Abstract
Pneumonia is a common reason for admission afflicting frail older adults. Those who are the frailest are more likely to be provided with a diagnosis of aspiration pneumonia. This diagnosis has no clear definition and no clinical consensus. It is therefore time to stop attempting to differentiate between pneumonia type and use the term frailty-associated pneumonia.
1. Introduction
The population in many countries is ageing, with the fastest growing cohort being very old (>80 years of age), who are projected to make up 12.3% of the world’s population by 2029 [1]. The ideal situation is for people to age well with minimal disability, maintaining functioning independence for as long as possible [2]. However, for many, increasing age is associated with increasing dependency and vulnerability. Geriatric syndromes (or giants) are medical problems that frequently present in older adults. They all have multiple aetiological factors and ultimately lead to physical decline and death. In recent years frailty and dysphagia have been included amongst these geriatric syndromes [3,4].
Pneumonia is a common reason for older people to be admitted to hospital, and the literature suggests that those who are the frailest are more likely to be diagnosed with aspiration pneumonia (AP). This paper has been written not to discuss frailty or sarcopenia, per se, but more so to discuss the interpretation of pneumonia in the context of frailty. We discuss the relationship between pneumonia and frailty and suggest that there should be a change of nomenclature and, rather than trying to differentiate pneumonia “types”, pneumonia in older frail adults should be called frailty-associated pneumonia (FAP).
2. Pneumonia
Pneumonia occurs in people of all age groups and is often classified depending on the frailty of the patient, the place of residence at the time of the infection (community, hospital, or ventilator), or its presumed methodological aetiology (e.g., aspiration) [5].
Increasing age, frailty, smoking, immunosuppression, and comorbid conditions are all risk factors for CAP [6]. The aetiological agents of CAP has varied little over the years with Streptococcus pneumoniae being accepted as most common pathogen; others include Staph Aureus, Legionella pneumophilia, Pseudomonas aeruginosa, and Haemophilus influenzae [6,7] and this has changed little over the years.
Between 2002 and 2017, the incidence of clinically diagnosed pneumonia increased from 1.5/1000 person years to 2.22 per 1000 person years [8], with the prevalence being reported as 6 times higher in those >75 years compared to those <60 years of age [9,10]; 164.3 cases/10,000 adults > 80 years of age accounting for 45% of diagnosed CAP occur in people >65 years of age [11]. Hospital-acquired pneumonia occurs in 5–10/1000 admissions [12]. Pneumonia is not a benign problem. CAP has a mortality rate of 2–5/1000 years [13,14]. In 2016, there were approximately 2.3 million deaths from pneumonia [15] and 2.5 million in 2019 [16]. A total of 3.2 million people die from influenza and pneumonia each year [17].
3. Nutrition
Good nutrition is pivotal to a healthy life. With increasing age, access to high quality food becomes increasingly difficult, not only because of illness but also because of socio-economic factors. Lack of good quality food in the right quantity coupled with anabolic resistance [18,19] can ultimately result in protein and micronutrient undernutrition. The clinical consequences of this can manifest as frailty, sarcopenia, and an ineffective immune system with an increase in morbidity and eventual death [19,20].
4. Frailty and Oral Frailty
Frailty has been classified as a wasting syndrome [21] characterised by weakness and a poor nutritional status [22]. Ferrucci et al. defined frailty as “a physiological syndrome, characterised by decreased reserve and diminished reserve to stressors, resulting from cumulative decline across multiple physiological systems, resulting in multisystem dysregulation and causing vulnerability to adverse outcomes” [23,24].
Fried et al. [21] argued that there is a frailty phenotype presenting with weight loss, exhaustion, low energy expenditure, reduced muscle strength, and slowness in walking [25]. Rockwood, on the other hand, viewed frailty as an accumulation of deficits rather than being a specific phenotype [26]. Many old frail adults have many comorbidities including lung disease, ischaemic heart disease, stroke, dementia, and diabetes.
The prevalence of frailty increases with age, such that one-quarter to one-third of adults >85 years will be frail [27,28] Severity of frailty increases the ability to cope with acute stressors, such as infection [27], and those with severe frailty have a significantly high mortality [26,27]. Hence, a cycle of decline occurs as recovery from any stressor is usually not associated with a return to the previous level of functional ability.
Sarcopenia, which is an intrinsic component of the frailty syndrome [29], not only involves axial muscles but also those involved in chewing (masseter) and swallowing (supra- and infra-hyoid groups of muscles) [30]. Difficulty in chewing has been termed “oral frailty” [31,32].
As people become more dependent on others for personal oral hygiene, there is a deterioration of oral health [32,33,34]. Higher oral bacterial counts are found [35,36], gram negative and anaerobic organisms are increasingly present in the microbiome, and the nature of any infection may change [37]. Studies have shown that, for those most at risk, effective proactive mouth care can mitigate any risk [38,39]. Poor oral health and oral frailty are associated with an increased mortality and morbidity [40].
5. Frailty and Immunity
Over the life span, people have multiple and repeated exposure to environmental toxins, resulting in a proinflammatory milieu as demonstrated by an increased white cell count, CRP, chemokine, and cytokines (inflammageing) [23,41]. This results in the expression of senescence-associated molecules [42], and hence a decreased efficiency of the adaptive and innate immune systems [43] or “immunosenescence” [44] with an impaired immune surveillance, a reduced response to antigens [44,45], and an inability to generate immunoreactive T cells [46].
In the presence of an infection, there is a maladaptive immune response with a reduced proliferation of mononuclear cells, and an attenuated adaptive immune response with an overexpression of inflammatory agents exacerbating the chronic inflammatory state and a cycle of functional decline [6,23,41]. This maladaptive and poorly effective response to infection (Figure 1) not only results in an increased risk of infection but any infection is likely to be more severe and is more likely to result in a decline in function or death [47].
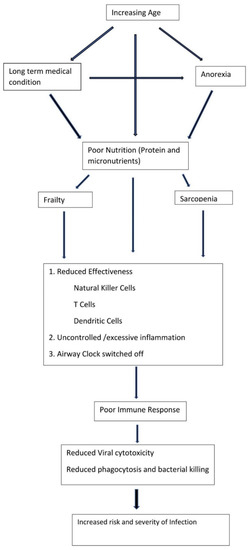
Figure 1.
Mechanism of increased infection risk in older frail adults.
6. Lungs and Immunity
The lungs have their own immunity milieu, which mirrors the systemic immune system, but also includes a resident microbiome [48,49,50,51]. Epithelial cells and alveolar macrophages modulate immunity by production of mucins, cytokines, and tissue necrosis factor [52]. This aspect of lung defence has an internal clock or circadian rhythm, which is important in maintaining the integrity of the lung’s immune response.
The physical defences of the lung include airway patency, a functional mucociliary escalator, and an effective cough. Mucus, produced by goblet cells and submucosal glands (also assisted by Clara cells and tissue fluid transudation) are conveyed into the trachea and larynx by a coordinated wave of ciliary motion of ciliated epithelial cells [53]. This itself can bring mucus up to the oral cavity to be swallowed or spat out.
As people get older and frailer, together with the immunosenescence described earlier, there is a disruption of the airway cell clock or circadian rhythm of mucus production [54], all resulting in an increased susceptibility of older frail adults to endotoxin damage resulting in pneumonia [46,55]. (Figure 1).
The ability to clear the lungs of any organism or foreign body inhaled or aspirated is also impaired. There is a reduction in laryngeal sensation (due to age or neurological disease, resulting in a reduced urge to cough) [44,56] and reduced respiratory muscle strength may result in a reduction in the peak expiratory cough velocity [57,58]. Mucus quality is poor, its immune function degraded, and mucociliary clearance becomes inefficient [59,60,61,62]. Air movement, tidal volume and functional residual capacity are reduced secondary to damaged lung elasticity in association with coexistent lung disease [59,60,61,62]. All of these may result in mucus pooling and increased risk of lung infection.
7. Dysphagia
Dysphagia is a common problem for frail older adults [30,63], with 55% of frail adults reporting problems with swallowing [63]. Issues include fatigue whilst chewing (oral frailty), taking longer to eat, and coughing and choking whilst taking medication or eating and drinking. For some, swallowing is intact until they become acutely unwell, then; due to their precarious physiological state, swallowing becomes transiently unsafe whilst they remain unwell. Rofes et al. reported that two-thirds of frail older adults presented with oropharyngeal residue, >50% had laryngeal penetration, and 17% had food and liquid entering the airway [64]. Frail adults who have a swallowing impairment have a higher mortality rate [64] and are more likely to develop pneumonia [65].
Dysphagia is present in many (53–92%) older adults who present with pneumonia [66,67] but is often not sought in the clinical environment [68]. Chojin et al., 2017 found that, of 153 people admitted to hospital with pneumonia (mean age 85.4 ± 9.9 years), 110 (72%) had an abnormal swallow assessment using the MASA (dysphagia and associated risk of aspiration) [69]. The premorbid prevalence of dysphagia in older adults’ people presenting with pneumonia is unknown; some have pre-existing dysphagia and other older people may well have decompensated swallowing as a secondary phenomenon of infection in the context of frailty.
8. Pneumonia and Frailty
The label, and hence the medical management, including antimicrobial treatment, given to “pneumonia” has been defined more by environmental considerations over the years rather than by microbiological evidence, hence the labels healthcare-acquired, community-acquired, and aspiration pneumonia. In reality, this separation lacks utility for the admitting physician and may adversely influence the medical care provided [70,71,72].
The aetiology of pneumonia in frail older adults is likely to be multifactorial in nature due to their lifetime exposure to toxins, multiple comorbidities (and polypharmacy), probable swallowing impairments [60,61], and maladaptive immunity [42]. Adults who have marked frailty (Clinical Frailty Score 7/8) with multiple comorbidities and who reside in a nursing home are more likely to be diagnosed with AP than other older adults [65,70,71,73,74,75,76,77].
This diagnosis is often made with little objectivity [10,78] and is dependent on the individual clinician’s subjective impression [79], and there is little documented consensus between clinicians [65].
The general clinical working definition for AP is “the development of pneumonia secondary to the presumed entry of oropharyngeal secretions into the lung, based solely on clinical suspicion and CXR changes with no supportive clinical observational or microbiological evidence” [70,80]. The American and British Thoracic and Respiratory Societies do not have guidelines or definitions of AP [12,81,82]. In Japan, the definition is one of “pneumonia in a patient with a predisposition to aspirate (due to dysphagia or swallowing disorders) and a predisposition to decreased airway clearance and pneumonia (due to a chronic lung disease or being bedbound)” [83].
Aspiration of saliva from the oral cavity into the tracheal-bronchial-alveolar tree via the pharynx is reported to be common but lung defences prevent any adverse outcomes [61]. Amongst older adults who are hospitalized with CAP, aspiration is observed in one-third of patients who are in their 50s, 50% of patients who are in their 60s, >80% of patients who are ≥70 years old [79], and possibly 92% of admitted frail older people [84]. Aspiration of oropharyngeal secretions is not a sine qua non of aspiration pneumonia [66]; Langmore et al. stated “just because someone has swallowing problems and may have aspiration, does not mean that aspiration is the cause of pneumonia” [85].
Pneumonia associated with aspiration can be the result of repeated aspiration of small amounts of pepsin within saliva [84], causing inflammation combined with reduced immune function [85] and impaired lung function, rather than an acute event. With chronic micro-aspiration and increased vascularity, there is an increase in cytokines (including TNFα and WEGF). Increased cytokine concentrations induce a decrease in muscle mass and strength (sarcopenia), increased frailty, worsening dysphagia, and possible further aspiration [56,84] (Figure 2).
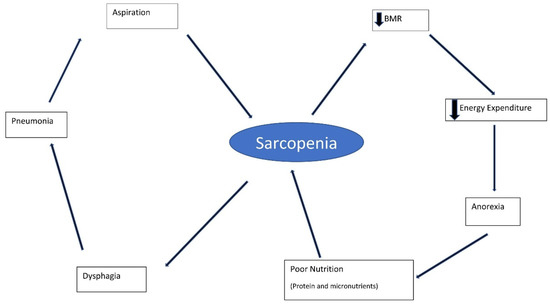
Figure 2.
Frailty–pneumonia cycle. BMR: Basal metabolic rate.
It is likely that the presence of risk factors for aspiration are more important than aspiration, per se [86], with many having more than one comorbidity, and a third may have >3 [87]. Manabe et al., 2015 suggested the following four factors, three of which could have been secondary to rather than aetiological to pneumonia [14]. Older and frail adults with polypathology frequent take many medications and, as a consequence, have a high anticholinergic burden (ACB). Castejon-Hermandez et al., 2021 found that those adults with an ACB ≥ 3 were >4 times more likely to develop dysphagia [88] and hence be at risk of aspiration and its complications [78].
9. Is It Time for Frailty-Associated Pneumonia?
Pneumonia commonly occurs following a stroke. In 2003, Hilker et al. coined the phrase stroke-associated pneumonia (SAP) to describe pneumonia occurring after an acute stroke, particularly in those admitted to intensive care units [89]. It has become accepted that SAP covers a spectrum of pulmonary infections [90,91] and that the aetiology of pneumonia after stroke is not purely infective in nature. Following a stroke, there is a transient inhibition of cell-mediated immunity demonstrated with a lymphopenia and monocyte deactivation, alteration of tracheal epithelium, and impaired airway clearance. Researchers studying animals noted that this inhibition resulted in spontaneous systemic bacterial infection within three days of the acute stroke [92]. This is driven by an overactivation of the hypothalamic–pituitary–adrenal axis and activation of the sympathetic nervous system [91,92,93], which has been inhibited by a beta receptor blockade [92].
Clinical risk factors for SAP are accepted to be stroke severity, reduced consciousness level, dysphagia, and the presence of long-term conditions (e.g., lung disease and ischaemic heart disease) [91].
As we have shown earlier, pneumonia occurring in older frail adults is complex and has many similarities to pneumonia in stroke (Table 1). Frail adults have a poorly functioning immune system, reduced airway clearance, altered bronchial epithelium, and multiple long-term conditions (Figure 1).

Table 1.
Factors implicated in stroke-associated pneumonia and frailty-associated pneumonia.
Given the frequency of aspiration and lack of microbiological differentiation between CAP, HAP, and AP, it is likely that they are all variations of the same clinical entity [76,94,95]. By clinically differentiating them, clinicians might ignore the potential for aspiration [66], potentially causing many people to be under-investigated [70].
In 2018, Ferguson et al. recommended dropping AP due to its lack of clinical accuracy and potential for causing harm to the patient [96]. Therefore, we suggest that it is time to designate pneumonia occurring in old and frail individuals as frailty-associated pneumonia (FAP) rather than CAP or AP.
Author Contributions
D.G.S. had the original idea for the paper. Writing of the paper was undertaken by D.G.S. and Y.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors have no conflict of interest.
References
- Eurostats. European Health Information Gateway European Mortality Database. Available online: https://gateway.euro.who.int/en/datasets/european-mortality-database/#population-and-icd-used (accessed on 9 December 2019).
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015.
- Smithard, D.G. Dysphagia: A geriatric giant? Med. Clin. Rev. 2016, 2, 5. [Google Scholar] [CrossRef]
- Baijens, L.W.; Clavé, P.; Cras, P.; Ekberg, O.; Forster, A.; Kolb, G.F.; Leners, J.C.; Masiero, S.; Del Nozal, J.M.; Ortega, O.; et al. European Society for Swallowing Disordrs—European Union Geriatric Medicine Society white paper: Oropharyngeal dysphagia as a geriatric syndrome. Clin. Investig. Aging 2016, 11, 1403–1428. [Google Scholar] [CrossRef]
- Higashiguchi, T.; Ohara, H.; Kamakura, Y.; Kikutani, T.; Kuzuya, M.; Enoki, H.; Sanada, H.; Matsuzaki, M.; Maruyama, M. Efficacy of a new post-mouthwash intervention (wiping plus oral nutritional supplements) for preventing aspiration pneumonia in elderly people: A multicentre, randomized, comparative trial. Ann. Nutr. Metab. 2017, 71, 253–260. [Google Scholar] [CrossRef]
- Torres, A.; Peetermans, W.E.; Viegi, G.; Blasi, F. Risk factors for community-acquired pneumonia in adults in Europe: A literature review. Thorax 2013, 68, 1057–1065. [Google Scholar] [CrossRef] [PubMed]
- Bohte, R.; Van Furth, R.; Broek, P.J.V.D. Aetiology of community-acquired pneumonia: A prospective study among adults requiring admission to hospital. Thorax 1995, 50, 543–647. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Douiri, A.; Gulliford, M. Pneumonia incidence trends in UK primary care from 2002–2017: Population based cohort study. Epidemiol. Infect. 2019, 147, e263. [Google Scholar] [CrossRef]
- Marik, P.E. Aspiration pneumonitis and aspiration pneumonia. N. Engl. J. Med. 2001, 344, 665–671. [Google Scholar] [CrossRef]
- Koivula, I.; Sten, M.; Makela, P.H. Risk factors for pneumonia in the elderly. Am. J. Med. 1994, 96, 313–320. [Google Scholar] [CrossRef]
- Jain, S.; Self, W.H.; Wunderink, R.G.; Fakhran, S.; Balk, R.; Bramley, A.M.; Reed, C.; Grijalva, C.G.; Anderson, E.J.; Courtney, C.M.; et al. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults. N. Engl. J. Med. 2015, 373, 415–427. [Google Scholar] [CrossRef]
- Metlay, J.P.; Waterer, G.W.; Long, A.C.; Anzueto, A.; Brozek, J.; Crothers, K.; Cooley, L.A.; Dean, N.C.; Fine, M.J.; Flander, S.A.S.; et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Disease Society of America. Am. J. Respir. Crit. Care Med. 2019, 200, e45–e67. [Google Scholar] [CrossRef]
- Feldman, C.; Anderson, R. Epidemiology, virulence factors and management of pneumococcus. F1000Research 2016, 5, 2320. [Google Scholar] [CrossRef] [PubMed]
- Manabe, T.; Teramoto, S.; Tamiya, N.; Okochi, J.; Hizawa, N. Risk factors for aspiration pneumonia in older adults. PLoS ONE 2015, 10, e0140060. [Google Scholar] [CrossRef] [PubMed]
- Meldrum, O.W.; Chotirmall, S.H. Mcus, microbiome and pulmonary disease. Biomedicines 2021, 9, 675. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://statistics.blf.org.uk/pneumonia (accessed on 24 July 2021).
- Samuelson, D.R.; Welsh, D.A.; Shellito, J.E. Regulation of lung immunity and host defense by intestinal microbiota. Front. Microbiol. 2015, 6, 1085. [Google Scholar] [CrossRef] [PubMed]
- Cramer, J.T.; Cruz-Jentoft, A.J.; Landi, F.; Hickson, M.; Zamboni, M.; Pereira, S.L.; Hustead, D.S.; Mustad, V.A. Impacts of high-protein oral nutritional supplements among malnourished men and women with sarcopenia: A multicenter randomized, double-blinded, controlled trial. J. Am. Med. Dir. Assoc. 2016, 17, 1044–1055. [Google Scholar] [CrossRef]
- Robinson, S.; Granic, A.; Sayer, A.A. Nurition and muscle strength, as a key component of sarcopenia: An overview of current evidence. Nutrients 2019, 11, 2942. [Google Scholar] [CrossRef] [PubMed]
- Welch, A. Micronutrient malnutrition across the life course, sarcopenia and frailty. Proc. Nutr. Soc. 2021, 80, 279–282. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older adults: Evidence for a phenotype. J. Gerontol. Med. Sci. 2001, 56A, M146–M156. [Google Scholar] [CrossRef]
- Gillick, M. Pinning down frailty. J. Gerontol. Med. Sci. 2001, 56A, M134–M135. [Google Scholar] [CrossRef]
- Li, H.; Manwani, B.; Leng, S.X. Frailty, inflammation, and immunity. Aging Dis. 2011, 6, 466–473. [Google Scholar]
- Ferrucci, L.; Penninx, B.W.; Volpato, S.; Harris, T.B.; Bandeen-Roche, K.; Balfour, J.; Leveille, S.G.; Fried, L.P.; Md, J.M. Change in muscle strength explains accelerated decline of physical function in older women with high interleukin-6 serum levels. J. Am. Geriatr. Soc. 2002, 50, 1947–1954. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Darer, J.; Walston, J. Frailty. In Geriatric Medicine; Springer: New York, NY, USA, 2003. [Google Scholar] [CrossRef]
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. Can. Med. Assoc. J. 2005, 173, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Xue, Q.-L. The frailty sundrome: Definition and natural history. Clin. Geriatr. Med. 2011, 27, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Ferrucci, L.; Darer, J.; Williamson, J.D.; Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J. Gerontol. Ser. A: Biol. Sci. Med. Sci. 2004, 59, M255–M263. [Google Scholar] [CrossRef]
- Phu, S.; Boersma, D.; Duque, G. Exercise and sarcopenia. J. Clin. Densitom. 2015, 18, 488–492. [Google Scholar] [CrossRef] [PubMed]
- Chichero, J.A.Y. Age related changes to eating and swallowing impact frailty: Aspiration, choking risk, modified food texture and autonomy of choice. Geriatrics 2018, 3, 69. [Google Scholar] [CrossRef]
- Semba, R.D.; Blaum, C.S.; Bartali, B.; Xue, Q.L.; Ricks, M.O.; Guralnik, J.M.; Fried, L.P. Denture use, malnutrition, frailty, and mortality among older women living in the community. J. Nutr. Health Aging 2006, 10, M151–M167. [Google Scholar]
- Morley, J.E. Oral Frailty. J. Nutr. Health Aging 2020, 24, 683–684. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, T.; Maeda, K.; Tahira, K.; Taniguchi, K.; Mori, K.; Kiyomiya, H.; Akagi, J. Silent aspiration predicts mortality in older adults with aspiration pneumonia admitted to acute hospitals. Geriatr. Gerontol. Int. 2018, 18, 828–832. [Google Scholar] [CrossRef]
- Yoneyama, T.; Yoshida, M.; Ohrui, T.; Mukaiyama, H.; Okamoto, H.; Hoshiba, K.; Ihara, S.; Yanagisawa, S.; Ariumi, S.; Morita, T.; et al. Oral care reduces pneumonia in older patients in nursing homes. J. Am. Geriatr. Soc. 2002, 50, 430–433. [Google Scholar] [CrossRef]
- Tohara, T.; Kikutani, T.; Tamura, F.; Yoshida, M.; Kuboki, T. Multicentred epidemiological study of factors associated with total bacterial count in the saliva of older people requiring nursing care. Geriatr. Gerontol. Int. 2017, 17, 219–225. [Google Scholar] [CrossRef]
- Nishizawa, T.; Niikura, Y.; Akasaka, K.; Watanabe, M.; Kurai, D.; Amano, M.; Ishii, H.; Matsushima, H.; Yamashita, N.; Takizawa, H. Pilot study for risk assessment of aspiration pneumonia on oral bacteria levels and serum biomarkers. BMC Infect. Dis. 2019, 19, 761. [Google Scholar] [CrossRef] [PubMed]
- Gosney, M.; Punekar, S.; Playfer, J.R.; Bilsborrow, P.K.; Martin, M.V. The incidence of oral gram-negative bacteria in patients with Parkinson’s disease. Eur. J. Intern. Med. 2003, 14, 484–487. [Google Scholar] [CrossRef] [PubMed]
- Martín, A.; Ortega, O.; Roca, M.; Arús, M.; Clavé Civit, P. Effect of a minimal-massive intervention in hosptalised older patients with oropharyngeal dysphagia: A proof of concept study. J. Nutr. Health Aging 2018, 22, 729–747. [Google Scholar]
- Liu, Z.-Y.; Wei, L.; Ye, R.-C.; Chen, J.; Nie, D.; Zhang, G.; Zhang, X.-P. Reducing the incidence of stroke-associated pneumonia: An evidence-based practice. BMC Neurol. 2022, 22, 297. [Google Scholar] [CrossRef] [PubMed]
- Foltyn, P. Aging, dementia and oral health. Aust. Dent. J. 2015, 60 (Suppl. S1), 86–94. [Google Scholar] [CrossRef]
- Ferruci, L.; Fabbri, E. Inflammageing: Chronic inflammation in ageing, cardiovascular disease, and frailty. Nat. Rev. Cardiol. 2018, 15, 505–522. [Google Scholar] [CrossRef] [PubMed]
- Thannickal, V.J.; Murthy, M.; Balch, W.E.; Chandel, N.S.; Meiners, S.; Eickelberg, O.; Selman, M.; Pardo, A.; White, E.S.; Levy, B.D.; et al. Blue journal conference. Aging and susceptibility to lung disease. Am. J. Respir. Crit. Care Med. 2015, 191, 261–269. [Google Scholar] [CrossRef] [PubMed]
- El-Solh, A.A.; Sikka, P.; Ramadan, F.; Davies, J. Etiology of Severe Pneumonia in the Very Elderly. Am. J. Respir. Crit. Care Med. 2001, 163, 645–651. [Google Scholar] [CrossRef]
- Kikawada, M.; Iwamoto, T.; Takasaki, M. Aspiration and infection in the elderly: Epidemiology, diagnosis and management. Drugs Aging 2005, 22, 115–130. [Google Scholar] [CrossRef]
- Sansoni, P.; Cossarizza, A.; Brianti, V.; Fagnoni, F.; Snelli, G.; Monti, D.; Marcato, A.; Passeri, G.; Ortolani, C.; Forti, E. Lymphocyte subsets and natural killer cell activity in healthy old people and centenarians. Blood 1993, 82, 2767–2773. [Google Scholar] [CrossRef] [PubMed]
- Meyer, K.C. The role of immunity in susceptibility to respiratory infection in the aging lung. Respir. Physiol. 2001, 128, 23–31. [Google Scholar] [CrossRef]
- Calder, P.C. Nutrition and immunity: Lessons for COVID-19. Eur. J. Clin. Nutr. 2021, 75, 1309–1318. [Google Scholar] [CrossRef] [PubMed]
- Segal, L.N.; Rom, W.N.; Weiden, M.D. Lung microbiome for clinicians. New discoveries about bugs in healthy and diseased lungs. Ann. Am. Thorac. Soc. 2014, 11, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Segal, L.N.; Clemente, J.C.; Tsay, J.C.; Koralov, S.B.; Keller, B.C.; Wu, B.G.; Li, Y.; Shen, N.; Ghedin, E.; Morris, A.; et al. Enrichment of the lung microbiome with oral taxa is associated with lung inflammation of a Th17 phenotype. Nat. Microbiol. 2016, 1, 16031. [Google Scholar] [CrossRef] [PubMed]
- Dickson, R.P.; Erb-Downward, J.R.; Huffnagle, G.B. Homeostasis and its disruption in the lung microbiome. Am. J. Physiol. Lung Cell. Mol. Physiol. 2015, 309, L1047–L1055. [Google Scholar] [CrossRef]
- Dickson, R.P.; Erb-Downward, J.R.; Freeman, C.M. Bacterial topography of the healthy human lower respiratory tract. mBio 2017, 8, 14. [Google Scholar] [CrossRef]
- Fujita, Y.; Kadota, T.; Araya, J.; Ochiya, T.; Kuwano, K. Extracellular vesicles: New players in lung immunity. Am. J. Respir. Cell Mol. Biol. 2018, 58, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Rubin, B.K. Physiology of airway mucus clearance. Respir. Care 2002, 47, 761–768. [Google Scholar] [PubMed]
- Nosal, C.; Ehlers, A.; Haspel, J.A. Why lungs keep time: Circadian rhythms and lung immunity. Annu. Rev. Physiol. 2020, 82, 391–412. [Google Scholar] [CrossRef]
- Weiskopf, D.; Weinberger, B.; Grubeck-Loebenstein, B. The Aging of the Immune System. Transpl. Int. 2009, 11, 1041–1050. [Google Scholar] [CrossRef] [PubMed]
- Komatsu, R.; Okazaki, T.; Ebihara, S.; Kobayashi, M.; Tsukita, Y.; Nihei, M.; Sugiura, H.; Niu, K.; Ebihara, T.; Ichinose, M. Aspiration pneumonia induces muscle atrophy in the respiratory, skeletal, and swallowing systems. J. Cachexia Sarcopenia Muscle 2018, 9, 643–653. [Google Scholar] [CrossRef] [PubMed]
- Woodford-Williams, E. Diagnosis and management of pneumonia in the aged. BMJ 1966, 1, 467. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bosch, X.; Formiga, F.; Cuerpo, S.; Torres, B.; Roson, B.; Lopez-Soto, A. Aspiration pneumonia in old patients with dementia. Prognostic factors of mortality. Eur. J. Intern. Med. 2012, 23, 720–726. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, C.M.; Marsland, B.J. Lung homeostasis: Influence of age, microbes, and the immune system. Immunity 2017, 46, 549. [Google Scholar] [CrossRef]
- Nohara, K.; Kaneko, N.; Uchida, Y.; Tanaka, N.; Sakai, T. Relationship between airway clearance function and aspiration pneumonia in geriatric nursing home residents. Dysphagia 2015, 30, 246–247. [Google Scholar]
- Petroianni, A.; Ceccarelli, D.; Conti, V.; Terzano, C. Aspiration pneumonia. Pathophysiological aspects, prevention and management. Panminerva Med. 2006, 48, 231–239. [Google Scholar]
- Marik, P.E.; Kaplan, D. Aspiration pneumonia and dysphagia in the elderly. Chest 2003, 124, 328–336. [Google Scholar] [CrossRef]
- Smithard, D.; Hansjee, D.; Henry, D.; Mitchell, L.; Sabaharwal, A.; Salkeld, J.; Yeung, E.; Younus, O.; Swaine, I. Inter-relationships between frailty, sarcopenia, undernutrition and dysphagia in older people who are admitted to acute frailty and medical wards: Is there an Older Adult Quartet. Geriatrics 2020, 5, 41. [Google Scholar] [CrossRef]
- Rofes, L.; Arreola, V.; Romea, M.; Palomera, E.; Almirall, J.; Cabré, M.; Serra-Prat, M.; Clavé, P. Pathophysiology of oropharyngeal dysphagia in the frail elderly. Neurogastroenterol. Motil. 2010, 22, 851-e230. [Google Scholar] [CrossRef]
- Van der Maarel-Wierink, C.D.; Vanobbergen, J.N.O.; Bronkhorst, E.M.; Schols, J.M.G.A.; de Baat, C. Meta-analysis of dysphagia and aspiration pneumonia in frail elders. J. Dent. Res. 2011, 90, 1398–1404. [Google Scholar] [CrossRef] [PubMed]
- Gleeson, K.; Maxwell, S.; Eggli, D.F. Quantitative aspiration during sleep in normal subjects. Chest 1997, 111, 1266–1272. [Google Scholar] [CrossRef] [PubMed]
- Almirall, J.; Rofes, L.; Serra-Prat, M.; Icart, R.; Palomera, E.; Arreola, V.; Clavé, P. Oropharyngeal dysphagia is a risk factor for community-acquired pneumonia in the elderly. Eur. Respir. J. 2013, 41, 923–926. [Google Scholar] [CrossRef] [PubMed]
- Smithard, D.; Westmark, S.; Melgaard, D. Evaluation of the prevalence of screening for dysphagia among older people admitted to medical services—An international survey. Geriatrics 2019, 3, 86. [Google Scholar] [CrossRef]
- Chojin, Y.; Kato, T.; Noguchi, S.; Rikihisa, M.; Omori, M.; Mukae, H.; Yatera, K. Evaluating a novel swallowing assessment as a predictor of mortality and recurring pneumonia in elderly patients with pneumonia. Respir. Investig. 2021, 59, 783–791. [Google Scholar] [CrossRef]
- Yoshimatsu, Y.; Smithard, D.G. A Paradigm Shift in the Diagnosis of Aspiration Pneumonia in Older Adults. J. Clin. Med. 2022, 11, 5214. [Google Scholar] [CrossRef]
- Yoshimatsu, Y.; Melgaard, D.; Westergren, A.; Skrubbeltrang, C.; Smithard, D.G. The Diagnosis of Aspiration Pneumonia: A Systematic Review. Eur. Geriatr. Med. 2022; in press. [Google Scholar] [CrossRef]
- Hollaar, V.; Van Der Maarel-Wierink, C.; Van Der Putten, G.-J.; Van Der Sanden, W.; De Swart, B.; De Baat, C. Defoning chracteristics and risk indicators for diagnosing nursing home-acquired pneumonia and aspiration pneumonia in nursing home residents, using the electronically-modified Delphi Method. BMC Geriatr. 2016, 16, 60. [Google Scholar] [CrossRef]
- Yoon, H.-Y.; Shim, S.S.; Kim, S.J.; Lee, J.H.; Chang, J.H.; Lee, S.H.; Ryu, Y.J. Long-term mortality and prognostic factors in aspiration pneumonia. J. Am. Dir. Assoc. 2019, 20, 1098–1104. [Google Scholar] [CrossRef]
- Yamauchi, Y.; Yasunaga, H.; Matsui, H.; Hasegawa, W.; Jo, T.; Takami, K.; Fushimi, K.; Nagase, T. Comparison of clinical characteristics and outcomes between aspiration pneumonia and community acquired pneumonia in patients with chronic obstructive pulmonary disease. BMC Pulm. Med. 2015, 15, 69. [Google Scholar] [CrossRef][Green Version]
- Akata, K.; Yatera, K.; Yamasaki, K.; Kawanami, T.; Naito, K.; Noguchi, S.; Fukuda, K.; Ishimoto, H.; Taniguchi, H.; Mukae, H. The significance of oral streptococci in patients with pneumonia with risk factors for aspiration: The bacterial floral analysis of 16S ribosomal RNA gene using bronchoalveolar lavage fluid. BMC Pulm. Med. 2016, 16, 79. [Google Scholar] [CrossRef]
- Lanspa, M.J.; Peyrani, P.; Wiemken, T.; Wilson, E.L.; Ramirez, J.A.; Dean, N.C. Characteristics associated with clinician diagnosis of aspiration pneumonia; a descriptive study of afflicted patients and their outcomes. J. Hosp. Med. 2015, 10, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Palacios-Cena, D.; Hernandez-Barrera, V.; Lopez-de-Andres, A.; Fernandez-de-Las-Penas, C.; Palacios-Cena, M.; de Miguel-Diez, J.; Carrasco-Garrido, P.; Jimenez-Garcia, R. Time trends in incidence and outcomes of hospitalizations for aspiration pneumonia among elderly people in Spain (2003–2013). Eur. J. Intern. Med. 2017, 38, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Marik, P.E. Pulmonary aspiration syndromes. Curr. Opin. Pulm. Med. 2011, 17, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Teramoto, S.; Fukuchi, Y.; Sasaki, H.; Sato, K.; Sekizawa, K.; Matsuse, T. High incidence of aspiration pneumonia in community and hospital-acquired pneumonia in hospitalized patients: A multicenter, prospective study in Japan. J. Am. Geriatr. Soc. 2008, 56, 577–579. [Google Scholar] [CrossRef] [PubMed]
- Sarin, J.; Balasubramaniam, R.; Corcoran, A.M.; Laudenbach, J.M.; Stoopler, E.T. Reducing risk of aspiration pneumonia among elderly patients in long-term care facilities through oral health interventions. J. Am. Med. Dir. Assoc. 2008, 9, 128–135. [Google Scholar] [CrossRef]
- Lim, W.S.; Baudouin, S.V.; George, R.C.; Hill, A.T.; Jamieson, C.; Le Jeune, I.; Macfarlane, J.T.; Read, R.C.; Roberts, H.J.; Levy, M.L.; et al. Pneumonia Guidelines Committee of the BTS Standards of Care Committee. BTS guidelines for the management of community acquired pneumonia in adults: Update 2009. Thorax 2009, 64 (Suppl. S3), iii1–iii55. [Google Scholar] [CrossRef] [PubMed]
- BTS Care Bundles for CAP and COPD. 2014. Available online: https://www.britthoracic.org.uk/audit-and-quality-improvement/bts-care-bundlesfor-cap-and-copd/ (accessed on 8 September 2022).
- The Japanese Respiratory Society. The JRS Guidelines for the Management of Pneumonia in Adults; Medical Review Co.: Tokyo, Japan, 2017. (In Japanese) [Google Scholar]
- Ebihara, S.; Sekiya, H.; Miyagi, M.; Ebihara, T.; Okazaki, T. Dysphagia, dystussia, and aspiration pneumonia in elderly people. J. Thorac. Dis. 2016, 8, 632–639. [Google Scholar] [CrossRef]
- Langmore, S.; Terpenning, M.S.; Schork, A.; Chen, Y.; Murray, J.T.; Lopatin, D.E.; Loesche, W.J. Predictors of Aspiration Pneumonia:How Important Is Dysphagia? Dysphagia 1998, 13, 69–81. [Google Scholar] [CrossRef]
- Noguchi, S.; Yatera, K.; Kato, T.; Chojin, Y.; Fujino, Y.; Akata, K.; Kawanami, T.; Sakamoto, N.; Mukae, H. Impact of the number of aspiration risk factors on mortality and recurrence in community-onset pneumonia. Clin. Int. Aging 2017, 12, 2087–2094. [Google Scholar] [CrossRef]
- Pieralli, F.; Vannucchi, V.; Mancini, A.; Grazzini, M.; Paolacci, G.; Morettini, A.; Nozzoli, C. Delirium is a predictor of in-hospital mortality in elderly patients with community acquired pneumonia. Intern. Emerg. Med. 2014, 9, 195–200. [Google Scholar] [CrossRef]
- Castejón-Hernández, S.; Latorre-Vallbona, N.; Molist-Brunet, N.; Cubí-Montanyà, D.; Espaulella-Panicot, J. Association between anticholinergic burden and oropharyngeal dysphagia among hospitalized older adults. Aging Clin. Exp. Res. 2021, 33, 1981–1985. [Google Scholar] [CrossRef] [PubMed]
- Hilker, R.; Poetter, C.; Findeisen, N.; Sobesky, J.; Jacobs, A.; Neveling, M.; Heiss, W.-D. Nosocomial pneumonia after stroke. Stroke 2003, 34, 975–981. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Yang, H.; Wei, H.; Chen, Y.; Lan, M. Stroke-associated pneumonia. A bibliometric analysis of worldwide trends from 2003 to 2020. Medicine 2021, 100, e27321. [Google Scholar] [CrossRef] [PubMed]
- Eltringham, S.A.; Kilner, K.; Gee, M.; Sage, K.; Bray, B.D.; Smith, C.J.; Pownall, S. Factors associated with risk of stroke-associated pneumonia in patients with dysphagia: A systematic review. Dysphagia 2020, 35, 735–744. [Google Scholar] [CrossRef]
- Prass, K.; Meisel, C.; Höflich, C.; Braun, J.; Halle, E.; Wolf, T.; Ruscher, K.; Victorov, I.V.; Priller, J.; Dirnagl, U.; et al. Stroke-induced immunodeficiency promotes spontaneous bacterial infections and is mediated by sympathetic activation reversal by post stroke T Helper cell type 1-like immunostimulation. J. Exp. Med. 2003, 198, 725–736. [Google Scholar] [CrossRef]
- O’Neill, P.A.; Davies, I.; Fullerton, K.; Bennet, D. Stress hormone and blood glucose response following acute stroke in the elderly. Stroke 1991, 22, 842–847. [Google Scholar] [CrossRef]
- Palmer, L.B.; Albulak, K.; Fields, S.; Filkin, A.M.; Simon, S.; Smaldone, G.C. Oral clearance and pathogenic colonistaion in the elderly. Am. J. Resp. Crit. Care Med. 2001, 164, 464–468. [Google Scholar] [CrossRef]
- Komiya, K.; Ishii, H.; Kadota, J. Healthcare-associated pneumonia and aspiration pneumonia. Aging Dis. 2015, 6, 27–37. [Google Scholar] [CrossRef]
- Ferguson, J.; Ravert, B.; Gailey, M. Aspiration: /aspə’rāSH(ə)n/: An ambiguous term used for a diagnosis of uncertainty. Clin. Pulm. Med. 2018, 25, 177–193. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).