Does Health Insurance Modify the Association Between Race and Cancer-Specific Survival in Patients with Urinary Bladder Malignancy in the U.S.?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Participants
2.3. Main Variables
2.4. Statistical Methods
2.5. Ethical Considerations
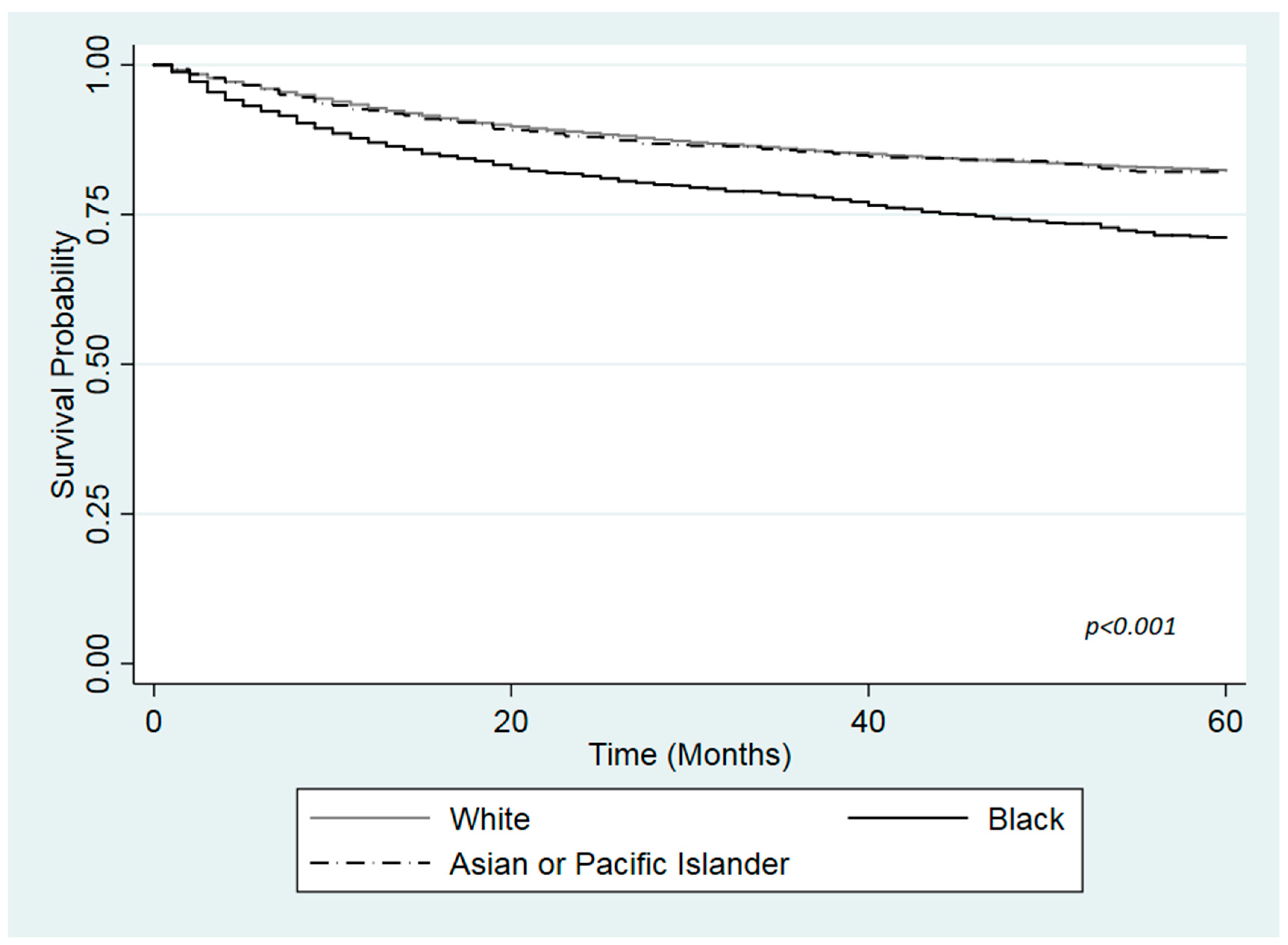
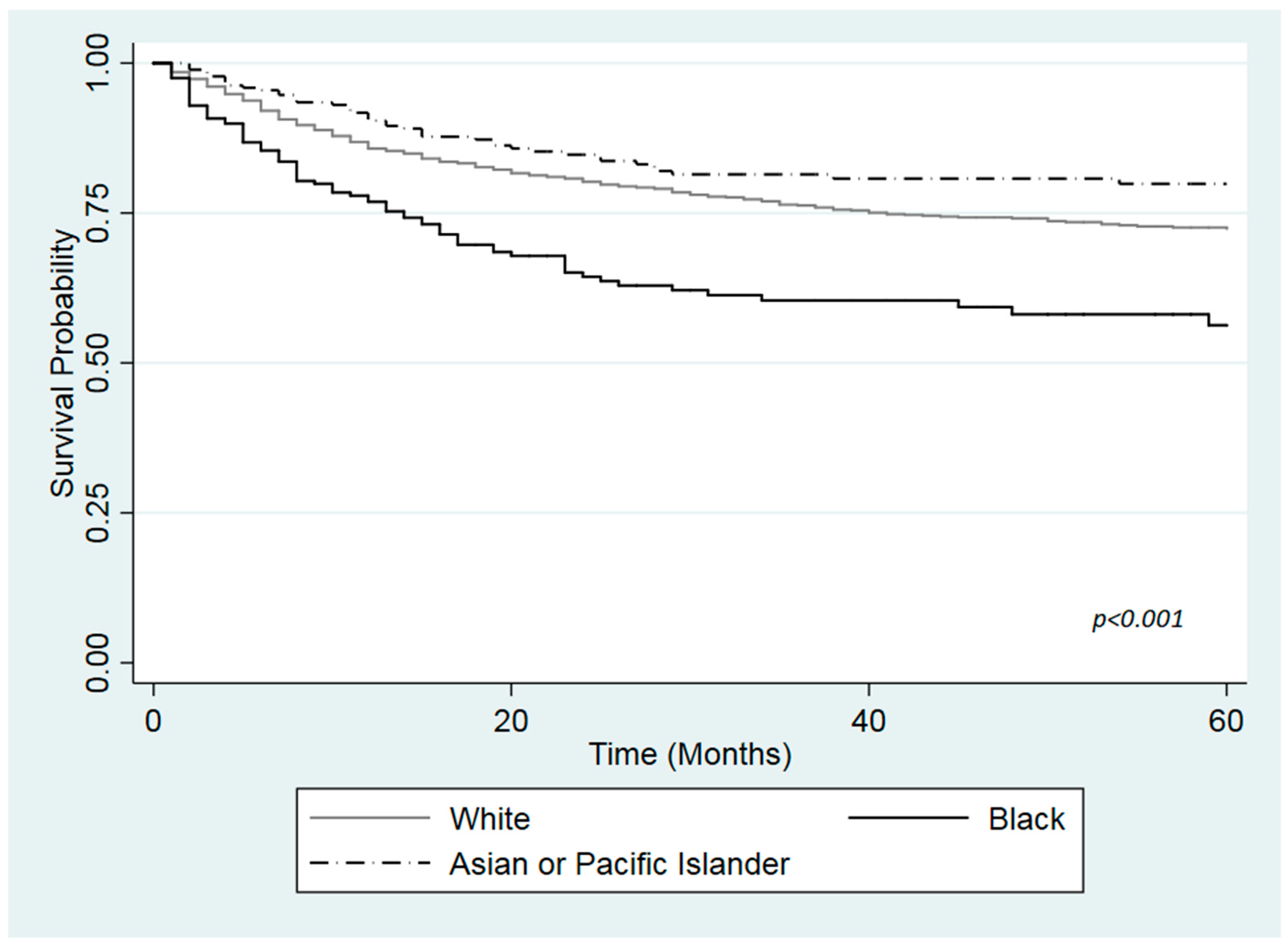
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2017. CA Cancer J. Clin. 2017, 67, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Weiner, A.B.; Keeter, M.; Manjunath, A.; Meeks, J.J. Discrepancies in staging, treatment, and delays to treatment may explain disparities in bladder cancer outcomes: An update from the national cancer data base (2004–2013). Urol. Oncol. 2018, 36, 237.e9–237.e17. [Google Scholar] [CrossRef] [PubMed]
- Yee, D.; Ishill, N.M.; Lowrance, W.T.; Herr, H.W.; Elkin, E. Ethnic differences in bladder cancer survival. Urology 2011, 78, 544–549. [Google Scholar] [CrossRef] [PubMed]
- Gild, P.; Wankowicz, S.A.; Sood, A.; von Landenberg, N.; Friedlander, D.F.; Alanee, S.; Chun, F.K.H.; Fisch, M.; Menon, M.; Trinh, Q.D.; et al. Racial disparity in quality of care and overall survival among black vs. white patients with muscle-invasive bladder cancer treated with radical cystectomy: A national cancer database analysis. Urol. Oncol. 2018, 36, 469.e1–469.e11. [Google Scholar] [CrossRef] [PubMed]
- Brookfield, K.F.; Cheung, M.C.; Gomez, C.; Yang, R.; Nieder, A.M.; Lee, D.J.; Koniaris, L.G. Survival disparities among African American women with invasive bladder cancer in Florida. Cancer 2009, 115, 4196–4209. [Google Scholar] [CrossRef] [PubMed]
- Mallin, K.; David, K.A.; Carroll, P.R.; Milowsky, M.I.; Nanus, D.M. Transitional cell carcinoma of the bladder: Racial and gender disparities in survival (1993 to 2002), stage and grade (1993 to 2007). J. Urol. 2011, 185, 1631–1636. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Chang, Q.; Li, Y. Racial differences in urinary bladder cancer in the United States. Sci. Rep. 2018, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Scosyrev, E.; Noyes, K.; Feng, C.; Messing, E. Sex and racial differences in bladder cancer presentation and mortality in the US. Cancer 2009, 115, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Prout, G.R.; Wesley, M.N.; McCarron, P.G.; Chen, V.W.; Greenberg, R.S.; Mayberry, R.M.; Edwards, B.K. Survival experience of black patients and white patients with bladder carcinoma. Cancer 2004, 100, 621–630. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, B.L.; Montgomery, J.S.; Zhang, Y.; Skolarus, T.A.; Weizer, A.Z.; Hollenbeck, B.K. Disparities in bladder cancer. Urol. Oncol. 2012, 30, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Fleshner, N.E.; Herr, H.W.; Stewart, A.K.; Murphy, G.P.; Mettlin, C.; Menck, H.R. The national cancer data base report on bladder carcinoma. The american college of surgeons commission on cancer and the American cancer society. Cancer 1996, 78, 1505–1513. [Google Scholar] [CrossRef]
- Niu, X.; Roche, L.M.; Pawlish, K.S.; Henry, K.A. Cancer survival disparities by health insurance status. Cancer Med. 2013, 2, 403–441. [Google Scholar] [CrossRef] [PubMed]
- Halpern, M.; Ward, E.; Pavluck, A.; Schrag, N.; Bian, J.; Chen, A. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: A retrospective analysis. Lancet Oncol. 2008, 9, 222–231. [Google Scholar] [CrossRef]
- Kaye, D.R.; Canner, J.K.; Kates, M.; Schoenberg, M.P.; Bivalacqua, T.J. Do African American patients treated with radical cystectomy for bladder cancer have worse overall survival? Accounting for pathologic staging and patient demographics beyond race makes a difference. Bladder Cancer 2016, 2, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Niu, Q.; Lu, Y.; Wu, Y.; Xu, S.; Shi, Q.; Huang, T.; Zhou, G.; Gu, X.; Yu, J. The effect of marital status on the survival of patients with bladder urothelial carcinoma: A SEER database analysis. Medicine 2018, 97, e11378. [Google Scholar] [CrossRef] [PubMed]
- U.S. Census Bureau. Health Insurance Coverage Status and Type of Coverage by Selected Characteristics: 2017. Available online: https://www.census.gov/data/tables/time-series/demo/income-poverty/cps-hi/hi-01.html (accessed on 12 September 2019).
- National Cancer Institute. Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) Research Data (1973–2015); National Cancer Institute: Bethesda, MD, USA, 2018.
- StataCorp LP. Stata Statistical Software: Release 14; StataCorp LP: College Station, TX, USA, 2015. [Google Scholar]
- Hollenbeck, B.K.; Dunn, R.L.; Ye, Z.; Hollingsworth, J.M.; Lee, C.T.; Birkmeyer, J.D. Racial differences in treatment and outcomes among patients with early stage bladder cancer. Cancer 2010, 116, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Barocas, D.A.; Alvarez, J.; Koyama, T.; Anderson, C.B.; Gray, D.T.; Fowke, J.H.; You, C.; Chang, S.S.; Cookson, M.S.; Smith, J.A., Jr.; et al. Racial variation in the quality of surgical care for bladder cancer. Cancer 2014, 120, 1018–1025. [Google Scholar] [CrossRef] [PubMed]
- Mayer, W.J.; McWhorter, W.P. Black/white differences in non-treatment of bladder cancer patients and implications for survival. Am. J. Public Health 1989, 79, 772–775. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Hu, L.; Chen, Y.; Hou, J. The prognostic value of histological subtype in patients with metastatic bladder cancer. Oncotarget 2017, 8, 28408–28417. [Google Scholar] [CrossRef] [PubMed]
- Seo, M.; Langabeer, J.R., II. Demographic and Survivorship Disparities in Non-muscle-invasive Bladder Cancer in the United States. J. Prev. Med. Public Health 2018, 51, 242–247. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Race | p-Value 2 | ||
|---|---|---|---|---|
| White (N = 33,876) | Black (N = 2005) | API 1 (N = 1990) | ||
| % | % | % | ||
| Age (years) | <0.001 | |||
| <50 | 4.78 | 7.73 | 4.37 | |
| 50–59 | 14.3 | 20.85 | 13.57 | |
| 60–69 | 27.95 | 31.22 | 26.18 | |
| 70–79 | 28.75 | 22.54 | 28.19 | |
| 80–89 | 20.51 | 14.71 | 22.76 | |
| 90+ | 3.21 | 2.94 | 4.92 | |
| Gender | <0.001 | |||
| Male | 77.31 | 67.28 | 74.87 | |
| Female | 22.69 | 32.72 | 25.13 | |
| Ethnicity | <0.001 | |||
| Non-Hispanic | 96.57 | 99.2 | 98.49 | |
| Hispanic | 4.43 | 0.8 | 1.51 | |
| Marital status | <0.001 | |||
| Partnered | 64.93 | 41.31 | 68.78 | |
| Unpartnered | 35.05 | 56.69 | 31.22 | |
| Insurance status | <0.001 | |||
| Uninsured | 1.47 | 3.68 | 1.58 | |
| Any Medicaid | 5.52 | 13.02 | 15.05 | |
| Insurance | 93.02 | 83.3 | 83.37 | |
| Stage | <0.001 | |||
| Localized | 79.78 | 70.82 | 77.82 | |
| Regional | 16.92 | 22.15 | 18.7 | |
| Distant | 3.3 | 7.03 | 3.47 | |
| Grade | <0.001 | |||
| Grade I/II | 32.98 | 24.44 | 33.07 | |
| Grade III | 13.24 | 15.62 | 11.61 | |
| Grade IV | 34.06 | 38.65 | 41.46 | |
| Not Graded | 19.72 | 21.75 | 13.87 | |
| Surgery | <0.001 | |||
| Surgery | 94.52 | 91.05 | 95.09 | |
| No Surgery | 5.48 | 0.95 | 4.91 | |
| Characteristics | Adjusted Estimates | |||||
|---|---|---|---|---|---|---|
| Uninsured | Medicaid | Insured | ||||
| (n = 571) | Wald Test p-Values | (n = 2304) | Wald Test p-Values | (n = 32,988) | Wald Test p-Values | |
| HR a (95% CI b) | HR (95% CI) | HR (95% CI) | ||||
| Race | 0.471 | 0.013 | <0.001 | |||
| White | Ref. c | Ref. | Ref. | |||
| Black | 1.19 (0.58–2.42) | 1.24 (0.95–1.61) | 1.46 (1.30–1.64) | |||
| API d | 0.44 (0.10–1.89) | 0.67 (0.48–0.94) | 0.99 (0.86–1.14) | |||
| Age (years) | 0.002 | <0.001 | <0.001 | |||
| <50 | Ref. | Ref. | Ref. | |||
| 50–59 | 1.23 (0.56–2.70) | 1.24 (0.83–1.85) | 1.22 (0.97–1.55) | |||
| 60–69 | 1.19 (0.54–2.62) | 1.18 (0.80–1.75) | 1.50 (1.20–1.87) | |||
| 70–79 | 1.42 (0.45–4.49) | 1.48 (0.98–2.22) | 2.03 (1.63–2.53) | |||
| 80–89 | 2.06 (0.59–7.22) | 2.29 (1.50–3.49) | 3.52 (2.83–4.38) | |||
| 90+ | 17.40 (4.28–70.65) | 2.61 (1.29–5.29) | 6.52 (5.13–8.27) | |||
| Gender | 0.888 | 0.176 | 0.058 | |||
| Male | Ref. | Ref. | Ref. | |||
| Female | 1.04 (0.59–1.83) | 1.16 (0.94–1.44) | 1.07 (1.00–1.15) | |||
| Ethnicity | 0.936 | 0.027 | 0.025 | |||
| Non-Hispanic | Ref. | Ref. | Ref. | |||
| Hispanic | 1.03 (0.42–2.53) | 0.68 (0.49–0.96) | 1.21 (1.02–1.43) | |||
| Marital Status | 0.966 | 0.121 | <0.001 | |||
| Partnered | Ref. | Ref. | Ref. | |||
| Unpartnered | 0.99 (0.62-1.59) | 1.19 (0.96–1.48) | 1.29 (1.21–1.38) | |||
| Stage | <0.001 | <0.001 | <0.001 | |||
| Localized | Ref. | Ref. | Ref. | |||
| Regional | 5.08 (2.73–9.44) | 5.05 (3.89–6.55) | 6.57 (6.08–7.09) | |||
| Distant | 18.54 (9.02–38.11) | 18.24 (13.54–24.55) | 26.75 (24.20–29.56) | |||
| Grade | 0.001 | <0.001 | <0.001 | |||
| Grade I/II | Ref. | Ref. | Ref. | |||
| Grade III | 10.57 (2.92–38.28) | 4.31 (2.68–6.94) | 3.14 (2.74–3.59) | |||
| Grade IV | 6.90 (1.97–24.15) | 3.73 (2.37–5.86) | 3.01 (2.65–3.42) | |||
| Not Graded | 2.83 (0.73–10.90) | 2.24 (1.34–3.66) | 1.90 (1.64–2.20) | |||
| Surgery | 0.013 | <0.001 | <0.001 | |||
| Surgery | Ref. | Ref. | Ref. | |||
| No Surgery | 3.08 (1.27–7.47) | 2.02 (1.44–2.83) | 1.90 (1.67–2.17) | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morales, J.; Malles, A.; Kimble, M.; Rodriguez de la Vega, P.; Castro, G.; Nieder, A.M.; Barengo, N.C. Does Health Insurance Modify the Association Between Race and Cancer-Specific Survival in Patients with Urinary Bladder Malignancy in the U.S.? Int. J. Environ. Res. Public Health 2019, 16, 3393. https://doi.org/10.3390/ijerph16183393
Morales J, Malles A, Kimble M, Rodriguez de la Vega P, Castro G, Nieder AM, Barengo NC. Does Health Insurance Modify the Association Between Race and Cancer-Specific Survival in Patients with Urinary Bladder Malignancy in the U.S.? International Journal of Environmental Research and Public Health. 2019; 16(18):3393. https://doi.org/10.3390/ijerph16183393
Chicago/Turabian StyleMorales, Juliana, Aaron Malles, Marrell Kimble, Pura Rodriguez de la Vega, Grettel Castro, Alan M. Nieder, and Noël C. Barengo. 2019. "Does Health Insurance Modify the Association Between Race and Cancer-Specific Survival in Patients with Urinary Bladder Malignancy in the U.S.?" International Journal of Environmental Research and Public Health 16, no. 18: 3393. https://doi.org/10.3390/ijerph16183393
APA StyleMorales, J., Malles, A., Kimble, M., Rodriguez de la Vega, P., Castro, G., Nieder, A. M., & Barengo, N. C. (2019). Does Health Insurance Modify the Association Between Race and Cancer-Specific Survival in Patients with Urinary Bladder Malignancy in the U.S.? International Journal of Environmental Research and Public Health, 16(18), 3393. https://doi.org/10.3390/ijerph16183393






