Subjective Deterioration of Physical and Psychological Health during the COVID-19 Pandemic in Taiwan: Their Association with the Adoption of Protective Behaviors and Mental Health Problems
Abstract
1. Introduction
1.1. The Impact of the Coronavirus Disease 2019 Pandemic
1.2. Physical and Psychological Health during the COVID-19 Pandemic
1.3. Factors Related to Deteriorating Physical and Psychological Health during the COVID-19 Pandemic
1.4. Deterioration of Physical and Psychological Health and the Adoption of Protective Behaviors against COVID-19 and Mental Health Problems
1.5. Aims of the Study
2. Methods
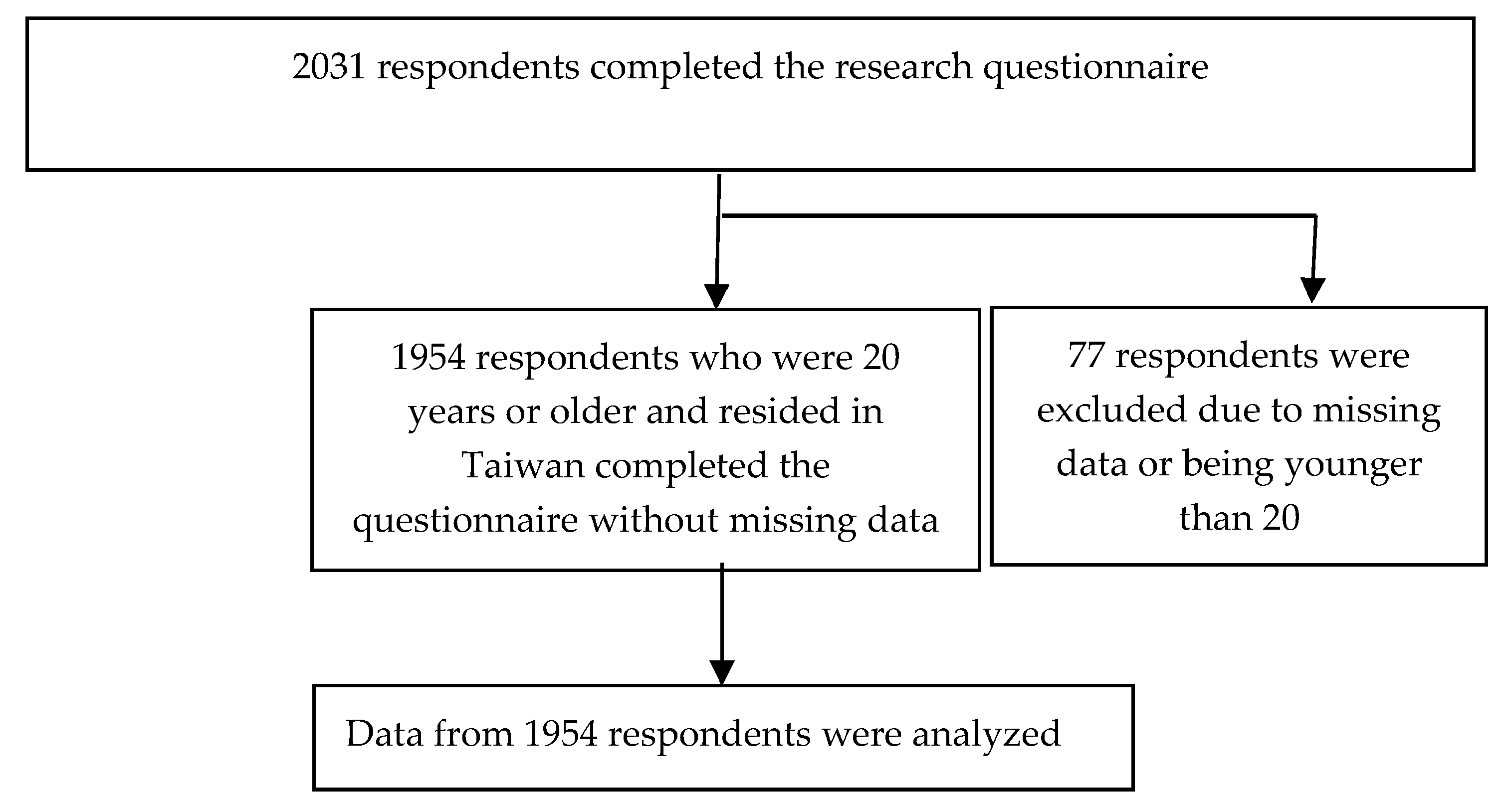
2.1. Participants
2.2. Measures
2.2.1. Subjective Deterioration of Physical and Psychological Health during the COVID-19 Pandemic
2.2.2. Cognitive and Affective Constructs of Health Beliefs Related to COVID-19
2.2.3. Perceived Social Support
2.2.4. Adoption of Protective Behaviors against COVID-19
2.2.5. Mental Health Problems
2.2.6. Demographic Characteristics
2.3. Statistical Analysis
3. Results
3.1. Participant Variables
3.2. Factors Related to the Deterioration of Physical and Psychological Health
3.3. Deterioration of Health and Adoption of Protective Behaviors against COVID-19 and Mental Health Problems
4. Discussion
4.1. Issues of Recruiting Participants from the Facebook Advertisements
4.2. Deterioration of Physical and Psychological Health
4.3. Factors Related to the Deterioration of Physical and Psychological Health
4.4. Deterioration of Health and Adoption of Protective Behaviors against COVID-19 and Mental Health Problems
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Science and Engineering at Johns Hopkins. Modeling 2019-nCoV. Available online: https://systems.jhu.edu/research/public-health/ncov-model/ (accessed on 18 July 2020).
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef]
- McIntyre, R.S.; Lee, Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry 2020, 19, 250–251. [Google Scholar] [CrossRef]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Rundle, A.G.; Park, Y.; Herbstman, J.B.; Kinsey, E.W.; Wang, Y.C. COVID-19–Related School Closings and Risk of Weight Gain Among Children. Obesity 2020, 28, 1008–1009. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ma, Z.F. Impact of the COVID-19 Pandemic on Mental Health and Quality of Life among Local Residents in Liaoning Province, China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 2381. [Google Scholar] [CrossRef] [PubMed]
- Crayne, M.P. The traumatic impact of job loss and job search in the aftermath of COVID-19. Psychol. Trauma: Theory Res. Pr. Policy 2020, 12, S180–S182. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, M.A.; Basch, C.; Oksanen, A.; Kaakinen, M.; Latikka, R.; Savolainen, I.; Savela, N.; Koivula, A. Regulation and Trust: 3-Month Follow-up Study on COVID-19 Mortality in 25 European Countries. JMIR Public Health Surveill. 2020, 6, e19218. [Google Scholar] [CrossRef]
- Huang, A.S.-E.; Shu, P.-Y.; Yang, C.-H. A new reportable disease is born: Taiwan Centers for Disease Control’s response to emerging Zika virus infection. J. Formos. Med. Assoc. 2016, 115, 223–225. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.-Y.; Li, S.-Y.; Yang, C.-H. Initial rapid and proactive response for the COVID-19 outbreak—Taiwan’s experience. J. Formos. Med. Assoc. 2020, 119, 771–773. [Google Scholar] [CrossRef]
- Directorate-General of Budget, Accounting and Statistics, Executive Yuan, Taiwan. Available online: https://www.dgbas.gov.tw/point.asp?index=3 (accessed on 18 July 2020).
- Ramage-Morin, P.L.; Polsky, J.Y. Health-related concerns and precautions during the COVID-19 pandemic: A comparison of Canadians with and without underlying health conditions. Health Rep. 2020, 31, 3–8. [Google Scholar]
- Ping, W.; Zheng, J.; Niu, X.; Guo, C.; Zhang, J.; Yang, H.; Shi, Y. Evaluation of health-related quality of life using EQ-5D in China during the COVID-19 pandemic. PLoS ONE 2020, 15, e0234850. [Google Scholar] [CrossRef] [PubMed]
- Kontoangelos, K.; Economou, M.; Papageorgiou, C. Mental Health Effects of COVID-19 Pandemia: A Review of Clinical and Psychological Traits. Psychiatry Investig. 2020, 17, 491–505. [Google Scholar] [CrossRef] [PubMed]
- Piscitelli, D.; Perin, C.; Tremolizzo, L.; Peroni, F.; Cerri, C.G.; Cornaggia, C.M. Functional movement disorders in a patient with COVID-19. Neurol. Sci. 2020, 41, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Alonzi, S.; La Torre, A.; Silverstein, M.W. The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychol. Trauma: Theory Res. Pr. Policy 2020, 12, S236–S238. [Google Scholar] [CrossRef] [PubMed]
- Findlay, L.C.; Arim, R.; Kohen, D. Understanding the Perceived Mental Health of Canadians During the COVID-19 Pandemic. Health Rep. 2020, 31, 22–27. [Google Scholar]
- Stanton, R.; To, G.Q.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon 2020, 6, 04315. [Google Scholar] [CrossRef]
- Tsamakis, K.; Rizos, E.; Manolis, A.J.; Chaidou, S.; Kympouropoulos, S.; Spartalis, E.; Spandidos, D.A.; Tsiptsios, D.; Triantafyllis, A.S. COVID-19 pandemic and its impact on mental health of healthcare professionals. Exp. Ther. Med. 2020, 19, 3451–3453. [Google Scholar] [CrossRef]
- Glanz, K.; Rimer, B.K.; Viswanath, K.V. Health Behavior: Theory, Research, and Practice; Jossey-Bass: San Francisco, CA, USA, 2015. [Google Scholar]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social Learning Theory and the Health Belief Model. Health Educ. Q. 1988, 15, 175–183. [Google Scholar] [CrossRef]
- Asmundson, G.J.G.; Taylor, S. Coronaphobia: Fear and the 2019-nCoV outbreak. J. Anxiety Disord. 2020, 70, 102196. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.H.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Liao, Q.; Cowling, B.J.; Lam, W.W.T.; Ng, D.M.; Fielding, R. Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: Ten cross-sectional surveys. BMC Infect. Dis. 2014, 14, 169. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020, 26, e923549-1. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. Neuroimaging 2020, 288, 112954. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.C.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Leung, G.M.; Lam, T.H.; Ho, L.-M.; Ho, S.-Y.; Chan, B.H.Y.; Wong, I.O.L.; Hedley, A.J. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J. Epidemiol. Community Health 2003, 57, 857–863. [Google Scholar] [CrossRef]
- Lin, I.-C.; Uddin, B.; Parush, A.; Wacht, O.; Gomes, R.; Frenkel, A. Human Factors Considerations in Using Personal Protective Equipment in the COVID-19 Pandemic Context: A Bi-national Survey Study (Preprint). J. Med. Internet Res. 2020, 22, 19947. [Google Scholar] [CrossRef]
- Dsouza, D.D.; Quadros, S.; Hyderabadwala, Z.J.; Mamun, M.A. Aggregated COVID-19 suicide incidences in India: Fear of COVID-19 infection is the prominent causative factor. Psychiatry Res. Neuroimaging 2020, 290, 113145. [Google Scholar] [CrossRef]
- Wang, P.-W.; Lu, W.-H.; Ko, N.-Y.; Chen, Y.-L.; Li, D.-J.; Chang, Y.-P.; Yen, C.-F. COVID-19-Related Information Sources and Their Relationships with Confidence of People in Coping with COVID-19: A Facebook Survey Study in Taiwan (Preprint). J. Med. Internet Res. 2020, 22, 20021. [Google Scholar] [CrossRef] [PubMed]
- Ko, N.-Y.; Lu, W.-H.; Chen, Y.-L.; Li, D.-J.; Chang, Y.-P.; Wu, C.-F.; Wang, P.-W.; Yen, C.-F. Changes in Sex Life among People in Taiwan during the COVID-19 Pandemic: The Roles of Risk Perception, General Anxiety, and Demographic Characteristics. Int. J. Environ. Res. Public Health 2020, 17, 5822. [Google Scholar] [CrossRef] [PubMed]
- Li, D.-J.; Ko, N.-Y.; Chen, Y.-L.; Wang, P.-W.; Chang, Y.-P.; Yen, C.-F.; Lu, W.-H. COVID-19-Related Factors Associated with Sleep Disturbance and Suicidal Thoughts among the Taiwanese Public: A Facebook Survey. Int. J. Environ. Res. Public Health 2020, 17, 4479. [Google Scholar] [CrossRef] [PubMed]
- Ko, C.-H.; Yen, C.-F.; Yen, J.-Y.; Yang, M.-J. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin. Neurosci. 2006, 60, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Tardy, C.H. Social support measurement. Am. J. Community Psychol. 1985, 13, 187–202. [Google Scholar] [CrossRef]
- Shek, D.T.L. Reliability and factorial structure of the Chinese version of the State-Trait Anxiety Inventory. J. Psychopathol. Behav. Assess. 1988, 10, 303–317. [Google Scholar] [CrossRef]
- Spielberger, C.; Gorusch, R.; Luschene, R. State Trait Anxiety Inventory: A Test Manual/Test Form; Consulting Psychologists Press: Palo Alto, CA, USA, 1970. [Google Scholar]
- Wu, C.-Y.; Lee, J.-I.; Lee, M.-B.; Liao, S.-C.; Chang, C.-M.; Chen3, H.-C.; Lung, F.-W. Predictive validity of a five-item symptom checklist to screen psychiatric morbidity and suicide ideation in general population and psychiatric settings. J. Formos. Med. Assoc. 2016, 115, 395–403. [Google Scholar] [CrossRef]
- Lee, M.-B.; Liao, S.-C.; Lee, Y.-J.; Wu, C.-H.; Tseng, M.-C.; Gau, S.-F.; Rau, C.-L. Development and verification of validity and reliability of a short screening instrument to identify psychiatric morbidity. J. Formos. Med. Assoc. 2003, 102, 687–694. [Google Scholar]
- Baron, R.M.; Kenny, D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Bobkowski, P.; Smith, J. Social media divide: Characteristics of emerging adults who do not use social network websites. Media Cult. Soc. 2013, 35, 771–781. [Google Scholar] [CrossRef]
- Whitaker, C.; Stevelink, S.A.M.; Fear, N.; Arcia, A.; Ashford, M. The Use of Facebook in Recruiting Participants for Health Research Purposes: A Systematic Review. J. Med. Internet Res. 2017, 19, e290. [Google Scholar] [CrossRef]
- National Health Insurance Administration, Ministry of Health and Welfare, Taiwan. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=9F2C9241555E0B42&topn=23C660CAACAA159D (accessed on 18 July 2020).
- Peçanha, T.; Goessler, K.F.; Roschel, H.; Gualano, B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am. J. Physiol. Circ. Physiol. 2020, 318, H1441–H1446. [Google Scholar] [CrossRef]
- Zamberg, I.; Iakovou, I.; Timmers, T.; Janssen, L.; Stohr, J.; Murk, J.; Berrevoets, M. Using eHealth to Support COVID-19 Education, Self-Assessment, and Symptom Monitoring in the Netherlands: Observational Study. JMIR mHealth uHealth 2020, 8, e19822. [Google Scholar] [CrossRef]
- Tsamakis, K.; Triantafyllis, A.S.; Tsiptsios, D.; Spartalis, E.; Mueller, C.; Tsamakis, C.; Chaidou, S.; Spandidos, D.A.; Fotis, L.; Economou, M.; et al. COVID-19 related stress exacerbates common physical and mental pathologies and affects treatment (Review). Exp. Ther. Med. 2020, 20, 159–162. [Google Scholar] [CrossRef] [PubMed]
- Hua, J.; Shaw, R. Corona Virus (COVID-19) “Infodemic” and Emerging Issues through a Data Lens: The Case of China. Int. J. Environ. Res. Public Health 2020, 17, 2309. [Google Scholar] [CrossRef] [PubMed]
- Kwasnicka, D.; Dombrowski, S.U.; White, M.; Sniehotta, F.F. Theoretical explanations for maintenance of behaviour change: A systematic review of behaviour theories. Health Psychol. Rev. 2016, 10, 277–296. [Google Scholar] [CrossRef]
- Codina, N.; Pestana, J.V. Estudio de la relación del entorno psicosocial en la práctica deportiva de la mujer. Rev. Psicol. Deporte 2012, 21, 243–251. [Google Scholar]
- Solomou, I.; Constantinidou, F. Prevalence and Predictors of Anxiety and Depression Symptoms during the COVID-19 Pandemic and Compliance with Precautionary Measures: Age and Sex Matter. Int. J. Environ. Res. Public Health 2020, 17, 4924. [Google Scholar] [CrossRef]
- Huang, J.; Liu, F.; Teng, Z.; Chen, J.; Zhao, J.; Wang, X.; Wu, Y.; Xiao, J.; Wang, Y.; Wu, R.-R. Public behavior change, perceptions, depression, and anxiety in relation to the COVID-19 outbreak. Open Forum Infect. Dis. 2020, 7, 273. [Google Scholar] [CrossRef]
- Khalsa, S.S.; Adolphs, R.; Cameron, O.G.; Critchley, H.; Davenport, P.W.; Feinstein, J.S.; Feusner, J.D.; Garfinkel, S.; Lane, R.D.; Mehling, W.E.; et al. Interoception and Mental Health: A Roadmap. Boil. Psychiatry: Cogn. Neurosci. Neuroimaging 2018, 3, 501–513. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
| Physical Health | Psychological Health | |||
|---|---|---|---|---|
| before the Pandemic | during the Pandemic | before the Pandemic | during the Pandemic | |
| n (%) | n (%) | n (%) | n (%) | |
| Much worse (Score 0) | 52 (2.7) | 36 (1.8) | 62 (3.2) | 73 (3.7) |
| Mildly worse (Score 1) | 462 (23.6) | 344 (17.6) | 231 (11.8) | 241 (12.3) |
| Same (Score 2) | 901 (46.1) | 1083 (55.4) | 842 (43.1) | 942 (48.2) |
| Mildly better (Score 3) | 404 (20.7) | 376 (19.2) | 572 (29.3) | 512 (26.2) |
| Much better (Score 4) | 135 (6.9) | 115 (5.9) | 247 (12.6) | 186 (9.5) |
| Changes from before to during the pandemic | ||||
| Deteriorated | ||||
| Severely (change for 3 scores) | 8 (0.4) | 8 (0.4) | ||
| Moderately (change for 2 scores) | 38 (1.9) | 72 (3.7) | ||
| Mildly (change for 1 score) | 211 (10.8) | 297 (15.2) | ||
| No change | 1353 (69.2) | 1363 (69.8) | ||
| Improved | ||||
| Mildly (change for 1 score) | 300 (15.4) | 180 (9.2) | ||
| Moderately (change for 2 scores) | 40 (2.0) | 32 (1.6) | ||
| Severely (change for 3 scores) | 3 (0.2) | 1 (0.1) | ||
| Profoundly (change for 4 scores) | 1 (0.1) | 1 (0.1) | ||
| Deterioration of health | 257 (13.2) | 377 (19.3) | ||
| No change or improvement of health | 1697 (86.8) | 1577 (80.7) | ||
| Deterioration of Physical Health | Deterioration of Psychological Health | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | B | cOR | 95% CI | p | No | Yes | B | cOR | 95% CI | p | |
| Gender, n (%) | ||||||||||||
| Female (n = 1305) | 1137 (87.1) | 168 (12.9) | 0.073 | 1.076 | 0.816–1.418 | 0.605 | 1035 (79.3) | 270 (20.7) | −0.279 | 0.757 | 0.591–0.969 | 0.027 |
| Male (n = 649) | 560 (86.3) | 89 (13.7) | 542 (83.5) | 107 (16.5) | ||||||||
| Age, n (%) | ||||||||||||
| Younger (n = 925) | 787 (85.1) | 138 (14.9) | −0.293 | 0.746 | 0.573–0.970 | 0.029 | 718 (77.6) | 207 (22.4) | −0.376 | 0.686 | 0.548–0.860 | 0.001 |
| Older (n = 1029) | 910 (88.4) | 119 (11.6) | 859 (83.5) | 170 (16.5) | ||||||||
| Education level, n (%) | ||||||||||||
| University or above (n = 1736) | 1505 (86.7) | 231 (13.3) | −0.125 | 0.882 | 0.573–1.359 | 0.570 | 1391 (80.1) | 345 (19.9) | −0.366 | 0.694 | 0.468–1.028 | 0.068 |
| High school or below (n = 218) | 192 (88.1) | 26 (11.9) | 186 (85.3) | 32 (14.7) | ||||||||
| Perceived susceptibility to COVID-19, n (%) | ||||||||||||
| Low (n = 1608) | 1405 (87.4) | 203 (12.6) | 0.247 | 1.280 | 0.924–1.772 | 0.137 | 1308 (81.3) | 300 (18.7) | 0.222 | 1.248 | 0.941–1.656 | 0.124 |
| High (n = 346) | 292 (84.4) | 54 (15.6) | 269 (77.7) | 77 (22.3) | ||||||||
| Perceived harm of COVID-19 relative to SARS, n (%) | ||||||||||||
| No (n = 575) | 520 (90.4) | 55 (9.6) | 0.484 | 1.623 | 1.184–2.224 | 0.003 | 489 (85.0) | 86 (15.0) | 0.419 | 1.521 | 1.169–1.979 | 0.002 |
| Yes (n = 1379) | 1177 (85.4) | 202 (14.6) | 1088 (78.9) | 291 (21.1) | ||||||||
| Sufficient knowledge and information about COVID-19, n (%) | ||||||||||||
| No (n = 191) | 175 (91.6) | 16 (8.4) | 0.549 | 1.732 | 1.020–2.941 | 0.042 | 159 (83.2) | 32 (16.8) | 0.190 | 1.209 | 0.812–1.799 | 0.350 |
| Yes (n = 1763) | 1522 (86.3) | 241 (13.7) | 1418 (80.4) | 345 (19.6) | ||||||||
| Confidence in coping with COVID-19, n (%) | ||||||||||||
| Low (n = 268) | 213 (79.5) | 55 (20.5) | -0.640 | 0.527 | 0.379–0.734 | <0.001 | 207 (77.2) | 61 (22.8) | −0.245 | 0.783 | 0.574–1.068 | 0.122 |
| High (n = 1686) | 1484 (88.0) | 202 (12.0) | 1370 (81.3) | 316 (18.7) | ||||||||
| Worry about COVID-19, n (%) | ||||||||||||
| Low (n = 726) | 648 (89.3) | 78 (10.7) | 0.349 | 1.418 | 1.068–1.882 | 0.016 | 627 (86.4) | 99 (13.6) | 0.617 | 1.853 | 1.443–2.381 | <0.001 |
| High (n = 1228) | 1049 (85.4) | 179 (14.6) | 950 (77.4) | 278 (22.6) | ||||||||
| Perceived social support, n (%) | ||||||||||||
| Low (n = 765) | 645 (84.3) | 120 (15.7) | −0.357 | 0.700 | 0.538–0.911 | 0.008 | 581 (75.9) | 184 (24.1) | −0.491 | 0.612 | 0.488–0.767 | <0.001 |
| High (n = 1189) | 1052 (88.5) | 137 (11.5) | 996 (83.8) | 193 (16.2) | ||||||||
| Deterioration of Physical Health | Deterioration of Psychological Health | |||||||
|---|---|---|---|---|---|---|---|---|
| B | aOR | 95% CI | p | B | aOR | 95% CI | p | |
| Male a | −0.172 | 0.842 | 0.654–1.083 | 0.180 | ||||
| Older age b | −0.270 | 0.763 | 0.584–0.997 | 0.048 | −0.303 | 0.738 | 0.587–0.929 | 0.010 |
| Perceived harm of COVID-19 more than SARS c | 0.421 | 1.524 | 1.107–2.099 | 0.010 | 0.339 | 1.403 | 1.073–1.835 | 0.013 |
| Sufficient knowledge and information about COVID-19 d | 0.763 | 2.146 | 1.247–3.692 | 0.006 | ||||
| High confidence in coping with COVID-19 e | −0.608 | 0.545 | 0.385–0.771 | 0.001 | ||||
| High worry about COVID-19 f | 0.183 | 1.201 | 0.896–1.611 | 0.220 | 0.503 | 1.653 | 1.280–2.136 | <0.001 |
| High social support g | −0.305 | 0.737 | 0.562–0.966 | 0.027 | −0.433 | 0.649 | 0.516–0.816 | <0.001 |
| Avoiding Crowded Places | Washing Hands | Wearing a Mask | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | aOR | 95% CI | p | B | aOR | 95% CI | p | B | aOR | 95% CI | p | |
| Deterioration of physical health | 0.259 | 1.296 | 0.890–1.886 | 0.177 | 0.260 | 1.297 | 0.918–1.832 | 0.140 | 0.328 | 1.388 | 0.971–1.986 | 0.072 |
| Deterioration of psychological health | 0.411 | 1.508 | 1.088–2.092 | 0.014 | 0.293 | 1.340 | 0.998–1.799 | 0.052 | 0.525 | 1.690 | 1.238–2.308 | 0.001 |
| Male a | −0.265 | 0.768 | 0.605–0.974 | 0.030 | −0.166 | 0.847 | 0.677–1.060 | 0.147 | −0.042 | 0.959 | 0.765–1.202 | 0.717 |
| Older age b | 0.450 | 1.568 | 1.241–1.983 | <0.001 | 0.390 | 1.477 | 1.188–1.837 | <0.001 | −0.022 | 0.979 | 0.787–1.216 | 0.846 |
| Low educational level c | −0.459 | 0.632 | 0.448–0.891 | 0.009 | −0.442 | 0.643 | 0.465–0.888 | 0.007 | −0.294 | 0.745 | 0.540–1.030 | 0.075 |
| General Anxiety | Sleep Problem | Suicidal Idea | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | aOR | 95% CI | p | B | aOR | 95% CI | p | B | aOR | 95% CI | p | |
| Deterioration of physical health | 0.687 | 1.989 | 1.499–2.639 | <0.001 | 0.259 | 1.295 | 0.980–1.712 | 0.069 | 0.285 | 1.330 | 0.878–2.015 | 0.179 |
| Deterioration of psychological health | 0.497 | 1.643 | 1.295–2.084 | <0.001 | 0.271 | 1.312 | 1.033–1.665 | 0.026 | −0.195 | 0.823 | 0.558–1.214 | 0.325 |
| Male a | −0.299 | 0.741 | 0.611–0.899 | 0.002 | −0.087 | 0.917 | 0.758–1.110 | 0.374 | −0.002 | 0.998 | 0.728–1.369 | 0.990 |
| Older age b | −0.127 | 0.881 | 0.733–1.059 | 0.176 | −0.279 | 0.756 | 0.630–0.908 | 0.003 | −1.341 | 0.262 | 0.187–0.365 | <0.001 |
| Low educational level c | 0.257 | 1.293 | 0.968–1.727 | 0.082 | 0.009 | 1.009 | 0.757–1.346 | 0.951 | 0.366 | 1.442 | 0.893–2.327 | 0.134 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, P.-W.; Ko, N.-Y.; Chang, Y.-P.; Wu, C.-F.; Lu, W.-H.; Yen, C.-F. Subjective Deterioration of Physical and Psychological Health during the COVID-19 Pandemic in Taiwan: Their Association with the Adoption of Protective Behaviors and Mental Health Problems. Int. J. Environ. Res. Public Health 2020, 17, 6827. https://doi.org/10.3390/ijerph17186827
Wang P-W, Ko N-Y, Chang Y-P, Wu C-F, Lu W-H, Yen C-F. Subjective Deterioration of Physical and Psychological Health during the COVID-19 Pandemic in Taiwan: Their Association with the Adoption of Protective Behaviors and Mental Health Problems. International Journal of Environmental Research and Public Health. 2020; 17(18):6827. https://doi.org/10.3390/ijerph17186827
Chicago/Turabian StyleWang, Peng-Wei, Nai-Ying Ko, Yu-Ping Chang, Chia-Fen Wu, Wei-Hsin Lu, and Cheng-Fang Yen. 2020. "Subjective Deterioration of Physical and Psychological Health during the COVID-19 Pandemic in Taiwan: Their Association with the Adoption of Protective Behaviors and Mental Health Problems" International Journal of Environmental Research and Public Health 17, no. 18: 6827. https://doi.org/10.3390/ijerph17186827
APA StyleWang, P.-W., Ko, N.-Y., Chang, Y.-P., Wu, C.-F., Lu, W.-H., & Yen, C.-F. (2020). Subjective Deterioration of Physical and Psychological Health during the COVID-19 Pandemic in Taiwan: Their Association with the Adoption of Protective Behaviors and Mental Health Problems. International Journal of Environmental Research and Public Health, 17(18), 6827. https://doi.org/10.3390/ijerph17186827






