Professional Quality of Life and Mental Health Outcomes among Health Care Workers Exposed to Sars-Cov-2 (Covid-19)
Abstract
1. Introduction
1.1. Literature Background
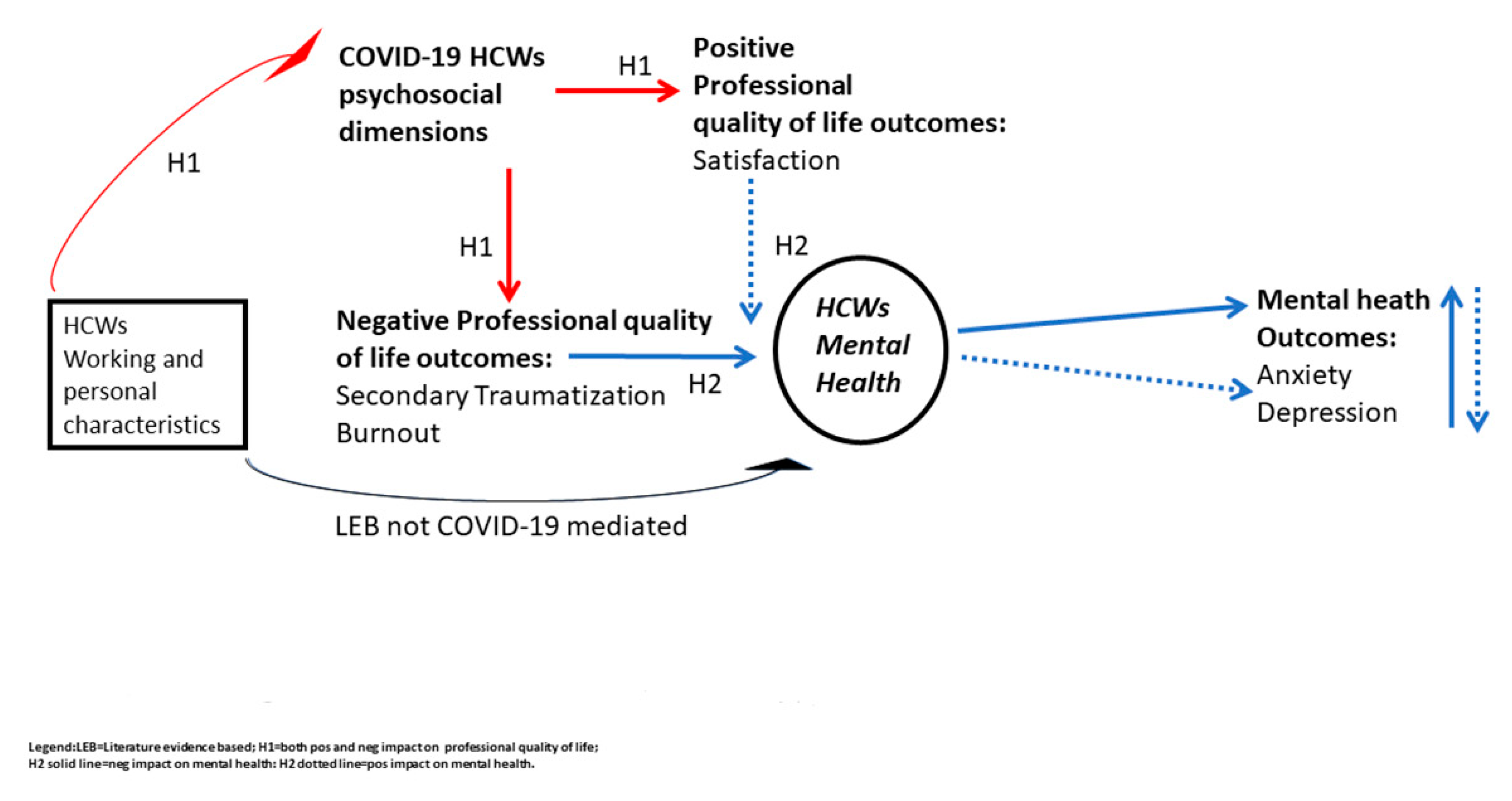
1.2. Study Aim and Hypotheses
2. Materials and Methods
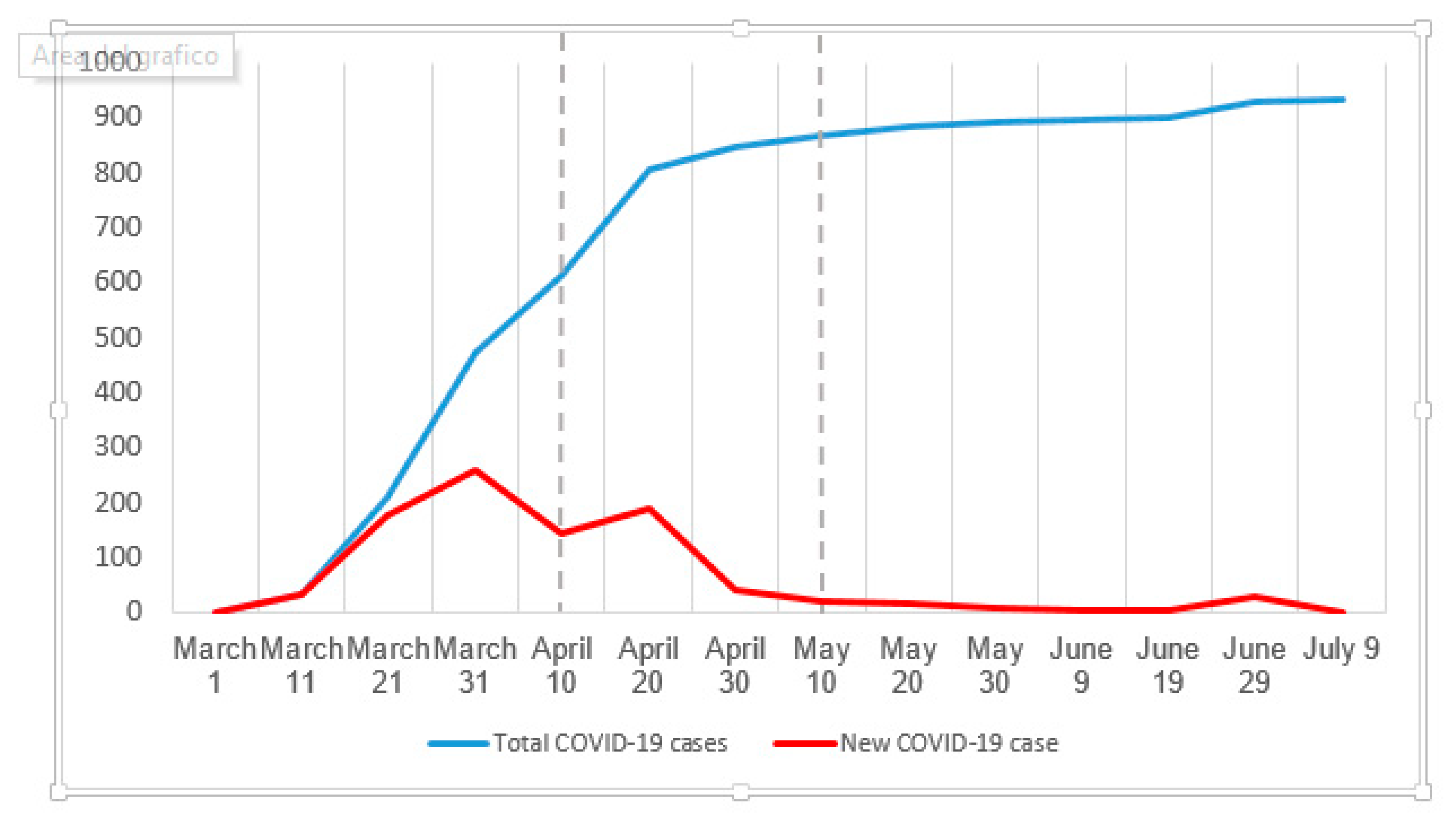
2.1. Study Sample and Procedures
2.2. Measures
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- WHO. Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV). 2020. Available online: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (accessed on 15 February 2020).
- WHO. Coronavirus Disease (COVID-19) Situation Report 163; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Orsini, A.; Corsi, M.; Santangelo, A.; Riva, A.; Peroni, D.; Foiadelli, T.; Savasta, S.; Striano, P. Challenges and management of neurological and psychiatric manifestations in SARS-CoV-2 (COVID-19) patients. Neurol. Sci. 2020, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Buselli, R.; Carmassi, C.; Corsi, M.; Baldanzi, S.; Battistin, G.; Chiumiento, M.; Massimetti, G.; Dell’Osso, L.; Cristaudo, A. Post-Traumatic stress symptoms in an Italian cohort of subjects complaining occupational stress. CNS Spectrum 2020, 1–27. [Google Scholar] [CrossRef]
- Buselli, R.; Veltri, A.; Baldanzi, S.; Marino, R.; Bonotti, A.; Chiumiento, M.; Girardi, M.; Pellegrini, L.; Guglielmi, G.; Dell’Osso, L.; et al. Plasma Brain-Derived Neurotrophic Factor (BDNF) and serum cortisol levels in a sample of workers exposed to occupational stress and suffering from Adjustment Disorders. Brain Behav. 2019, 9, e01298. [Google Scholar] [CrossRef]
- Buselli, R.; Baldanzi, S.; Corsi, M.; Chiumiento, M.; Del Lupo, E.; Carmassi, C.; Dell’Osso, L.; Cristaudo, A. Psychological Care of Health Workers during the COVID-19 Outbreak in Italy: Preliminary Report of an Occupational Health Department (AOUP) Responsible for Monitoring Hospital Staff Condition. Sustainability 2020, 12, 5039. [Google Scholar] [CrossRef]
- Ramaci, T.; Barattucci, M.; Ledda, C.; Rapisarda, V. Social Stigma during COVID-19 and its Impact on HCWs Outcomes. Sustainability 2020, 12, 3834. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatry 2020, 52, 102066. [Google Scholar] [CrossRef]
- Liu, C.-Y.; Yang, Y.-Z.; Zhang, X.-M.; Xu, X.; Dou, Q.-L.; Zhang, W.-W.; Cheng, A.S.K. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol. Infect. 2020, 148, 1–17. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated with Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Chong, M.-Y.; Wang, W.-C.; Hsieh, W.-C.; Lee, C.-Y.; Chiu, N.-M.; Yeh, W.-C.; Huang, T.-L.; Wen, J.-K.; Chen, C.-L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry 2004, 185, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Wu, P. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry 2009, 54, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Salimi, R.; Gomar, R.; Heshmati, B. The COVID-19 outbreak in Iran. J. Glob. Health 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Wang, J.; Luo, C.; Hu, S.; Lin, X.; Anderson, A.E.; Bruera, E.; Yang, X.; Wei, S.; Qian, Y. A Comparison of Burnout Frequency Among Oncology Physicians and Nurses Working on the Frontline and Usual Wards During the COVID-19 Epidemic in Wuhan, China. J. Pain Symptom Manag. 2020, 60, e60–e65. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Fernández, M.D.; Pérez-García, E.; Ortega-Galán, A.M. Quality of Life in Nursing Professionals: Burnout, Fatigue, and Compassion Satisfaction. Int. J. Environ. Res. Public Health 2020, 17, 1253. [Google Scholar] [CrossRef] [PubMed]
- Tieges, Z.; McGregor, D.; Georgiou, M.; Smith, N.; Saunders, J.; Millar, R.; Morison, G.; Chastin, S. The Impact of Regeneration and Climate Adaptations of Urban Green–Blue Assets on All-Cause Mortality: A 17-Year Longitudinal Study. Int. J. Environ. Res. Public Health 2020, 17, 4577. [Google Scholar] [CrossRef]
- Hunsaker, S.; Chen, H.-C.; Maughan, D.; Heaston, S. Factors That Influence the Development of Compassion Fatigue, Burnout, and Compassion Satisfaction in Emergency Department Nurses. J. Nurs. Scholarsh. 2015, 47, 186–194. [Google Scholar] [CrossRef]
- Sacco, T.L.; Ciurzynski, S.M.; Harvey, M.E.; Ingersoll, G.L. Compassion Satisfaction and Compassion Fatigue Among Critical Care Nurses. Crit. Care Nurse 2015, 35, 32–42. [Google Scholar] [CrossRef]
- Nolte, A.G.; Downing, C.; Temane, A.; Hastings-Tolsma, M. Compassion fatigue in nurses: A metasynthesis. J. Clin. Nurs. 2017, 26, 4364–4378. [Google Scholar] [CrossRef]
- Potter, P.; Deshields, T.; Divanbeigi, J.; Berger, J.; Cipriano, D.; Norris, L.; Olsen, S. Compassion Fatigue and Burnout. Clin. J. Oncol. Nurs. 2010, 14, e56–e62. [Google Scholar] [CrossRef]
- Kelly, L.; Runge, J.; Spencer, C. Predictors of Compassion Fatigue and Compassion Satisfaction in Acute Care Nurses. J. Nurs. Sch. 2015, 47, 522–528. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Ruotsalainen, J.; Serra, C.; Mariné, A.; Verbeek, J.H. Systematic review of interventions for reducing occupational stress in health care workers. Scand. J. Work. Environ. Health 2008, 34, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Y.-T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef]
- Magnavita, N.; Tripepi, G.; Di Prinzio, R.R. Symptoms in Health Care Workers during the COVID-19 Epidemic. A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 5218. [Google Scholar] [CrossRef]
- Carmassi, C.; Gesi, C.; Corsi, M.; Cremone, I.M.; Bertelloni, C.; Massimetti, E.; Olivieri, M.C.; Conversano, C.; Santini, M.; Dell’Osso, L. Exploring PTSD in emergency operators of a major University Hospital in Italy: A preliminary report on the role of gender, age, and education. Ann. Gen. Psychiatry 2018, 17, 17. [Google Scholar] [CrossRef]
- Carmassi, C.; Cerveri, G.; Bui, E.; Gesi, C.; Dell’Osso, L. Defining Effective Strategies to Prevent Post-Traumatic Stress in Healthcare Emergency Workers Facing the COVID-19 Pandemic in Italy. CNS Spectr. 2020, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Foghi, C.; Dell’Oste, V.; Cordone, A.; Bertelloni, C.A.; Bui, E.; Dell’Osso, L. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID-19 pandemic. Psychiatry Res. 2020, 292, 113312. [Google Scholar] [CrossRef] [PubMed]
- Spoorthy, M.S.; Pratapa, S.K.; Mahant, S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J. Psychiatry 2020, 51, 102119. [Google Scholar] [CrossRef] [PubMed]
- Stamm, B.H. The Concise ProQOL Manual. 2010. Pocatello, ID: ProQOL.org. Available online: http://ProQOL.org/uploads/ProQOL_Concise_2ndEd_12-2010.pdf (accessed on 10 July 2020).
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Mo, Y.; Deng, L.; Zhang, L.; Lang, Q.; Liao, C.; Wang, N.; Qin, M.; Huang, H. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020, 28, 1002–1009. [Google Scholar] [CrossRef] [PubMed]
- Park, C.L.; Mills-Baxter, M.A.; Fenster, J.R. Post-Traumatic Growth from Life’s Most Traumatic Event: Influences on Elders’ Current Coping and Adjustment. Traumatology 2005, 11, 297–306. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Gorringe, G.; Menaker, R.; Storz, K.A.; Reeves, D.; Buskirk, S.J.; Sloan, J.A.; Swensen, S.J. Impact of Organizational Leadership on Physician Burnout and Satisfaction. Mayo Clin. Proc. 2015, 90, 432–440. [Google Scholar] [CrossRef]
- Kessler, R.C.; Chiu, W.T.; Demler, O.V.; Walters, E.E.; Merikangas, K.R. Prevalence, Severity, and Comorbidity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Tolin, D.F.; Foa, E.B. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychol. Bull. 2006, 132, 959–992. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Corsi, M.; Bertelloni, C.A.; Pedrinelli, V.; Massimetti, G.; Peroni, D.; Bonuccelli, A.; Orsini, A.; Dell’Osso, L. Post-traumatic stress spectrum symptoms in parents of children affected by epilepsy: Gender differences. Seizure 2020, 80, 169–174. [Google Scholar] [CrossRef]
- Olff, M. Sex and gender differences in post-traumatic stress disorder: An update. Eur. J. Psychotraumatol. 2017, 8, 1351204. [Google Scholar] [CrossRef]
- Carmassi, C.; Foghi, C.; Dell’Oste, V.; Bertelloni, C.A.; Fiorillo, A.; Dell’Osso, L. Risk and Protective Factors for PTSD in Caregivers of Adult Patients with Severe Medical Illnesses: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 5888. [Google Scholar] [CrossRef]
- Jakimowicz, S.; Perry, L.; Lewis, J. Compassion satisfaction and fatigue: A cross-sectional survey of Australian intensive care nurses. Aust. Crit. Care 2018, 31, 396–405. [Google Scholar] [CrossRef]
| N (%) | Compassion Satifaction (Mean ± SD) | p | Burnout (Mean ± SD) | p | Secondary Traumatic Stress (Mean ± SD) | p | PHQ-9 (Mean ± SD) | p | GAD-7 (Mean ± SD) | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total sample | 265 (100.0) | 38.2 ± 7.0 | - | 19.8 ± 5.0 | - | 18.0 ± 5.6 | - | 4.5 ± 6.4 | - | 4.2 ± 4.6 | - |
| Male | 84 (31.7) | 37.3 ± 6.4 | 0.095 (Choen’s d = −0.19) | 19.2 ± 4.1 | 0.519 | 16.8 ± 4.7 | 0.041 (Choen’s d = −0.34) | 4.0 ± 5.8 | 0.412 | 3.3 ± 4.0 | 0.020 (Choen’s d = −030) |
| Female | 181 (68.9) | 38.6 ± 7.3 | 20.1 ± 5.3 | 18.6 ± 5.9 | 4.8 ± 6.7 | 4.7 ± 4.8 | |||||
| ICU staff | 78 (29.4) | 39.3 ± 5.7 | 0.084 | 19.9 ± 5.0 | 0.586 | 18.0 ± 6.3 | 0.535 | 4.9 ± 6.5 | 0.088 | 4.5 ± 4.6 | 0.073 |
| no-ICU staff | 187 (70.6) | 37.8 ± 7.5 | 19.7 ± 4.8 | 18.0 ± 5.3 | 3.7 ± 6.2 | 3.7 ± 4.5 | |||||
| First line staff | 117 (44.2) | 39.4 ± 5.5 | 0.008 (Choen’s d = 0.31) | 19.8 ± 4.9 | 0.598 | 18.3 ± 6.1 | 0.955 | 4.7 ± 5.9 | 0.245 | 4.1 ± 3.9 | 0.486 |
| no-First line staff | 148 (55.8) | 37.3 ± 7.9 | 19.8 ± 5.0 | 17.9 ± 5.2 | 4.4 ± 7.0 | 4.5 ± 5.3 | |||||
| Hospital duty time <1 year | 51 (19.2) | 39.3 ± 6.4 | 0.205 | 18.6 ± 3.9 | 0.084 | 17.2 ± 6.0 | 0.103 | 4.9 ± 6.4 | 0.13 (Choen’s d = 0.30) | 4.5 ± 4.7 | 0.014 (Choen’s d = 0.35) |
| Hospital duty time ≥1 year | 214 (80.8) | 38.0 ± 7.2 | 20.1 ± 5.1 | 18.2 ± 5.5 | 3.0 ± 6.4 | 3.0 ± 3.8 | |||||
| Physicians | 85 (32.1) | 37.1 ± 5.6 | 0.021 * | 20.2 ± 4.4 | 0.062 | 18.0 ± 5.7 | 0.208 | 5.4 ± 6.2 | 0.083 | 4.4 ± 3.8 | 0.087 |
| Nurses | 133 (50.2) | 38.4 ± 6.8 | 19.9 ± 4.7 | 18.5 ± 5.8 | 4.4 ± 6.7 | 4.56 ± 5.23 | |||||
| Healthcare assistants | 47 (17.7) | 40.0 ± 9.4 | 18.9 ± 6.6 | 16.7 ± 4.9 | 3.4 ± 5.8 | 3.1 ± 3.6 |
| Predictive Factors | b (S.E.) | β | CI95% | p |
|---|---|---|---|---|
| Age | −0.01 (0.04) | −0.02 | −0.078–0.060 | 0.794 |
| Gender | −0.42 (0.83) | −0.03 | −2.045–1.210 | 0.614 |
| Physician role | 0.94 (0.84) | −0.07 | −0.722–2.600 | 0.266 |
| First line activity | 1.36 (1.14) | 0.10 | −0.885–3.597 | 0.234 |
| ICU working | −2.08 (1.23) | −0.15 | −4.506–0.351 | 0.093 |
| Compassion Satisfaction | −0.03 (0.05) | −0.04 | −0.138–0.074 | 0.557 |
| Burnout | 0.39 (0.10) | 0.30 | 0.190–0.589 | <0.001 |
| Secondary Traumatization | 0.24 (0.09) | 0.21 | 0.067–0.421 | 0.007 |
| k | −5.50 (3.26) | - | −11.930–0.924 | 0.093 |
| Predictive Factors | b (S.E.) | β | CI95% | p |
|---|---|---|---|---|
| Age | −0.03 (0.02) | −0.07 | −0.070–0.009 | 0.129 |
| Gender | 0.15 (0.48) | 0.02 | −0.789–1.084 | 0.757 |
| Physician role | 0.12 (0.49) | 0.01 | −0.836–1.075 | 0.806 |
| First line activity | 1.76 (0.65) | 0.19 | 0.470–3.048 | 0.008 |
| ICU working | −2.29 (0.71) | −0.23 | −3.683–0.889 | 0.001 |
| Compassion Satisfaction | −0.00 (0.03) | −0.00 | −0.064–0.058 | 0.933 |
| Burnout | 0.20 (0.06) | 0.22 | 0.085–0.314 | 0.001 |
| Secondary Traumatization | 0.42 (0.05) | 0.52 | 0.319–0.522 | <0.001 |
| k | −6.24 (1.88) | - | −9.938–−2.544 | 0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buselli, R.; Corsi, M.; Baldanzi, S.; Chiumiento, M.; Del Lupo, E.; Dell'Oste, V.; Bertelloni, C.A.; Massimetti, G.; Dell’Osso, L.; Cristaudo, A.; et al. Professional Quality of Life and Mental Health Outcomes among Health Care Workers Exposed to Sars-Cov-2 (Covid-19). Int. J. Environ. Res. Public Health 2020, 17, 6180. https://doi.org/10.3390/ijerph17176180
Buselli R, Corsi M, Baldanzi S, Chiumiento M, Del Lupo E, Dell'Oste V, Bertelloni CA, Massimetti G, Dell’Osso L, Cristaudo A, et al. Professional Quality of Life and Mental Health Outcomes among Health Care Workers Exposed to Sars-Cov-2 (Covid-19). International Journal of Environmental Research and Public Health. 2020; 17(17):6180. https://doi.org/10.3390/ijerph17176180
Chicago/Turabian StyleBuselli, Rodolfo, Martina Corsi, Sigrid Baldanzi, Martina Chiumiento, Elena Del Lupo, Valerio Dell'Oste, Carlo Antonio Bertelloni, Gabriele Massimetti, Liliana Dell’Osso, Alfonso Cristaudo, and et al. 2020. "Professional Quality of Life and Mental Health Outcomes among Health Care Workers Exposed to Sars-Cov-2 (Covid-19)" International Journal of Environmental Research and Public Health 17, no. 17: 6180. https://doi.org/10.3390/ijerph17176180
APA StyleBuselli, R., Corsi, M., Baldanzi, S., Chiumiento, M., Del Lupo, E., Dell'Oste, V., Bertelloni, C. A., Massimetti, G., Dell’Osso, L., Cristaudo, A., & Carmassi, C. (2020). Professional Quality of Life and Mental Health Outcomes among Health Care Workers Exposed to Sars-Cov-2 (Covid-19). International Journal of Environmental Research and Public Health, 17(17), 6180. https://doi.org/10.3390/ijerph17176180









