The Pros and Cons of the Prediction Game: The Never-ending Debate of Mortality in the Intensive Care Unit
Abstract
1. Introduction
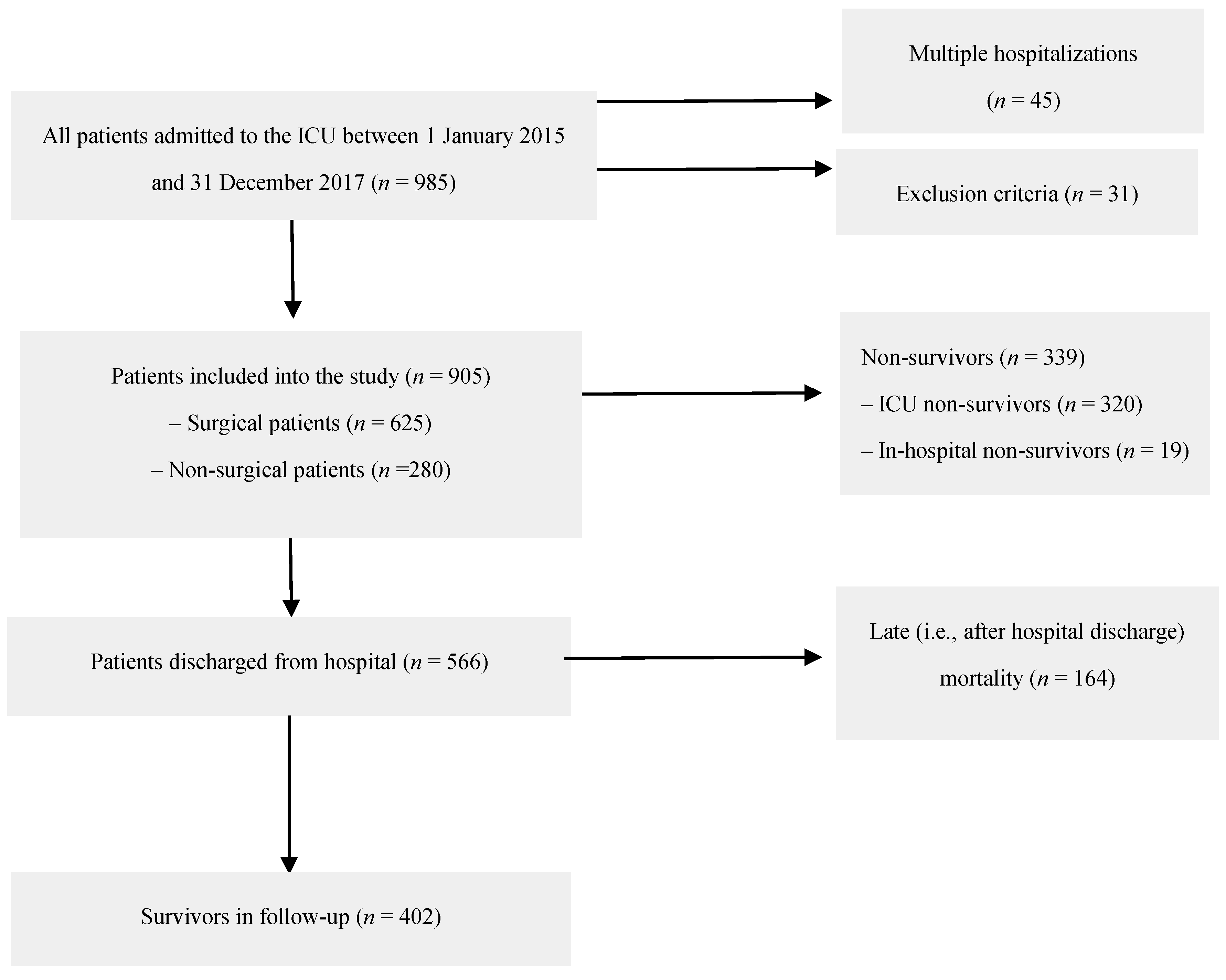
2. Materials and Methods
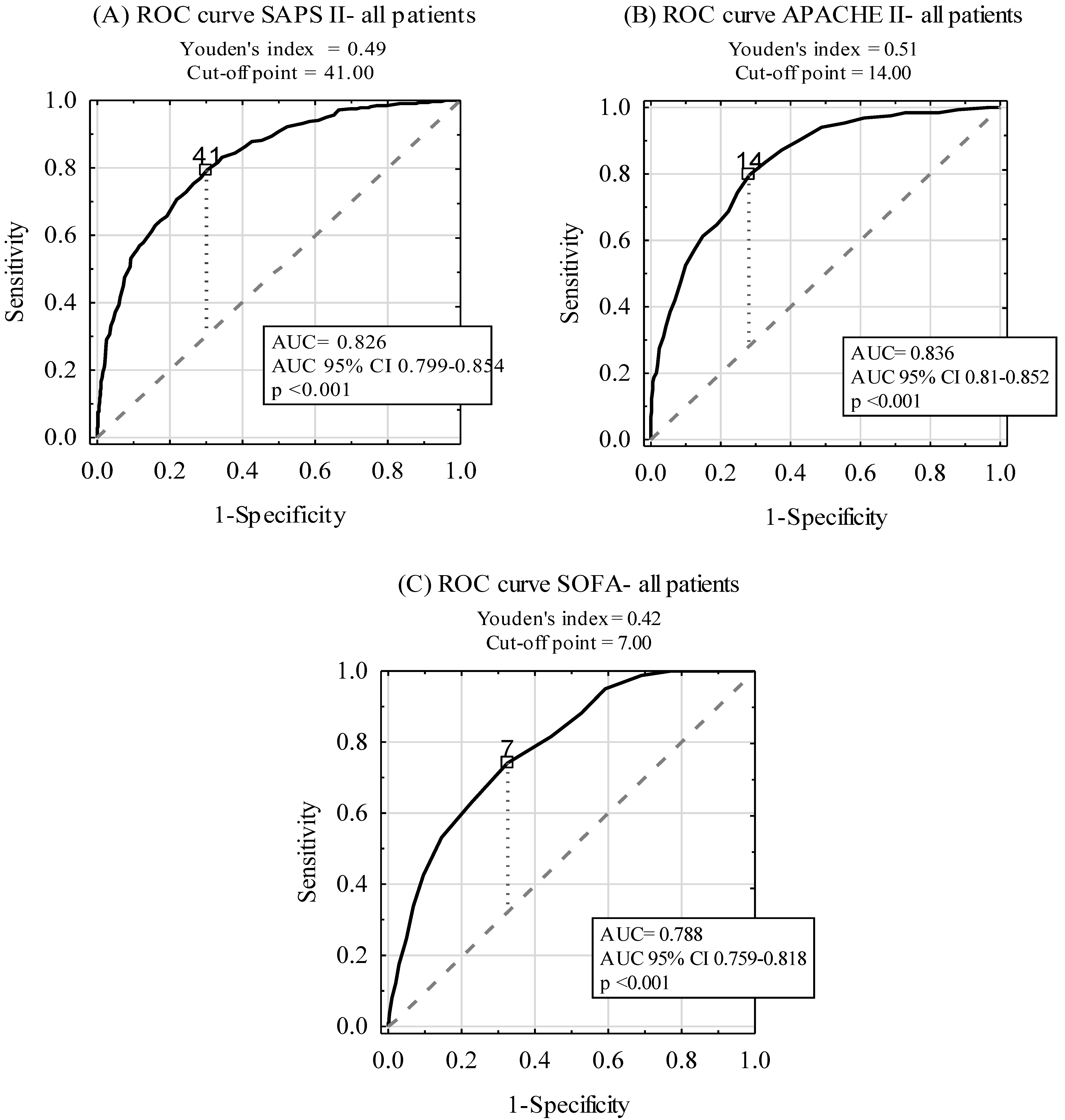
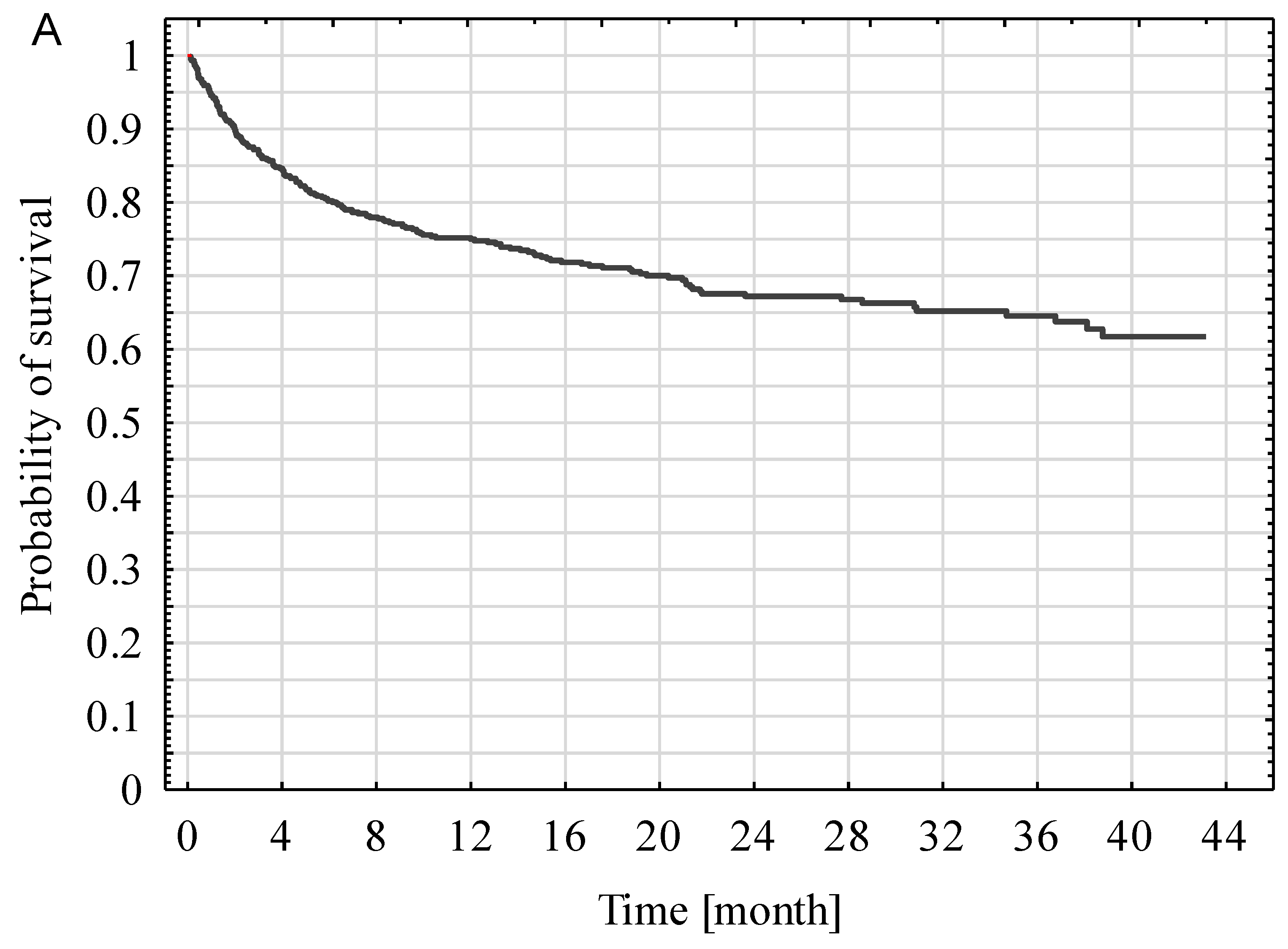
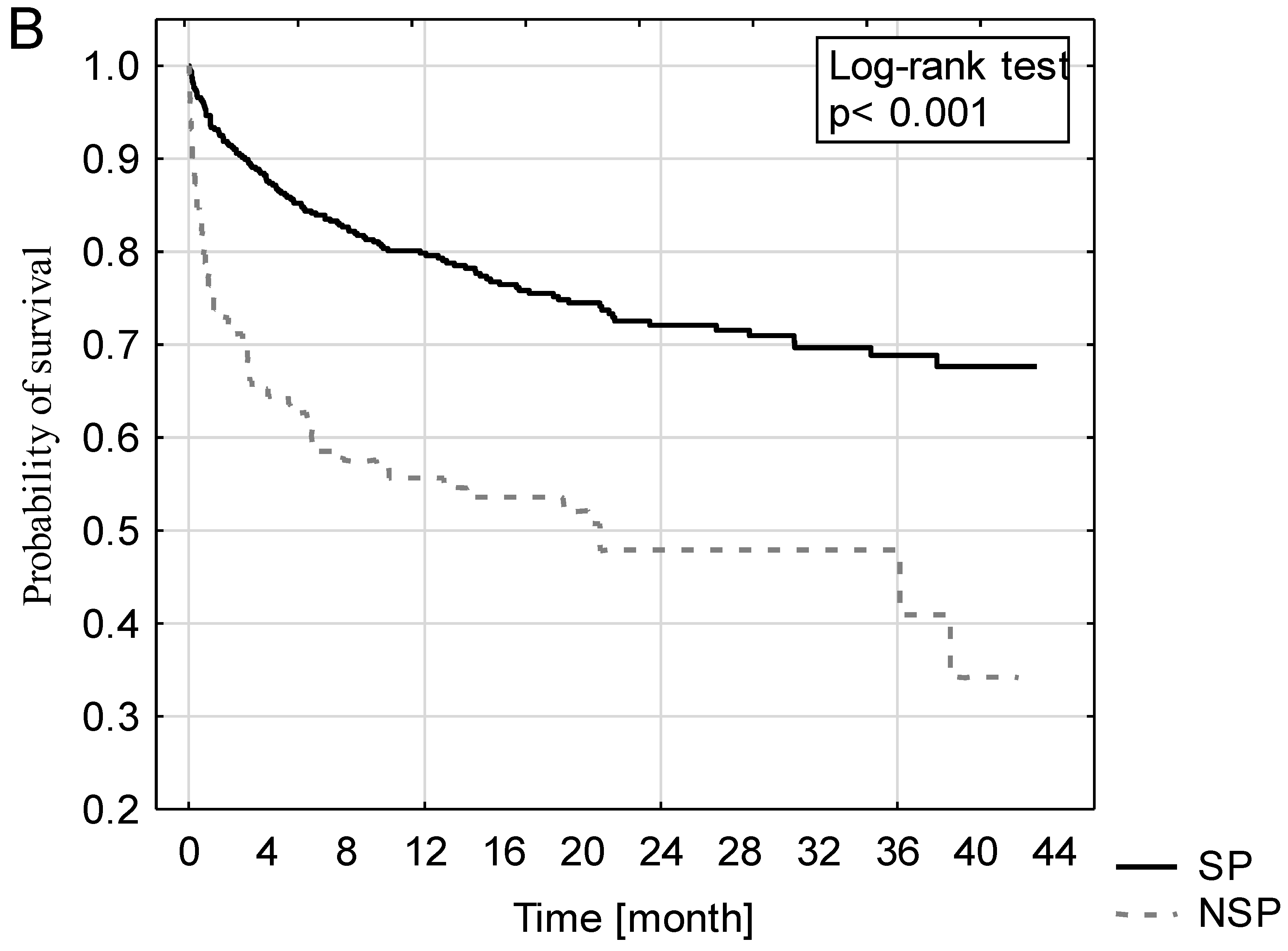
3. Results
4. Discussion
5. Conclusions
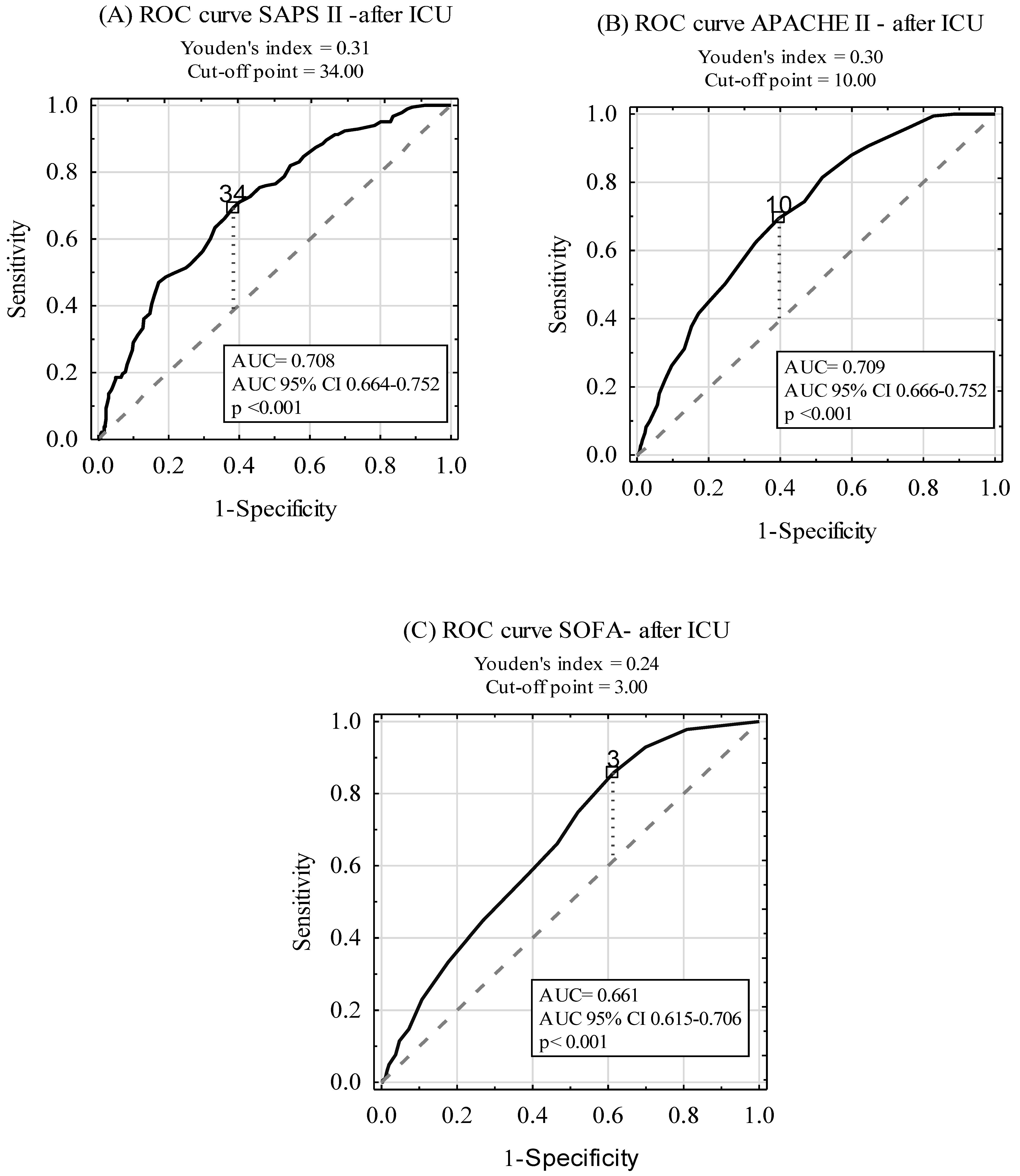
- APACHE II and SAPS II are good predictors of the ICU mortality.
- APACHE II, SAPS II, and SOFA fail to predict long-term mortality.
- Surgical patients have better prognosis than medical ICU patients.
- Further studies are needed to create reliable tools for the prognostication of critically ill patients successfully discharged from the ICU.
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ICU | Intensive Care Unit |
| SAPS | Simplified Acute Physiology Score |
| APACHE | Acute Physiology and Chronic Health Evaluation |
| SOFA | Sequential Organ Failure Assessment |
| SCCM | Society of Critical Care Medicine |
| SP | surgical patients (subjects) |
| NSP | non-surgical patients (subjects) |
References
- Weigl, W.; Adamski, J.; Goryński, P.; Kański, A.; Hultström, M. Mortality rate is higher in polish intensive care units than in other European countries. Intensive Care Med. 2017, 43, 1430–1432. [Google Scholar] [CrossRef] [PubMed]
- Adamski, J.; Goraj, R.; Onichimowski, D.; Gawlikowska, E.; Weigl, W. The differences between two selected intensive care units located in central and northern Europe—preliminary observation. Anaesthesiol. Intensive Ther. 2015, 47, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Knapik, P.; Krzych, Ł.J.; Weigl, W.; Adamski, J.; Hultstom, M. Mortality rate in polish intensive care units is lower than predicted according to the APACHE II scoring system. Intensive Care Med. 2017, 43, 1745–1746. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Siegel, T.; Adamski, J.; Nowakowski, P.; Onichimowski, D.; Weigl, W. Prospective assessment of standardized mortality ratio (SMR) as a measure of quality of care in intensive care unit—a single-centre study. Anaesthesiol. Intensive Ther. 2015, 47, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Lefrant, J.Y.; Kotfis, K.; Nanchal, R.; Martin-Loeches, I.; Wittebole, X.; Sakka, S.G.; Pickkers, P.; Moreno, R. Comparison of European ICU patients in 2012 (ICON) versus 2002 (SOAP). Intensive Care Med. 2018, 44, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: a severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Lemeshow, S.; Le-Gall, J.R. Modeling the severity of illness of ICU patients a systems update. JAMA 1994, 272, 1049–1055. [Google Scholar] [CrossRef]
- Safari, S.; Shojaee, M.; Rahmati, F.; Barartloo, A.; Hahshemi, B.; Forouzanfar, M.M.; Mohammadi, E. Accuracy of SOFA score in prediction of 30-day outcome of critically ill patients. Turk. J. Emerg. Med. 2016, 16, 146–150. [Google Scholar] [CrossRef]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Rapsang, A.G.; Shyam, D.C. Scoring systems in the intensive care unit: A compendium. Indian J. Crit. Care Med. 2014, 18, 220–228. [Google Scholar] [CrossRef]
- Niewiński, G.; Starczewska, M.; Kański, A. Prognostic scoring systems for mortality in intensive care units- the APACHE model. Anaesthesiol. Intensive Ther. 2014, 46, 46–49. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Lim, C.W.; Hong, H.P.; Ju, J.W.; Jeon, Y.T.; Hwang, J.W.; Park, H.P. Efficacy of the APACHE II Score at ICU Discharge in Predicting post-ICU Mortality and ICU readmission in critically ill surgical patients. Anaesth. Intensive Care 2015, 43, 175–186. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.J.; Cook, J.A.; Adey, G.; Cuthbertson, B.H. Predicting death and readmission after intensive care discharge. Br. J. Anaesth. 2008, 100, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Lin, M.C.; Lin, Y.C.; Chang, H.W. ICU discharge APACHE II scores help to predict post-ICU death. Chang Gung Med. J. 2007, 30, 142–150. [Google Scholar] [PubMed]
- Rojek-Jarmuła, A.; Hombach, R.; Krzych, Ł. Does the APACHE II score predict performance of activities of daily living in patients discharged from a weaning center? Polish J. Thorac. Cardiovasc. Surg. 2016, 13, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Aminiahidashti, H.; Bozorgi, F.; Montazer, S.H.; Baboli, M.; Firouzian, A. Comparison of APACHE II and SAPS II scoring systems in prediction of critically Ill patients’ outcome. Emerg (Tehran) 2017, 5, e4. [Google Scholar] [PubMed]
- Le Gall, J.-R.; Lameshow, S.; Saulnier, F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 1993, 270, 2957–2963. [Google Scholar] [CrossRef]
- Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Guidelines for intensive care unit admission, discharge, and triage. Crit. Care Med. 1999, 27, 633–638. [Google Scholar] [CrossRef]
- Czempik, P.; Cieśla, D.; Knapik, P.; Krzych, Ł. Mortality of patients with acute kidney injury requiring renal replacement therapy. Adv. Clin. Exp. Med. 2018, 27, 327–333. [Google Scholar] [CrossRef]
- Naqvi, I.H.; Mahmood, K.; Ziaullaha, S.; Kashif, S.M.; Sharif, A. Better prognostic marker in ICU - APACHE II, SOFA or SAPS II. Pak. J. Med. Sci. 2016, 32, 1146–1151. [Google Scholar] [CrossRef]
- Khwannimit, B.; Geater, A. A comparison of APACHE II and SAPS II scoring systems in predicting hospital mortality in Thai adult intensive care units. J. Med. Assoc. Thai. 2007, 90, 643–652. [Google Scholar] [PubMed]
- Sadaka, F.; EthmaneAbouElMaali, C.; Cytron, M.A.; Fowler, K.; Javaux, V.M.; O’Brien, J. Predicting mortality of patients with sepsis: A comparison of APACHE II and APACHE III scoring systems. J. Clin. Med. Res. 2017, 9, 907–910. [Google Scholar] [CrossRef] [PubMed]
- Beck, D.H.; Smith, G.B.; Pappachan, J.V.; Millar, B. External validation of the SAPS II, APACHE II and APACHE III prognostic models in South England: A multicentre study. Intensive Care Med. 2003, 29, 249. [Google Scholar] [CrossRef] [PubMed]
- Gilani, M.T.; Razavi, M.; Azad, A. A comparison of Simplified Acute Physiology Score II, Acute Physiology and Chronic Health Evaluation II and Acute Physiology and Chronic Health Evaluation III scoring system in predicting mortality and length of stay at surgical intensive care unit. Niger Med. J. 2014, 55, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Sungurtekin, H.; Gurses, E.; Balci, C. Evaluation of several clinical scoring tools in organophosphate poisoned patients. Clin. Toxicol. (Phila) 2006, 44, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, A.L.; Watts, C. Patients readmitted to ICUs: A systematic review of risk factors and outcomes. Chest 2000, 118, 492–502. [Google Scholar] [CrossRef]
- Wallis, C.B.; Davies, H.T.; Shearer, A.J. Why do patients die on general wards after discharge from intensive care units? Anaesthesia 1997, 52, 9–14. [Google Scholar] [CrossRef]
- Daly, K.; Beale, R.; Chang, R.W. Reduction in mortality after inappropriate early discharge from intensive care unit: Logistic regression triage model. BMJ 2001, 322, 1274–1276. [Google Scholar] [CrossRef]
| Score | SAPS II | APACHE II | SOFA | |
|---|---|---|---|---|
| Overall | 41.1 ± 20.34 | 14.07 ± 8.73 | 6.33 ± 4.12 | |
| Reason for admission | Surgical | 36.01 ± 18.86 | 11.67 ± 7.59 | 5.51 ± 3.9 |
| Nonsurgical | 52.44 ± 18.9 | 19.44 ± 8.72 | 8.15 ± 4.03 | |
| ‘p’ | <0.001 | <0.001 | <0.001 | |
| Priority of admission | First | 42.47 ± 18.73 | 14.45 ± 8.26 | 6.7 ± 3.83 |
| Second | 15.89 ± 9.85 | 4.88 ± 3.47 | 0.92 ± 1.84 | |
| Third | 63.54 ± 16.44 | 24.0 2± 7.62 | 9.92 ± 3.04 | |
| ‘p’ | <0.001 | <0.001 | <0.001 | |
| Score | ICU Survivors | ICU Non-survivors | ‘p’ | |
|---|---|---|---|---|
| SAPS II | Overall | 32.98 ± 16.38 | 56.04 ± 18.29 | <0.001 |
| Surgical | 30.37 ± 15.33 | 52.68 ± 18.48 | <0.001 | |
| Nonsurgical | 43.01 ± 16.53 | 59.31 ± 17.54 | <0.001 | |
| APACHE II | Overall | 10.44 ± 6.5 | 20.71 ± 8.37 | <0.001 |
| Surgical | 9.3 ± 5.77 | 18.65 ± 8.01 | <0.001 | |
| Nonsurgical | 14.96 ± 7.25 | 22.71 ± 8.24 | <0.001 | |
| SOFA | Overall | 4.86 ± 3.6 | 9 ± 3.62 | <0.001 |
| Surgical | 4.51 ± 3.49 | 8.44 ± 3.53 | <0.001 | |
| Nonsurgical | 6.24 ± 3.76 | 9.55 ± 3.63 | <0.001 | |
| Score | Surgical Patients | Non-surgical Patients | ||
|---|---|---|---|---|
| AUC (95%CI) | ‘p’ | AUC (95%CI) | ‘p’ | |
| SAPS II | 0.826 (0.788–0.863) | <0.001 | 0.742 (0.686–0.799) | <0.001 |
| APACHE II | 0.836 (0.801– 0.872) | <0.001 | 0.748 (0.691–0.804) | <0.001 |
| SOFA | 0.781 (0.743–0.82) | <0.001 | 0.739 (0.679–0.798) | <0.001 |
| Score | ICU Survivors Remaining Alive During Follow-up | ICU Survivors Who Died During Follow-up | ‘p’ | |
|---|---|---|---|---|
| SAPS II | Overall | 29.29 ± 15.6 | 40.9 ± 15,21 | <0.001 |
| Surgical | 28.11 ± 14.83 | 36.71 ± 15.03 | <0.001 | |
| Non-surgical | 36.31 ± 18.19 | 49.48 ± 11.64 | <0.001 | |
| APACHE II | Overall | 9.03 ± 6.1 | 13.55 ± 6.29 | <0.001 |
| Surgical | 8.51 ± 5.66 | 11.52 ± 5.51 | <0.001 | |
| Non-surgical | 12.12 ± 7.58 | 17.7 ± 5.77 | <0.001 | |
| SOFA | Overall | 4.25 ± 3.55 | 6.2 ± 3.39 | <0.001 |
| Surgical | 4.09 ± 3.47 | 5.7 ± 3.3 | <0.001 | |
| Non-surgical | 5.22 ± 3.9 | 7.22 ± 3.39 | 0.002 | |
| Score | Surgical Patients | Non-surgical Patients | ||
|---|---|---|---|---|
| AUC (95%CI) | ‘p’ | AUC (95%CI) | ‘p’ | |
| SAPS II | 0.659 (0.605–0.713) | <0.001 | 0.719 (0.624–0.814) | <0.001 |
| APACHE II | 0.666 (0.614–0.717) | <0.001 | 0.723 (0.63–0.817) | <0.001 |
| SOFA | 0.641 (0.587–0.694) | <0.001 | 0.663 (0.564–0.762) | 0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fuchs, P.A.; Czech, I.J.; Krzych, Ł.J. The Pros and Cons of the Prediction Game: The Never-ending Debate of Mortality in the Intensive Care Unit. Int. J. Environ. Res. Public Health 2019, 16, 3394. https://doi.org/10.3390/ijerph16183394
Fuchs PA, Czech IJ, Krzych ŁJ. The Pros and Cons of the Prediction Game: The Never-ending Debate of Mortality in the Intensive Care Unit. International Journal of Environmental Research and Public Health. 2019; 16(18):3394. https://doi.org/10.3390/ijerph16183394
Chicago/Turabian StyleFuchs, Piotr A., Iwona J. Czech, and Łukasz J. Krzych. 2019. "The Pros and Cons of the Prediction Game: The Never-ending Debate of Mortality in the Intensive Care Unit" International Journal of Environmental Research and Public Health 16, no. 18: 3394. https://doi.org/10.3390/ijerph16183394
APA StyleFuchs, P. A., Czech, I. J., & Krzych, Ł. J. (2019). The Pros and Cons of the Prediction Game: The Never-ending Debate of Mortality in the Intensive Care Unit. International Journal of Environmental Research and Public Health, 16(18), 3394. https://doi.org/10.3390/ijerph16183394






