Total Hip Arthroplasty in Post-Bariatric Surgery Patients: Increased Risks and Economic Burden?
Abstract
1. Introduction
Research Questions
2. Methods
2.1. Dataset Description
2.2. Study Timeline and Data Source
2.3. Inclusion Criteria and Exclusion Parameters
2.4. Statistical Approach and Matching Protocol
2.5. Identification of Comorbidities and Clinical Outcomes
2.6. Ethical Considerations
3. Results
3.1. Comparative Analysis of THA Patients with and Without a History of Bariatric Surgery
3.2. Comparative Analysis of Comorbidities in THA Patients with and Without a History of Bariatric Surgery
3.3. Propensity Score-Matched Analysis of Comorbidities in THA Patients with and Without a History of Bariatric Surgery
3.4. Comparison of Hospitalization Outcomes in Propensity Score-Matched THA Patients
3.5. Comparison of Select Postoperative Complications in Propensity Score-Matched THA Patients with and Without a History of Bariatric Surgery
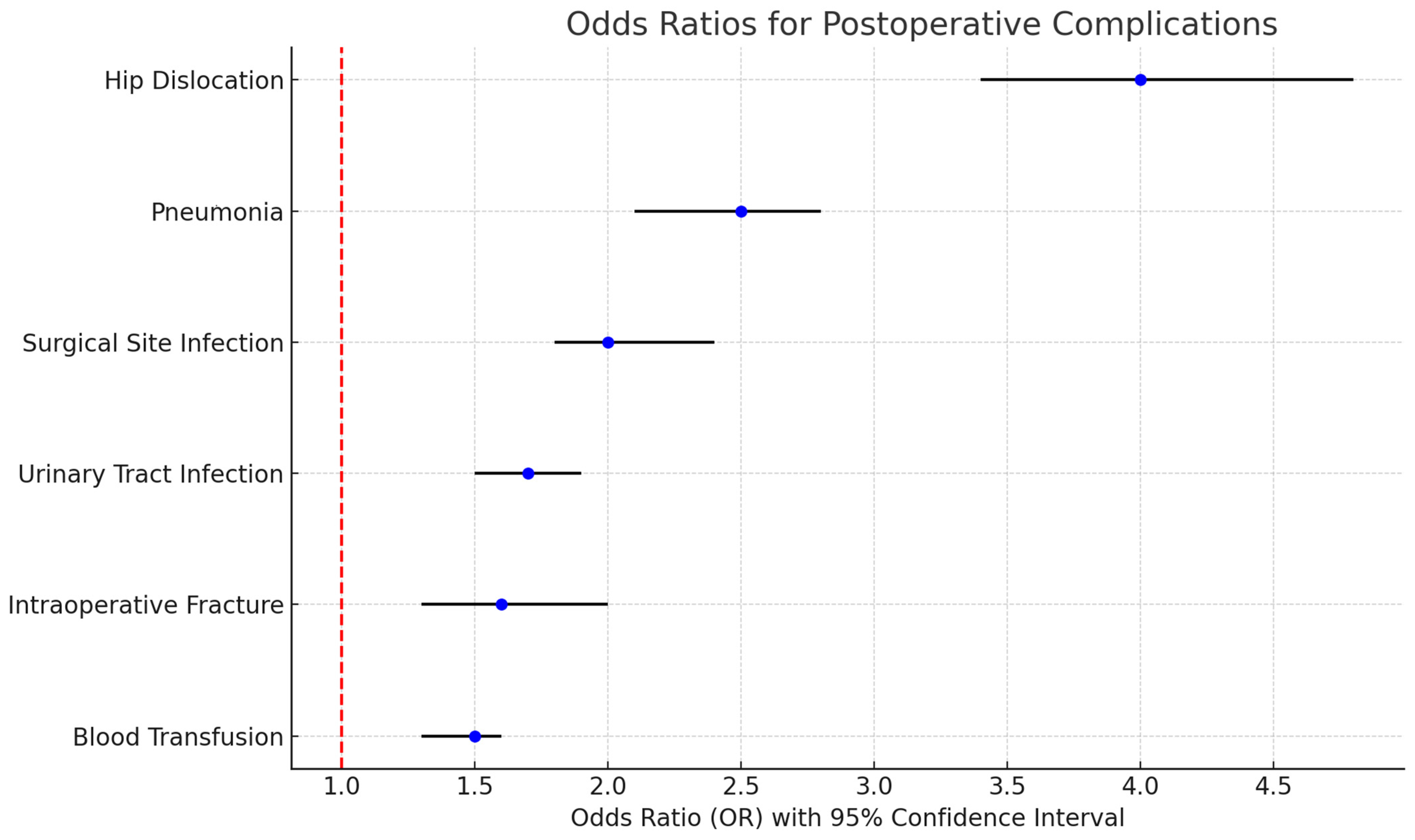
3.6. Elevated Risk Ratios for Complications in THA Patients with a History of Bariatric Surgery Compared to Propensity Score-Matched Patients Without Such History
4. Discussion
4.1. Main Findings
4.1.1. Increased Prevalence of THA in Post-Bariatric Surgery Patients
4.1.2. Economic Impact and Length of Hospital Stay
4.1.3. Increased Postoperative Complications
4.1.4. Short-Term Benefits vs. Long-Term Outcomes
4.1.5. Emerging Pharmacological Interventions
4.2. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CKD | Chronic Kidney Disease |
| DM | Diabetes Mellitus |
| ICD-10 | International Classification of Diseases, 10th Revision |
| LOS | Length of Stay |
| NIS | Nationwide Inpatient Sample |
| OR | Odds Ratio |
| OSA | Obstructive Sleep Apnea |
| SSI | Surgical Site Infection |
| THA | Total Hip Arthroplasty |
| UTI | Urinary Tract Infection |
Appendix A
| ICD 10 CODES/PROCEDURE CODE. | |
| I5021, I5031, I5033, I5041, I5043 | Heart Failure |
| N170, N171, N172, N178, N179 | Acute Kidney Injury |
| I2101, I2102, I2109, I211, I2119, I2111, I212, I2129, I213, I214, I219 | Acute Coronary Artery Disease |
| I60, I61, I62, I63, I650, I688, O873, O2250, O2251, O2252 | Stroke |
| J810, J811, I501 | Pulmonary Edema |
| I10 (start with) | Hypertension |
| D62 (start with) | Blood Loss Anemia |
| J189, J159, J22 | Pneumonia |
| I2602, I2609, I2692, I2699 | Pulmonary Embolism |
| I82401, I82402, I82403, I82409, I82411, I82412, I82413, I82419, I82421, I82422, I82423, I82429 | DVT |
| E78 (start with) | Dyslipidemia |
| G473 | Obstructive Sleep Apnea |
| D64 (start with) | Chronic Anemia |
| F10 | Alcohol Abuse History |
| M81, M82 | Osteoporosis |
| F (start with) | Mental Disorders |
| G20 (start with) | Parkinson Disease |
| E11 (start with) | Type 2 Diabetes Mellitus |
| N18 (start with) | Chronic Kidney Disease |
| I500, I501, I509 | Congestive Heart Failure |
| J44 (start with) | Chronic Lung Disease |
References
- Fontalis, A.; Epinette, J.A.; Thaler, M.; Zagra, L.; Khanduja, V.; Haddad, F.S. Advances and innovations in total hip arthroplasty. SICOT J. 2021, 7, 26. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Apovian, C.M. Obesity: Definition, comorbidities, causes, and burden. Am. J. Manag. Care 2016, 22 (Suppl. S7), s176–s185. [Google Scholar] [PubMed]
- Hennrikus, M.; Hennrikus, W.P.; Lehman, E.; Skolka, M.; Hennrikus, E. The obesity paradox and orthopedic surgery. Medicine 2021, 100, e26936. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- DeMik, D.E.; Bedard, N.A.; Dowdle, S.B.; Elkins, J.M.; Brown, T.S.; Gao, Y.; Callaghan, J.J. Complications and Obesity in Arthroplasty-A Hip is Not a Knee. J. Arthroplast. 2018, 33, 3281–3287. [Google Scholar] [CrossRef] [PubMed]
- Uebelhart, B. Effects of bariatric surgery on bone. Jt. Bone Spine 2016, 83, 271–275. [Google Scholar] [CrossRef]
- Lazzati, A. Epidemiology of the surgical management of obesity. J. Visc. Surg. 2023, 160, S3–S6. [Google Scholar] [CrossRef] [PubMed]
- AMTCO Group; Bettencourt-Silva, R.; Neves, J.S.; Pedro, J.; Guerreiro, V.; Ferreira, M.J.; Salazar, D.; Souteiro, P.; Magalhães, D.; Oliveira, S.C.; et al. Comparative Effectiveness of Different Bariatric Procedures in Super Morbid Obesity. Obes. Surg. 2019, 29, 281–291. [Google Scholar] [CrossRef] [PubMed]
- Tsui, S.T.; Yang, J.; Zhang, X.; Tatarian, T.; Docimo, S.; Spaniolas, K.; Pryor, A.D. Health disparity in access to bariatric surgery. Surg. Obes. Relat. Dis. 2021, 17, 249–255. [Google Scholar] [CrossRef] [PubMed]
- van Rijswijk, A.-S.; van Olst, N.; Schats, W.; van der Peet, D.L.; van de Laar, A.W. What is weight loss after bariatric surgery expressed in percentage total weight loss (%TWL)? A systematic review. Obes. Surg. 2021, 31, 3833–3847. [Google Scholar] [CrossRef]
- Schwarzkopf, R.; Lavery, J.A.; Hooper, J.; Parikh, M.; Gold, H.T. Bariatric Surgery and Time to Total Joint Arthroplasty: Does It Affect Readmission and Complication Rates? Obes. Surg. 2018, 28, 1395–1401. [Google Scholar] [CrossRef] [PubMed]
- McLawhorn, A.S.; Levack, A.E.; Lee, Y.Y.; Ge, Y.; Do, H.; Dodwell, E.R. Bariatric Surgery Improves Outcomes After Lower Extremity Arthroplasty in the Morbidly Obese: A Propensity Score-Matched Analysis of a New York Statewide Database. J. Arthroplast. 2018, 33, 2062–2069.e4. [Google Scholar] [CrossRef] [PubMed]
- Aderinto, N.; Olatunji, G.; Kokori, E.; Olaniyi, P.; Isarinade, T.; Yusuf, I.A. Recent advances in bariatric surgery: A narrative review of weight loss procedures. Ann. Med. Surg. 2023, 85, 6091–6104. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Y.; Guo, X.; Lu, X.; Mattar, S.; Kassab, G. Mechanisms of Weight Loss After Sleeve Gastrectomy and Adjustable Gastric Banding: Far More Than Just Restriction. Obesity 2019, 27, 1776–1783. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Deng, Z.; Meng, J.; Dai, Q.; Chen, T.; Bao, N. Impact of Bariatric Surgery on Inpatient Complication, Cost, and Length of Stay Following Total Hip or Knee Arthroplasty. J. Arthroplast. 2019, 34, 2884–2889.e4. [Google Scholar] [CrossRef]
- van de Pas, K.G.H.; Noushi, A.E.; Janssen, L.; Vreugdenhil, A.C.E.; Leclercq, W.K.G.; van Dielen, F.M.H.; Dutch Audit for Treatment of Obesity Research Group. A Population-Based Cohort Study on Efficacy and Safety of Bariatric Surgery in Young Adults Versus Adults. Obes. Surg. 2023, 33, 2475–2484. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cooiman, M.I.; Aarts, E.O.; Janssen, I.M.C.; Hazebroek, E.J.; Berends, F.J. Weight Loss, Remission of Comorbidities, and Quality of Life After Bariatric Surgery in Young Adult Patients. Obes. Surg. 2019, 29, 1851–1857. [Google Scholar] [CrossRef] [PubMed]
- Perdomo, C.M.; Landecho, M.F.; Valentí, V.; Moncada, R.; Frühbeck, G. Clinical Perspectives, Eligibility, and Success Criteria for Bariatric/Metabolic Surgery. Adv. Exp. Med. Biol. 2024, 1460, 677–695. [Google Scholar] [CrossRef] [PubMed]
- Rajesh, D.A.; Witvoet, S.; Coppolecchia, A.; Scholl, L.; Chen, A.F. Length of Stay and Discharge Disposition After Total Hip Arthroplasty: A Large Multicenter Propensity Matched Comparison of Robotic-Assisted and Manual Techniques. J. Arthroplast. 2024, 39, S117–S123. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, M.W.; Gibbs, B.; Ronald, A.A.; Novikov, D.; Yang, A.; Salavati, S.; Abdeen, A. Is a Rapid Recovery Protocol for THA and TKA Associated With Decreased 90-day Complications, Opioid Use, and Readmissions in a Health Safety-net Hospital? Clin. Orthop. Relat. Res. 2024, 482, 1442–1451. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Holanda, N.; Crispim, N.; Carlos, I.; Moura, T.; Nóbrega, E.; Bandeira, F. Musculoskeletal effects of obesity and bariatric surgery—A narrative review. Arch. Endocrinol. Metab. 2022, 66, 621–632. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, J.; Nimeri, A.; Khorgami, Z.; El Chaar, M.; Lima, A.G.; Vosburg, R.W.; American Society for Metabolic and Bariatric Surgery (ASMBS) Clinical Issues Committee. Metabolic bone changes after bariatric surgery: 2020 update, American Society for Metabolic and Bariatric Surgery Clinical Issues Committee position statement. Surg. Obes. Relat. Dis. 2021, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gagner, M. Comment on: Metabolic bone changes after bariatric surgery: 2020 update, American Society for Metabolic and Bariatric Surgery Clinical Issues Committee position statement. Surg. Obes. Relat. Dis. 2021, 17, 1229–1230. [Google Scholar] [CrossRef] [PubMed]
- Valera, R.J.; Sarmiento-Cobos, M.; Montorfano, L.; Khan, M.; Menzo, E.L.; Szomstein, S.; Rosenthal, R.J. Predictors and outcomes of acute kidney injury after bariatric surgery: Analysis of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program data registry. Surg. Obes. Relat. Dis. 2023, 19, 1302–1307. [Google Scholar] [CrossRef] [PubMed]
- Hanipah, Z.N.; Punchai, S.; Augustin, T.; Brethauer, S.A.; Schauer, P.R.; Aminian, A. Impact of Early Postbariatric Surgery Acute Kidney Injury on Long-Term Renal Function. Obes. Surg. 2018, 28, 3580–3585. [Google Scholar] [CrossRef] [PubMed]
- Koppe, U.; Nitsch, D.; E Mansfield, K.; Mathur, R.; Bhaskaran, K.; Batterham, R.L.; Smeeth, L.; Douglas, I.J. Long-term effects of bariatric surgery on acute kidney injury: A propensity-matched cohort in the UK Clinical Practice Research Datalink. BMJ Open 2018, 8, e020371. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cai, H.; Zhan, Y.; Lu, J.; Zhu, M.; Liu, S.; Mei, J.; Zhang, P.; Liu, R.; Ni, Z.; Zhang, W.; et al. Body mass index combined with waist circumference can predict moderate chronic kidney disease: A retrospective study. Medicine 2021, 100, e25017. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kounatidis, D.; Vallianou, N.G.; Stratigou, T.; Voukali, M.; Karampela, I.; Dalamaga, M. The Kidney in Obesity: Current Evidence, Perspectives and Controversies. Curr. Obes. Rep. 2024, 13, 680–702. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.I.; Khilnani, T.K.; LaValva, S.M.; Goodman, S.M.; Della Valle, A.G.; Lee, G.C. Utilization of Glucagon-Like Peptide-1 Receptor Agonist at the Time of Total Hip Arthroplasty for Patients Who Have Morbid Obesity. J. Arthroplast. 2024; in press. [Google Scholar] [CrossRef] [PubMed]
- Maman, D.; Mahamid, A.; Finkel, B.; Gan-Or, H.; Fournier, L.; Berkovich, Y.; Behrbalk, E. Comparative evaluation of postoperative outcomes and expenditure between robotic and conventional single-level lumbar fusion surgery: A comprehensive analysis of nationwide inpatient sample data. Eur. Spine J. 2024, 33, 2637–2645. [Google Scholar] [CrossRef]
- Maman, D.; Laver, L.; Becker, R.; Takrori, L.A.; Mahamid, A.; Finkel, B.; Gan-Or, H.; Yonai, Y.; Berkovich, Y. Trends and Epidemiology in Robotic-Assisted Total Knee Arthroplasty: Reduced Complications and Shorter Hospital Stays. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 3281–3288. [Google Scholar] [CrossRef]
- Maman, D.; Mahamid, A.; Yonai, Y.; Berkovich, Y. Comparing Complication Rates, Costs, and Length of Stay between Unicompartmental and Total Knee Arthroplasty: Insights from a Big Data Analysis Using the National Inpatient Sample Dataset. J. Clin. Med. 2024, 13, 3888. [Google Scholar] [CrossRef]

| Parameter | No History of Bariatric Surgery | History of Bariatric Surgery | Significance |
|---|---|---|---|
| Total Surgeries | 1,474,380 | 20,429 | - |
| Average Age (y) | 66.0 | 60.3 | p < 0.01 |
| Female (%) | 55.5 | 75.0 | p < 0.01 |
| payer—Medicare (%) | 55.2 | 43.5 | p < 0.01 |
| payer—Medicaid (%) | 4.5 | 5.6 | |
| payer—private including HMO (%) | 37.2 | 47.6 | |
| payer—self-pay (%) | 0.7 | 0.3 | |
| payer—no charge (%) | 0 | 0 | |
| payer—other (%) | 2.3 | 2.9 |
| Parameter | No History of Bariatric Surgery | History of Bariatric Surgery | Significance |
|---|---|---|---|
| Hypertension (%) | 52.5 | 55.3 | p < 0.01 |
| Dyslipidemia (%) | 43 | 34 | p < 0.01 |
| Obstructive Sleep Apnea (%) | 9.9 | 22.1 | p < 0.01 |
| Chronic Anemia (%) | 5.6 | 8.4 | p < 0.01 |
| Alcohol Abuse (%) | 1.3 | 1.5 | p < 0.01 |
| Osteoporosis (%) | 4.4 | 5.8 | p < 0.01 |
| Chronic Kidney Disease (%) | 6.3 | 5.4 | p < 0.01 |
| Congestive Heart Failure (%) | 1.1 | 1.5 | p < 0.01 |
| Chronic Lung Disease (%) | 6.3 | 5 | p < 0.01 |
| Diabetes Mellitus (%) | 14.9 | 21.2 | p < 0.01 |
| Obesity (%) | 23.3 | 54.2 | p < 0.01 |
| Chronic use of anticoagulants (%) | 5.5 | 7.6 | p < 0.01 |
| Parameter | No History of Bariatric Surgery | History of Bariatric Surgery | Sign. |
|---|---|---|---|
| Total Surgeries | 20,429 | 20,429 | - |
| Average Age (y) | 60.2 | 60.3 | p = 0.13 |
| Female (%) | 74.8 | 75 | p = 0.61 |
| payer—Medicare (%) | 42.7 | 42.7 | p = 0.32 |
| payer—Medicaid (%) | 5.8 | 6.1 | |
| payer—private including HMO (%) | 48.4 | 47.9 | |
| payer—self-pay (%) | 0.5 | 0.5 | |
| payer—no charge (%) | 0.1 | 0 | |
| payer—other (%) | 2.5 | 2.8 | |
| Hypertension (%) | 55.7 | 55.3 | p = 0.40 |
| Dyslipidemia (%) | 34 | 34 | p = 1 |
| Obstructive Sleep Apnea (%) | 21.9 | 22.1 | p = 0.64 |
| Chronic Anemia (%) | 8.1 | 8.4 | p = 0.10 |
| Alcohol Abuse (%) | 1.6 | 1.5 | p = 0.16 |
| Osteoporosis (%) | 5.5 | 5.8 | p = 0.54 |
| Chronic Kidney Disease (%) | 5 | 5.4 | p = 0.06 |
| Congestive Heart Failure (%) | 1.2 | 1.5 | p = 0.09 |
| Chronic Lung Disease (%) | 5.1 | 5.0 | p = 0.82 |
| Diabetes Mellitus (%) | 21 | 21.2 | p = 0.63 |
| Obesity (%) | 54.6 | 54.2 | p = 0.40 |
| Chronic use of anticoagulants (%) | 7.8 | 7.6 | p = 0.34 |
| No History of Bariatric Surgery | History of Bariatric Surgery | Significance | |
|---|---|---|---|
| Length of stay mean in days | 2.37 (Std. deviation 1.6) | 2.17 (Std. deviation 2.1) | p = 0.03 |
| Total charges mean in $ | 62,883 (Std. deviation 33,835) | 63,631 ( Std. deviation 36,975) | p < 0.01 |
| Parameter | No History of Bariatric Surgery | History of Bariatric Surgery | Significance |
|---|---|---|---|
| AKI (%) | 1.6 | 1.3 | p = 0.01 |
| DVT (%) | 0.1 | 0.1 | p = 0.16 |
| Blood Loss Anemia (%) | 20.1 | 20.5 | p = 0.36 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berkovich, Y.; Rosenberg, L.; Fournier, L.; Steinfeld, Y.; Maman, D. Total Hip Arthroplasty in Post-Bariatric Surgery Patients: Increased Risks and Economic Burden? Healthcare 2025, 13, 887. https://doi.org/10.3390/healthcare13080887
Berkovich Y, Rosenberg L, Fournier L, Steinfeld Y, Maman D. Total Hip Arthroplasty in Post-Bariatric Surgery Patients: Increased Risks and Economic Burden? Healthcare. 2025; 13(8):887. https://doi.org/10.3390/healthcare13080887
Chicago/Turabian StyleBerkovich, Yaron, Lahav Rosenberg, Linor Fournier, Yaniv Steinfeld, and David Maman. 2025. "Total Hip Arthroplasty in Post-Bariatric Surgery Patients: Increased Risks and Economic Burden?" Healthcare 13, no. 8: 887. https://doi.org/10.3390/healthcare13080887
APA StyleBerkovich, Y., Rosenberg, L., Fournier, L., Steinfeld, Y., & Maman, D. (2025). Total Hip Arthroplasty in Post-Bariatric Surgery Patients: Increased Risks and Economic Burden? Healthcare, 13(8), 887. https://doi.org/10.3390/healthcare13080887






