Fatal Case of a Child Harboring Enterobius vermicularis
Abstract
1. Introduction
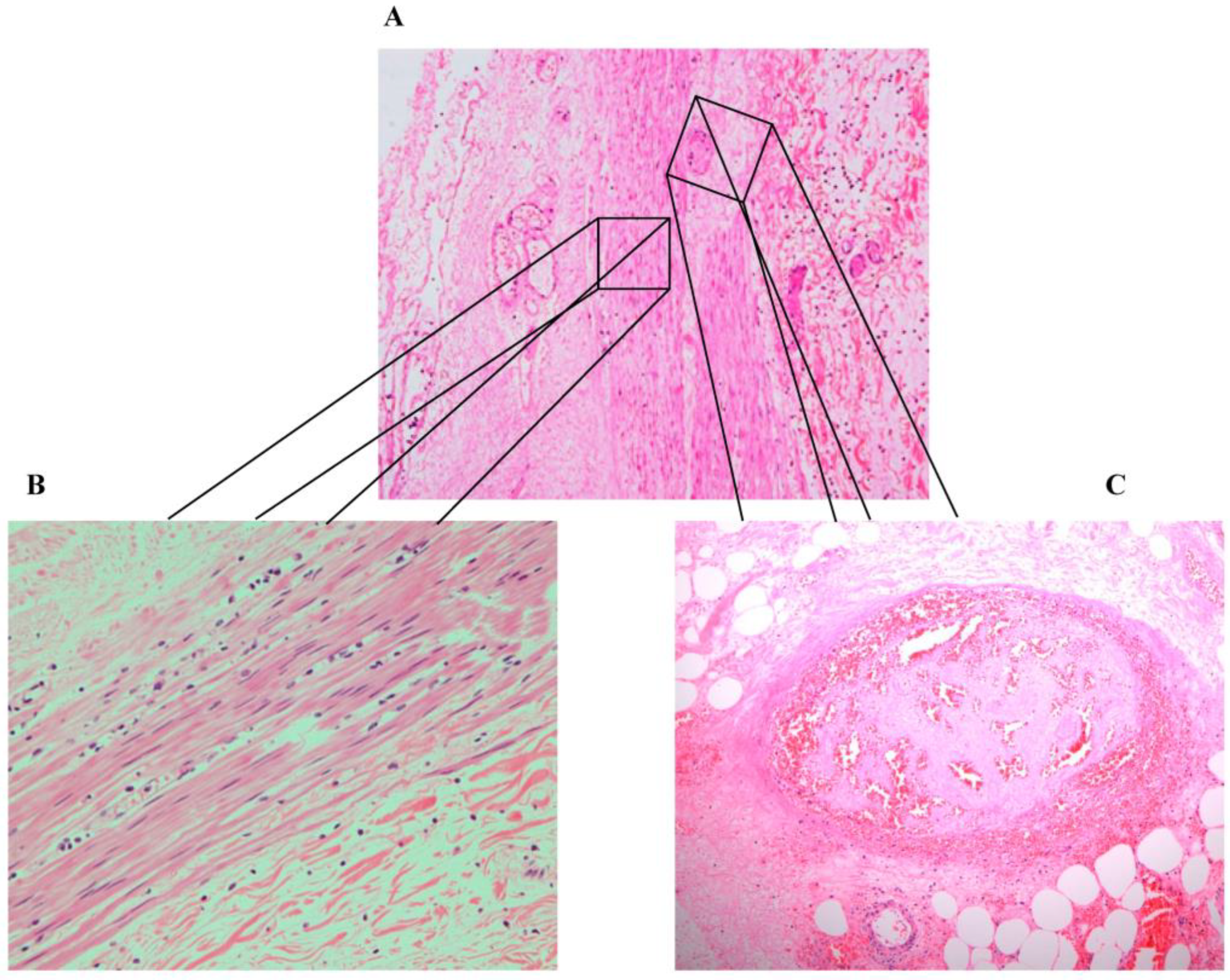
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Neva, F.A.; Brown, H.W. Basic Clinical Parasitology, 6th ed.; McGraw-Hill Education/Medical: New York, NY, USA, 1994. [Google Scholar]
- Lamps, L.W. Surgical Pathology of the Gastrointestinal System: Bacterial, Fungal, Viral, and Parasitic Infections, 1st ed.; Springer: New York, NY, USA, 2010. [Google Scholar]
- Wendt, S.; Trawinski, H.; Schubert, S.; Rodloff, A.C.; Mössner, J.; Lübbert, C. The Diagnosis and Treatment of Pinworm Infection. Dtsch. Arztebl. Int. 2019, 116, 213–219. [Google Scholar] [CrossRef]
- Stĕrba, J.; Vlcek, M.; Noll, P.; Vorel, F. Contribution to the question of relationships between Enterobius vermicularis (L.) and inflammatory processes in the appendix. Folia Parasitol. 1985, 32, 231–235. [Google Scholar]
- Kucik, C.J.; Martin, G.L.; Sortor, B.V. Common intestinal parasites. Am. Fam. Physician 2004, 69, 1161–1168. [Google Scholar]
- Arkoulis, N.; Zerbinis, H.; Simatos, G.; Nisiotis, A. Enterobius vermicularis (pinworm) infection of the liver mimicking malignancy: Presentation of a new case and review of current literature. Int. J. Surg. Case Rep. 2012, 3, 6–9. [Google Scholar] [CrossRef]
- Isik, B.; Yilmaz, M.; Karadag, N.; Kahraman, L.; Sogutlu, G.; Yilmaz, S.; Kirimlioglu, V. Appendiceal Enterobius vermicularis infestation in adults. Int. Surg. 2007, 92, 221–225. [Google Scholar]
- Zahariou, A.; Karamouti, M.; Papaioannou, P. Enterobius vermicularis in the male urinary tract: A case report. J. Med. Case Rep. 2007, 1, 137. [Google Scholar] [CrossRef]
- Sammour, Z.M.; Gomes, C.M.; Tome, A.L.; Bruschini, H.; Srougi, M. Prolonged irritative voiding symptoms due to Enterobius vermicularis bladder infestation in an adult patient. Braz. J. Infect. Dis. Off. Publ. Braz. Soc. Infect. Dis. 2008, 12, 352. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cateau, E.; Yacoub, M.; Tavilien, C.; Becq-Giraudon, B.; Rodier, M.H. Enterobius vermicularis in the kidney: An unusual location. J. Med. Microbiol. 2010, 59, 860–861. [Google Scholar] [CrossRef] [PubMed]
- Dick, L.; Hannay, J. Enterobius vermicularis presentation during laparoscopic cholecystectomy. J. Surg. Case Rep. 2017, 2017, rjw239. [Google Scholar] [CrossRef]
- Ngui, R.; Ravindran, S.; Ong, D.B.; Chow, T.K.; Low, K.P.; Nureena, Z.S.; Rajoo, Y.; Chin, Y.T.; Amir, A.; Ahmad, A.F.; et al. Enterobius vermicularis salpingitis seen in the setting of ectopic pregnancy in a Malaysian patient. J. Clin. Microbiol. 2014, 52, 3468–3470. [Google Scholar] [CrossRef][Green Version]
- Mentessidou, A.; Theocharides, C.; Patoulias, I.; Panteli, C. Enterobius vermicularis-Associated Pelvic Inflammatory Disease in a Child. J. Pediatr. Adolesc. Gynecol. 2016, 29, e25–e27. [Google Scholar] [CrossRef] [PubMed]
- Babady, N.E.; Awender, E.; Geller, R.; Miller, T.; Scheetz, G.; Arguello, H.; Weisenberg, S.A.; Pritt, B. Enterobius vermicularis in a 14-year-old girl’s eye. J. Clin. Microbiol. 2011, 49, 4369–4370. [Google Scholar] [CrossRef] [PubMed]
- Hammood, Z.D.; Salih, A.M.; Mohammed, S.H.; Kakamad, F.H.; Salih, K.M.; Omar, D.A.; Hassan, M.N.; Sidiq, S.H.; Mustafa, M.Q.; Habibullah, I.J.; et al. Enterobius vermicularis causing acute appendicitis, a case report with literature review. Int. J. Surg. Case Rep. 2019, 63, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Taghipour, A.; Olfatifar, M.; Javanmard, E.; Norouzi, M.; Mirjalali, H.; Zali, M.R. The neglected role of Enterobius vermicularis in appendicitis: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0232143. [Google Scholar] [CrossRef]
- Efared, B.; Atsame-Ebang, G.; Soumana, B.M.; Tahiri, L.; Hammas, N.; El Fatemi, H.; Chbani, L. Acute suppurative appendicitis associated with Enterobius vermicularis: An incidental finding or a causative agent? A case report. BMC Res. Notes 2017, 10, 494. [Google Scholar] [CrossRef]
- Rajendran, S.; Carmody, E.; Murphy, M.; Barry, B. Enterobius granulomas as a cause of abdominal pain. BMJ Case Rep. 2015, 2015, bcr2015210464. [Google Scholar] [CrossRef]
- Mansueto, G.; De Simone, M.; Ciamarra, P.; Capasso, E.; Feola, A.; Campobasso, C.P. Infections Are a Very Dangerous Affair: Enterobiasis and Death. Healthcare 2021, 9, 1641. [Google Scholar] [CrossRef]
- Mendos, A.; Mathison, B.A.; Pritt, B.S.; Lamps, L.W.; Pai, S.A. Intramural Ova of Enterobius vermicularis in the Appendix—An Egg-Topic Location! Int. J. Surg. Pathol. 2022, 30, 214–216. [Google Scholar] [CrossRef]
- Harumatsu, T.; Baba, T.; Orokawa, T.; Sunagawa, H.; Ieiri, S. A rare case of acute appendicitis with Enterobius vermicularis. Pediatr. Int. 2022, 64, e15195. [Google Scholar] [CrossRef]
- Liu, L.X.; Chi, J.; Upton, M.P.; Ash, L.R. Eosinophilic colitis associated with larvae of the pinworm Enterobius vermicularis. Lancet 1995, 346, 410–412. [Google Scholar] [CrossRef]
- Rajamanickam, A.; Usmani, A.; Suri, S.; Dimov, V. Chronic diarrhea and abdominal pain: Pin the pinworm. J. Hosp. Med. 2009, 4, 137–139. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sousa, J.; Hawkins, R.; Shenoy, A.; Petroze, R.T.; Mustafa, M.M.; Taylor, J.A.; Larson, S.D.; Islam, S. Enterobius vermicularis-associated appendicitis: A 22-year case series and comprehensive review of the literature. J. Pediatr. Surg. 2021, 57, 1494–1498. [Google Scholar] [CrossRef] [PubMed]
- Hamdona, S.M.; Lubbad, A.M.; Al-Hindi, A.I. Histopathological study of Enterobius vermicularis among appendicitis patients in Gaza strip, Palestine. J. Parasit. Dis. Off. Organ Indian Soc. Parasitol. 2016, 40, 176–183. [Google Scholar] [CrossRef]
- Ames, P.R.; Aloj, G.; Gentile, F. Eosinophilia and thrombosis in parasitic diseases: An overview. Clin. Appl. Thromb. Hemost. Off. J. Int. Acad. Clin. Appl. Thromb. Hemost. 2011, 17, 33–38. [Google Scholar] [CrossRef]
- Moxon, C.A.; Alhamdi, Y.; Storm, J.; Toh, J.M.H.; McGuinness, D.; Ko, J.Y.; Murphy, G.; Lane, S.; Taylor, T.E.; Seydel, K.B.; et al. Parasite histones are toxic to brain endothelium and link blood barrier breakdown and thrombosis in cerebral malaria. Blood Adv. 2020, 4, 2851–2864. [Google Scholar] [CrossRef] [PubMed]
- Waters, M.; Krajden, S.; Kim, C.; Elsobky, R.; Lychacz, B.; Cheung, M.; Crowther, M.; Keystone, J. Case Report: Two Cases of Strongyloidiasis Presenting with Thrombotic Events. Am. J. Trop. Med. Hyg. 2019, 101, 418–421. [Google Scholar] [CrossRef]
- Nowak, S.P.; Pielok, Ł.; Stefaniak, J. Thrombosis of inferior vena cava in the course of advanced alveolar echinococcosis. Pol. Arch. Intern. Med. 2019, 129, 204–205. [Google Scholar] [CrossRef]
- Ozsay, O.; Gungor, F.; Karaisli, S.; Kokulu, I.; Dilek, O.N. Hydatid cyst of the pancreas causing both acute pancreatitis and splenic vein thrombosis. Ann. R. Coll. Surg. Engl. 2018, 100, e178–e180. [Google Scholar] [CrossRef]
- Kaur, J.; Gupta, A.; Wadhwa, N. Hepatic Visceral Larva Migrans Causing Hepatic Venous Thrombosis and Prolonged Fever. Indian Pediatr. 2017, 54, 882–884. [Google Scholar] [CrossRef]
- Takeda, A.; Hayashi, S.; Teranishi, Y.; Imoto, S.; Nakamura, H. Portomesenteric Vein Thrombosis After Excision of Parasitic Peritoneal Myomas. J. Minim. Invasive Gynecol. 2017, 24, 501–505. [Google Scholar] [CrossRef]
- Mosli, M.H.; Chan, W.W.; Morava-Protzner, I.; Kuhn, S.M. Schistosomiasis Presenting as a Case of Acute Appendicitis with Chronic Mesenteric Thrombosis. Can. J. Infect. Dis. Med. Microbiol. 2016, 2016, 5863219. [Google Scholar] [CrossRef] [PubMed]
- Leite, L.A.C.; de Cássia dos Santos Ferreira, R.; Hatzlhofer, B.L.D.; Correia, M.C.B.; Bandeira, Â.P.; Owen, J.S.; Lima, V.; Domingues, A.L.C.; Lopes, E. Portal vein thrombosis associated with protein C deficiency and elevated Factor VIII in hepatosplenic schistosomiasis. Blood Coagul. Fibrinolysis Int. J. Haemost. Thromb. 2016, 27, 210–212. [Google Scholar] [CrossRef] [PubMed]
- Abo-Salem, E.S.; Ramadan, M.M. A huge thrombosed pulmonary artery aneurysm without pulmonary hypertension in a patient with hepatosplenic schistosomiasis. Am. J. Case Rep. 2015, 16, 140–145. [Google Scholar] [PubMed]
- Singla, N.; Gupta, M.; Singh, R.; Kumar, A. Atypical neurological manifestations of malaria. BMJ Case Rep. 2014, 2014, bcr2014204807. [Google Scholar] [CrossRef] [PubMed]
- Olveda, D.U.; Olveda, R.M.; Montes, C.J.; Chy, D.; Abellera, J.M.B., III; Cuajunco, D.; Lam, A.K.; McManus, D.P.; Li, Y.; Ross, A.G.P. Clinical management of advanced schistosomiasis: A case of portal vein thrombosis-induced splenomegaly requiring surgery. BMJ Case Rep. 2014, 2014, bcr2014203897. [Google Scholar] [CrossRef]
- Patsantara, G.G.; Piperaki, E.T.; Tzoumaka-Bakoula, C.; Kanariou, M.G. Immune responses in children infected with the pinworm Enterobius vermicularis in central Greece. J. Helminthol. 2016, 90, 337–341. [Google Scholar] [CrossRef]



| Location of Enterobius vermicularis Infection | Age, Gender, Country of Origin | Therapy | Outcome | Ref |
|---|---|---|---|---|
| Urinary tract | 65-year-old male from Greece | Mebendazole 100 mgs for 3 days followed by two more courses with 3 week time interval. | Complete resolution of symptoms. | [8] |
| Bladder | 54-year-old female from Brazil | Mebendazole 200 mgs for 3 days. | Complete resolution of the voiding symptoms and normalization of urinalysis. | [9] |
| Kidney | 51-year-old female from France | Nephrectomy and amoxicillin; gentamicin. | Complete resolution of symptoms. | [10] |
| Biliary tree | 73-year-old female from UK | Laparoscopic cholecystectomy with intra-operative cholangiogram | Recovered after surgery. | [11] |
| Fallopian tube | 23-year-old female from Malaysia | Laparotomy with a right salpingo-oophorectomy. Albendazole for a week upon discharge. | Recovered after surgery. | [12] |
| Pelvis | 11-year-old female from Greece | Laparotomy was performed. Intravenous cefoxitin, amikacin, and metronidazole postoperatively. | Recovered after Surgery. | [13] |
| Nares and ocular orbit | 14-year-old female from the United States | Mebendazole 300 mg twice daily for 3 days. | Complete resolution of symptoms. | [14] |
| Blood Cell Count | Patient’s Results | Reference Range |
|---|---|---|
| Total white blood cell | 1.1 × 109/L | 4.5–11.0 × 109/L |
| Lymphocytes | 1.5–4.0 × 109/L | |
| Neutrophils | 2–7.5 × 109/L | |
| Eosinophils | 0.1 × 109/L | 0.0–0.4 × 109/L |
| Monocytes | 0.2–1.0 × 109/L | |
| Basophils | 0.0–0.5 × 109/L |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Shouli, S.T.; Barry, M.; Binkhamis, K.; AlHogail, N.; Alafaleq, N.O.; Dufailu, O.A.; Aljerian, K. Fatal Case of a Child Harboring Enterobius vermicularis. Healthcare 2023, 11, 917. https://doi.org/10.3390/healthcare11060917
Al-Shouli ST, Barry M, Binkhamis K, AlHogail N, Alafaleq NO, Dufailu OA, Aljerian K. Fatal Case of a Child Harboring Enterobius vermicularis. Healthcare. 2023; 11(6):917. https://doi.org/10.3390/healthcare11060917
Chicago/Turabian StyleAl-Shouli, Samia T., Mazin Barry, Khalifa Binkhamis, Nourah AlHogail, Nouf Omar Alafaleq, Osman Adamu Dufailu, and Khaldoon Aljerian. 2023. "Fatal Case of a Child Harboring Enterobius vermicularis" Healthcare 11, no. 6: 917. https://doi.org/10.3390/healthcare11060917
APA StyleAl-Shouli, S. T., Barry, M., Binkhamis, K., AlHogail, N., Alafaleq, N. O., Dufailu, O. A., & Aljerian, K. (2023). Fatal Case of a Child Harboring Enterobius vermicularis. Healthcare, 11(6), 917. https://doi.org/10.3390/healthcare11060917







