Frailty Prevention Care Management Program (FPCMP) on Frailty and Health Function in Community-Dwelling Older Adults: A Quasi-Experimental Trial Protocol
Abstract
:1. Introduction
- (1)
- To develop and implement a program for the Frailty Prevention Care Management Program of community-dwelling older adults;
- (2)
- To assess the impact of the intervention regarding frailty (physical, psychologic, and social domain), health function, and nutrition in the two groups (experimental and control group);
- (3)
- To assess the impact of the Frailty Prevention Care Management Program intervention regarding frailty (physical, psychologic, and social domain) and nutrition immediately post-intervention and 3 months post intervention in the two groups.
2. Materials and Methods
2.1. Participants and Eligibility
2.1.1. Establish a Cooperative Relationship with the Local Township Head, Village Head, or Person in Charge of the Base
2.1.2. Preliminary Solicitation of Patients Willing to Participate in the Testing
2.2. Recruitment of Participants
3. Outcome Measures and Measurement Procedures
3.1. Description of Outcome Measures
3.1.1. Baseline Measures
Chronic Disease and Health Problems
3.1.2. Primary Outcome
Frailty
3.1.3. Secondary Outcomes
Health Function (Physical Function—Senior Fitness Test, SFT)
Health Function (Nutrition—Mini Nutritional Assessment-Short Form, MNA-SF)
4. Therapeutic Intervention
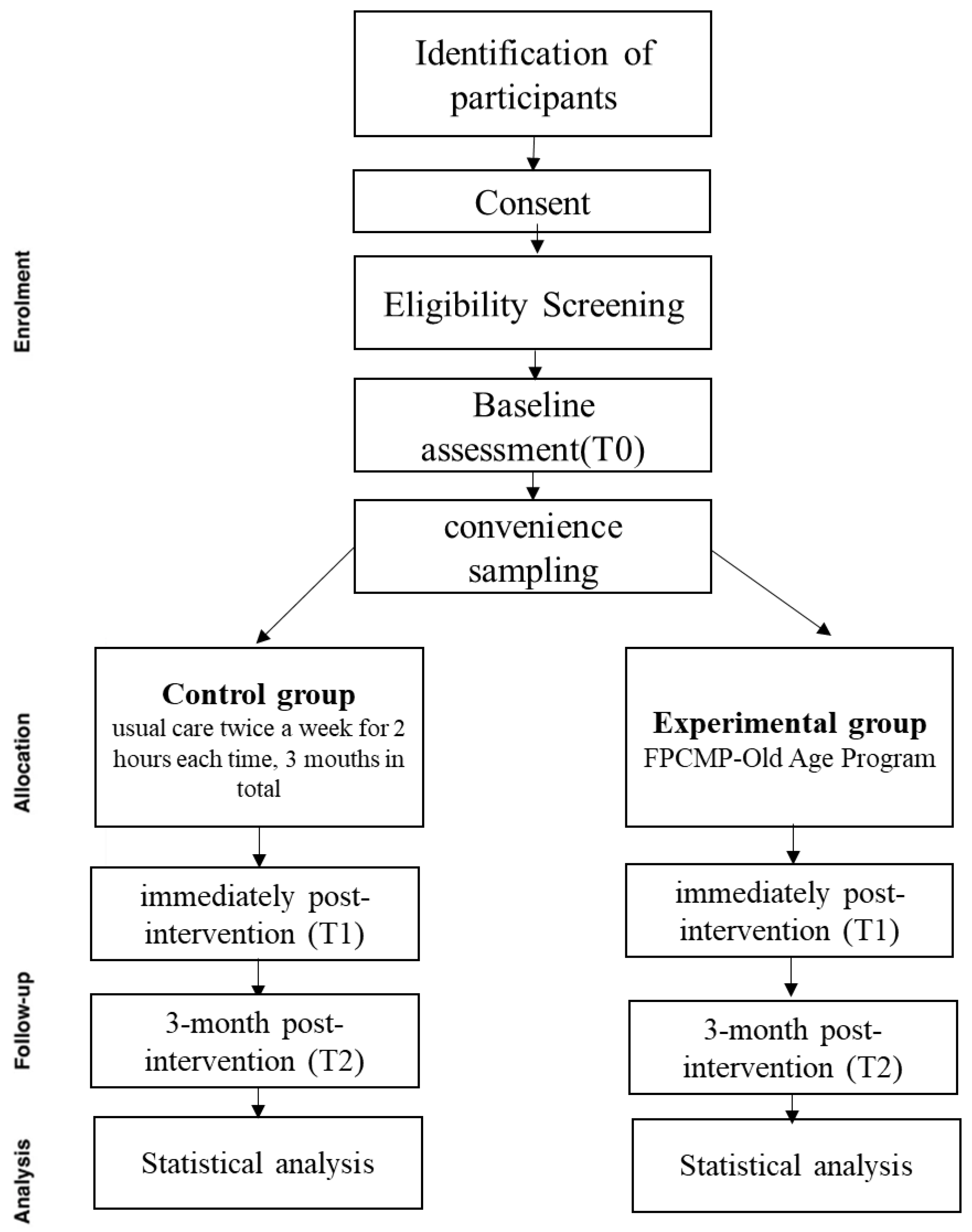
4.1. Study Protocol
4.2. Experimental Group
4.2.1. Frailty Prevention Care Management Program-Old Age Program
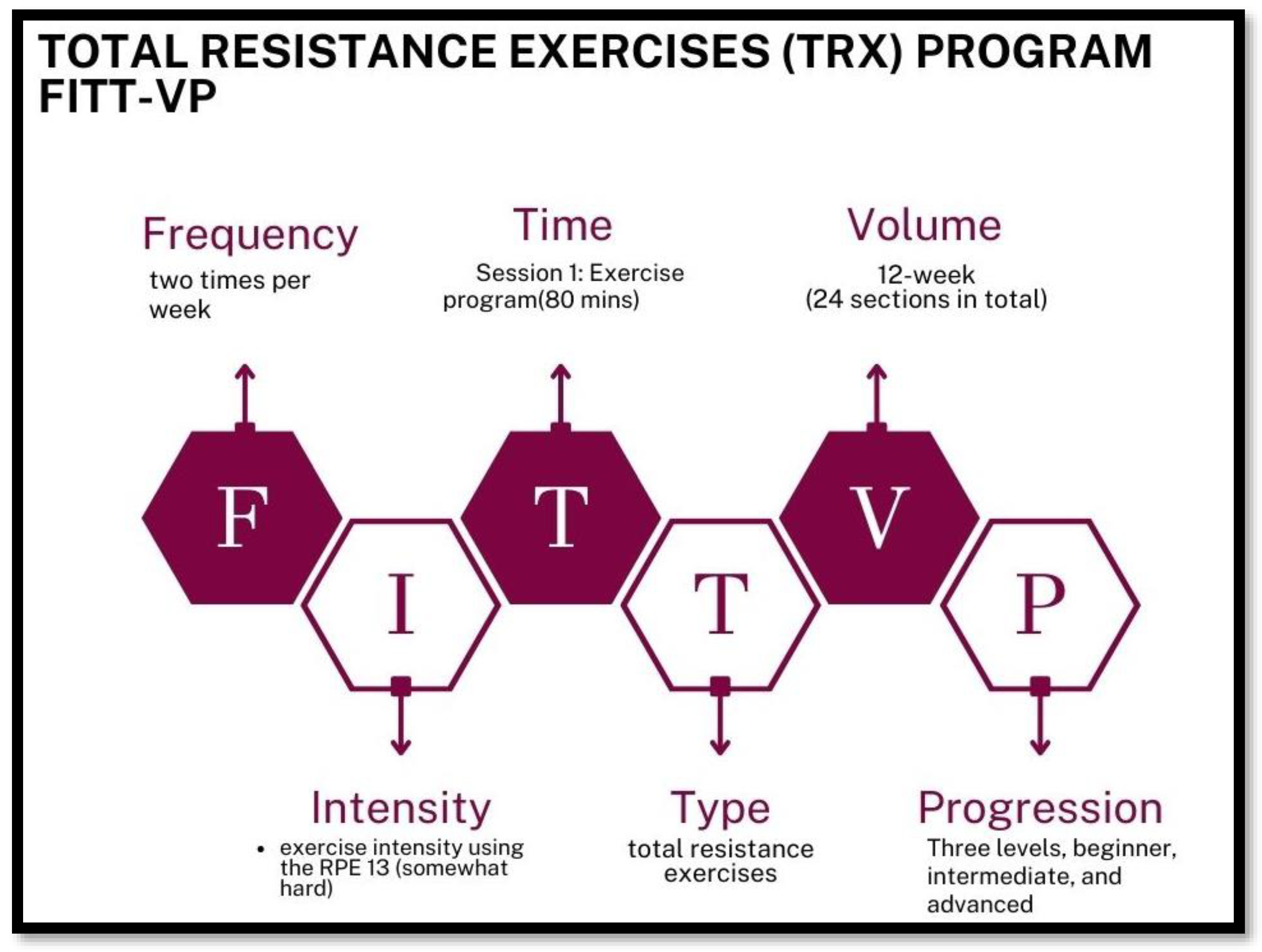
4.2.2. Session 1: Exercise Program-Total Resistance Exercises (TRX) Program
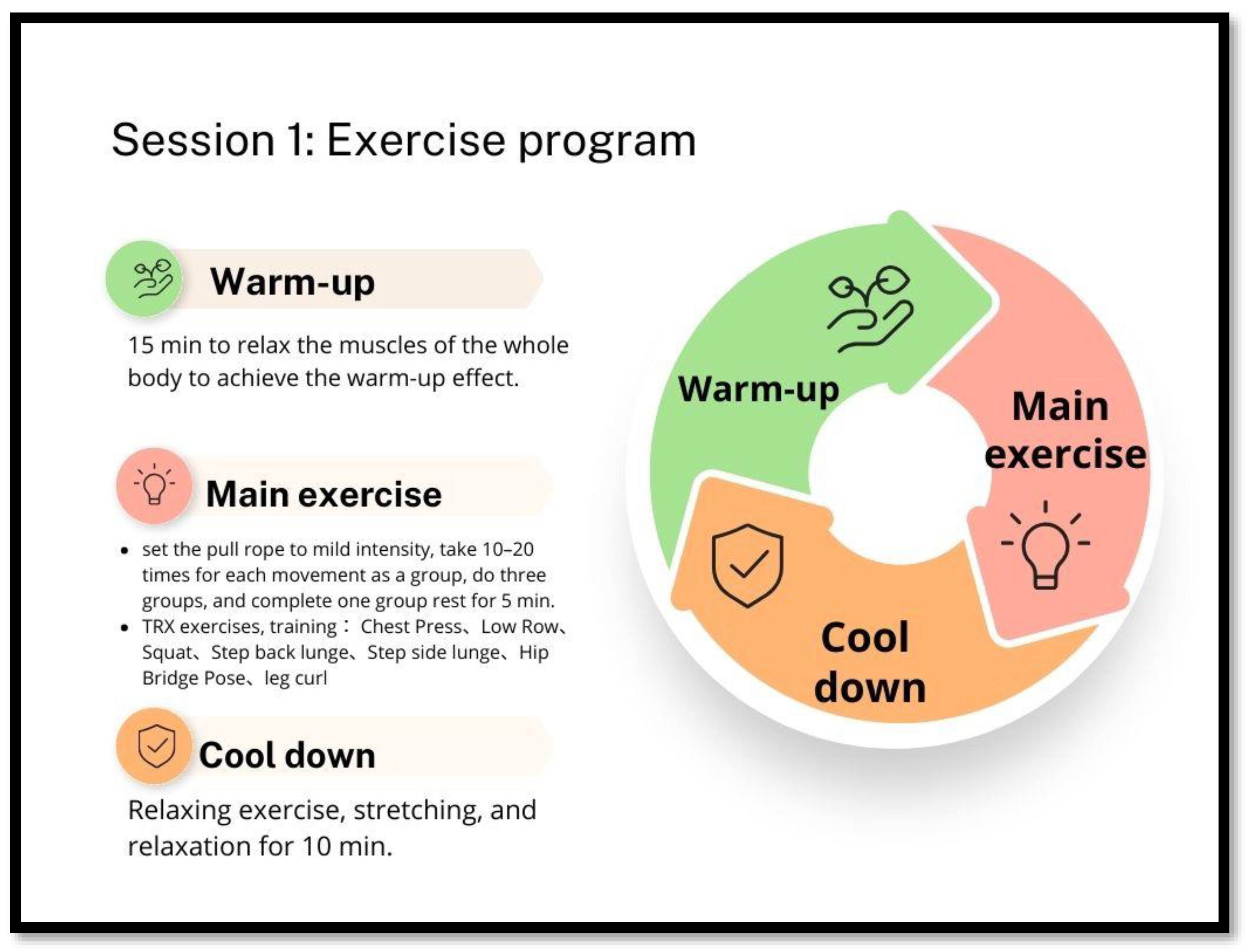
Each Course Is Divided into Three Parts
- (1)
- Warm-up: A total of 15 min to relax the muscles of the whole body to achieve the warm-up effect.
- (2)
- Main exercise: According to the physical function of older adults, they will start training from the simplest movements and angles, set the pull rope to mild intensity, take 10–20 times for each movement as a group, perform three sets as a group, and complete one group rest for 5 min. The following was a description of the scheduled execution movements: performing upper limb TRX exercises, such as ‘Chest Press’ movements (training pectoralis major, anterior deltoid muscles, and triceps brachii) and ‘Low Row’ movements (training back muscles, rear deltoid, and biceps); performing lower body TRX exercises, as as ‘Squat’ (lower body muscles) and ‘Step Back Lunge’ and ‘Step Side Lunge’ (lower body muscles, stability, balance, single leg stability, and power hip adductors). Further, they will perform the ‘Hip Bridge Pose’ (triceps, core, hip flexors, quadriceps, and hamstrings), ‘Leg Curl’ (biceps and core muscles), and eight other movements [40].
- (3)
- Cool down: Relaxing exercise, stretching, and relaxation for 10 min.
4.2.3. Session 2: Nutrition Program
4.3. Control Group
5. Statistical Analysis
5.1. Data Analysis
5.2. Sample Size
5.3. Data Management
6. Discussion
FPCMP-Old Age Program Development Challenges and Solutions
7. Expected Results and Possible Benefits
- Exercise and adequate nutritional support appear to have promising effects on preventing frailty and improving physical activity and overall functioning, with significant effects on physical function and preventing frailty in older adults.
- Provide an exercise prescription-FPCMP-Old Age Program to prevent frailty in older adults and verify its effectiveness through the intervention of this study.
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ofori-Asenso, R.; Chin, K.L.; Mazidi, M.; Zomer, E.; Ilomaki, J.; Zullo, A.R.; Gasevic, D.; Ademi, Z.; Korhonen, M.J.; LoGiudice, D. Global incidence of frailty and prefrailty among community-dwelling older adults: A systematic review and meta-analysis. JAMA Netw. Open 2019, 2, e198398. [Google Scholar] [CrossRef] [PubMed]
- Cesari, M.; Vellas, B.; Hsu, F.-C.; Newman, A.B.; Doss, H.; King, A.C.; Manini, T.M.; Church, T.; Gill, T.M.; Miller, M.E. A physical activity intervention to treat the frailty syndrome in older persons—Results from the LIFE-P study. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2015, 70, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Masel, M.C.; Ostir, G.V.; Ottenbacher, K.J. Frailty, mortality, and health-related quality of life in older Mexican Americans. J. Am. Geriatr. Soc. 2010, 58, 2149–2153. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef] [PubMed]
- Levers, M.J.; Estabrooks, C.A.; Ross Kerr, J.C. Factors contributing to frailty: Literature review. J. Adv. Nurs. 2006, 56, 282–291. [Google Scholar] [CrossRef]
- Gobbens, R.J.; van Assen, M.A.; Luijkx, K.G.; Wijnen-Sponselee, M.T.; Schols, J.M. Determinants of frailty. J. Am. Med. Dir. Assoc. 2010, 11, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Brown, I.; Renwick, R.; Raphael, D. Frailty: Constructing a common meaning, definition, and conceptual framework. Int. J. Rehabil. Res. 1995, 18, 93–102. [Google Scholar] [CrossRef]
- Makizako, H.; Kubozono, T.; Kiyama, R.; Takenaka, T.; Kuwahata, S.; Tabira, T.; Kanoya, T.; Horinouchi, K.; Shimada, H.; Ohishi, M. Associations of social frailty with loss of muscle mass and muscle weakness among community-dwelling older adults. Geriatr. Gerontol. Int. 2019, 19, 76–80. [Google Scholar] [CrossRef]
- Cook, M.J.; Oldroyd, A.; Pye, S.R.; Ward, K.A.; Gielen, E.; Ravindrarajah, R.; Adams, J.E.; Lee, D.M.; Bartfai, G.; Boonen, S. Frailty and bone health in European men. Age Ageing 2017, 46, 635–641. [Google Scholar] [CrossRef]
- Pek, K.; Chew, J.; Lim, J.P.; Yew, S.; Tan, C.N.; Yeo, A.; Ding, Y.Y.; Lim, W.S. Social frailty is independently associated with mood, nutrition, physical performance, and physical activity: Insights from a theory-guided approach. Int. J. Environ. Res. Public Health 2020, 17, 4239. [Google Scholar] [CrossRef]
- Quach, L.T.; Primack, J.; Bozzay, M.; Madrigal, C.; Erqou, S.; Rudolph, J.L. The intersection of physical and social frailty in older adults. Rhode Isl. Med. J. (2013) 2021, 104, 16. [Google Scholar]
- Ha, J.; Park, Y.-H. Effects of a person-centered nursing intervention for frailty among prefrail community-dwelling older adults. Int. J. Environ. Res. Public Health 2020, 17, 6660. [Google Scholar] [CrossRef] [PubMed]
- Drennan, V.; Walters, K.; Avgerinou, C.; Gardner, B.; Goodman, C.; Frost, R.; Kharicha, K.; Iliffe, S.; Manthorpe, J. Moving upstream in health promoting policies for older people with early frailty in England? A policy analysis. J. Health Serv. Res. Policy 2018, 23, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Abizanda, P.; López, M.D.; García, V.P.; de Dios Estrella, J.; da Silva González, Á.; Vilardell, N.B.; Torres, K.A. Effects of an oral nutritional supplementation plus physical exercise intervention on the physical function, nutritional status, and quality of life in frail institutionalized older adults: The ACTIVNES study. J. Am. Med. Dir. Assoc. 2015, 16, 439.e9–439.e16. [Google Scholar] [CrossRef] [PubMed]
- Haider, S.; Dorner, T.E.; Luger, E.; Kapan, A.; Titze, S.; Lackinger, C.; Schindler, K.E. Impact of a home-based physical and nutritional intervention program conducted by lay-volunteers on handgrip strength in prefrail and frail older adults: A randomized control trial. PLoS ONE 2017, 12, e0169613. [Google Scholar] [CrossRef] [PubMed]
- Casas-Herrero, A.; Anton-Rodrigo, I.; Zambom-Ferraresi, F.; Sáez de Asteasu, M.L.; Martinez-Velilla, N.; Elexpuru-Estomba, J.; Marin-Epelde, I.; Ramon-Espinoza, F.; Petidier-Torregrosa, R.; Sanchez-Sanchez, J.L. Effect of a multicomponent exercise programme (VIVIFRAIL) on functional capacity in frail community elders with cognitive decline: Study protocol for a randomized multicentre control trial. Trials 2019, 20, 1–12. [Google Scholar] [CrossRef] [PubMed]
- American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013. [Google Scholar]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Nash, K.C. The effects of exercise on strength and physical performance in frail older people: A systematic review. Rev. Clin. Gerontol. 2012, 22, 274–285. [Google Scholar] [CrossRef]
- de Labra, C.; Guimaraes-Pinheiro, C.; Maseda, A.; Lorenzo, T.; Millán-Calenti, J.C. Effects of physical exercise interventions in frail older adults: A systematic review of randomized controlled trials. BMC Geriatr. 2015, 15, 154. [Google Scholar] [CrossRef]
- Gaedtke, A.; Morat, T. TRX suspension training: A new functional training approach for older adults–development, training control and feasibility. Int. J. Exerc. Sci. 2015, 8, 224. [Google Scholar]
- Kang, H.; Jung, J.; Yu, J. Comparison of trunk muscle activity during bridging exercises using a sling in patients with low back pain. J. Sports Sci. Med. 2012, 11, 510. [Google Scholar]
- Kim, J.H.; Kim, Y.E.; Bae, S.H.; Kim, K.Y. The effect of the neurac sling exercise on postural balance adjustment and muscular response patterns in chronic low back pain patients. J. Phys. Ther. Sci. 2013, 25, 1015–1019. [Google Scholar] [CrossRef] [PubMed]
- Essam-Eldeen, R.M. Influence of sling exercises (TRX) on certain physical variables and performance level of high jump for female college students. Ovidius Univ. Ann. Ser. Phys. Educ. Sport/Sci. Mov. Health 2017, 17, 59–66. [Google Scholar]
- Mohamed, T.S. Effect of Trx Suspension Training as a Prevention Program to Avoid the Shoulder Pain for Swimmers. Ovidius Univ. Ann. Ser. Phys. Educ. Sport/Sci. Mov. Health 2016, 16, 222–227. [Google Scholar]
- Aslani, M.; Minoonejad, H.; Rajabi, R. Comparing the effect of trx exercise and hoping on balance in male university student athletes. Phys. Treat.-Specif. Phys. Ther. J. 2018, 7, 241–250. [Google Scholar] [CrossRef]
- Bae, C.-H.; Jung, Y.-W.; Lee, D.-W.; Cho, S.-H. The effect of sling exercise on muscular strength and range of motion in female patients who received total knee replacement. 한국산학기술학회 논문지 2014, 15, 4395–4403. [Google Scholar]
- Elley, C.R.; Kerse, N.; Chondros, P. Randomised trials-cluster versus individual randomisation: Primary Care Alliance for Clinical Trials (PACT) network. Aust. Fam. Physician 2004, 33, 759–763. [Google Scholar]
- Kelaiditi, E.; Cesari, M.; Canevelli, M.; Abellan van Kan, G.; Ousset, P.-J.; Gillette-Guyonnet, S.; Ritz, P.; Duveau, F.; Soto, M.; Provencher, V. Cognitive frailty: Rational and definition from an (IANA/IAGG) international consensus group. J. Nutr. Health Aging 2013, 17, 726–734. [Google Scholar] [CrossRef]
- Pao, H.-P. The Influence of Emotional Health Status by Healthy Dietary and Exercise Behaviors among Family Medicine Outpatient of Middle-Aged Patients; National Taipei University of Nursing and Health Sciences: Taipei City, Taiwan, 2011. [Google Scholar]
- Lin, C.-H.; Liu, C.-Y.; Rong, J.-R. Psychometric properties of the Taiwanese version of the Tilburg frailty indicator for community-dwelling older adults. Healthcare 2021, 9, 1193. [Google Scholar] [CrossRef]
- Bhattacharya, P.K.; Deka, K.; Roy, A. Assessment of inter-rater variability of the Senior Fitness Test in the geriatric population: A community based study. Int. J. Biomed. Adv. Res. 2016, 7, 208–212. [Google Scholar] [CrossRef]
- Różańska-Kirschke, A.; Kocur, P.; Wilk, M.; Dylewicz, P. The Fullerton Fitness Test as an index of fitness in the elderly. Med. Rehabil. 2006, 10, 15–19. [Google Scholar]
- Rikli, R.E.; Jones, C.J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.-D.; Quach, B.; Chung, P.-K. Further understanding of the Senior Fitness Test: Evidence from community-dwelling high function older adults in Hong Kong. Arch. Gerontol. Geriatr. 2019, 82, 286–292. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, X.; Zhu, Y.; Tao, J.; Zhang, Z.; Zhang, Y.; Wang, Y.; Ke, Y.; Ren, C.; Xu, J. Predictive value of nutritional risk screening 2002 and mini nutritional assessment short form in mortality in Chinese hospitalized geriatric patients. Clin. Interv. Aging 2020, 15, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.-L.; Courtney, M.D.; Shortridge-Baggett, L.M.; Finlayson, K.; Isenring, E.A. Validity of the malnutrition screening tool for older adults at high risk of hospital readmission. J. Gerontol. Nurs. 2012, 38, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Gulmez, I. Effects of angle variations in suspension push-up exercise. J. Strength Cond. Res. 2017, 31, 1017–1023. [Google Scholar] [CrossRef] [PubMed]
- Williams, N. The Borg rating of perceived exertion (RPE) scale. Occup. Med. 2017, 67, 404–405. [Google Scholar] [CrossRef]
- Dawes, J. Complete Guide to TRX Suspension Training; Human Kinetics: Champaign, IL, USA, 2017. [Google Scholar]
- Dent, E.; Lien, C.; Lim, W.S.; Wong, W.C.; Wong, C.H.; Ng, T.P.; Woo, J.; Dong, B.; de la Vega, S.; Poi, P.J.H. The Asia-Pacific clinical practice guidelines for the management of frailty. J. Am. Med. Dir. Assoc. 2017, 18, 564–575. [Google Scholar] [CrossRef]
- Wu, S.-Y.; Hsu, L.-L.; Hsu, C.-C.; Hsieh, T.-J.; Su, S.-C.; Peng, Y.-W.; Guo, T.-M.; Kang, Y.-W.; Pan, W.-H. Dietary education with customised dishware and food supplements can reduce frailty and improve mental well-being in elderly people: A single-blind randomized controlled study. Asia Pac. J. Clin. Nutr. 2018, 27, 1018–1030. [Google Scholar]
- Liang, K.-Y.; Zeger, S.L. Regression analysis for correlated data. Annu. Rev. Public Health 1993, 14, 43–68. [Google Scholar] [CrossRef]
- Stillman, S. Review of generalized estimating equations by Hardin and Hilbe. Stata J. 2003, 3, 208–210. [Google Scholar] [CrossRef]
- Bell, M.L.; Fiero, M.; Horton, N.J.; Hsu, C.-H. Handling missing data in RCTs; a review of the top medical journals. BMC Med. Res. Methodol. 2014, 14, 118. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wu, J.; Wang, X.; Zheng, G. Baduanjin exercise for balance function in community-dwelling older adults with cognitive frailty: A randomized controlled trial protocol. BMC Complement. Med. Ther. 2022, 22, 295. [Google Scholar] [CrossRef] [PubMed]
- Kasim, N.F.; van Zanten, J.V.; Aldred, S. Tai Chi is an effective form of exercise to reduce markers of frailty in older age. Exp. Gerontol. 2020, 135, 110925. [Google Scholar] [CrossRef] [PubMed]
- Fiatarone, M.A.; O’Neill, E.F.; Ryan, N.D.; Clements, K.M.; Solares, G.R.; Nelson, M.E.; Roberts, S.B.; Kehayias, J.J.; Lipsitz, L.A.; Evans, W.J. Exercise training and nutritional supplementation for physical frailty in very elderly people. N. Engl. J. Med. 1994, 330, 1769–1775. [Google Scholar] [CrossRef]
- Fayazmilani, R.; Abbasi, A.; Hovanloo, F.; Rostami, S. The effect of TRX and bodyweight training on physical fitness and body composition in prepubescent soccer athletes. Sport Sci. Health 2022, 18, 1369–1377. [Google Scholar] [CrossRef]
- Dolati, M.; Ghazalian, F.; Abednatanzi, H. The effect of a period of TRX training on lipid profile and body composition in overweight women. Int. J. Sport. Sci. 2017, 7, 151–158. [Google Scholar]
- Smith, L.E.; Snow, J.; Fargo, J.S.; Buchanan, C.A.; Dalleck, L.C. The acute and chronic health benefits of TRX Suspension Training® in healthy adults. Int. J. Res. Exerc. Physiol. 2016, 11, 1–15. [Google Scholar]
- Izquierdo, M.; Rodriguez-Mañas, L.; Casas-Herrero, A.; Martinez-Velilla, N.; Cadore, E.L.; Sinclair, A.J. Is it ethical not to prescribe physical activity for the elderly frail? J. Am. Med. Dir. Assoc. 2016, 17, 779–781. [Google Scholar] [CrossRef]
- Fleg, J.L. Aerobic exercise in the elderly: A key to successful aging. Discov. Med. 2012, 13, 223–228. [Google Scholar] [PubMed]
- McDermott, A.Y.; Mernitz, H. Exercise and older patients: Prescribing guidelines. Am. Fam. Physician 2006, 74, 437–444. [Google Scholar] [PubMed]
| Outcome/Variable | Scale | Baseline (T0) | Immediately Post Intervention (T1) | 3 Months Post Intervention (T2) |
|---|---|---|---|---|
| Descriptive variables | Demographic variables and Chronic Disease and Health Problems Scale | X | ||
| Frailty | Tilburg frailty indicator (TFI-T) | X | X | X |
| Health function (1) Physical function | Senior Fitness Test (SFT) | |||
| Chair sit-and-reach test | X | X | X | |
| Back scratch test | X | X | X | |
| Chair stand test | X | X | X | |
| The Biceps Curl Test | X | X | X | |
| 8-foot up-and-go test | X | X | X | |
| 2 min step test | X | X | X | |
| (2) Nutrition | Mini Nutritional Assessment-Short Form (MNA-SF) | X | X | X |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-H.; Liu, M.-Y.; Chen, N.-F. Frailty Prevention Care Management Program (FPCMP) on Frailty and Health Function in Community-Dwelling Older Adults: A Quasi-Experimental Trial Protocol. Healthcare 2023, 11, 3188. https://doi.org/10.3390/healthcare11243188
Lin C-H, Liu M-Y, Chen N-F. Frailty Prevention Care Management Program (FPCMP) on Frailty and Health Function in Community-Dwelling Older Adults: A Quasi-Experimental Trial Protocol. Healthcare. 2023; 11(24):3188. https://doi.org/10.3390/healthcare11243188
Chicago/Turabian StyleLin, Chia-Hui, Ming-Yi Liu, and Nan-Fu Chen. 2023. "Frailty Prevention Care Management Program (FPCMP) on Frailty and Health Function in Community-Dwelling Older Adults: A Quasi-Experimental Trial Protocol" Healthcare 11, no. 24: 3188. https://doi.org/10.3390/healthcare11243188





