Breastfeeding at 1, 3 and 6 Months after Birth according to the Mode of Birth: A Correlation Study
Abstract
1. Introduction
2. Methods
2.1. Design
2.2. Ethical Considerations
2.3. Participants
2.4. Study Measures
2.4.1. Sociodemographic Variables
2.4.2. Independent Variables
2.4.3. Dependent Variables
2.5. Data Collection Procedure
2.6. Data Analysis
3. Results
3.1. Description of Sample and Study Variables
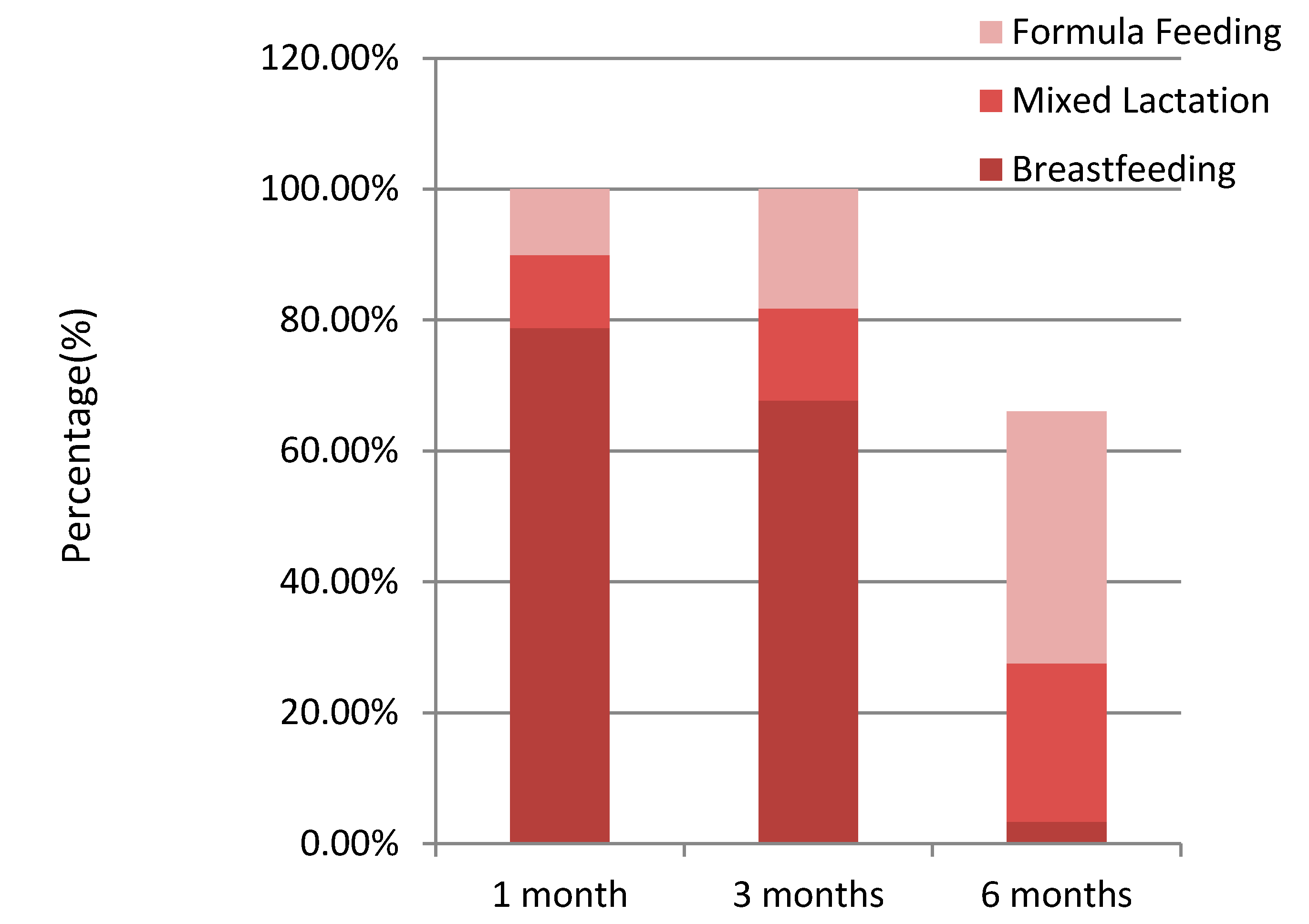
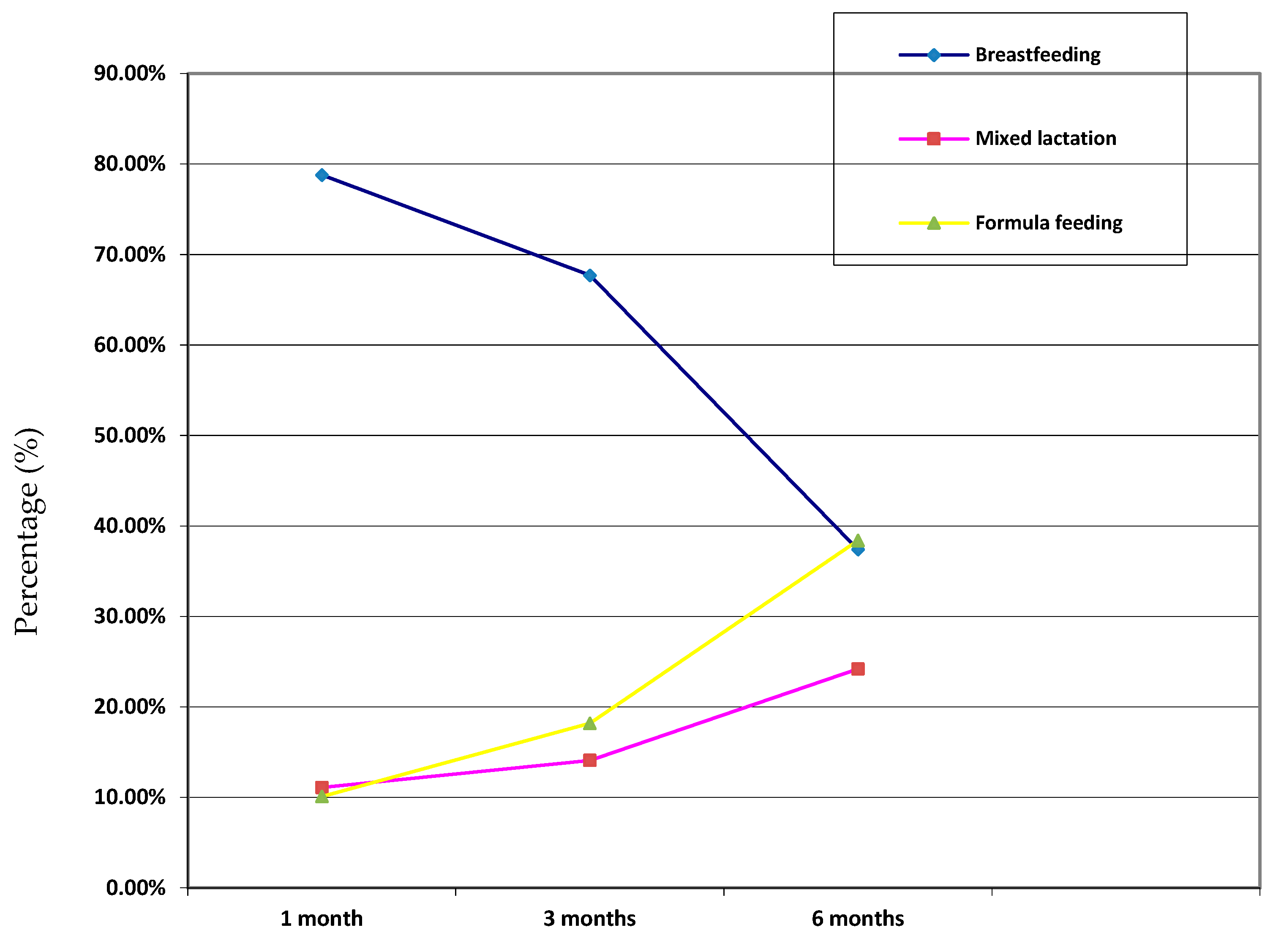
3.2. Evolution of the Type of Lactation in the First Six Months after Birth
3.3. Correlation between the Study Variables
3.3.1. Type of Lactation at One Month after Birth
3.3.2. Type of Lactation at 3 Months after Birth
3.3.3. Type of Lactation at Six Months after Birth
3.3.4. Duration of Breastfeeding
4. Discussion
Limitations
5. Conclusions
- The type of lactation during the first six months after birth is associated with birth variables such as epidural analgesia, episiotomy, perineal tears and parity.
- The duration of breastfeeding increases in women with episiotomy and the absence of perineal tear.
- Breastfeeding duration is shorter in women who received epidural analgesia and women with great parity.
- The mode of birth (vaginal birth, obstetric birth or caesarean birth) is related neither to the type of lactation during the first six months after birth nor to the total duration of breastfeeding.
- In Spain, there is no official breastfeeding temporal monitoring system that follows the international guidelines to unify the indicators and methodology recommended to obtain comparable results, thus, further research on this topic is needed.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- European Network for Public Health Nutrition. Infant and Young Child Feeding: Standard Recommendations for the European Union. Available online: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/publications/external-publications/infant-and-young-child-nutrition (accessed on 17 November 2016).
- Ministry of Health of Spain. Clinical Practice Guide on Breastfeeding. Available online: https://redets.mscbs.gob.es/documentos/GPCLactancia_Osteba.pdf (accessed on 17 November 2016).
- World Health Organization. Breastfeeding. Available online: http://www.who.int/nutrition/topics/exclusive_breastfeeding/es/ (accessed on 18 November 2016).
- Tanase-Nakao, K.; Arata, N.; Kawasaki, M.; Yasuhi, I.; Sone, H.; Mori, R.; Ota, E. Potential protective effect of lactation against incidence of type 2 diabetes in women with previous gestational diabetes mellitus: A systematic review and meta-analysis. Diabetes Metab. Res. Rev. 2017, 33, e2875. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health of Spain, Spanish Statistics Institute. National Health Survey 2017. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2017.htm (accessed on 18 November 2016).
- Health department of the Andalusian government. Screening for Metabolopathies Programme of Andalusian. Available online: https://www.juntadeandalucia.es/organismos/saludyfamilias/areas/salud-vida/salud-bebe/paginas/prueba-talon.html (accessed on 20 November 2016).
- Ministry of Health of Spain. Strategy for Health Promotion and Prevention in the National Health System. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/Estrategia/docs/EstrategiaPromocionSaludyPrevencionSNS.pdf (accessed on 20 November 2016).
- Ministry of Health, Social Services and Equality. Strategy for Nutrition, Physical Activity and the Prevention of Obesity (NAOS). Available online: http://www.aecosan.msssi.gob.es/AECOSAN/web/nutricion/seccion/estrategia_naos.htm (accessed on 20 November 2016).
- Primary Healthcare Service of Andalusian, Spain. Promotion of Breastfeeding. Available online: http://www.juntadeandalucia.es/servicioandaluzdesalud/principal/documentosacc.asp?pagina=gr_cartera_I_3_1_1_1 (accessed on 20 November 2016).
- Andalusian Government, Spain. Andalusian Integral Plan to Fight Obesity 2007–2012 (PIOBIN). Available online: https://www.juntadeandalucia.es/organismos/saludyfamilias/areas/planificacion/plan-integral/paginas/piobin.html (accessed on 20 November 2016).
- Santacruz-Salas, E.; Aranda-Reneo, I.; Segura-Fragoso, A.; Cobo-Cuenca, A.I.; Laredo-Aguilera, J.A.; Carmona-Torres, J.M. Mothers’ Expectations and Factors Influencing Exclusive Breastfeeding during the First 6 Months. Int. J. Environ. Res. Public Health 2019, 17, 77. [Google Scholar] [CrossRef] [PubMed]
- Sacristán, A.M.; Lozano, J.E.; Gil, M.; Vega, A.T. Situación actual y factores que condicionan la lactancia materna en Castilla y León. Rev. Pediatr. Aten. Primaria 2011, 13, 33–46. [Google Scholar] [CrossRef]
- Martinez-Galiano, J.M. Factores asociados al abandono de la lactancia materna. Metas Enfermería 2010, 13, 61–67. [Google Scholar]
- Fernández-Cañadas, A.; Durán, M.; Hernández, A.B.; Muriel, C.; Martínez, B.; Oscoz, A.; Pérez, P.; Salcedo, A.; Royuela, A.; Casillas, M.L.; et al. A comparison of factors associated with cessation of exclusive breastfeeding at 3 and 6 months. Breastfeed Med. 2017, 12, 430–435. [Google Scholar] [CrossRef]
- Brown, A.; Jordan, S. Impact of birth complications on breastfeeding duration: An internet survey. J. Adv. Nurs. 2013, 69, 828–839. [Google Scholar] [CrossRef]
- Carlander, A.K.; Edman, G.; Christensson, K.; Andolf, E.; Wiklund, I. Contact between mother, child and partner and attitudes towards breastfeeding in relation to mode of delivery. Sex. Reprod. Healthc. 2010, 1, 27–34. [Google Scholar] [CrossRef]
- Watt, S.; Sword, W.; Sheehan, D.; Foster, G.; Thabane, L.; Krueger, P.; Landy, C.K. The effect of delivery method on breastfeeding initiation from the the Ontario Mother and Infant Study (TOMIS) III. J. Obstet. Gynecol. Neonatal Nurs. 2012, 41, 728–737. [Google Scholar] [CrossRef]
- Fernandez-Cañadas, A.; Duran, M.; Hernandez, A.B.; Muriel, C.; Pérez, P.; Salcedo, A.; Royuela, A.; Casillas, M.L.; Marín, M.A. Cessation of breastfeeding in association with oxytocin administration and type of birth. A prospective cohort study. Women Birth 2019, 32, 43–48. [Google Scholar] [CrossRef]
- Hobbs, A.J.; Mannion, C.A.; McDonald, S.W.; Brockway, M.; Tough, S.C. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth 2016, 16, 90. [Google Scholar] [CrossRef]
- Regan, J.; Thompson, A.; DeFranco, E. The influence of mode of delivery on breastfeeding initiation in women with a prior cesarean delivery: A population-based study. Breastfeed Med. 2013, 8, 181–186. [Google Scholar] [CrossRef]
- Rabiepoor, S.; Hamidiazar, P.; Sadeghi, E. The relationship between type of delivery and successful breastfeeding. Int. J. Pediatr. (Masshad) 2017, 5, 4899–4907. [Google Scholar]
- Sharifi, F.; Nouraei, S.; Sharifi, N. Factors affecting the choice of type of delivery with breast feeding in Iranian mothers. Electron. Physician 2017, 9, 5265–5269. [Google Scholar] [CrossRef]
- Gil Urquiza, M.T. Factors that Intervene in the Start and Maintenance of Breastfeeding in Cantabria; Medical and Surgical Sciences, University of Cantabria: Santander, Spain, 2017. [Google Scholar]
- Herrera-Gómez, A.; Ramos-Torrecillas, J.; Ruiz, C.; Ocaña, F.; de Luna, E.; García-Martínez, O. Prevalencia del inicio precoz de la lactancia materna. Nutr. Hosp. 2019, 36, 786–791. [Google Scholar] [PubMed]
- Alvarez, R.; Serwint, J.R.; Levine, D.M.; Bertram, A.; Sattari, M. Lawyer mothers: Infant-feeding intentions and behavior. South Med. J. 2015, 108, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Health Canada; Canadian Paediatric Society; Dietitians of Canada; Breastfeeding Committee for Canada. Nutrition for healthy term infants: Recommendations from birth to six months. Can. J. Diet Pract. Res. 2012, 73, 204. [Google Scholar] [CrossRef] [PubMed]
- Mercado, J.A.M. Factors that Influence the Interruption of Exclusive Breastfeeding of Infants up to 6 Months of Age. Bachelor’s Medicine Thesis, University of Perú, Lima, Peru, 2017. [Google Scholar]
- Rojas, M.S.; Salvatierra, E.S.; Lahura, R.C.H. Factores asociados al inicio de la lactancia materna precoz. Rev. Peru. Investig. Matern. Perinat. 2019, 7, 31–36. [Google Scholar]
- Pertile, R.; Bombarda, L.; Pedron, M.; Clivati, E.; Piffer, S. Breastfeeding during the first year of life: Estimates using records generated in general pediatrics. Minerva Pediatr. 2019, 71, 116–124. [Google Scholar] [CrossRef]
- Lind, J.N.; Perrine, C.G.; Li, R. Relationship between use of labor pain medications and delayed onset of lactation. J. Hum. Lact. 2014, 30, 167–173. [Google Scholar] [CrossRef]
- French, C.A.; Cong, X.; Chung, K.S. Labor Epidural Analgesia and Breastfeeding: A Systematic Review. J. Hum. Lact. 2016, 32, 507–520. [Google Scholar] [CrossRef]
- Health Centres IHAN UNICEF/WHO, Initiative for a More Human Birth and Lactation Care. IHAN Health Centers Strategy. Manual for Accreditation. Available online: https://www.ihan.es/docs/documentacion-acreditacion/centros_salud/Manual_para_la_acreditacion_IHAN_en_AP_2018.pdf (accessed on 17 December 2016).
- Royal College of Obstetricians and Gynaecologists (RCOG). Perineal Tears during Childbirth. Royal College of Obstetricians and Gynaecologists. Available online: https://www.rcog.org.uk/en/patients/tears/tears-childbirth/ (accessed on 20 November 2016).
- Aasheim, V.; Nilsen, A.; Reinar, L.; Lukasse, M. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst. Rev. 2017, 6, CD006672. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health of Spain, Spanish Statistics. Institute Fertility Indicators. Available online: https://www.ine.es/dynt3/inebase/es/index.htm?padre=1149&capsel=2044 (accessed on 25 February 2020).
- Ministry of Health of Spain, Spanish Statistics Institute. Type of Breastfeeding According to Sex and Autonomous Community. Population from 6 Months to 4 Years. Available online: https://www.ine.es/jaxi/tabla.do?path=/t15/p419/a2006/p07/l0/&file=03111.px&type=pcaxis&L=0 (accessed on 25 February 2020).
- Theurich, M.A.; Davanzo, R.; Busck-Rasmussen, M.; Díaz-Gómez, N.M.; Brennan, C.; Kylberg, E.; Baerug, A.; McHugh, L.; Weikert, C.; Abraham, K.; et al. Breastfeeding Rates and Programs in Europe: A Survey of 11 National Breastfeeding Committees and Representatives. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 400–407. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | N | % |
|---|---|---|
| Parity | ||
| Primiparous | 64 | 53.30% |
| Multiparous | 56 | 46.6% |
| Breastfeeding Education a | 57 | 47.20% |
| Mode of Birth | ||
| Vaginal | 95 | 79.60% |
| Obstetric | 14 | 11.60% |
| Caesarean | 11 | 9.10% |
| Epidural Analgesia a | 57 | 47.40% |
| Episiotomy a | 24 | 20.60% |
| Perineal Tears | ||
| No trauma | 70 | 58.30% |
| Type I | 17 | 14.10% |
| Type II | 31 | 25.80% |
| Type III | 2 | 1.60% |
| Sex of Newborn | ||
| Female | 72 | 60.10% |
| Male | 48 | 39.80% |
| MA | BE | P | EA | E | PT | MB | L1 | L3 | L6 | BD | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| MA | - | ||||||||||
| BE | - | - | |||||||||
| P | 0.299 ** | 0.271 ** | - | ||||||||
| EA | - | - | 0.283 ** | - | |||||||
| E | 0.205 * | - | - | - | - | ||||||
| PT | - | - | −0.071 ** | - | 0.356 * | - | |||||
| MB | - | - | - | −0.314 ** | - | - | - | ||||
| L1 | - | - | - | - | 0.112 * | - | - | - | |||
| L3 | - | - | - | −0.140 ** | - | - | - | 0.497 ** | - | ||
| L6 | - | - | 0.051 ** | 0.013 ** | 0.347 * | - | - | 0.417 ** | 0.704 ** | - | |
| BD | - | - | −0.055 ** | 0.057 ** | −0.267 ** | - | - | −0.602 ** | −0.846 ** | - | - |
| Type of Lactation 1 Month | Type of Lactation 3 Months | ||||
|---|---|---|---|---|---|
| BF | ML | BF | ML | FF | |
| Perineal Tear | |||||
| No | |||||
| Corrected residuals | 1.2 | −1.2 | 2.1 | −1.6 | −1.1 |
| Type I | |||||
| Corrected residuals | 1.2 | −1.2 | −3.5 | 1.0 | 3.5 |
| Type II | |||||
| Corrected residuals | −2.2 | 2.2 | 0.4 | 1.1 | −1.5 |
| Type III | |||||
| Corrected residuals | 0.4 | −0.4 | 0.7 | −0.4 | −0.5 |
| Breastfeeding | Mixed Lactation | Formula Feeding | ||
|---|---|---|---|---|
| Perineal Tears | ||||
| No | Corrected Residuals | 1.0 | 0.4 | −1.3 |
| Type I | Corrected Residuals | −1.4 | −1.6 | 2.9 |
| Type II | Corrected Residuals | −0.3 | 1.0 | −0.6 |
| Type III | Corrected Residuals | 1.3 | −0.6 | −0.8 |
| Episiotomy | ||||
| Yes | Corrected Residuals | 3.3 | −0.6 | −2.8 |
| No | Corrected Residuals | −3.3 | 0.6 | 2.8 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agea-Cano, I.; Linares-Abad, M.; Ceballos-Fuentes, A.G.; Calero-García, M.J. Breastfeeding at 1, 3 and 6 Months after Birth according to the Mode of Birth: A Correlation Study. Int. J. Environ. Res. Public Health 2020, 17, 6828. https://doi.org/10.3390/ijerph17186828
Agea-Cano I, Linares-Abad M, Ceballos-Fuentes AG, Calero-García MJ. Breastfeeding at 1, 3 and 6 Months after Birth according to the Mode of Birth: A Correlation Study. International Journal of Environmental Research and Public Health. 2020; 17(18):6828. https://doi.org/10.3390/ijerph17186828
Chicago/Turabian StyleAgea-Cano, Irene, Manuel Linares-Abad, Antonio Gregorio Ceballos-Fuentes, and María José Calero-García. 2020. "Breastfeeding at 1, 3 and 6 Months after Birth according to the Mode of Birth: A Correlation Study" International Journal of Environmental Research and Public Health 17, no. 18: 6828. https://doi.org/10.3390/ijerph17186828
APA StyleAgea-Cano, I., Linares-Abad, M., Ceballos-Fuentes, A. G., & Calero-García, M. J. (2020). Breastfeeding at 1, 3 and 6 Months after Birth according to the Mode of Birth: A Correlation Study. International Journal of Environmental Research and Public Health, 17(18), 6828. https://doi.org/10.3390/ijerph17186828





