Mild Cognitive Impairment Is Associated with Poorer Nutritional Status on Hospital Admission and after Discharge in Acutely Hospitalized Older Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
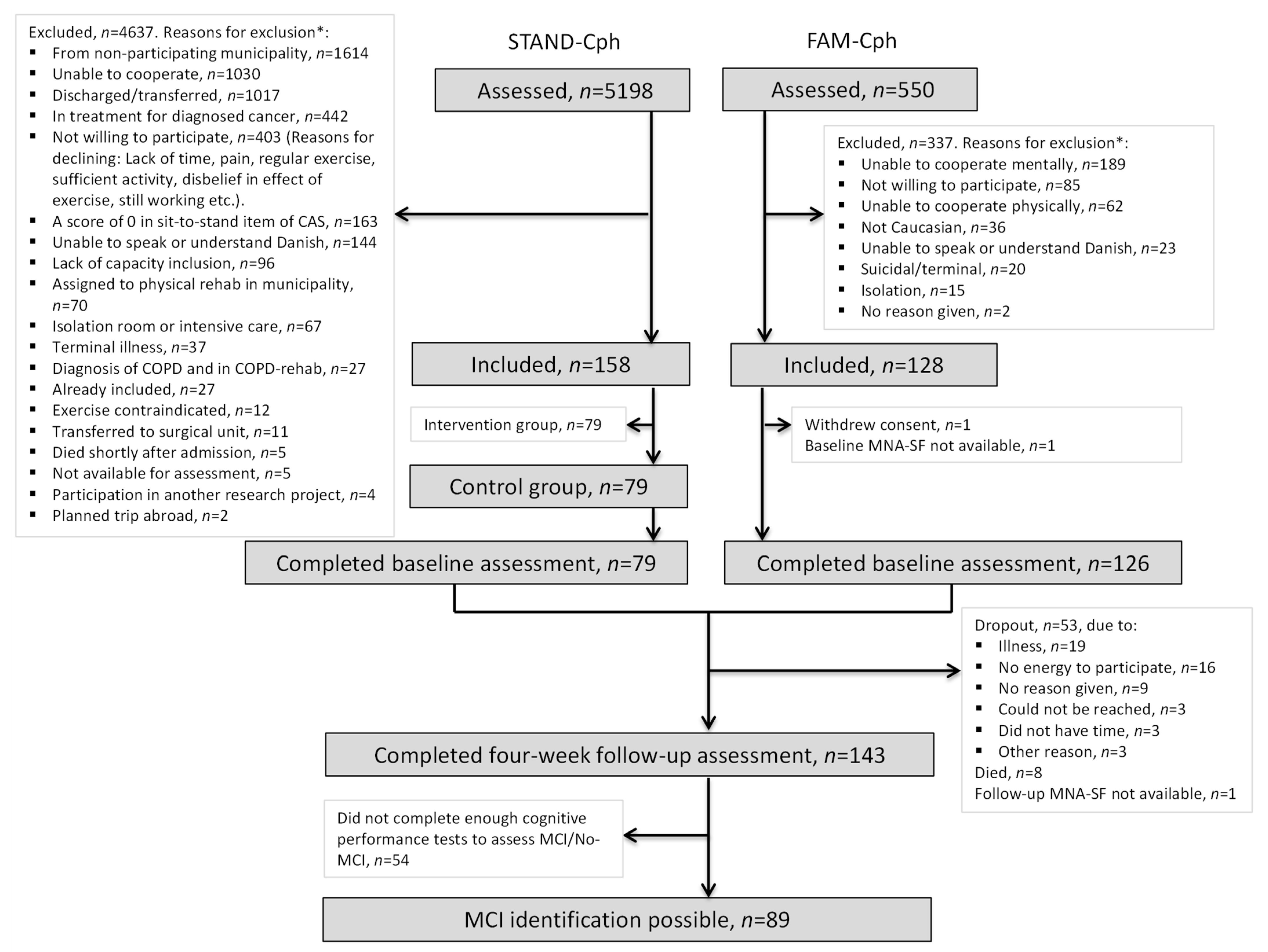
2.3. Participants and Recruitment
2.4. Variables
2.4.1. Dependent Variable—Nutritional Status
2.4.2. Independent Variable—Mild Cognitive Impairment
2.4.3. Potential Confounders
2.4.4. Descriptive Variables
2.5. Data Sources
2.6. Statistical Analyses
3. Results
3.1. Participant Characteristics
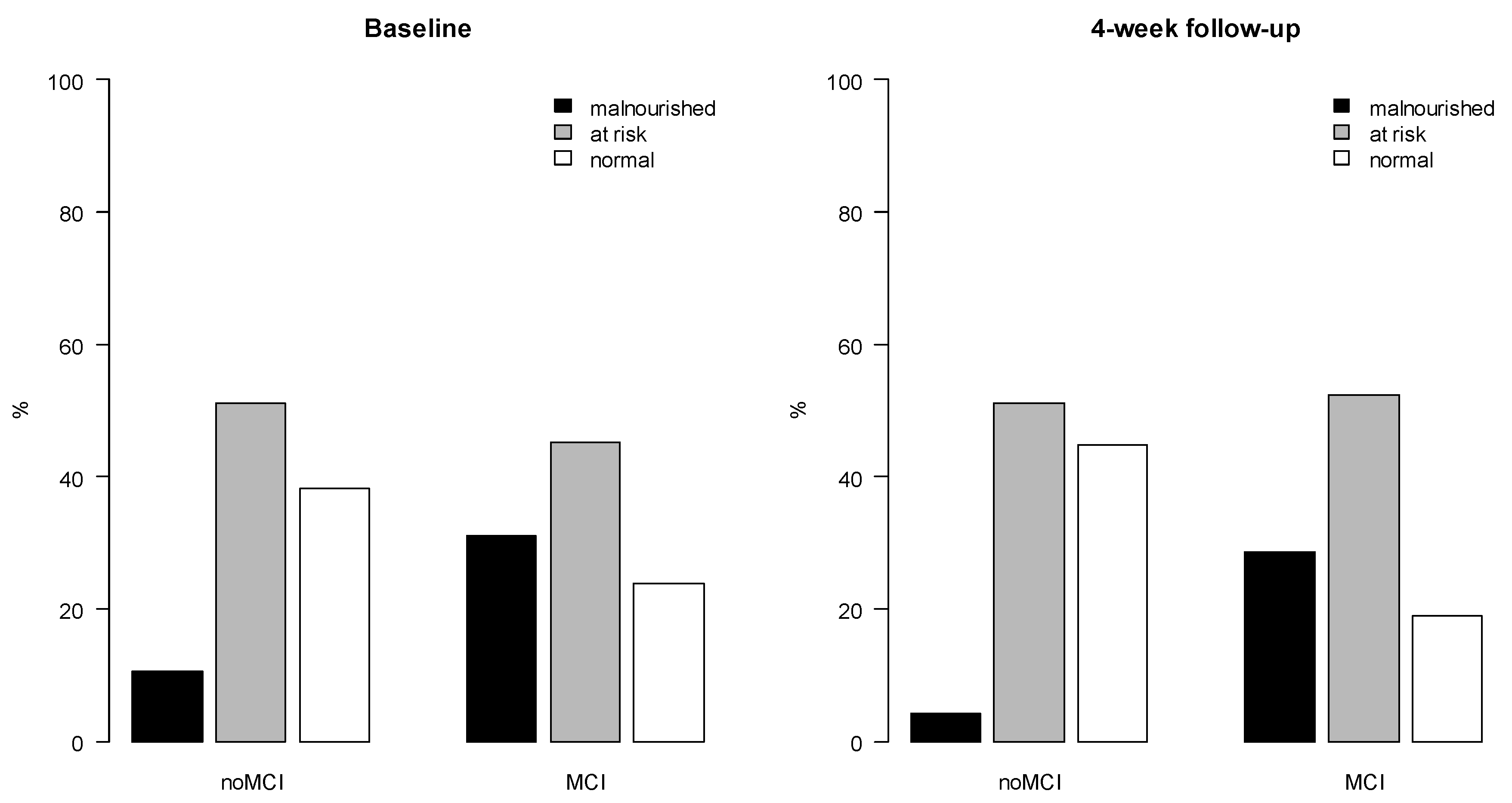
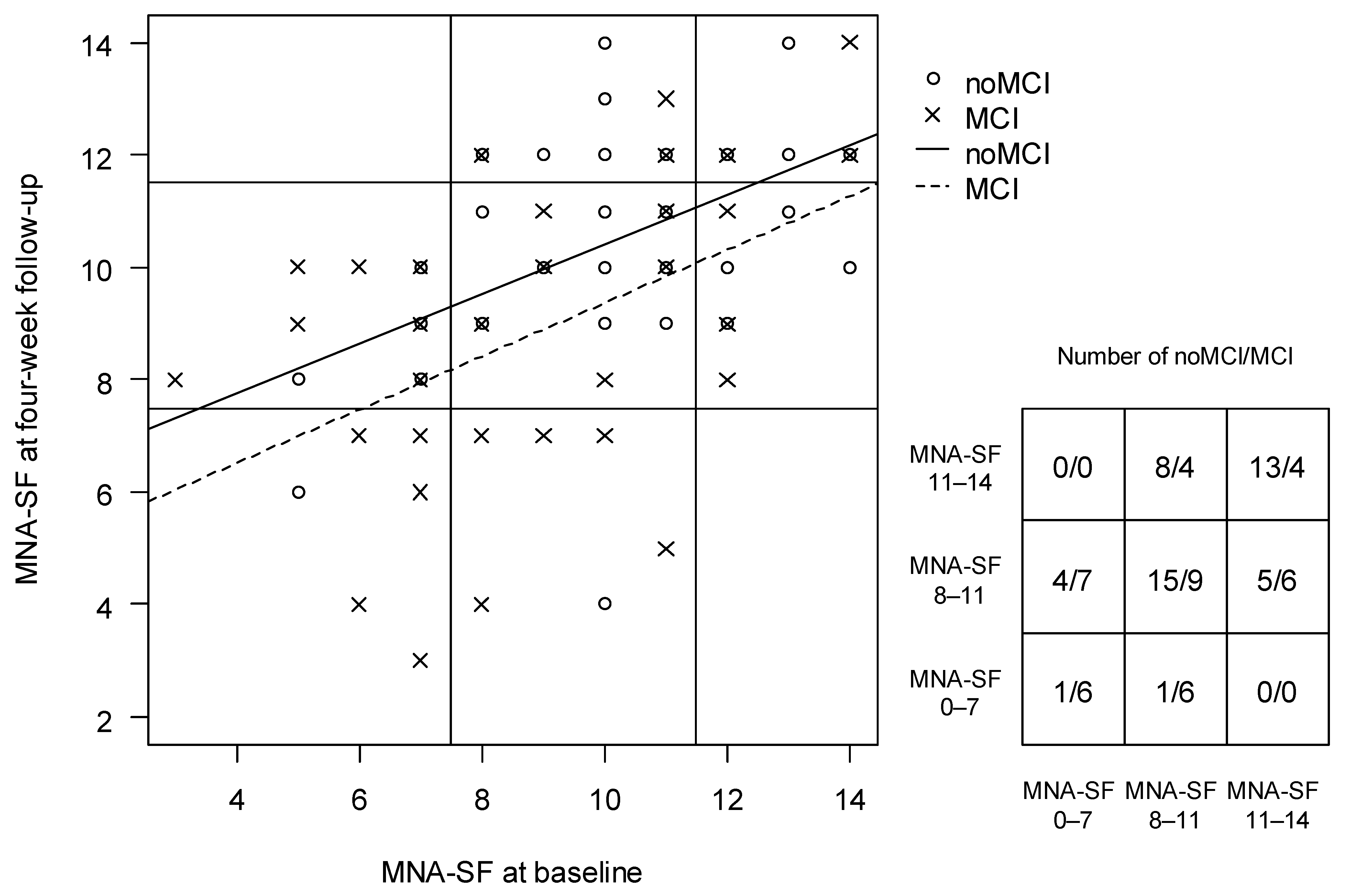
3.2. The Association between MCI and Nutritional Status at Baseline and 4-Week Follow-Up
3.3. The Association between MCI and Change in Nutritional Status from Baseline to 4-Week Follow-Up
3.4. Sensitivity Analysis
4. Discussion
4.1. Main Findings
4.2. Results in the Context of Other Studies and Significant Findings
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations; Department of Economic and Social Affairs; Population Division. World Population Ageing, 2019 Highlights; United Nations: New York, NY, USA, 2020; ISBN 978-92-1-148325-3. [Google Scholar]
- Statistikbanken. Available online: https://www.statistikbanken.dk/IND02 (accessed on 20 April 2021).
- Lawson-Smith, L.; Petersen, J.; Jensen, P.S.; Sivertsen, D.M.; Pedersen, M.M.; Ellekilde, G.; Lindhardt, T.; Andersen, O. Nutritional Risk in Acutely Admitted Older Medical Patients. Am. J. Food Nutr. 2015, 3, 84–89. [Google Scholar]
- Pereira, G.F.; Bulik, C.M.; Weaver, M.A.; Holland, W.C.; Platts-Mills, T.F. Malnutrition among Cognitively Intact, Non-Critically Ill Older Adults in the Emergency Department. Ann. Emerg. Med. 2015, 65, 85–91. [Google Scholar] [CrossRef]
- Bolado Jiménez, C.; Fernádez Ovalle, H.; Muñoz Moreno, M.F.; Aller de la Fuente, R.; de Luis Román, D.A. Undernutrition Measured by the Mini Nutritional Assessment (MNA) Test and Related Risk Factors in Older Adults under Hospital Emergency Care. Nutrition 2019, 66, 142–146. [Google Scholar] [CrossRef]
- Fogg, C.; Meredith, P.; Culliford, D.; Bridges, J.; Spice, C.; Griffiths, P. Cognitive Impairment Is Independently Associated with Mortality, Extended Hospital Stays and Early Readmission of Older People with Emergency Hospital Admissions: A Retrospective Cohort Study. Int. J. Nurs. Stud. 2019, 96, 1–8. [Google Scholar] [CrossRef]
- Fogg, C.; Meredith, P.; Bridges, J.; Gould, G.P.; Griffiths, P. The Relationship between Cognitive Impairment, Mortality and Discharge Characteristics in a Large Cohort of Older Adults with Unscheduled Admissions to an Acute Hospital: A Retrospective Observational Study. Age Ageing 2017, 46, 794–801. [Google Scholar] [CrossRef]
- Reynish, E.L.; Hapca, S.M.; De Souza, N.; Cvoro, V.; Donnan, P.T.; Guthrie, B. Epidemiology and Outcomes of People with Dementia, Delirium, and Unspecified Cognitive Impairment in the General Hospital: Prospective Cohort Study of 10,014 Admissions. BMC Med. 2017, 15, 140. [Google Scholar] [CrossRef]
- Buurman, B.M.; Hoogerduijn, J.G.; de Haan, R.J.; Abu-Hanna, A.; Lagaay, A.M.; Verhaar, H.J.; Schuurmans, M.J.; Levi, M.; de Rooij, S.E. Geriatric Conditions in Acutely Hospitalized Older Patients: Prevalence and One-Year Survival and Functional Decline. PLoS ONE 2011, 6, e26951. [Google Scholar] [CrossRef]
- Volkert, D.; Chourdakis, M.; Faxen-Irving, G.; Frühwald, T.; Landi, F.; Suominen, M.H.; Vandewoude, M.; Wirth, R.; Schneider, S.M. ESPEN Guidelines on Nutrition in Dementia. Clin. Nutr. 2015, 34, 1052–1073. [Google Scholar] [CrossRef] [PubMed]
- Burks, C.E.; Jones, C.W.; Braz, V.A.; Swor, R.A.; Richmond, N.L.; Hwang, K.S.; Hollowell, A.G.; Weaver, M.A.; Platts-Mills, T.F. Risk Factors for Malnutrition among Older Adults in the Emergency Department: A Multicenter Study. J. Am. Geriatr. Soc. 2017, 65, 1741–1747. [Google Scholar] [CrossRef] [PubMed]
- Orsitto, G.; Fulvio, F.; Tria, D.; Turi, V.; Venezia, A.; Manca, C. Nutritional Status in Hospitalized Elderly Patients with Mild Cognitive Impairment. Clin. Nutr. 2009, 28, 100–102. [Google Scholar] [CrossRef] [PubMed]
- Orsitto, G. Different components of nutritional status in older inpatients with cognitive impairment. J. Nutr. 2012, 16, 4. [Google Scholar] [CrossRef] [PubMed]
- Shawky Khater, M.; Fawzy Abouelezz, N. Nutritional Status in Older Adults with Mild Cognitive Impairment Living in Elderly Homes in Cairo, Egypt. J. Nutr. Health Aging 2011, 15, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Buhl, S.F.; Andersen, A.L.; Andersen, J.R.; Andersen, O.; Jensen, J.-E.B.; Rasmussen, A.M.L.; Pedersen, M.M.; Damkjær, L.; Gilkes, H.; Petersen, J. The Effect of Protein Intake and Resistance Training on Muscle Mass in Acutely Ill Old Medical Patients—A Randomized Controlled Trial. Clin. Nutr. 2016, 35, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Vivanti, A.; Isenring, E.; Baumann, S.; Powrie, D.; O’Neill, M.; Clark, D.; Courtice, S.; Campbell, K.; Ferguson, M. Emergency Department Malnutrition Screening and Support Model Improves Outcomes in a Pilot Randomised Controlled Trial. Emerg. Med. J. 2015, 32, 180–183. [Google Scholar] [CrossRef]
- Sharma, Y.; Thompson, C.H.; Kaambwa, B.; Shahi, R.; Hakendorf, P.; Miller, M. Investigation of the Benefits of Early Malnutrition Screening with Telehealth Follow up in Elderly Acute Medical Admissions. QJM Int. J. Med. 2017, 110, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Nationalt Videnscenter for Demens Mild Cognitive Impairment. Available online: https://videnscenterfordemens.dk/da/mild-cognitive-impairment (accessed on 29 September 2021).
- Brigola, A.G.; Rossetti, E.S.; dos Santos, B.R.; Neri, A.L.; Zazzetta, M.S.; Inouye, K.; Pavarini, S.C.I. Relationship between Cognition and Frailty in Elderly: A Systematic Review. Dement. Neuropsychol. 2015, 9, 110–119. [Google Scholar] [CrossRef]
- Vetrano, D.L.; Palmer, K.; Marengoni, A.; Marzetti, E.; Lattanzio, F.; Roller-Wirnsberger, R.; Lopez Samaniego, L.; Rodríguez-Mañas, L.; Bernabei, R.; Onder, G.; et al. Frailty and Multimorbidity: A Systematic Review and Meta-Analysis. J. Gerontol. Ser. A 2019, 74, 659–666. [Google Scholar] [CrossRef]
- Taylor, C.A.; Bouldin, E.D.; Greenlund, K.J.; McGuire, L.C. Comorbid Chronic Conditions Among Older Adults with Subjective Cognitive Decline, United States, 2015–2017. Innov. Aging 2020, 4, igz045. [Google Scholar] [CrossRef]
- Prasad, N.; Gupta, A.; Sinha, A.; Sharma, R.K.; Saxena, A.; Kaul, A.; Bhaduria, D.; Gupta, A. Confounding Effect of Comorbidities and Malnutrition on Survival of Peritoneal Dialysis Patients. J. Ren. Nutr. 2010, 20, 384–391. [Google Scholar] [CrossRef]
- Smichenko, J.; Gil, E.; Zisberg, A. Relationship Between Changes in Sedative-Hypnotic Medications Burden and Cognitive Outcomes in Hospitalized Older Adults. J. Gerontol. Ser. A 2020, 75, 1699–1705. [Google Scholar] [CrossRef]
- Bell, J.S.; Mezrani, C.; Blacker, N.; LeBlanc, T.; Frank, O.; Alderman, C.P.; Rossi, S.; Rowett, D.; Shute, R. Anticholinergic and Sedative Medicines. Aust. Fam. Physician 2012, 41, 45–49. [Google Scholar] [PubMed]
- Lee, J.E.; Ju, Y.J.; Chun, K.H.; Lee, S.Y. The Frequency of Sleep Medication Use and the Risk of Subjective Cognitive Decline (SCD) or SCD With Functional Difficulties in Elderly Individuals Without Dementia. J. Gerontol. Ser. A 2020, 75, 1693–1698. [Google Scholar] [CrossRef] [PubMed]
- Field, N.; Cohen, T.; Struelens, M.J.; Palm, D.; Cookson, B.; Glynn, J.R.; Gallo, V.; Ramsay, M.; Sonnenberg, P.; MacCannell, D.; et al. Strengthening the Reporting of Molecular Epidemiology for Infectious Diseases (STROME-ID): An Extension of the STROBE Statement. Lancet Infect. Dis. 2014, 14, 341–352. [Google Scholar] [CrossRef]
- Pedersen, M.M.; Petersen, J.; Beyer, N.; Damkjær, L.; Bandholm, T. Supervised Progressive Cross-Continuum Strength Training Compared with Usual Care in Older Medical Patients: Study Protocol for a Randomized Controlled Trial (the STAND-Cph Trial). Trials 2016, 17, 176. [Google Scholar] [CrossRef] [PubMed]
- Intranet. Available online: https://intranet.regionh.dk/ahh/data/find-data/soeg-data-efter-afdeling/Documents/Akutmodtagelsen/Indl%C3%A6ggelsm%C3%A5de.pdf (accessed on 20 April 2021).
- Andersen, A.L.; Nielsen, R.L.; Houlind, M.B.; Tavenier, J.; Rasmussen, L.J.H.; Jørgensen, L.M.; Treldal, C.; Beck, A.M.; Pedersen, M.M.; Andersen, O.; et al. Risk of Malnutrition upon Admission and after Discharge in Acutely Admitted Older Medical Patients: A Prospective Observational Study. Nutrients 2021, 13, 2757. [Google Scholar] [CrossRef] [PubMed]
- Winblad, B.; Palmer, K.; Kivipelto, M.; Jelic, V.; Fratiglioni, L.; Wahlund, L.-O.; Nordberg, A.; Backman, L.; Albert, M.; Almkvist, O.; et al. Mild Cognitive Impairment—Beyond Controversies, towards a Consensus: Report of the International Working Group on Mild Cognitive Impairment. J. Intern. Med. 2004, 256, 240–246. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Harker, J.O.; Salva, A.; Guigoz, Y.; Vellas, B. Screening for Undernutrition in Geriatric Practice: Developing the Short-Form Mini-Nutritional Assessment (MNA-SF). J. Gerontol. Ser. A Biol. Sci. Med Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef]
- Soysal, P.; Veronese, N.; Arik, F.; Kalan, U.; Smith, L.; Isik, A.T. Mini Nutritional Assessment Scale-Short Form Can Be Useful for Frailty Screening in Older Adults. Clin. Interv. Aging 2019, 14, 693–699. [Google Scholar] [CrossRef]
- Petersen, R.C.; Lopez, O.; Armstrong, M.J.; Getchius, T.S.D.; Ganguli, M.; Gloss, D.; Gronseth, G.S.; Marson, D.; Pringsheim, T.; Day, G.S.; et al. Practice Guideline Update Summary: Mild Cognitive Impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 2018, 90, 126–135. [Google Scholar] [CrossRef]
- Petersen, R.C.; Smith, G.E.; Waring, S.C.; Ivnik, R.J.; Tangalos, E.G.; Kokmen, E. Mild Cognitive Impairment: Clinical Characterization and Outcome. Arch. Neurol. 1999, 56, 303. [Google Scholar] [CrossRef]
- Shapiro, A.M.; Benedict, R.H.; Schretlen, D.; Brandt, J. Construct and Concurrent Validity of the Hopkins Verbal Learning Test—Revised. Clin. Neuropsychol. 1999, 13, 348–358. [Google Scholar] [CrossRef] [PubMed]
- Benedict, R.H.; Schretlen, D.; Groninger, L.; Brandt, J. Hopkins Verbal Learning Test—Revised: Normative Data and Analysis of Inter-Form and Test-Retest Reliability. Clin. Neuropsychol. 1998, 12, 43–55. [Google Scholar] [CrossRef]
- Vogel, A.; Stokholm, J.; Jørgensen, K. Performances on Symbol Digit Modalities Test, Color Trails Test, and Modified Stroop Test in a Healthy, Elderly Danish Sample. Aging Neuropsychol. Cogn. 2013, 20, 370–382. [Google Scholar] [CrossRef] [PubMed]
- Bowie, C.R.; Harvey, P.D. Administration and Interpretation of the Trail Making Test. Nat. Protoc. 2006, 1, 2277–2281. [Google Scholar] [CrossRef]
- Ivnik, R.J.; Malec, J.F.; Smith, G.E.; Tangalos, E.G.; Petersen, R.C. Neuropsychological Tests’ Norms above Age 55: COWAT, BNT, MAE Token, WRAT-R Reading, AMNART, STROOP, TMT, and JLO. Clin. Neuropsychol. 1996, 10, 262–278. [Google Scholar] [CrossRef]
- Stokholm, J.; Jørgensen, K.; Vogel, A. Performances on Five Verbal Fluency Tests in a Healthy, Elderly Danish Sample. Aging Neuropsychol. Cogn. 2013, 20, 22–33. [Google Scholar] [CrossRef]
- Fällman, K.; Lundgren, L.; Wressle, E.; Marcusson, J.; Classon, E. Normative Data for the Oldest Old: Trail Making Test A, Symbol Digit Modalities Test, Victoria Stroop Test and Parallel Serial Mental Operations. Aging Neuropsychol. Cogn. 2020, 27, 567–580. [Google Scholar] [CrossRef]
- Verghese, J.; Wang, C.; Lipton, R.B.; Holtzer, R. Motoric Cognitive Risk Syndrome and the Risk of Dementia. J. Gerontol. Ser. A 2013, 68, 412–418. [Google Scholar] [CrossRef]
- Thomas, K.R.; Edmonds, E.C.; Eppig, J.S.; Wong, C.G.; Weigand, A.J.; Bangen, K.J.; Jak, A.J.; Delano-Wood, L.; Galasko, D.R.; Salmon, D.P.; et al. MCI-to-normal Reversion Using Neuropsychological Criteria in the Alzheimer’s Disease Neuroimaging Initiative. Alzheimer’s Dement. 2019, 15, 1322–1332. [Google Scholar] [CrossRef]
- Petersen, R. Mild Cognitive Impairment: Current Research and Clinical Implications. Semin. Neurol. 2007, 27, 22–31. [Google Scholar] [CrossRef]
- Klausen, H.H.; Petersen, J.; Bandholm, T.; Juul-Larsen, H.G.; Tavenier, J.; Eugen-Olsen, J.; Andersen, O. Association between Routine Laboratory Tests and Long-Term Mortality among Acutely Admitted Older Medical Patients: A Cohort Study. BMC Geriatr. 2017, 17, 62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- D’Hoore, W.; Bouckaert, A.; Tilquin, C. Practical Considerations on the Use of the Charlson Comorbidity Index with Administrative Data Bases. J. Clin. Epidemiol. 1996, 49, 1429–1433. [Google Scholar] [CrossRef]
- Deyo, R.A. Adapting A Clinical Comorbidity Index For Use With ICD-G-CM Administrative Databases. J. Clin. Epidemiol. 1992, 45, 613–619. [Google Scholar] [CrossRef]
- Patrick, S.R.; Leslie, L.R.; James, G. Jollis Adapting a Clinical Comorbidity Index for Use with ICD-9-CM Administrative Data: Differin Perspectives. J. Clin. Epidemiol. 1993, 46, 1075–1079. [Google Scholar]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.-M.; Sundararajan, V. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data From 6 Countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef]
- Renom-Guiteras, A.; Meyer, G.; Thürmann, P.A. The EU(7)-PIM List: A List of Potentially Inappropriate Medications for Older People Consented by Experts from Seven European Countries. Eur. J. Clin. Pharm. 2015, 71, 861–875. [Google Scholar] [CrossRef]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A Review of the Measurement of Grip Strength in Clinical and Epidemiological Studies: Towards a Standardised Approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef]
- Mehmet, H.; Robinson, S.R.; Yang, A.W.H. Assessment of Gait Speed in Older Adults. J. Geriatr. Phys. Ther. 2020, 43, 42–52. [Google Scholar] [CrossRef]
- Jones, C.J.; Rikli, R.E.; Beam, W.C. A 30-s Chair-Stand Test as a Measure of Lower Body Strength in Community-Residing Older Adults. Res. Q. Exerc. Sport 1999, 70, 113–119. [Google Scholar] [CrossRef]
- Janssen, M.F.; Pickard, A.S.; Golicki, D.; Gudex, C.; Niewada, M.; Scalone, L.; Swinburn, P.; Busschbach, J. Measurement Properties of the EQ-5D-5L Compared to the EQ-5D-3L across Eight Patient Groups: A Multi-Country Study. Qual. Life Res. 2013, 22, 1717–1727. [Google Scholar] [CrossRef] [PubMed]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and Preliminary Testing of the New Five-Level Version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jørgensen, K.; Nielsen, T.R.; Nielsen, A.; Waldorff, F.B.; Høgh, P.; Jakobsen, S.; Gottrup, H.; Vestergaard, K.; Waldemar, G. Brief Assessment of Impaired Cognition (BASIC)—Validation of a New Dementia Case-finding Instrument Integrating Cognitive Assessment with Patient and Informant Report. Int. J. Geriatr. Psychiatry 2019, 34, 1724–1733. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, T.R.; Andersen, B.B.; Gottrup, H.; Lützhøft, J.H.; Høgh, P.; Waldemar, G. Validation of the Rowland Universal Dementia Assessment Scale for Multicultural Screening in Danish Memory Clinics. Dement. Geriatr. Cogn. Disord. 2013, 36, 354–362. [Google Scholar] [CrossRef]
- Schultz-Larsen, K.; Lomholt, R.K.; Kreiner, S. Mini-Mental Status Examination: A Short Form of MMSE Was as Accurate as the Original MMSE in Predicting Dementia. J. Clin. Epidemiol. 2007, 60, 260–267. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. Mini-Mental State. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Okuno, J.; Yanagi, H.; Tomura, S. Is Cognitive Impairment a Risk Factor for Poor Compliance among Japanese Elderly in the Community? Eur. J. Clin. Pharmacol. 2001, 57, 589–594. [Google Scholar] [CrossRef] [PubMed]
- Chudiak, A.; Uchmanowicz, I.; Mazur, G. Relation between Cognitive Impairment and Treatment Adherence in Elderly Hypertensive Patients. Clin. Interv. Aging 2018, 13, 1409–1418. [Google Scholar] [CrossRef]
- Laur, C.V.; McNicholl, T.; Valaitis, R.; Keller, H.H. Malnutrition or Frailty? Overlap and Evidence Gaps in the Diagnosis and Treatment of Frailty and Malnutrition. Appl. Physiol. Nutr. Metab. 2017, 42, 449–458. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older Adults: Evidence for a Phenotype. J. Gerontol. Ser. A Biol. Sci. Med Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef]
- Nationalt Videnscenter for Demens Behandling Af MCI. Available online: https://videnscenterfordemens.dk/da/behandling-af-mci (accessed on 1 March 2022).
- Lopez, O.L.; Becker, J.T.; Chang, Y.-F.; Sweet, R.A.; DeKosky, S.T.; Gach, M.H.; Carmichael, O.T.; McDade, E.; Kuller, L.H. Incidence of Mild Cognitive Impairment in the Pittsburgh Cardiovascular Health Study–Cognition Study. Neurology 2012, 79, 1599–1606. [Google Scholar] [CrossRef] [PubMed]
- Suhr, J.A.; Patterson, S.M.; Austin, A.W.; Heffner, K.L. The Relation of Hydration Status to Declarative Memory and Working Memory in Older Adults. J. Nutr. Health Aging 2010, 14, 840–843. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer Europe. Alzheimer Europe Dementia in Europe Yearbook 2019, Estimating the Prevalence of Dementia in Europe; Alzheimer Europe: Luxembourg, 2019. [Google Scholar]
- Bradford, A.; Kunik, M.E.; Schulz, P.; Williams, S.P.; Singh, H. Missed and Delayed Diagnosis of Dementia in Primary Care: Prevalence and Contributing Factors. Alzheimer Dis. Assoc. Disord. 2009, 23, 306–314. [Google Scholar] [CrossRef] [PubMed]

| MCI (n = 42) | n | noMCI (n = 47) | n | |
|---|---|---|---|---|
| Demographic Variables | ||||
| Age | 81.8 (9.1) | 42 | 77.1 (6.0) | 47 |
| Sex, female, n (%) | 20 (47.6) | 42 | 34 (72.3) | 47 |
| Smoking, n (%) * | 42 | 47 | ||
| Yes | 5 (11.9) | 6 (12.8) | ||
| Used to | 20 (47.6) | 19 (40.4) | ||
| Never | 17 (40.5) | 22 (46.8) | ||
| Education, n (%) * | 41 | 47 | ||
| Primary school | 13 (31.7) | 8 (17.0) | ||
| Secondary education | 20 (48.8) | 29 (61.7) | ||
| Higher education | 8 (19.5) | 10 (21.3) | ||
| Anthropometry | ||||
| Body weight, kg | 72.8 (23.8) | 42 | 77.2 (18.5) | 47 |
| BMI a | 25.1 (6.3) | 42 | 27.5 (5.4) | 47 |
| Physical Performance | ||||
| Max hand grip strength, kg | 24.5 (12.1) | 38 | 24.5 (9.8) | 46 |
| Gait speed, m/s | 0.7 (0.3) | 40 | 0.9 (0.3) | 46 |
| Social Variables | ||||
| Living alone, yes, n (%) * | 29 (69.0) | 42 | 31 (66.0) | 47 |
| Assistance, yes, n (%) | ||||
| Cleaning | 29 (70.7) | 41 | 25 (53.2) | 47 |
| Purchases | 19 (46.3) | 41 | 8 (17.0) | 47 |
| Dressing | 11 (26.8) | 41 | 1 (2.1) | 47 |
| Medication | 18 (43.9) | 41 | 2 (4.3) | 47 |
| Laundry | 20 (48.8) | 41 | 6 (12.8) | 47 |
| EQ-5D-5L b, VAS c | 63.3 (18.3) | 70.5 (18.6) | ||
| Cognitive Performance | ||||
| MMSE-score d ≤ 24, n (%) | 11 (26.2) | 42 | 1 (2.1) | 47 |
| MNA | Model Adjusted for | Beta (95 % CI) | p-Value |
|---|---|---|---|
| Baseline | Unadjusted | −1.29 (−2.30; −0.28) | 0.013 * |
| Age | −0.85 (−1.86; 0.17) | 0.100 | |
| Age, frailty ** | −0.92 (−1.95; 0.10) | 0.077 | |
| Age, comorbidity | −0.84 (−1.87; −0.17) | 0.102 | |
| Age, medication | −0.98 (−2.00; 0.05) | 0.061 | |
| Age, frailty, comorbidity, medication ** | −1.10 (−2.15; −0.06) | 0.039 * | |
| 4 w fw | Unadjusted | −1.64 (−2.57; −0.70) | <0.001 * |
| Age | −1.29 (−2.25; −0.34) | 0.009 * | |
| Age, frailty ** | −1.43 (−2.39; −0.46) | 0.004 * | |
| Age, comorbidity | −1.29 (−2.25; −0.33) | 0.009 * | |
| Age, medication | −1.29 (−2.27; −0.32) | 0.010 * | |
| Age, frailty, comorbidity, medication ** | −1.45 (−2.44; −0.45) | 0.005 * | |
| Change | Unadjusted | −0.34 (−1.32; 0.63) | 0.486 |
| Age | −0.44 (−1.47; 0.58) | 0.393 | |
| Age, frailty ** | −0.33 (−1.32; 0.67) | 0.513 | |
| Age, comorbidity | −0.44 (−1.47; 0.58) | 0.393 | |
| Age, medication | −0.24 (−1.22; 0.75) | 0.632 | |
| Age, frailty, comorbidity, medication ** | −0.34 (−1.41; 0.72) | 0.522 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bornæs, O.; Andersen, A.L.; Houlind, M.B.; Kallemose, T.; Tavenier, J.; Aharaz, A.; Nielsen, R.L.; Jørgensen, L.M.; Beck, A.M.; Andersen, O.; et al. Mild Cognitive Impairment Is Associated with Poorer Nutritional Status on Hospital Admission and after Discharge in Acutely Hospitalized Older Patients. Geriatrics 2022, 7, 95. https://doi.org/10.3390/geriatrics7050095
Bornæs O, Andersen AL, Houlind MB, Kallemose T, Tavenier J, Aharaz A, Nielsen RL, Jørgensen LM, Beck AM, Andersen O, et al. Mild Cognitive Impairment Is Associated with Poorer Nutritional Status on Hospital Admission and after Discharge in Acutely Hospitalized Older Patients. Geriatrics. 2022; 7(5):95. https://doi.org/10.3390/geriatrics7050095
Chicago/Turabian StyleBornæs, Olivia, Aino L. Andersen, Morten B. Houlind, Thomas Kallemose, Juliette Tavenier, Anissa Aharaz, Rikke L. Nielsen, Lillian M. Jørgensen, Anne M. Beck, Ove Andersen, and et al. 2022. "Mild Cognitive Impairment Is Associated with Poorer Nutritional Status on Hospital Admission and after Discharge in Acutely Hospitalized Older Patients" Geriatrics 7, no. 5: 95. https://doi.org/10.3390/geriatrics7050095








