Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China
Abstract
1. Introduction
2. Revisiting Health Disparity and Institutions of Healthcare Resources Distribution
2.1. Health Disparity and the Uneven Distribution of Healthcare Resources
2.2. China’s Healthcare Institutions: From Central Planning to Radical Marketization
3. Data and Methodology
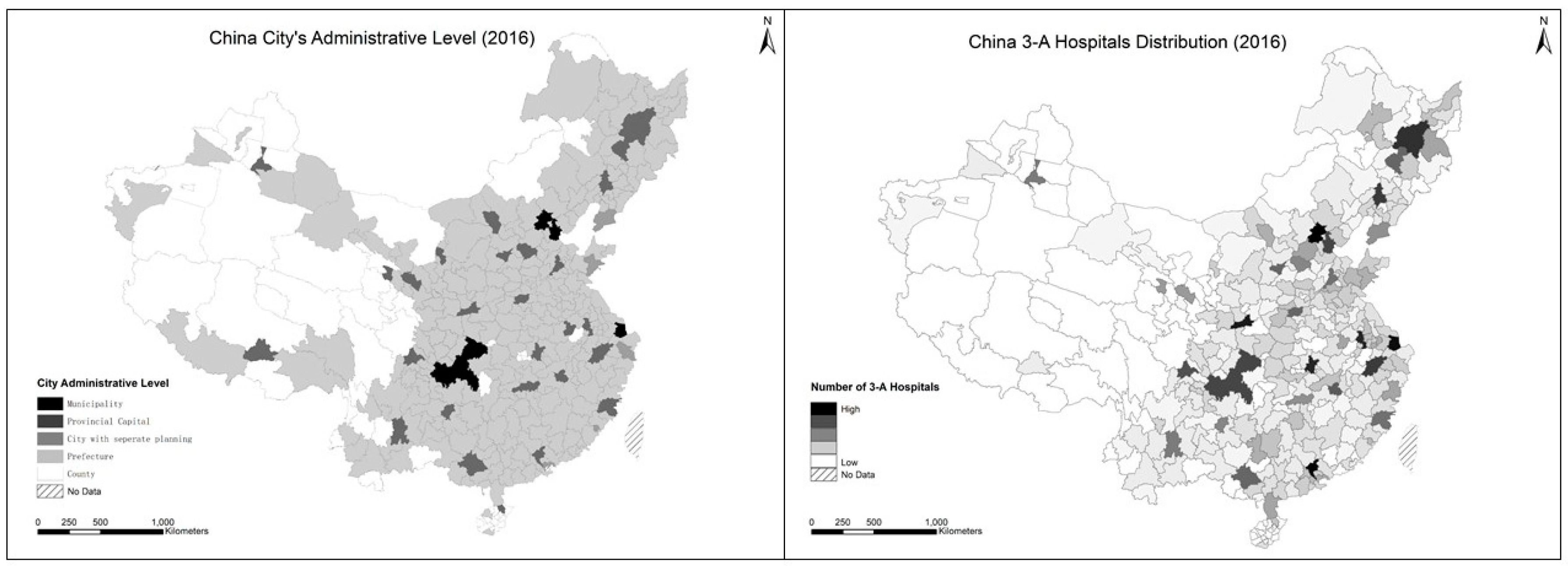
3.1. Developing an Integrated Database of High-Quality Hospitals
3.2. Modeling a Comprehensive Evaluation Framework
3.3. Measuring Uneven Distribution of High-Quality Healthcare Resources
3.3.1. Inequality Measurement Methods
3.3.2. Inequality Decomposition by Subgroups
4. Empirical Results and Major Findings
4.1. Determinants of 3-A Hospitals’ Performance
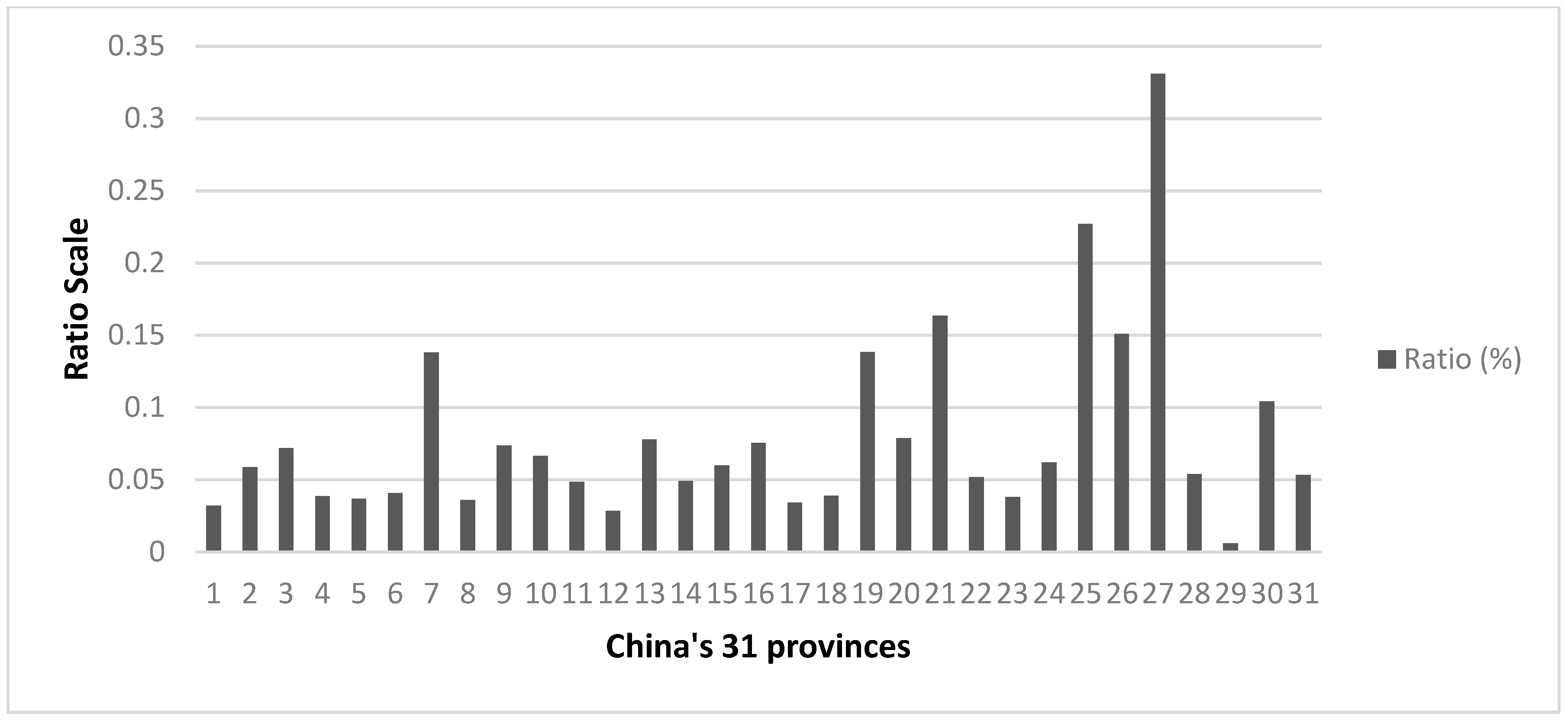
4.2. 3-A Hospitals Scores Distribution and GE() Values at Multiple Scales
4.3. Interpreting the Unevenness at Different Scales
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Chang, J. Chinese Spur Medical-Tourism Growth in the US. China Daily USA. 2015. Available online: http://usa.chinadaily.com.cn/epaper/2015-08/07/content_21527300.htm (accessed on 20 April 2019).
- Liu, Y.; Rao, K.; Wu, J.; Gakidou, E. China’s health system performance. Lancet 2008, 372, 1914–1923. [Google Scholar] [CrossRef]
- Tang, S.; Meng, Q.; Chen, L.; Bekedam, H.; Evans, T.; Whitehead, M. Tackling the challenges to health equity in China. Lancet 2008, 372, 1493–1501. [Google Scholar] [CrossRef]
- Zhang, X.; Kanbur, R. Spatial inequality in education and health care in China. China Econ. Rev. 2005, 16, 189–204. [Google Scholar] [CrossRef]
- State Council, Central Committee of CPC. Outline of the Plan for “Healthy China 2030”. 2016. Available online: https://china.lexiscn.com/law/law-english-1-2961294-T.html (accessed on 15 April 2019).
- State Council of China. China to Continue Improving Fairness, Accessibility of Health Service: Minister. Official Website of the State Council of China; 2017. Available online: http://english.gov.cn/state_council/ministries/2017/05/23/content_281475664671834.htm (accessed on 11 July 2019).
- Liu, M.; Zhang, Q.; Lu, M.; Kwon, C.; Quan, H. Rural and urban disparity in health services utilization in China. Med Care 2007, 45, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Braveman, P.; Gottlieb, L. The social determinants of health: Its time to consider the causes of the causes. Public Health Rep. 2014, 129 (Suppl. 2), 19–31. [Google Scholar] [CrossRef]
- Rich, R.F.; Elkins, C.L. Health disparities. In Encyclopedia of Health Services Research; Mullner, R., Ed.; Sage: Los Angeles, CA, USA, 2009; Available online: http://sk.sagepub.com.eproxy.lib.hku.hk/reference/healthservices/n174.xml (accessed on 10 July 2019).
- Braveman, P. What are health disparities and health equity? We need to be clear. Public Health Rep. 2014, 129 (Suppl. 2), 5–8. [Google Scholar] [CrossRef]
- Eriksson, T.; Pan, J.; Qin, X. The intergenerational inequality of health in China. China Econ. Rev. 2014, 31, 392–409. [Google Scholar] [CrossRef]
- Guo, H. Research on the Equity of Rural and Urban Residents Basic Medical Insurance Scheme: The Case of Chengdu; Southwest University of Finance and Economics Press: Chengdu, China, 2014. (In Chinese) [Google Scholar]
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef]
- U.S. Department of Health & Human Services. Healthy People 2010: Understanding and Improving Health; U.S. Department of Health & Human Services: Washington, DC, USA, 2000; 63p.
- World Health Organ; Commission on Social Determinants of Health. CSDH Final Report: Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- U.S. Department of Health & Human Services. Healthy People 2020 Framework; U.S. Department of Health & Human Services: Washington, DC, USA, 2011. Available online: http://www.healthypeople.gov/2020/Co (accessed on 9 July 2019).
- U.S. Department of Health & Human Services. Healthy People 2000: National Health Promotion and Disease Prevention Objectives; U.S. Department of Health & Human Services: Washington, DC, USA, 1991.
- U.K. Department of Health and Social Care. Tackling Health Inequalities: A Programme for Action; U.K. Department of Health and Social Care: London, UK, 2003.
- Bleich, S.N.; Jarlenski, M.P.; Bell, C.N.; Laveist, T.A. Health inequalities: Trends, progress, and policy. Annu. Rev. Public Health 2012, 33, 7–40. [Google Scholar] [CrossRef]
- Doorslaer, E.V. Inequalities in access to medical care by income in developed countries. Can. Med Assoc. J. 2006, 174, 177–183. [Google Scholar] [CrossRef]
- Yip, W.; Hsiao, W. Chinas health care reform: A tentative assessment. China Econ. Rev. 2009, 20, 613–619. [Google Scholar] [CrossRef]
- La Foucade, A.; Scott, E. Equity in health. In The SAGE Encyclopedia of World Poverty; Odekon, M., Ed.; SAGE: Thousand Oaks, CA, USA, 2015; Available online: http://sk.sagepub.com.eproxy.lib.hku.hk/reference/healthservices/n174.xml (accessed on 11 July 2019).
- Evandrou, M.; Falkingham, J.; Feng, Z.; Vlachantoni, A. Individual and province inequalities in health among older people in China: Evidence and policy implications. Health Place 2014, 30, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Miao, J.; Wu, X. Urbanization, socioeconomic status and health disparity in China. Health Place 2016, 42, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A. Spatial analysis of disparities in LDL-C testing for older diabetic adults: A socio-environmental framework focusing on race, poverty, and health access in Mississippi. Appl. Geogr. 2014, 55, 248–256. [Google Scholar] [CrossRef]
- Wang, L. Unequal spatial accessibility of integration-promoting resources and immigrant health: A mixed-methods approach. Appl. Geogr. 2018, 92, 140–149. [Google Scholar] [CrossRef]
- Zhang, W.; Wu, Y. Individual educational attainment, neighborhood-socioeconomic contexts, and self-rated health of middle-aged and elderly Chinese: Exploring the mediating role of social engagement. Health Place 2017, 44, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Gulliford, M.; Morgan, M. Access to Health Care; Routledge: London, UK, 2003. [Google Scholar]
- Jacobs, B.; Ir, P.; Bigdeli, M.; Annear, P.L.; Van Damme, W. Addressing access barriers to health services: An analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan. 2012, 27, 288–300. [Google Scholar] [CrossRef] [PubMed]
- McGrail, M.R.; Humphreys, J.S. Measuring spatial accessibility to primary health care services: Utilising dynamic catchment sizes. Appl. Geogr. 2014, 54, 182–188. [Google Scholar] [CrossRef]
- Yin, C.; He, Q.; Liu, Y.; Chen, W.; Gao, Y. Inequality of public health and its role in spatial accessibility to medical facilities in China. Appl. Geogr. 2018, 92, 50–62. [Google Scholar] [CrossRef]
- Pei, X.; Rodriguez, E. Provincial income inequality and self-reported health status in China during 1991–1997. J. Epidemiol. Community Health 2006, 60, 1065–1069. [Google Scholar] [CrossRef]
- Yip, W.C.; Hsiao, W.C.; Chen, W.; Hu, S.; Ma, J.; Maynard, A. Early appraisal of Chinas huge and complex health-care reforms. Lancet 2012, 379, 833–842. [Google Scholar] [CrossRef]
- Ding, M.; Zhang, X.; Liu, G. Research on the Reform of Social Governance of China, 1st ed.; China Economic Publishing House: Beijing, China, 2009; pp. 52–54. (In Chinese) [Google Scholar]
- Mertha, A.C. Chinas “Soft” centralization: Shifting Tiao/Kuai authority relations. China Q. 2005, 184, 791–810. Available online: https://www.cambridge.org/core/journals/china-quarterly/article/chinas-soft-centralization-shifting-tiaokuai-authority-relations/70295A675B87106E598FB0F9864A75EC (accessed on 19 July 2019). [CrossRef]
- Nundy, M. Transformation of health insurance schemes in China: Lessons for access. China Rep. 2014, 50, 31–43. [Google Scholar] [CrossRef]
- Jin, J.; Wang, J.; Ma, X.; Wang, Y.; Li, R. Equality of medical health resource allocation in China based on the Gini coefficient method. Iran. J. Public Health 2015, 44, 445–457. [Google Scholar] [PubMed]
- Sun, J.; Luo, H. Evaluation on equality and efficiency of health resources allocation and health services utilization in China. Int. J. Equity Health 2017, 16, 127. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Xu, Y.; Ren, J.; Sun, L.; Liu, C. Inequality in the distribution of health resources and health services in China: Hospitals versus primary care institutions. Int. J. Equity Health 2017, 16, 42. [Google Scholar] [CrossRef] [PubMed]
- Cowell, F.A. Estimation of inequality indices. In Handbook of Income Inequality Measurement; Springer: Dordrecht, The Netherlands, 1999; pp. 123–143. [Google Scholar]
- Cowell, F.A.; Kuga, K. Additivity and the entropy concept: An axiomatic approach to inequality measurement. J. Econ. Theory 1981, 25, 131–143. Available online: https://www.sciencedirect.com/science/article/pii/002205318190020X (accessed on 27 July 2004). [CrossRef]
- Toyoda, T. Inequalities of income distributions: Their comparisons and inequality measures. Kokumin Keizai 1975, 134, 15–41. [Google Scholar]
- Jansen, P.W.; Mensah, F.K.; Nicholson, J.M.; Wake, M. Family and neighbourhood socioeconomic inequalities in childhood trajectories of BMI and overweight: Longitudinal study of Australian children. PLoS ONE 2013, 8, e69676. [Google Scholar] [CrossRef]
- Jenkins, S.P. Estimation and Interpretation of Measures of Inequality, Poverty, and Social Welfare Using Stata. North American Stata Users’ Group Meetings 2006. 2008. Available online: https://ideas.repec.org/p/boc/asug06/16.html (accessed on 10 July 2019).
- World Bank Poverty Manual—pofunmare.files.wordpress.com. Available online: https://pofunmare.files.wordpress.com/2015/08/world-bank-poverty-manual.pdf (accessed on 11 July 2019).
- Biewen, M.; Jenkins, S.P. Variance estimation for generalized entropy and Atkinson inequality indices: The complex survey data case*. Oxf. Bull. Econ. Stat. 2006, 68, 371–383. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1468-0084.2006.00166.x (accessed on 10 July 2019). [CrossRef]
- Ma, J.; Lu, M.; Quan, H. From a national, centrally planned health system to a system based on the market: Lessons from China. Health Aff. 2008, 27, 937–948. [Google Scholar] [CrossRef] [PubMed]
- Haughton, H.; Khandker, S. Handbook on Poverty and Inequality; The World Bank: Washington, DC, USA, 2009; ISBN 9780821376133. Available online: http://siteresources.worldbank.org/INTPA/Resources/429966-1259774805724/Poverty_Inequality_Handbook_FrontMatter.pdf (accessed on 11 July 2019).
- Zhu, J.S. Breaking down the institutional barriers for the allocation of medical resources guided by medical insurance. China Health Insur. 2017, 12, 12–15. Available online: http://www.cqyuzhong.com/UploadFile/news/20172915113140738.pdf (accessed on 9 July 2019). (In Chinese).
- Xue, D. Defect and improvement of the administration management in health care system: From the perspective of medical resource allocation efficiency and equity. Chin. Hosp. Manag. 2013, 33, 1–3. (In Chinese) [Google Scholar]
- Kanbur, R. Chapter 13 Income distribution and development. In Handbook of Income Distribution; Elsevier: Amsterdam, The Netherlands, 2000; pp. 791–841. [Google Scholar]
- Wang, X.; Wei, W.; Ma, C.; Zhou, D.; Wang, S.; Feng, Z. Reasons and destination features of medical personnel flow in township hospitals in Hubei province. Chin. J. Public Health 2014, 30, 1312–1314. Available online: http://html.rhhz.net/ZGGGWS/html/20141025.htm (accessed on 11 July 2019). (In Chinese).
- Wu, S.; Liu, X.; Jiang, X.; Huang, Q.; Yuan, Z. Turnover of healthcare technical personnel in township health centers of Jangxi province. Chin. J. Public Health 2017, 33, 1048–1050. Available online: http://html.rhhz.net/ZGGGWS/html/20170704.htm (accessed on 12 July 2019). (In Chinese).
- Gu, X. The transformation in public finance and the return of government’s responsibility for healthcare financing. Soc. Sci. China 2010, 2010, 103–120. Available online: http://kns.cnki.net.eproxy.lib.hku.hk//KXReader/Detail?TIMESTAMP=636983844539036250&DBCODE=CJFD&TABLEName=CJFD2010&FileName=ZSHK201002008&RESULT=1&SIGN=tc%2f3JUXxGx69%2blzA7b1AUvGpsEo%3d (accessed on 10 July 2019). (In Chinese).
- Du, C.; Zhu, H.P. The evolutionary logic in urban China’s healthcare and medical system. Soc. Sci. China 2016, 2016, 66–89. Available online: http://big5.oversea.cnki.net.eproxy.lib.hku.hk/kcms/detail/detail.aspx?dbCode=cjfd&QueryID=37&CurRec=4&filename=ZSHK201608004&dbname=CJFDLAST2016&uid=WEEvREcwSlJHSldRa1Fhb09jT0pjQnpiNUFtQmhqUmRVTkNNcDR2eVkrdz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4IQMovwHtwkF4VYPoHbKxJw!! (accessed on 10 July 2019). (In Chinese).
- Yu, Y.X.; Yang, D.K. Theoretical and empirical research on equity of healthcare resource allocation in China. Reform Econ. Syst. 2008, 2008, 160–163. Available online: http://www.cqvip.com/qk/91904x/200806/29122406.html (accessed on 12 June 2019). (In Chinese).
- Wu, S.; Fu, Y.; Shen, H.; Liu, F. Using ranked weights and Shannon entropy to modify regional sustainable society index. Sustain. Cities Soc. 2018, 41, 443–448. Available online: https://www.sciencedirect.com/science/article/pii/S2210670717312441 (accessed on 23 May 2019). [CrossRef]

| Variable Details in Equation (1) | Category | Data Source |
|---|---|---|
| y: 379 Ailibi 3A hospital score | Ailibi-2016-ranking | |
| var1: No. of total staff (person) | Hospitals’ official websites. For missing information and data, we visit other websites such as www.haodf.com and https://www.jobmd.cn/ | |
| var2: city2016 permanent population (unit: 10,000 person) | China City Statistical Yearbook 2017 | |
| var3: city 2016 disposable income (yuan) | ||
| var4: ownership |
| Hospitals’ official websites |
| var5: medical treatment style |
| Hospitals’ official websites |
| var6: church & charity initiated |
| Hospitals’ official websites |
| var7: university affiliation |
| Hospitals’ official websites |
| var8: NHFPC direct administration |
| NHFPC website |
| var9: provincial HFPC direct administration |
| Websites of the Health and Family Planning Commission of each province |
| var10: municipality HFPC direct administration |
| http://wjw.beijing.gov.cn/ http://wsjk.tj.gov.cn/html/wsjn/portal/index/index.htm http://wsjkw.sh.gov.cn/index.html http://wsjkw.cq.gov.cn/ |
| var11: prefecture bureau of Health and Family Planning Commission administration |
| Authors’ summary |
| var12: military affiliation |
| https://www.yaofangwang.com/yiyuan/ |
| var13: city administrative level |
| China City Statistical Yearbook 2017 |
| Linear regression Number of obs = 368 F(21, 346) = 29.16 Prob > F = 0.0000 R-squared = 0.5959 Root MSE = 115.83 Robust | |||||
|---|---|---|---|---|---|
| y | Standard Error | t | P > t | (95% Confidence Interval) | |
| var1 | 0.0436 | 0.0080 | 5.50 | 0.000 *** | 0.0280–0.0592 |
| var2 | 0.0356 | 0.0203 | 1.75 | 0.081 * | −0.0044–0.0755 |
| var3 | 0.0042 | 0.0008 | 5.39 | 0.000 *** | 0.0027–0.0058 |
| var4 = 1 | 105.3848 | 32.6609 | 3.23 | 0.001 *** | 41.1459–169.6237 |
| var5 = | |||||
| 2 | −105.664 | 18.3378 | −5.76 | 0.000 *** | −141.7317–−69.5964 |
| 3 | −142.515 | 40.0669 | −3.56 | 0.000 *** | −221.3204–−63.7096 |
| var6 = 1 | 44.8862 | 16.5621 | 2.71 | 0.007 *** | 12.3111–77.4613 |
| var12 = 1 | 171.0338 | 59.9637 | 2.85 | 0.005 *** | 53.0946–288.9731 |
| var9 = 1 | 23.8974 | 32.1457 | 0.74 | 0.458 | −39.3281–87.1230 |
| var10 = 1 | 13.3541 | 38.2681 | 0.35 | 0.727 | −61.9132–88.6215 |
| var8 * var7 | |||||
| 0 1 | −94.1936 | ||||
| 1 0 | 60.0584 | 34.6160 | −2.72 | 0.007 *** | −162.278–−26.1093 |
| 1 1 | 0 (omitted) | 38.9043 | 1.54 | 0.124 | −16.4603–136.577 |
| var11 * var7 | |||||
| 0 1 | −67.3168 | ||||
| 1 0 | 159.3906 | 32.0474 | −2.10 | 0.036 * | −130.3491–−4.2845 |
| 1 1 | 0 (omitted) | 39.2444 | 4.06 | 0.000 *** | 82.2029–236.5783 |
| var13 * var7 | |||||
| 1 1 | 257.8345 | 64.8942 | 3.97 | 0.000 *** | 130.1978–385.4712 |
| 2 0 | 59.5823 | 59.4744 | 1.00 | 0.317 | −57.3946–176.5593 |
| 2 1 | 283.7637 | 72.0074 | 3.94 | 0.000 *** | 142.1364–425.391 |
| 3 0 | −24.1865 | 66.7344 | −0.36 | 0.717 | −155.4427–107.0697 |
| 3 1 | 300.5646 | 96.5215 | 3.11 | 0.002 *** | 110.7219–490.4072 |
| 4 0 | −25.5099 | 65.3923 | −0.39 | 0.697 | −154.1263–103.1066 |
| 4 1 | 270.0733 | 80.1628 | 3.37 | 0.001 *** | 112.4057–427.741 |
| _cons | 63.0924 | 77.3488 | 0.82 | 0.415 | −89.0406–215.2255 |
| City’s Aggregated 3-A Hospital Score | Average 3-A Hospitals Score Per 10,000 People | |||||
|---|---|---|---|---|---|---|
| Ranking | City Name | City Administrative Level | Province | City Name | City Administrative Level | Province |
| 1 | Beijing | Municipality | Beijing | Xining | Provincial capital | Qinghai |
| 2 | Guangzhou | Provincial capital | Guangdong | Urumqi | Autonomous capital | Xinjiang |
| 3 | Shanghai | Municipality | Shanghai | Nanchang | Provincial capital | Jiangxi |
| 4 | Nanjing | Provincial capital | Jiangsu | Nanjing | Provincial capital | Jiangsu |
| 5 | Wuhan | Provincial capital | Hubei | Taiyuan | Provincial capital | Shanxi |
| 6 | Xi’an | Provincial capital | Shaanxi | Shenyang | Provincial capital | Liaoning |
| 7 | Hangzhou | Provincial capital | Zhejiang | Xi’an | Provincial capital | Shaanxi |
| 8 | Shenyang | Provincial capital | Liaoning | Lhasa | Autonomous capital | Tibet |
| 9 | Chengdu | Provincial capital | Sichuan | Beijing | Municipality | Beijing |
| 10 | Harbin | Provincial capital | Heilongjiang | Guangzhou | Provincial capital | Guangdong |
| Grouping at City Level N = Observation, aw: Analytical Weight | Theil’s L GE(0) | Theil’s T GE(1) |
|---|---|---|
| City (N = 308, aw: city population) | 0.337 | 0.330 |
| Subgroups by city administrative level (N = 308, aw: city population) | Theil’s L GE(0) | Theil’s T GE(1) |
| 2-Provincial capital 3-Sub-provincial leveled city 4-Prefecture | 0.055 0.091 0.184 | 0.052 0.098 0.175 |
| GE_W(α) GE_B(α) | 47.52% 52.47% | 35.93% 64.07% |
| 32 Provinces | GE(0) | GE(1) | 7 Regions | GE(0) | GE(1) | 3 Zones | GE(0) | GE(1) |
|---|---|---|---|---|---|---|---|---|
| Total | 0.34 | 0.32 | Total | 0.34 | 0.32 | Total | 0.34 | 0.32 |
| 1-Heilongjiang | 0.28 | 0.18 | 1-NE | 0.32 | 0.25 | 1-Eastern China | 0.28 | 0.27 |
| 2-Jilin | 0.38 | 0.32 | 2-NC | 0.39 | 0.36 | 2-Central China | 0.37 | 0.35 |
| 3-Liaoning | 0.30 | 0.27 | 3-EC | 0.25 | 0.25 | 3-Western China | 0.37 | 0.38 |
| 4-Beijing | 0 | 0 | 4-CC | 0.38 | 0.38 | |||
| 5-Tianjin | 0 | 0 | 5-SC | 0.26 | 0.26 | |||
| 6-Hebei | 0.18 | 0.15 | 6-SW | 0.28 | 0.28 | |||
| 7-Shanxi | 0.43 | 0.47 | 7-NW | 0.42 | 0.37 | |||
| 8-Inner Mongolia | 0.34 | 0.36 | ||||||
| 9-Shanghai | 0 | 0 | ||||||
| 10-Jiangsu | 0.37 | 0.36 | ||||||
| 11-Zhejiang | 0.19 | 0.21 | ||||||
| 12-Anhui | 0.19 | 0.18 | Note: 1-NE comprises provinces No. 1~3; 2-NC comprises provinces No. 4~8; 3-EC comprises provinces No. 9~14; 4-CC comprises provinces No. 15~18; 5-SC comprises provinces No. 19~21; 6-SW comprises provinces No. 22~26; 7-NW comprises provinces No. 27~32. | Note: 1-Eastern China comprises provinces No. 3, 4, 5, 6, 9, 10, 11, 13, 14, 19, 20 and 21; 2-Central China comprises provinces No. 1, 2, 8, 12, 15, 16, 17 and 18; 3-Western China comprises provinces No. 22, 23, 24, 25, 26, 27, 28, 29, 30, 31 and 32. | ||||
| 13-Fujian | 0.27 | 0.26 | ||||||
| 14-Shandong | 0.18 | 0.18 | ||||||
| 15-Henan | 0.35 | 0.30 | ||||||
| 16-Hubei | 0.34 | 0.32 | ||||||
| 17-Hunan | 0.26 | 0.28 | ||||||
| 18-Jiangxi | 0.52 | 0.57 | ||||||
| 19-Guangdong | 0.24 | 0.26 | ||||||
| 20-Hainan | 0.002 | 0.002 | ||||||
| 21-Guangxi | 0.27 | 0.25 | ||||||
| 22-Chongqing | 0 | 0 | ||||||
| 23-Sichuan | 0.28 | 0.26 | ||||||
| 24-Guizhou | 0.41 | 0.46 | ||||||
| 25-Yunnan | 0.31 | 0.34 | ||||||
| 26-Tibet | 0 | 0 | ||||||
| 27-Shaanxi | 0.43 | 0.39 | ||||||
| 28-Gansu | 0.33 | 0.34 | ||||||
| 29-Qinghai | 0 | 0 | ||||||
| 30-Ningxia | 0 | 0 | ||||||
| 31-Xinjiang | 0.43 | 0.33 | ||||||
| 32-XPCC | 0 | 0 | ||||||
| GE_W() GE_B() | 80.36% 19.64% | 76.13% 23.87% | GE_W() GE_B() | 92.82% 7.18% | 92.52% 7.47% | GE_W() GE_B() | 97.43% 2.56% | 97.35% 2.65% |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, M.; He, S.; Wu, D.; Zhu, H.; Webster, C. Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China. Int. J. Environ. Res. Public Health 2019, 16, 2813. https://doi.org/10.3390/ijerph16162813
Yu M, He S, Wu D, Zhu H, Webster C. Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China. International Journal of Environmental Research and Public Health. 2019; 16(16):2813. https://doi.org/10.3390/ijerph16162813
Chicago/Turabian StyleYu, Meng, Shenjing He, Dunxu Wu, Hengpeng Zhu, and Chris Webster. 2019. "Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China" International Journal of Environmental Research and Public Health 16, no. 16: 2813. https://doi.org/10.3390/ijerph16162813
APA StyleYu, M., He, S., Wu, D., Zhu, H., & Webster, C. (2019). Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China. International Journal of Environmental Research and Public Health, 16(16), 2813. https://doi.org/10.3390/ijerph16162813






