Feasibility Trial of an eHealth Intervention for Health-Related Quality of Life: Implications for Managing Patients with Chronic Pain During the COVID-19 Pandemic
Abstract
1. Introduction
2. Methods
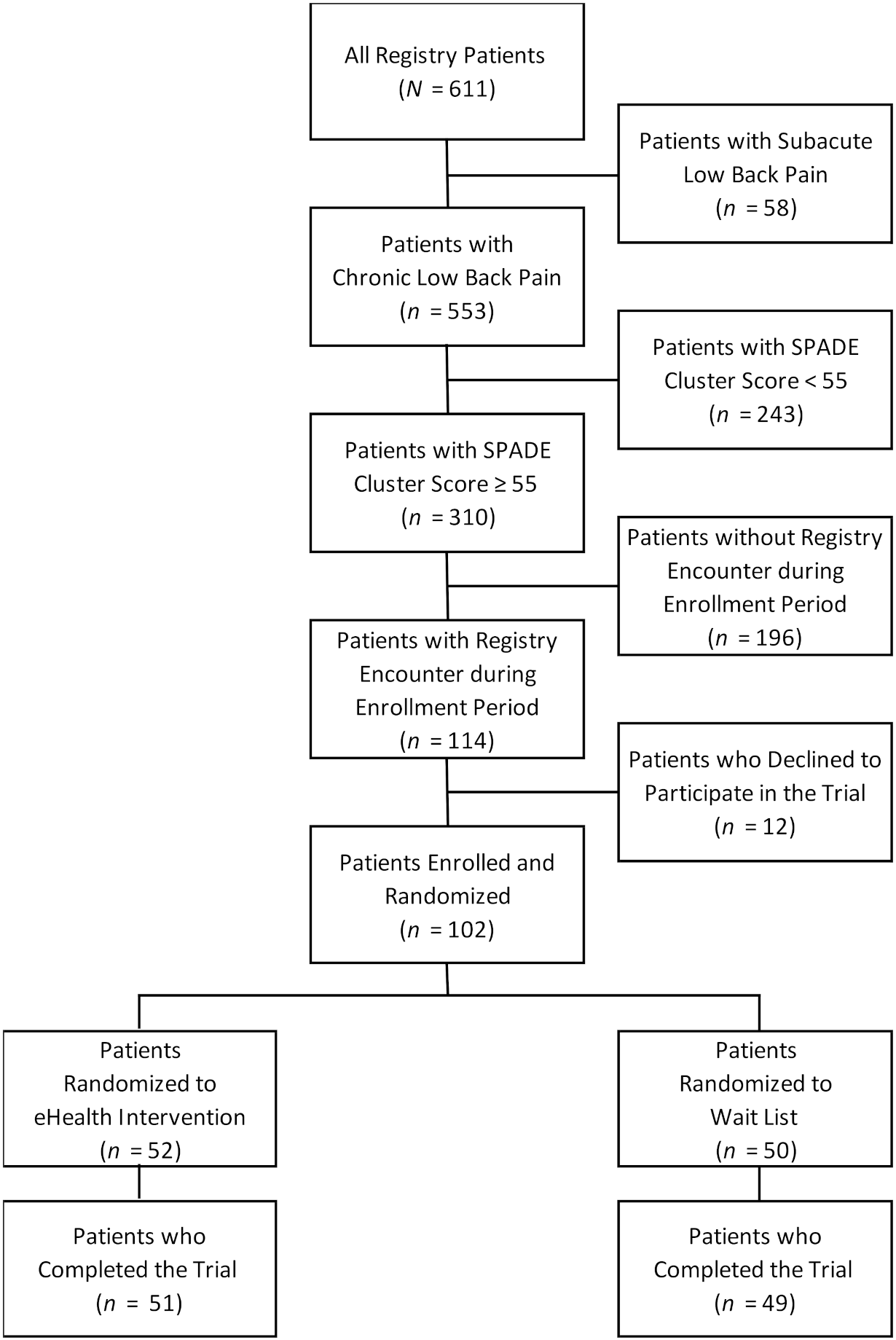
2.1. Registry Overview and Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Experimental and Control Treatments
2.4. Survey of the Value and Utility of the eHealth Intervention
2.5. Outcome Measures
2.6. Sample Size
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- The White House. Proclamation on Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak. Available online: https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/#:~:text=Proclamation%20on%20Declaring%20a%20National%20Emergency%20Concerning%20the,Disease%20(COVID%2D19)%20Outb (accessed on 10 August 2020).
- Dahlhamer, J.M.; Lucas, J.; Zelaya, C.; Nahin, R.; Mackey, S.; DeBar, L.; Kerns, R.; Von Korff, M.; Porter, L.; Helmick, C. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults—United States, 2016. Morb. Mortal. Wkly. Rep. 2018, 67, 1001–1006. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, C.; Blyth, F.M.; Dear, B.F.; Fisher, E.A.; Keefe, F.J.; Lynch, M.E.; Palermo, T.M.; Reid, M.C.; Williams, A.C.D.C. Managing patients with chronic pain during the COVID-19 outbreak. Pain 2020, 161, 889–893. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. eHealth. Available online: http://www.emro.who.int/health-topics/ehealth/ (accessed on 10 August 2020).
- Gatchel, R.J.; Reuben, D.B.; Dagenais, S.; Turk, D.C.; Chou, R.; Hershey, A.D.; Hicks, G.E.; Licciardone, J.C.; Horn, S.D. Research Agenda for the Prevention of Pain and Its Impact: Report of the Work Group on the Prevention of Acute and Chronic Pain of the Federal Pain Research Strategy. J. Pain 2018, 19, 837–851. [Google Scholar] [CrossRef] [PubMed]
- Interagency Pain Research Coordinating Committee Members Announced. J. Investig. Med. 2012, 60, 761–765. [CrossRef]
- Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research; The National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Interagency Pain Research Coordinating Committee. National Pain Strategy: A Comprehensive Population Health-Level Strategy for Pain. US Department of Health and Human Services, National Institutes of Health. Available online: https://www.iprcc.nih.gov/sites/default/files/HHSNational_Pain_Strategy_508C.pdf (accessed on 10 August 2020).
- Northwestern University. PROMIS Adult Profile Instruments. Available online: https://www.healthmeasures.net/explore-measurement-systems/promis (accessed on 29 September 2020).
- Deyo, R.A.; Dworkin, S.F.; Amtmann, D.; Andersson, G.; Borenstein, D.; Carragee, E.; Carrino, J.; Chou, R.; Cook, K.; Delitto, A.; et al. Report of the NIH Task Force on Research Standards for Chronic Low Back Pain. Phys. Ther. 2015, 95, e1–e18. [Google Scholar] [CrossRef]
- Davis, L.L.; Kroenke, K.; Monahan, P.; Kean, J.; Stump, T.E. The SPADE Symptom Cluster in Primary Care Patients With Chronic Pain. Clin. J. Pain 2016, 32, 388–393. [Google Scholar] [CrossRef]
- Gliklich, R.E.; Dreyer, N.A. Registries for Evaluating Patient Outcomes: A User’s Guide, 2nd ed.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2020. Available online: https://effectivehealthcare.ahrq.gov/products/registries-guide-2nd-edition/research/ (accessed on 29 September 2020).
- Licciardone, J.C.; Gatchel, R.J.; Phillips, N.; Aryal, S. The Pain Registry for Epidemiological, Clinical, and Interventional Studies and Innovation (PRECISION): Registry overview and protocol for a propensity score-matched study of opioid prescribing in patients with low back pain. J. Pain Res. 2018, 11, 1751–1760. [Google Scholar] [CrossRef]
- Roland, M.; Morris, R. A Study of the Natural History of Back Pain. Spine 1983, 8, 141–144. [Google Scholar] [CrossRef]
- Dean, A.G.; Sullivan, K.M.; Soe, M.M. OpenEpi: Open Source Epidemiologic Statistics for Public Health. Available online: www.OpenEpi.com (accessed on 10 August 2020).
- McGough, J.J.; Faraone, S.V. Estimating the size of treatment effects: Moving beyond p values. Psychiatry (Edgmont) 2009, 6, 21–29. [Google Scholar]
- Ballantyne, J.C.; Sullivan, M.D. Intensity of Chronic Pain—The Wrong Metric? New Engl. J. Med. 2015, 373, 2098–2099. [Google Scholar] [CrossRef]
- Sullivan, M.D.; Ballantyne, J.C. Must we reduce pain intensity to treat chronic pain? Pain 2016, 157, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Dowell, D.; Haegerich, T.M.; Chou, R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. Recomm. Rep. 2016, 65, 1–49. [Google Scholar] [CrossRef] [PubMed]
- Qaseem, A.; Wilt, T.J.; McLean, R.M.; Forciea, M.A. Clinical Guidelines Committee of the American College of Physicians Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann. Intern. Med. 2017, 166, 514–530. [Google Scholar] [CrossRef] [PubMed]
- Furlan, A.D.; Pennick, V.; Bombardier, C.; Van Tulder, M. 2009 Updated Method Guidelines for Systematic Reviews in the Cochrane Back Review Group. Spine 2009, 34, 1929–1941. [Google Scholar] [CrossRef]
- Chung, J.W.; Zeng, Y.; Wong, T.K. Drug therapy for the treatment of chronic nonspecific low back pain: Systematic review and meta-analysis. Pain Phys. 2013, 16, E685–E704. [Google Scholar]
- Licciardone, J.C. Demographic Characteristics Associated with Utilization of Noninvasive Treatments for Chronic Low back Pain and Related Clinical Outcomes during the COVID-19 Pandemic in the United States. J. Am. Board. Fam. Med. 2020. Available online: https://www.jabfm.org/content/covid-19-ahead-print-subject-collection#25 (accessed on 29 September 2020).
- El-Tallawy, S.N.; Nalamasu, R.; Pergolizzi, J.V.; Gharibo, C. Pain Management During the COVID-19 Pandemic. Pain Ther. 2020, 1–14. [Google Scholar] [CrossRef]
- Shanthanna, H.; Strand, N.H.; Provenzano, D.A.; Lobo, C.A.; Eldabe, S.; Bhatia, A.; Wegener, J.; Curtis, K.; Cohen, S.P.; Narouze, S. Caring for patients with pain during the COVID-19 pandemic: Consensus recommendations from an international expert panel. Anaesthesia 2020, 75, 935–944. [Google Scholar] [CrossRef]
- Cohen, S.P.; Baber, Z.B.; Buvanendran, A.; McLean, L.T.C.B.C.; Chen, Y.; Hooten, W.M.; Laker, S.R.; Wasan, W.A.D.; Kennedy, D.J.; Sandbrink, F.; et al. Pain Management Best Practices from Multispecialty Organizations during the COVID-19 Pandemic and Public Health Crises. Pain Med. 2020, 21, 1331–1346. [Google Scholar] [CrossRef]
- Javed, S.; Hung, J.; Huh, B.K. Impact of COVID-19 on chronic pain patients: A pain physician’s perspective. Pain Manag. 2020, 10, 275–277. [Google Scholar] [CrossRef]
- Kroenke, K.; Talib, T.L.; Stump, T.E.; Kean, J.; Haggstrom, D.A.; DeChant, P.; Lake, K.R.; Stout, M.; Monahan, P.O. Incorporating PROMIS Symptom Measures into Primary Care Practice—A Randomized Clinical Trial. J. Gen. Intern. Med. 2018, 33, 1245–1252. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Experimental Treatment (eHealth Intervention) | Control Treatment (Wait List) | p |
|---|---|---|---|
| n = 52 | n = 50 | ||
| % | % | ||
| Age (year), mean ± SD | 51.3 ± 13.7 | 50.7 ± 13.0 | 0.84 |
| Female gender | 81 | 88 | 0.32 |
| Non-White race | 25 | 18 | 0.39 |
| Hispanic ethnicity | 14 | 6 | 0.32 |
| College education or higher | 37 | 32 | 0.63 |
| Current cigarette smoker | 19 | 8 | 0.10 |
| Low back pain duration greater than 5 years | 71 | 60 | 0.24 |
| Ever unemployed or unable to do usual work | |||
| for one month or longer due to low back pain | 58 | 54 | 0.71 |
| Ever received disability or workers’ compensation | |||
| benefits relating to low back pain | 25 | 28 | 0.73 |
| Ever involved in a lawsuit or legal claim relating to low back pain | 10 | 10 | >0.99 |
| Currently using NSAIDs for low back pain | 62 | 72 | 0.26 |
| Currently using opioids for low back pain | 50 | 42 | 0.42 |
| Ever had surgery for low back pain | 23 | 22 | 0.90 |
| Comorbidities ever reported | |||
| Herniated disc | 48 | 44 | 0.68 |
| Sciatica | 52 | 58 | 0.54 |
| Osteoporosis | 17 | 16 | 0.86 |
| Osteoarthritis | 39 | 48 | 0.33 |
| Heart disease | 10 | 12 | 0.70 |
| Hypertension | 48 | 40 | 0.41 |
| Diabetes mellitus | 33 | 24 | 0.33 |
| Asthma | 23 | 20 | 0.71 |
| Depression | 64 | 64 | 0.95 |
| SPADE cluster score, mean ± SD | 61.8 ± 4.2 | 61.4 ± 4.3 | 0.67 |
| SPADE scale scores | |||
| Sleep disturbance, mean ± SD | 60.8 ± 7.1 | 61.1 ± 7.7 | 0.83 |
| Pain interference with activities, mean ± SD | 66.4 ± 5.1 | 66.5 ± 5.7 | 0.93 |
| Anxiety, mean ± SD | 59.6 ± 7.4 | 58.3 ± 7.7 | 0.40 |
| Depression, mean ± SD | 59.6 ± 7.9 | 55.9 ± 8.0 | 0.02 |
| Low energy/fatigue, mean ± SD | 62.5 ± 7.9 | 65.1 ± 6.6 | 0.07 |
| NRS score, mean ± SD | 6.0 ± 1.7 | 6.2 ± 1.9 | 0.55 |
| RMDQ score, mean ± SD | 17.3 ± 4.2 | 16.3 ± 5.3 | 0.28 |
| Survey Item | % |
|---|---|
| Overall value rating of the report (100-point NRS) (mean ± SD) | 62.9 ± 29.0 |
| Report was easy to understand after reading the interpretation guide | |
| Strongly agree | 47 |
| Agree | 39 |
| Neither agree nor disagree | 8 |
| Disagree | 4 |
| Strongly disagree | 2 |
| Report provided information about quality of life that I did not know | |
| Strongly agree | 24 |
| Agree | 55 |
| Neither agree nor disagree | 12 |
| Disagree | 6 |
| Strongly disagree | 4 |
| Patient actions prompted by the report | |
| Reading or learning more about improving health-related quality of life | 77 |
| Beginning a new program to improve health-related quality of life | 41 |
| Outcome Measure | Experimental Treatment (eHealth Intervention) | Control Treatment (Wait List) | p | Effect Size (SMD) |
|---|---|---|---|---|
| n = 51 | n = 49 | |||
| Mean Change Score (95% CI) | Mean Change Score (95% CI) | |||
| Primary Outcome Measures | ||||
| SPADE cluster score | 1.2 (0.2–2.2) | 0.2 (−1.1–1.5) | 0.23 | 0.24 |
| SPADE scale scores | ||||
| Sleep disturbance | 1.0 (−0.6–2.6) | 0.1 (−1.5–1.8) | 0.47 | 0.15 |
| Pain interference with activities | 1.3 (−0.1–2.6) | 0.9 (−0.5–2.4) | 0.72 | 0.07 |
| Anxiety | 1.2 (−1.0–3.4) | −0.8 (−3.1–1.6) | 0.23 | 0.24 |
| Depression | 1.9 (−0.1–3.9) | −1.1 (−3.6–1.4) | 0.06 | 0.37 |
| Low energy/fatigue | 0.7 (−1.1–2.5) | 1.8 (−0.6–4.2) | 0.47 | −0.15 |
| Secondary Outcome Measures | ||||
| Low back pain intensity (NRS score) | −0.3 (−0.8–0.2) | −0.1 (−0.5–0.3) | 0.59 | −0.11 |
| Back-related disability (RMDQ score) | 0.9 (−0.3–2.1) | −0.4 (−1.2–0.4) | 0.07 | 0.36 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Licciardone, J.C.; Pandya, V. Feasibility Trial of an eHealth Intervention for Health-Related Quality of Life: Implications for Managing Patients with Chronic Pain During the COVID-19 Pandemic. Healthcare 2020, 8, 381. https://doi.org/10.3390/healthcare8040381
Licciardone JC, Pandya V. Feasibility Trial of an eHealth Intervention for Health-Related Quality of Life: Implications for Managing Patients with Chronic Pain During the COVID-19 Pandemic. Healthcare. 2020; 8(4):381. https://doi.org/10.3390/healthcare8040381
Chicago/Turabian StyleLicciardone, John C., and Vishruti Pandya. 2020. "Feasibility Trial of an eHealth Intervention for Health-Related Quality of Life: Implications for Managing Patients with Chronic Pain During the COVID-19 Pandemic" Healthcare 8, no. 4: 381. https://doi.org/10.3390/healthcare8040381
APA StyleLicciardone, J. C., & Pandya, V. (2020). Feasibility Trial of an eHealth Intervention for Health-Related Quality of Life: Implications for Managing Patients with Chronic Pain During the COVID-19 Pandemic. Healthcare, 8(4), 381. https://doi.org/10.3390/healthcare8040381




