Nonlinear Associations between Medical Expenditure, Perceived Medical Attitude, and Sociodemographics, and Older Adults’ Self-Rated Health in China: Applying the Extreme Gradient Boosting Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Description
2.2. Data Acquisition
2.3. Variables Definition
2.3.1. Outcome
2.3.2. Medical Expenditure and Perceived Medical Attitudes
2.3.3. Related Health Risk Factors and Sociodemographic Characteristics
2.4. The Extreme Gradient Boosting Model
2.5. Model Evaluation
3. Results
3.1. Importance of Various Factors on Older Adult’s Self-Rated Health
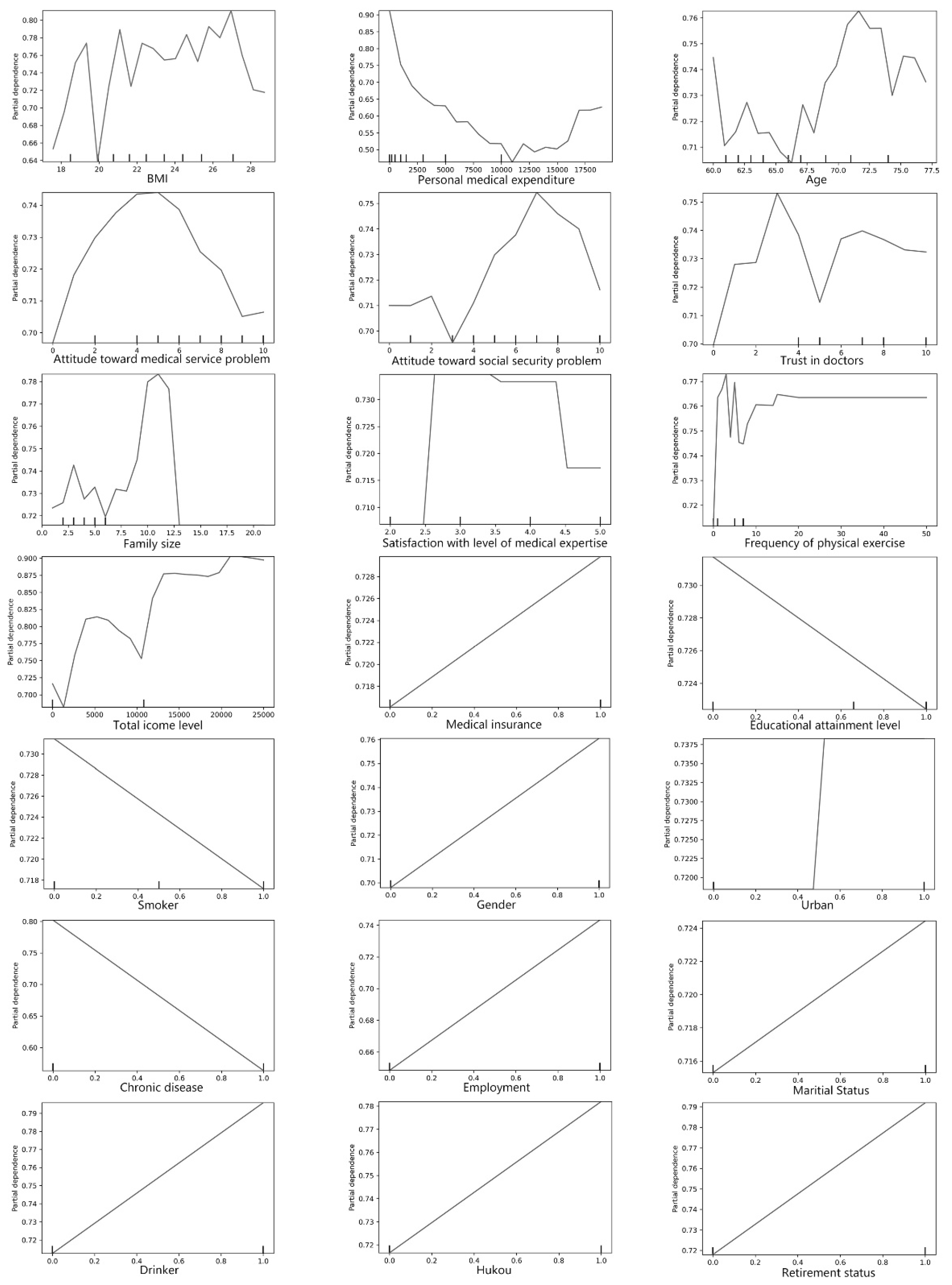
3.2. Association between Factors and Older Adults’ Self-Rated Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Ageing and Health in China. Available online: https://www.who.int/china/health-topics/ageing (accessed on 19 March 2021).
- Fang, P. Greenbook of Health Reform and Development: Report on the Development of China’s Medical and Health Services in 2014; People’s Publishing House: Beijing, China, 2015. [Google Scholar]
- Friedman, E. Money isn’t everything: Nonfinancial barriers to access. JAMA 1994, 271, 1535–1538. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Jiang, Y.; Li, Y.; Zhang, Y.; Wang, X.; Ma, S.; Wang, Y. Medical expenditure for middle-aged and elderly in Beijing. BMC Health Serv. Res. 2019, 19, 360. [Google Scholar] [CrossRef]
- Choi, J.-W.; Choi, J.-W.; Kim, J.-H.; Yoo, K.-B.; Park, E.-C. Association between chronic disease and catastrophic health expenditure in Korea. BMC Health Serv. Res. 2015, 15, 26. [Google Scholar] [CrossRef] [PubMed]
- Sheng, B.; Feng, C.; Zhang, D.; Spitler, H.; Shi, L. Associations between obesity and spinal diseases: A medical expenditure panel study analysis. Int. J. Environ. Res. Public Health 2017, 14, 183. [Google Scholar] [CrossRef]
- Xia, K.; Wang, L.-F.; Yang, X.-C.; Jiang, H.-Y.; Zhang, L.-J.; Yao, D.-K.; Hu, D.-Y.; Ding, R.-J. Comparing the effects of depression, anxiety, and comorbidity on quality-of-life, adverse outcomes, and medical expenditure in Chinese patients with acute coronary syndrome. Chin. Med. J. 2019, 132, 1045. [Google Scholar] [CrossRef]
- Abdulraheem, b.I.; Olapipo, A.; Amodu, M. Primary health care services in Nigeria: Critical issues and strategies for enhancing the use by the rural communities. J. Public Health Epidemiol. 2012, 4, 5–13. [Google Scholar] [CrossRef]
- Iezzoni, L.I.; Killeen, M.B.; O’Day, B.L. Rural residents with disabilities confront substantial barriers to obtaining primary care. Health Serv. Res. 2006, 41, 1258–1275. [Google Scholar] [CrossRef]
- Alazri, M.; Neal, R. The association between satisfaction with services provided in primary care and outcomes in Type 2 diabetes mellitus. Diabet. Med. 2003, 20, 486–490. [Google Scholar] [CrossRef]
- Kavalnienė, R.; Deksnyte, A.; Kasiulevičius, V.; Šapoka, V.; Aranauskas, R.; Aranauskas, L. Patient satisfaction with primary healthcare services: Are there any links with patients’ symptoms of anxiety and depression? BMC Fam. Pract. 2018, 19, 90. [Google Scholar] [CrossRef]
- Klest, B.; Tamaian, A.; Boughner, E. A model exploring the relationship between betrayal trauma and health: The roles of mental health, attachment, trust in healthcare systems, and nonadherence to treatment. Psychol. Trauma Theory Res. Pract. Policy 2019, 11, 656. [Google Scholar] [CrossRef]
- Netemeyer, R.G.; Dobolyi, D.G.; Abbasi, A.; Clifford, G.; Taylor, H. Health literacy, health numeracy, and Trust in Doctor: Effects on key patient health outcomes. J. Consum. Aff. 2020, 54, 3–42. [Google Scholar] [CrossRef]
- Blödt, S.; Müller-Nordhorn, J.; Seifert, G.; Holmberg, C. Trust, medical expertise and humaneness: A qualitative study on people with cancer’satisfaction with medical care. Health Expect. 2021, 24, 317–326. [Google Scholar] [CrossRef]
- Crawford, R. Risk ritual and the management of control and anxiety in medical culture. Health 2004, 8, 505–528. [Google Scholar] [CrossRef] [PubMed]
- Hämäläinen, J.; Isometsä, E.; Sihvo, S.; Pirkola, S.; Kiviruusu, O. Use of health services for major depressive and anxiety disorders in Finland. Depress. Anxiety 2008, 25, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Liebman, B.L. Malpractice mobs: Medical dispute resolution in China. Columbia Law Rev. 2013, 113, 181–264. [Google Scholar]
- Bora, J.K.; Saikia, N. Gender differentials in self-rated health and self-reported disability among adults in India. PLoS ONE 2015, 10, e0141953. [Google Scholar] [CrossRef] [PubMed]
- Moss, N.E. Gender equity and socioeconomic inequality: A framework for the patterning of women’s health. Soc. Sci. Med. 2002, 54, 649–661. [Google Scholar] [CrossRef]
- Leinonen, R.; Heikkinen, E.; Jylhä, M. Self-rated health and self-assessed change in health in elderly men and women—A five-year longitudinal study. Soc. Sci. Med. 1998, 46, 591–597. [Google Scholar] [CrossRef]
- Pinillos-Franco, S.; García-Prieto, C. The gender gap in self-rated health and education in Spain. A multilevel analysis. PLoS ONE 2017, 12, e0187823. [Google Scholar] [CrossRef]
- Mizuochi, M. Effect of Retirement Timing on Health. In Exploring the Effect of Retirement on Health in Japan; Springer: Berlin/Heidelberg, Germany, 2021; pp. 73–93. [Google Scholar]
- Zavras, D.; Tsiantou, V.; Pavi, E.; Mylona, K.; Kyriopoulos, J. Impact of economic crisis and other demographic and socio-economic factors on self-rated health in Greece. Eur. J. Public Health 2013, 23, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Burström, B.; Chen, J.; Burström, K. Rural-urban inequalities in poor self-rated health, functional disabilities and depression among Chinese older adults: Evidence from the China Health and Retirement Longitudinal Study 2011 and 2015. Res. Sq. 2020, preprint. [Google Scholar] [CrossRef]
- Chen, J. Internal migration and health: Re-examining the healthy migrant phenomenon in China. Soc. Sci. Med. 2011, 72, 1294–1301. [Google Scholar] [CrossRef] [PubMed]
- Abu-Omar, K.; Rütten, A.; Robine, J.-M. Self-rated health and physical activity in the European Union. Soz. -Und Präventivmedizin/Soc. Prev. Med. 2004, 49, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.P.; Ho, S.Y.; Lo, W.S.; Lai, M.K.; Lam, T.H. Smoking is associated with poor self-rated health among adolescents in Hong Kong. Nicotine Tob. Res. 2012, 14, 682–687. [Google Scholar] [CrossRef] [PubMed]
- Frisher, M.; Mendonça, M.; Shelton, N.; Pikhart, H.; de Oliveira, C.; Holdsworth, C. Is alcohol consumption in older adults associated with poor self-rated health? Cross-sectional and longitudinal analyses from the English Longitudinal Study of Ageing. BMC Public Health 2015, 15, 703. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Okosun, I.S.; Choi, S.; Matamoros, T.; Dever, G.A. Obesity is associated with reduced self-rated general health status: Evidence from a representative sample of white, black, and Hispanic Americans. Prev. Med. 2001, 32, 429–436. [Google Scholar] [CrossRef]
- Bardage, C.; Pluijm, S.M.; Pedersen, N.L.; Deeg, D.J.; Jylhä, M.; Noale, M.; Blumstein, T.; Otero, Á. Self-rated health among older adults: A cross-national comparison. Eur. J. Ageing 2005, 2, 149–158. [Google Scholar] [CrossRef]
- Franks, P.; Gold, M.R.; Fiscella, K. Sociodemographics, self-rated health, and mortality in the US. Soc. Sci. Med. 2003, 56, 2505–2514. [Google Scholar] [CrossRef]
- Liu, Z. Institution and inequality: The hukou system in China. J. Comp. Econ. 2005, 33, 133–157. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. Xgboost: A scalable tree boosting system. In Proceedings of Proceedings of the 22nd Acm Sigkdd International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Wang, L.; Zhao, C.; Liu, X.; Chen, X.; Li, C.; Wang, T.; Wu, J.; Zhang, Y. Non-linear effects of the built environment and social environment on bus use among older adults in china: An application of the xgboost model. Int. J. Environ. Res. Public Health 2021, 18, 9592. [Google Scholar] [CrossRef]
- Wang, W.; Zhang, Y.; Zhao, C.; Liu, X.; Chen, X.; Li, C.; Wang, T.; Wu, J.; Wang, L. Nonlinear Associations of the Built Environment with Cycling Frequency among Older Adults in Zhongshan, China. Int. J. Environ. Res. Public Health 2021, 18, 10723. [Google Scholar] [CrossRef]
- Minagawa, Y.; Saito, Y. The role of underweight in active life expectancy among older adults in Japan. J. Gerontol. Ser. B 2021, 76, 756–765. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.Q.; Allebach, J.P. Feature ranking and selection used in a machine learning framework for predicting uniformity of printed pages. Electron. Imaging 2017, 2017, 166–173. [Google Scholar] [CrossRef]
- Lundberg, S.M.; Lee, S.-I. A unified approach to interpreting model predictions. In Proceedings of the 31st International Conference on Neural Information Processing Systems, Long Beach, CA, USA, 4–9 December 2017; pp. 4768–4777. [Google Scholar]
- Friedman, J.H. Greedy function approximation: A gradient boosting machine. Ann. Stat. 2001, 29, 1189–1232. [Google Scholar] [CrossRef]
- Lorem, G.F.; Schirmer, H.; Emaus, N. What is the impact of underweight on self-reported health trajectories and mortality rates: A cohort study. Health Qual. Life Outcomes 2017, 15, 1–14. [Google Scholar] [CrossRef]
- Imai, K.; Gregg, E.W.; Chen, Y.J.; Zhang, P.; De Rekeneire, N.; Williamson, D.F. The association of BMI with functional status and self-rated health in US adults. Obesity 2008, 16, 402–408. [Google Scholar] [CrossRef]
- Xinhua. Over 95% of Chinese Covered by Basic Medical Insurance. Available online: http://english.www.gov.cn/statecouncil/ministries/202006/26/content_WS5ef5b225c6d05a0f897062fb.html (accessed on 5 November 2021).
- Youmans, E.G. Age group, health, and attitudes. Gerontologist 1974, 14, 249–254. [Google Scholar] [CrossRef]
- Morey, M.C.; Sloane, R.; Pieper, C.F.; Peterson, M.J.; Pearson, M.P.; Ekelund, C.C.; Crowley, G.M.; Demark-Wahnefried, W.; Snyder, D.C.; Clipp, E.C. Effect of physical activity guidelines on physical function in older adults. J. Am. Geriatr. Soc. 2008, 56, 1873–1878. [Google Scholar] [CrossRef]
- Warburton, D.E.; Bredin, S.S. Reflections on physical activity and health: What should we recommend? Can. J. Cardiol. 2016, 32, 495–504. [Google Scholar] [CrossRef]
- Warburton, D.E.; Bredin, S.S. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef]
- Gold, M.; Franks, P.; Erickson, P. Assessing the health of the nation: The predictive validity of a preference-based measure and self-rated health. Med. Care 1996, 34, 163–177. [Google Scholar] [CrossRef]
- Molarius, A.; Janson, S. Self-rated health, chronic diseases, and symptoms among middle-aged and elderly men and women. J. Clin. Epidemiol. 2002, 55, 364–370. [Google Scholar] [CrossRef]
- Song, Q.; Smith, J.P. Hukou system, mechanisms, and health stratification across the life course in rural and urban China. Health Place 2019, 58, 102150. [Google Scholar] [CrossRef]
- Lee, J.-A.; Park, J.H.; Kim, M. Social and physical environments and self-rated health in urban and rural communities in Korea. Int. J. Environ. Res. Public Health 2015, 12, 14329–14341. [Google Scholar] [CrossRef]
- Wang, M.; Webber, M.; Finlayson, B.; Barnett, J. Rural industries and water pollution in China. J. Environ. Manag. 2008, 86, 648–659. [Google Scholar] [CrossRef]
- Shi, L. Health care in China: A rural-urban comparison after the socioeconomic reforms. Bull. World Health Organ. 1993, 71, 723. [Google Scholar] [PubMed]
- LeCun, Y.; Boser, B.; Denker, J.; Henderson, D.; Howard, R.; Hubbard, W.; Jackel, L. Handwritten digit recognition with a back-propagation network. Adv. Neural Inf. Process. Syst. 1989, 2, 396–404. [Google Scholar]
- Long, J.; Shelhamer, E.; Darrell, T. Fully convolutional networks for semantic segmentation. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Boston, MA, USA, 7–15 June 2015; pp. 3431–3440. [Google Scholar]
- Zhao, R.; Yan, R.; Wang, J.; Mao, K. Learning to monitor machine health with convolutional bi-directional LSTM networks. Sensors 2017, 17, 273. [Google Scholar] [CrossRef]
| Variable | Definition | Mean | SD |
|---|---|---|---|
| Self-rated health | 1 = Good SRH, 0 = Poor SRH | 0.721 | 0.448 |
| Age (Age > =60) | Continuous variables (years) | 66.657 | 5.241 |
| Gender | 1 = Male, 0 = Female | 0.571 | 0.495 |
| Urban | 1 = Urban residents, 0 = Rural residents | 0.365 | 0.481 |
| Education | 1 = Junior high school and above, 0 = otherwise | 0.701 | 0.458 |
| Income | Total income, continuous variables (yuan) | 3624.729 | 13,664.587 |
| Medical expenditure | Total personal expenditure on medical, continuous variables (yuan) | 4676.916 | 15,681.112 |
| Marital Status | 1 = Married, 0 = otherwise | 0.870 | 0.336 |
| Hukou | 1 = Urban hukou, 0 = non-urban hukou | 0.166 | 0.372 |
| Employment | 1 = employed, 0 = otherwise | 0.777 | 0.416 |
| Smoke | 1 = Current smoker, 0 = non-current smoker | 0.499 | 0.500 |
| Drink | 1 = Current drinker, 0 = non-current drinker | 0.207 | 0.405 |
| Exercise | Frequency of physical exercise, continuous variables (times) | 3.167 | 3.600 |
| Retirement | 1 = retiree, 0 = otherwise | 0.113 | 0.316 |
| Insurance | 1 = respondents had medical insurance, 0 = otherwise | 0.652 | 0.476 |
| Satisfaction with level of medical | The level of medical expertise, Ordinal variable 1 (very bad) to 5 (very good) | 3.610 | 0.914 |
| Chronic | 1 = Had a chronic disease, 0 = no chronic disease | 0.281 | 0.450 |
| Family size | Continuous variables | 3.987 | 2.168 |
| Attitude toward medical service problem | Ordinal variable, (0) no problem to (10) extremely serious problem | 5.991 | 2.958 |
| Attitude toward security problem | Ordinal variable, (0) no problem to (10) extremely serious problem | 5.400 | 3.010 |
| Trust in doctors | Ordinal variable, (0) distrustful to (10) very trusting | 7.022 | 2.471 |
| BMI | Continuous variables | 22.832 | 3.605 |
| Predictors | Ranking of Feature Importanceby F-Score | Ranking of Feature Importance by SHAP |
|---|---|---|
| Related health predictors | ||
| BMI | 1 | 3 |
| Chronic disease | 16 | 2 |
| Smoke | 13 | 20 |
| Drink | 19 | 13 |
| Physical exercise | 9 | 7 |
| Medical expenditure and perceived medical attitudes | ||
| Personal medical expenditure | 2 | 1 |
| Attitude toward medical service problem | 4 | 11 |
| Attitude toward social security problem | 5 | 9 |
| Trust in doctors | 6 | 12 |
| Satisfaction with level of medical expertise | 8 | 16 |
| Sociodemographic predictors | ||
| Age | 3 | 6 |
| Gender | 14 | 4 |
| Marital status | 18 | 21 |
| Educational attainment level | 12 | 19 |
| Household total income level | 10 | 5 |
| Family sizes | 7 | 17 |
| Employment status | 17 | 8 |
| Hukou status | 20 | 10 |
| Retirement status | 21 | 15 |
| Insurance | 11 | 18 |
| Urban | 15 | 14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liang, Y.; Zheng, W.; Lee, W.-S. Nonlinear Associations between Medical Expenditure, Perceived Medical Attitude, and Sociodemographics, and Older Adults’ Self-Rated Health in China: Applying the Extreme Gradient Boosting Model. Healthcare 2022, 10, 39. https://doi.org/10.3390/healthcare10010039
Liang Y, Zheng W, Lee W-S. Nonlinear Associations between Medical Expenditure, Perceived Medical Attitude, and Sociodemographics, and Older Adults’ Self-Rated Health in China: Applying the Extreme Gradient Boosting Model. Healthcare. 2022; 10(1):39. https://doi.org/10.3390/healthcare10010039
Chicago/Turabian StyleLiang, Yuqing, Wanwan Zheng, and Woon-Seek Lee. 2022. "Nonlinear Associations between Medical Expenditure, Perceived Medical Attitude, and Sociodemographics, and Older Adults’ Self-Rated Health in China: Applying the Extreme Gradient Boosting Model" Healthcare 10, no. 1: 39. https://doi.org/10.3390/healthcare10010039
APA StyleLiang, Y., Zheng, W., & Lee, W.-S. (2022). Nonlinear Associations between Medical Expenditure, Perceived Medical Attitude, and Sociodemographics, and Older Adults’ Self-Rated Health in China: Applying the Extreme Gradient Boosting Model. Healthcare, 10(1), 39. https://doi.org/10.3390/healthcare10010039





