | −0.15 | 0.05 |
| Cut-Off | AUC | 95% CI | Sensitivity | Specificity | PPV | NPV | p | |
|---|---|---|---|---|---|---|---|---|
| Vitamin D Deficiency | ||||||||
| GGT | >19 | 0.69 | 0.53–0.77 | 63% | 64% | 88% | 28% | 0.04 |
| Severe Vitamin D Deficiency | ||||||||
| GGT | >21 | 0.63 | 0.51–0.74 | 81% | 56% | 41% | 86% | 0.04 |
| GGT ≤ 19 (n = 66) | GGT > 19 (n = 103) | p | |
|---|---|---|---|
| Age, years | 77 (65–85) | 77 (68–82) | 0.6 |
| Sex, men n (%) | 23 (34.8) | 35 (34.0) | 0.9 |
| Systemic hypertension n (%) | 51 (77.2) | 84 (81.5) | 0.7 |
| Hyperlipidemia n (%) | 40 (60.6) | 61 (59.2) | 0.5 |
| Diabetes mellitus n (%) | 17 (25.7) | 33 (32.0) | 0.2 |
| Prior myocardial infarction n (%) | 10 (15.2) | 16 (15.5) | 0.9 |
| BMI | 26 (23–30) | 27 (24–31) | 0.4 |
| Leucocytes (103/mm3) | 5.7 (5.1–7.0) | 7.0 (5.6–8.9) | 0.01 |
| Erythrocytes (106/mm3) | 4.2 (3.9–4.4) | 4.2 (3.9–4.7) | 0.6 |
| Lymphocytes (103/mm3) | 2.1 (1.9–2.6) | 2.2 (1.8–3.0) | 0.4 |
| Neutrophils (103/mm3) | 3.1 (2.5–4.6) | 4.0 (2.9–5.5) | 0.01 |
| Hemoglobin (g/dL) | 12.4 (11.6–13.1) | 12.7 (12.0–13.8) | 0.2 |
| Hematocrit (%) | 38 (36–40) | 39 (37–42) | 0.2 |
| Platelets (103/mm3) | 216 (190–253) | 209 (160–279) | 0.2 |
| Total cholesterol (mmol/L) | 4.4 (3.5–5.4) | 4.4 (3.7–5.4) | 0.7 |
| HDL cholesterol (mmol/L) | 1.5 (1.2–1.7) | 1.3 (1.0–1.8) | 0.1 |
| LDL cholesterol (mmol/L) | 2.5 (1.7–3.4) | 2.5 (1.6–3.2) | 0.7 |
| Triglycerides (mmol/L) | 1.0 (0.9–1.4) | 1.1 (1.0–1.6) | 0.7 |
| Serum creatinine (μmol/L) | 73 (65–91) | 75 (62–92) | 0.7 |
| Aspartate aminotransferase (AST) (U/L) | 18 (16–20) | 18 (15–23) | 0.8 |
| Alanine aminotransferase (ALT) (U/L) | 14 (11–16) | 17 (11–22) | 0.02 |
| Bilirubin (mmol/L) | 9.9 (8.2–11.1) | 10.90 (8.4–19.2) | 0.02 |
| Total protein (g/L) | 60.5 (57.3–64.0) | 60.9 (58.0–68.4) | 0.7 |
| Albumin (mg/mL) | 34 (33–38) | 34 (31–38) | 0.2 |
| 25(OH)D (ng/mL) | 13.8 (11.0 –21.0) | 10.9 (8.4–15.2) | 0.0001 |
|
• Vitamin D insufficiency (25(OH)D 20–30 ng/mL) n (%) | 10 (15.2) | 18 (17.1) | |
|
• Moderate vitamin D deficiency (25(OH)D 10–20 ng/mL) | 38 (57.7) | 44 (42.7) | 0.0002 |
| • Severe vitamin D deficiency (25(OH)D < 10 ng/mL) n (%) | 18 (27.1) | 41 (39.8) |
| 25[OH]D Serum Level < 30 ng/mL, Odds Ratio (95% Confidence Intervals), p-Value | ||
|---|---|---|
| Unadjusted Model 1 Model 2 | 1.07 (1.02–1.11) 1.06 (1.02–1.12) 1.05 (1.01–1.11) | 0.004 0.01 0.04 |
| Model 1, adjusted for age, sex, weight, waist circumference Model 2 adjusted for age, sex, weight, waist circumference, serum albumin, neutrophil count, ALT, serum bilirubin | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Danikiewicz, A.; Hudzik, B.; Nowak, J.; Kowalska, J.; Zieleń-Zynek, I.; Szkodzinski, J.; Naung Tun, H.; Zubelewicz-Szkodzinska, B. Serum Gamma Glutamyltransferase Is Associated with 25-Hydroxyvitamin D Status in Elderly Patients with Stable Coronary Artery Disease. Int. J. Environ. Res. Public Health 2020, 17, 8980. https://doi.org/10.3390/ijerph17238980
Danikiewicz A, Hudzik B, Nowak J, Kowalska J, Zieleń-Zynek I, Szkodzinski J, Naung Tun H, Zubelewicz-Szkodzinska B. Serum Gamma Glutamyltransferase Is Associated with 25-Hydroxyvitamin D Status in Elderly Patients with Stable Coronary Artery Disease. International Journal of Environmental Research and Public Health. 2020; 17(23):8980. https://doi.org/10.3390/ijerph17238980
Chicago/Turabian StyleDanikiewicz, Aleksander, Bartosz Hudzik, Justyna Nowak, Joanna Kowalska, Iwona Zieleń-Zynek, Janusz Szkodzinski, Han Naung Tun, and Barbara Zubelewicz-Szkodzinska. 2020. "Serum Gamma Glutamyltransferase Is Associated with 25-Hydroxyvitamin D Status in Elderly Patients with Stable Coronary Artery Disease" International Journal of Environmental Research and Public Health 17, no. 23: 8980. https://doi.org/10.3390/ijerph17238980
APA StyleDanikiewicz, A., Hudzik, B., Nowak, J., Kowalska, J., Zieleń-Zynek, I., Szkodzinski, J., Naung Tun, H., & Zubelewicz-Szkodzinska, B. (2020). Serum Gamma Glutamyltransferase Is Associated with 25-Hydroxyvitamin D Status in Elderly Patients with Stable Coronary Artery Disease. International Journal of Environmental Research and Public Health, 17(23), 8980. https://doi.org/10.3390/ijerph17238980





