Screening for Obstructive Sleep Apnea Among the Adult Population in the Northeastern Region of Romania
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Instruments
2.2.1. The STOP-Bang Questionnaire
2.2.2. Epworth Questionnaire—Daytime Sleepiness Scale (ESS)
2.3. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Analysis of the STOP-Bang Questionnaire
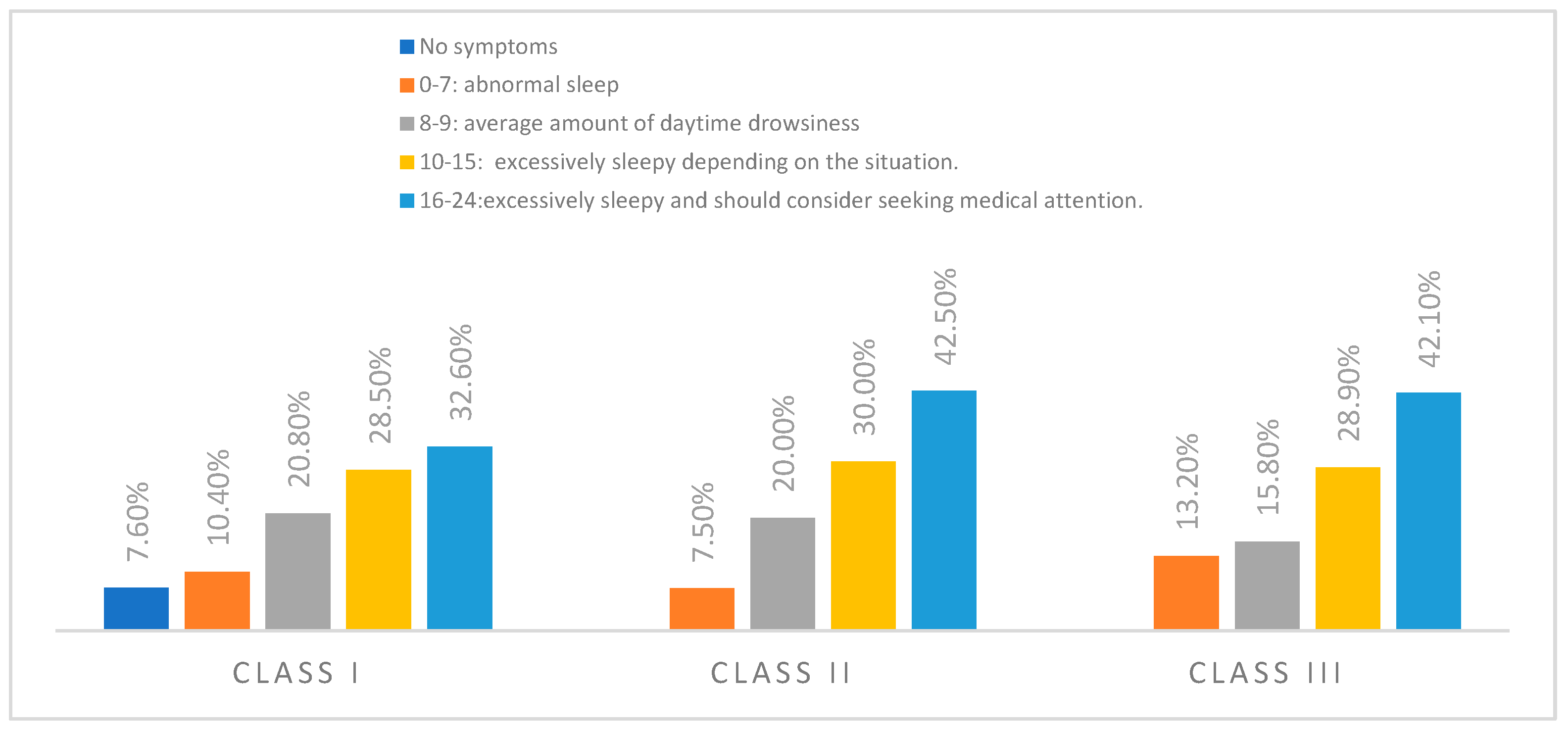
3.3. Epworth Questionnaire (ESS) Analysis
4. Discussion
4.1. Key Predictive Risk Factors
4.2. Screening Tool Performance and Practicality
4.3. Craniofacial Factors and OSA Risk
4.4. Study Limitations
4.5. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abramson, Z.; Susarla, S.M.; Lawler, M.; Bouchard, C.; Troulis, M.; Kaban, L.B. Three-dimensional computed tomographic airway analysis of patients with obstructive sleep apnea treated by maxillomandibular advancement. J. Oral. Maxillofac. Surg. 2011, 69, 677–686. [Google Scholar] [CrossRef]
- Schwartz, A.R.; Patil, S.P.; Laffan, A.M.; Polotsky, V.; Schneider, H.; Smith, P.L. Obesity and obstructive sleep apnea: Pathogenic mechanisms and therapeutic approaches. Proc. Am. Thorac. Soc. 2008, 5, 185–192. [Google Scholar] [CrossRef]
- Foster, G.D.; Borradaile, K.E.; Sanders, M.H.; Millman, R.; Zammit, G.; Newman, A.B.; Wadden, T.A.; Kelley, D.; Wing, R.R.; Pi-Sunyer, F.X.; et al. A randomized study on the effect of weight loss on obstructive sleep apnea among obese patients with type 2 diabetes: The Sleep AHEAD study. Arch. Intern. Med. 2009, 169, 1619–1626. [Google Scholar] [CrossRef]
- Jehan, S.; Zizi, F.; Pandi-Perumal, S.R.; Wall, S.; Auguste, E.; Myers, A.K.; Jean-Louis, G.; McFarlane, S.I. Obstructive Sleep Apnea and Obesity: Implications for Public Health. Sleep Med. Disord. 2017, 1, 00019. [Google Scholar] [PubMed]
- Bonsignore, M.R.; McNicholas, W.T.; Montserrat, J.M.; Eckel, J. Adipose tissue in obesity and obstructive sleep apnoea. Eur. Respir. J. 2012, 39, 746–767. [Google Scholar] [CrossRef]
- Somers, V.K.; Dyken, M.E.; Clary, M.P.; Abboud, F.M. Sympathetic neural mechanisms in obstructive sleep apnea. J. Clin. Investig. 1995, 96, 1897–1904. [Google Scholar] [CrossRef] [PubMed]
- Somers, V.K.; Mark, A.L.; Zavala, D.C.; Abboud, F.M. Contrasting effects of hypoxia and hypercapnia on ventilation and sympathetic activity in humans. J. Appl. Physiol. 1989, 67, 2101–2106. [Google Scholar] [CrossRef] [PubMed]
- Kapur, V.K. Obstructive sleep apnea: Diagnosis, epidemiology, and economics. Respir. Care 2010, 55, 1155–1167. [Google Scholar]
- Hla, K.M.; Young, T.B.; Bidwell, T.; Palta, M.; Skatrud, J.B.; Dempsey, J. Sleep apnea and hypertension. A population-based study. Ann. Intern. Med. 1994, 120, 382–388. [Google Scholar] [CrossRef]
- Nieto, F.J.; Young, T.B.; Lind, B.K.; Shahar, E.; Samet, J.M.; Redline, S.; D’Agostino, R.B.; Newman, A.B.; Lebowitz, M.D.; Pickering, T.G. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 2000, 283, 1829–1836. [Google Scholar] [CrossRef]
- Schäfer, H.; Koehler, U.; Ewig, S.; Hasper, E.; Tasci, S.; Lüderitz, B. Obstructive sleep apnea as a risk marker in coronary artery disease. Cardiology 1999, 92, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Marshall, N.S.; Wong, K.K.H.; Liu, P.Y.; Cullen, S.R.J.; Knuiman, M.W.; Grunstein, R.R. Sleep apnea as an independent risk factor for all-cause mortality: The Busselton Health Study. Sleep 2008, 31, 1079–1085. [Google Scholar]
- Young, T.; Finn, L.; Peppard, P.E.; Szklo-Coxe, M.; Austin, D.; Nieto, F.J.; Stubbs, B.R.; Hla, K.M. Sleep disordered breathing and mortality: Eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 2008, 31, 1071–1078. [Google Scholar] [PubMed]
- Yaggi, H.K.; Concato, J.; Kernan, W.N.; Lichtman, J.H.; Brass, L.M.; Mohsenin, V. Obstructive sleep apnea as a risk factor for stroke and death. N. Engl. J. Med. 2005, 353, 2034–2041. [Google Scholar] [CrossRef] [PubMed]
- Punjabi, N.M. The epidemiology of adult obstructive sleep apnea. Proc. Am. Thorac. Soc. 2008, 5, 136–143. [Google Scholar] [CrossRef]
- Young, T.; Evans, L.; Finn, L.; Palta, M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 1997, 20, 705–706. [Google Scholar] [CrossRef]
- Flemons, W.W.; Whitelaw, W.A.; Brant, R.; Remmers, J.E. Likelihood ratios for a sleep apnea clinical prediction rule. Am. J. Respir. Crit. Care Med. 1994, 150, 1279–1285. [Google Scholar] [CrossRef]
- Hoffstein, V.; Szalai, J.P. Predictive value of clinical features in diagnosing obstructive sleep apnea. Sleep 1993, 16, 118–122. [Google Scholar]
- Kump, K.; Whalen, C.; Tishler, P.V.; Browner, I.; Ferrette, V.; Strohl, K.P.; Rosenberg, C.; Redline, S. Assessment of the validity and utility of a sleep-symptom questionnaire. Am. J. Respir. Crit. Care Med. 1994, 150, 735–741. [Google Scholar] [CrossRef]
- Maislin, G.; Pack, A.I.; Kribbs, N.B.; Smith, P.L.; Schwartz, A.R.; Kline, L.R.; Schwab, R.J.; Dinges, D.F. A survey screen for prediction of apnea. Sleep 1995, 18, 158–166. [Google Scholar] [CrossRef]
- Viner, S.; Szalai, J.P.; Hoffstein, V. Are history and physical examination a good screening test for sleep apnea? Ann. Intern. Med. 1991, 115, 356–359. [Google Scholar] [CrossRef]
- Abrishami, A.; Khajehdehi, A.; Chung, F. A systematic review of screening questionnaires for obstructive sleep apnea. Can. J. Anaesth. 2010, 57, 423–438. [Google Scholar] [CrossRef] [PubMed]
- Douglass, A.B.; Bomstein, R.; Nino-Murcia, G.; Keenan, S.; Miles, L.; Zarcone, V.P.; Guilleminault, C.; Dement, W.C. The Sleep Disorders Questionnaire. I: Creation and multivariate structure of SDQ. Sleep 1994, 17, 160–167. [Google Scholar] [CrossRef]
- Netzer, N.C.; Stoohs, R.A.; Netzer, C.M.; Clark, K.; Strohl, K.P. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann. Intern. Med. 1999, 131, 485–491. [Google Scholar] [CrossRef]
- Chung, F.; Yegneswaran, B.; Liao, P.; Chung, S.A.; Vairavanathan, S.; Islam, S.; Khajehdehi, A.; Shapiro, C.M. STOP questionnaire: A tool to screen patients for obstructive sleep apnea. Anesthesiology 2008, 108, 812–821. [Google Scholar] [CrossRef]
- Chung, F.; Subramanyam, R.; Liao, P.; Sasaki, E.; Shapiro, C.; Sun, Y. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br. J. Anaesth. 2012, 108, 768–775. [Google Scholar] [CrossRef] [PubMed]
- Farney, R.J.; Walker, B.S.; Farney, R.M.; Snow, G.L.; Walker, J.M. The STOP-Bang equivalent model and prediction of severity of obstructive sleep apnea: Relation to polysomnographic measurements of the apnea/hypopnea index. J. Clin. Sleep Med. 2011, 7, 459–465. [Google Scholar] [CrossRef]
- Nunes, F.S.; Danzi-Soares, N.J.; Genta, P.R.; Drager, L.F.; Cesar, L.A.; Lorenzi-Filho, G. Critical evaluation of screening questionnaires for obstructive sleep apnea in patients undergoing coronary artery bypass grafting and abdominal surgery. Sleep Breath. 2015, 19, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Silva, G.E.; Vana, K.D.; Goodwin, J.L.; Sherrill, D.L.; Quan, S.F. Identification of patients with sleep disordered breathing: Comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth sleepiness scales. J. Clin. Sleep Med. 2011, 7, 467–472. [Google Scholar] [CrossRef]
- Oshita, H.; Fuchita, H.; Ito, N.; Senoo, M.; Isoyama, S.; Yamamoto, Y.; Yoshida, A.; Osaki, K.; Kawasaki, K.; Okusaki, K. Validation of the Japanese version of the STOP-Bang test for the risk assessment of obstructive sleep apnea syndrome. J. Jpn. Prim. Care Assoc. 2019, 42, 26–31. [Google Scholar] [CrossRef]
- Verwimp, J.; Ameye, L.; Bruyneel, M. Correlation between sleep parameters, physical activity and quality of life in somnolent moderate to severe obstructive sleep apnea adult patients. Sleep Breath. 2013, 17, 1039–1046. [Google Scholar] [CrossRef] [PubMed]
- Vana, K.D.; Silva, G.E.; Goldberg, R. Predictive abilities of the STOP-Bang and Epworth Sleepiness Scale in identifying sleep clinic patients at risk for obstructive sleep apnea. Res. Nurs. Health 2013, 36, 84–94. [Google Scholar] [CrossRef]
- Kim, H.C.; Kim, J.Y.; Lee, S.H.; Kim, D.K. Predictors for Presence and Severity of Obstructive Sleep Apnea in Snoring Patients. J. Sleep Med. 2015, 12, 47–52. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; Gu, W.; Li, Y.; Liu, M.; Li, Y.; Gao, X. Age-group-specific associations between the severity of obstructive sleep apnea and relevant risk factors in male and female patients. PLoS ONE 2014, 11, 9. [Google Scholar] [CrossRef]
- Westreich, R.; Gozlan-Talmor, A.; Geva-Robinson, S.; Schlaeffer-Yosef, T.; Slutsky, T.; Chen-Hendel, E.; Braiman, D.; Sherf, Y.; Arotsker, N.; Abu-Fraiha, Y.; et al. The Presence of Snoring as Well as its Intensity Is Underreported by Women. J. Clin. Sleep Med. 2019, 15, 471–476. [Google Scholar] [CrossRef]
- Gharib, A.; Loza, S. Factors affecting the severity of the apnea hypoapnea index: A retrospective study on 838 Egyptian patients diagnosed with obstructive sleep apnea. Egypt. J. Bronchol. 2020, 14, 34. [Google Scholar] [CrossRef]
- Tkacova, R.; McNicholas, W.T.; Javorsky, M.; Fietze, I.; Sliwinski, P.; Parati, G.; Grote, L.; Hedner, J. Nocturnal intermittent hypoxia predicts prevalent hypertension in the European sleep Apnoea database cohort study. Eur. Respir. J. 2014, 44, 931–941. [Google Scholar] [CrossRef]
- Tanigawa, T.; Tachibana, N.; Yamagishi, K.; Muraki, I.; Kudo, M.; Ohira, T.; Kitamura, A.; Sato, S.; Shimamoto, T.; Iso, H. Relationship between sleep-disordered breathing and blood pressure levels in community-based samples of Japanese men. Hypertens. Res. 2004, 27, 479–484. [Google Scholar] [CrossRef]
- Appleton, S.L.; Gill, T.K.; Lang, C.J.; Taylor, A.W.; McEvoy, R.D.; Stocks, N.P.; González-Chica, D.A.; Adams, R.J. Prevalence and comorbidity of sleep conditions in Australian adults: 2016 sleep Health Foundation national survey. Sleep Health 2018, 4, 13–19. [Google Scholar] [CrossRef]
- Zhou, X.; Zhou, B.; Li, Z.; Lu, Q.; Li, S.; Pu, Z.; Luo, F. Gender differences of clinical and polysomnographic findings with obstructive sleep apnea syndrome. Sci. Rep. 2021, 11, 5938. [Google Scholar] [CrossRef]
- Bixler, E.O.; Vgontzas, A.N.; Lin, H.M.; Have, T.T.; Rein, J.; Vela-Bueno, A.; Kales, A. Prevalence of sleep-disordered breathing in women: Effects of gender. Am. J. Respir. Crit. Care Med. 2001, 163, 608–613. [Google Scholar] [CrossRef] [PubMed]
- Redline, S.; Kump, K.; Tishler, P.V.; Browner, I.; Ferrette, V. Gender differences in sleep disordered breathing in a community-based sample. Am. J. Respir. Crit. Care Med. 1994, 149, 722–726. [Google Scholar] [CrossRef] [PubMed]
- Perger, E.; Mattaliano, P.; Lombardi, C. Menopause and sleep apnea. Maturitas 2019, 124, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Botnaru, V.; Corlateanu, A.; Moldovanu, I. Sindromul de Apnee Obstructivă în Somn: Protocol Clinic Naţional PCN-276; Ministerul Sănătății al Republicii Moldova: Chișinău, Moldova, 2017.
- Asavasupreechar, T.; Saito, R.; Edwards, D.P.; Sasano, H.; Boonyaratanakornkit, V. Progesterone receptor isoform B expression in pulmonary neuroendocrine cells decreases cell proliferation. J. Steroid Biochem. 2019, 190, 212–223. [Google Scholar] [CrossRef]
- Thompson, C.; Legault, J. A portrait of obstructive sleep apnea risk factors in middle-aged and older adults in the Canadian Longitudinal Study on Aging. Sci. Rep. 2022, 12, 5127. [Google Scholar] [CrossRef]
- Siwasaranond, N.; Nimitphong, H.; Manodpitipong, A.; Saetung, S.; Chirakalwasan, N.; Thakkinstian, A.; Reutrakul, S. The Relationship between Diabetes-Related Complications and Obstructive Sleep Apnea in Type 2 Diabetes. J. Diabetes Res. 2018, 2018, 9269170. [Google Scholar] [CrossRef]
- Mokhlesi, B.; Ham, S.A.; Gozal, D. The effect of sex and age on the comorbidity burden of OSA: An observational analysis from a large nationwide US health claims database. Eur. Respir. J. 2016, 47, 1162–1169. [Google Scholar] [CrossRef]
- Senaratna, C.V.; Perret, J.L.; Lodge, C.J.; Lowe, A.J.; Campbell, B.E.; Matheson, M.C.; Hamilton, G.S.; Dharmage, S.C. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med. Rev. 2017, 34, 70–81. [Google Scholar] [CrossRef]
- Engleman, H.M.; Douglas, N.J. Sleepiness, cognitive function, and quality of life in obstructive sleep apnoea/hypopnoea syndrome. Thorax 2004, 59, 618–622. [Google Scholar] [CrossRef]
- Chiu, H.Y.; Chen, P.Y.; Chuang, L.P.; Chen, N.H.; Tu, Y.K.; Hsieh, Y.J.; Wang, Y.C.; Guilleminault, C. Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP, and Epworth sleepiness scale in detecting obstructive sleep apnea: A bivariate meta-analysis. Sleep Med. Rev. 2017, 36, 57–70. [Google Scholar] [CrossRef] [PubMed]
- Kimoff, R.S. Obstructive Sleep Apnea. In International Encyclopedia of Public Health, 6th ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2016; pp. 308–314. [Google Scholar]
- Chan, A.S.; Phillips, C.L.; Cistulli, P.A. Obstructive sleep apnoea—An update. Intern. Med. J. 2010, 40, 102–106. [Google Scholar] [CrossRef]
- Marshall, N.S.; Wong, K.K.; Phillips, C.L.; Liu, P.Y.; Knuiman, M.W.; Grunstein, R.R. Is sleep apnea an independent risk factor for prevalent and incident diabetes in the Busselton Health Study? J. Clin. Sleep Med. 2009, 5, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Vasu, T.S.; Grewal, R.; Doghramji, K. Obstructive sleep apnea syndrome and perioperative complications: A systematic review of the literature. J. Clin. Sleep Med. 2012, 8, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Vasu, T.S.; Doghramji, K.; Cavallazzi, R.; Grewal, R.; Hirani, A.; Leiby, B.; Markov, D.; Reiter, D.; Kraft, W.K.; Witkowski, T. Obstructive Sleep Apnea Syndrome and Postoperative Complications: Clinical Use of the STOP-Bang Questionnaire. Sleep Med. 2012, 13, 929–934. [Google Scholar] [CrossRef]
- Pack, A.I.; Gislason, T. Obstructive sleep apnea and cardiovascular disease: A perspective and future directions. Prog. Cardiovasc. Dis. 2009, 51, 434–451. [Google Scholar] [CrossRef]
- Bearpark, H.; Elliott, L.; Grunstein, R.; Cullen, S.; Schneider, H.; Althaus, W.; Sullivan, C. Snoring and sleep apnea. A population study in Australian men. Am. J. Respir. Crit. Care Med. 1995, 151, 1459–1465. [Google Scholar] [CrossRef]
- Ip, M.S.; Lam, B.; Tang, L.C.; Lauder, I.J.; Ip, T.Y.; Lam, W.K. A community study of sleep-disordered breathing in middle-aged Chinese women in Hong Kong: Prevalence and gender differences. Chest 2004, 125, 127–134. [Google Scholar] [CrossRef]
- Pirelli, P.; Saponara, M.; Guilleminault, C. Rapid maxillary expansion before and after adenotonsillectomy in children with obstructive sleep apnea. Somnologie 2012, 16, 125–132. [Google Scholar] [CrossRef]
- Abdolreza, J.; Saeed, K.; Alireza, D. Treatment Protocol for Skeletal Class III Malocclusion in Growing Patients. In Motamedi MH. A Textbook of Advanced Oral and Maxillofacial Surgery; IntechOpen: London, UK, 2016; Volume 3. [Google Scholar]
- Schwab, R.J.; Pasirstein, M.; Pierson, R.; Mackley, A.; Hachadoorian, R.; Arens, R.; Maislin, G.; Pack, A.I. Identification of upper air-way anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am. J. Respir. Crit. Care Med. 2003, 168, 522–530. [Google Scholar] [CrossRef]
- Neelapu, B.C.; Kharbanda, O.P.; Sardana, H.K.; Balachandran, R.; Sardana, V.; Kapoor, P.; Gupta, A.; Vasamsetti, S. Craniofacial and upper airway morphology in adult obstructive sleep apnea patients: A systematic review and meta-analysis of cephalometric studies. Sleep Med. Rev. 2017, 31, 79–90. [Google Scholar] [CrossRef] [PubMed]

| No | % | |
|---|---|---|
| Age | 61.25 ± 7.165 Years (Minimum Age: 42, Maximum Age: 75) | |
| Gender | ||
| Female | 91 | 41.0 |
| Male | 131 | 59.0 |
| Residence | ||
| Urban | 151 | 68.0 |
| Rural | 71 | 32.0 |
| Socio-economic level | ||
| High socio-economic level | 125 | 56.3 |
| Medium socio-economic level | 68 | 30.6 |
| Low socio-economic level | 29 | 13.1 |
| Distribution of participants diagnosed with OSA | ||
| No | 190 | 85.6 |
| Yes | 32 | 14.4 |
| Distribution of participants according to BMI | ||
| Normal weight (<25 kg/m2) | 1 | .5 |
| Overweight (25–30 kg/m2) | 75 | 33.8 |
| Obese (>30 kg/m2) | 146 | 65.8 |
| Distribution of participants according to associated pathologies | ||
| No | 15 | 6.8 |
| Yes | 207 | 93.2 |
| Gender | BMI | Associated Pathologies | ||||||
|---|---|---|---|---|---|---|---|---|
| Female | Male | Normal Weight | Increased Weight | Obese | No | Yes | ||
| You snore loudly | No | 33.0% | 22.9% | 100.0% | 46.7% | 16.4% | 100.0% | 21.7% |
| Yes | 67.0% | 77.1% | 53.3% | 83.6% | 78.3% | |||
| p | 0.097 | 0.000 | 0.000 | |||||
| You are tired, exhausted, or sleepy during the day | No | 31.9% | 38.9% | 74.7% | 16.4% | 80.0% | 32.9% | |
| Yes | 68.1% | 61.1% | 100.0% | 25.3% | 83.6% | 20.0% | 67.1% | |
| p | 0.281 | 0.000 | 0.000 | |||||
| You have sleep apnea | No | 49.5% | 45.0% | 74.7% | 32.9% | 80.0% | 44.4% | |
| Yes | 50.5% | 55.0% | 100.0% | 25.3% | 67.1% | 20.0% | 55.6% | |
| p | 0.517 | 0.000 | 0.008 | |||||
| You have high blood pressure | No | 60.4% | 49.6% | 100.0% | 60.0% | 50.7% | 86.7% | 51.7% |
| Yes | 39.6% | 50.4% | 40.0% | 49.3% | 13.3% | 48.3% | ||
| p | 0.112 | 0.275 | 0.009 | |||||
| You are over 50 years old | No | 2.2% | 8.4% | 100.0% | 16.0% | 86.7% | ||
| Yes | 97.8% | 91.6% | 84.0% | 100.0% | 13.3% | 100.0% | ||
| p | 0.053 | 0.000 | 0.000 | |||||
| Circumference <40 cm | 52.7% | 64.9% | 100.0% | 86.7% | 45.9% | 100.0% | 57.0% | |
| Circumference >41 cm | 47.3% | 35.1% | 13.3% | 54.1% | 43.0% | |||
| p | 0.070 | 0.000 | 0.001 | |||||
| Low risk of obstructive sleep apnea: “Yes” to 0–2 questions | 15.4% | 16.8% | 100.0% | 46.7% | 86.7% | 11.1% | ||
| Medium risk of obstructive sleep apnea: “Yes” to 3–4 questions | 27.5% | 32.8% | 41.3% | 25.3% | 32.9% | |||
| Increased risk of obstructive sleep apnea: “Yes” to 5–8 questions | 57.1% | 50.4% | 12.0% | 74.7% | 13.3% | 56.0% | ||
| p | 0.598 | 0.000 | 0.001 | |||||
| RISK | B | Std. Error | Wald | Sig. | Exp(B) | 95% Confidence Interval for Exp(B) | ||
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| Low risk of obstructive sleep apnea | Intercept | −1.360 | 0.208 | 42.690 | 0.000 | |||
| [age2 = 1.00] | 1.697 | 0.621 | 7.453 | 0.006 | 5.455 | 1.614 | 18.441 | |
| Medium risk of obstructive sleep apnea | Intercept | −0.633 | 0.160 | 15.705 | 0.000 | |||
| [age2 = 1.00] | 1.103 | 0.592 | 3.471 | 0.062 | 3.013 | 0.944 | 9.616 | |
| Medium risk of obstructive sleep apnea | Intercept | −1.080 | 0.190 | 32.245 | 0.000 | |||
| [Body mass index = 1] | 0.529 | 0.000 | 1.698 | 1.698 | 1.698 | |||
| [Body mass index = 2] | 2.317 | 0.424 | 29.901 | 0.000 | 10.147 | 4.422 | 23.283 | |
| Gender | IMC | Associated Pathologies | |||||
|---|---|---|---|---|---|---|---|
| Female | Male | Normal Weight | Increased Weight | Obese > 30 kg/m2 | No | Yes | |
| Sitting and reading a book or a newspaper | |||||||
| Never doze/fall asleep | 2.2% | 8.4% | 100.0% | 16.0% | 86.7% | ||
| Low probability of dozing/falling asleep | 13.2% | 24.4% | 58.7% | 21.3% | |||
| Moderate likelihood of dozing/falling asleep | 62.6% | 38.2% | 25.3% | 60.3% | 51.7% | ||
| High probability of dozing/falling asleep | 22.0% | 29.0% | 39.7% | 13.3% | 27.1% | ||
| p | 0.002 | 0.000 | 0.000 | ||||
| Watching a show on TV | |||||||
| Never doze/fall asleep | 2.2% | 8.4% | 100.0% | 16.0% | 86.7% | ||
| Low probability of dozing/falling asleep | 16.0% | 28.0% | 10.1% | ||||
| Moderate likelihood of dozing/falling asleep | 48.4% | 38.9% | 56.0% | 36.3% | 45.9% | ||
| High probability of dozing/falling asleep | 49.5% | 36.6% | 63.7% | 13.3% | 44.0% | ||
| p | 0.000 | 0.000 | 0.000 | ||||
| Sitting, inactive, in a public place (cinema, theatre, waiting room) | |||||||
| Never doze/fall asleep | 2.2% | 24.4% | 100.0% | 44.0% | 86.7% | 10.1% | |
| Low probability of dozing/falling asleep | 2.2% | 16.0% | 25.3% | 2.7% | 11.1% | ||
| Moderate likelihood of dozing/falling asleep | 78.0% | 46.6% | 30.7% | 74.7% | 13.3% | 62.8% | |
| High probability of dozing/falling asleep | 17.6% | 13.0% | 22.6% | 15.9% | |||
| p | 0.000 | 0.000 | 0.000 | ||||
| Passenger in a vehicle for a trip of at least 1 h | |||||||
| Never doze/fall asleep | 1.1% | 8.4% | 100.0% | 14.7% | 80.0% | ||
| Low probability of dozing/falling asleep | 3.3% | 32.1% | 54.7% | 2.7% | 6.7% | 21.3% | |
| Moderate likelihood of dozing/falling asleep | 35.2% | 24.4% | 43.8% | 13.3% | 30.0% | ||
| High probability of dozing/falling asleep | 60.4% | 35.1% | 30.7% | 53.4% | 48.8% | ||
| p | 0.000 | 0.00 | 0.000 | ||||
| Sitting in bed, after lunch | |||||||
| Never doze/fall asleep | 2.2% | 8.4% | 100.0% | 16.0% | 86.7% | ||
| Low probability of dozing/falling asleep | 13.2% | 24.4% | 58.7% | 21.3% | |||
| Moderate likelihood of dozing/falling asleep | 62.6% | 38.2% | 25.3% | 60.3% | 51.7% | ||
| High probability of dozing/falling asleep | 22.0% | 29.0% | 39.7% | 13.3% | 27.1% | ||
| p | 0.002 | 0.000 | 0.000 | ||||
| Sitting and talking to someone | |||||||
| Never doze/fall asleep | 56.0% | 58.8% | 90.7% | 41.1% | 80.0% | 56.0% | |
| Low probability of dozing/falling asleep | 41.8% | 31.3% | 100.0% | 9.3% | 48.6% | 20.0% | 36.7% |
| Moderate likelihood of dozing/falling asleep | 2.2% | 9.9% | 10.3% | 7.2% | |||
| High probability of dozing/falling asleep | 56.0% | 58.8% | 90.7% | 41.1% | 80.0% | 56.0% | |
| p | 0.039 | 0.000 | 0.167 | ||||
| Seated, after a meal without alcoholic beverages | |||||||
| Never doze/fall asleep | 31.9% | 32.1% | 100.0% | 58.7% | 17.8% | 93.3% | 27.5% |
| Low probability of dozing/falling asleep | 30.8% | 32.8% | 41.3% | 27.4% | 6.7% | 33.8% | |
| Moderate likelihood of dozing/falling asleep | 37.4% | 35.1% | 54.8% | 38.6% | |||
| High probability of dozing/falling asleep | 31.9% | 32.1% | 100.0% | 58.7% | 17.8% | 93.3% | 27.5% |
| p | 0.929 | 0.000 | 0.000 | ||||
| Driving a car during a traffic stop lasting a few minutes | |||||||
| Never doze/fall asleep | 33.0% | 41.2% | 100.0% | 72.0% | 19.9% | 100.0% | 33.3% |
| Low probability of dozing/falling asleep | 45.1% | 35.9% | 28.0% | 45.9% | 42.5% | ||
| Moderate likelihood of dozing/falling asleep | 22.0% | 22.9% | 34.2% | 24.2% | |||
| p | 0.345 | 0.000 | 0.000 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanellari, O.; Alushi, A.; Toti, C.; Balcos, C.; Armencia, A.O.; Panaite, T.; Zetu, I. Screening for Obstructive Sleep Apnea Among the Adult Population in the Northeastern Region of Romania. Dent. J. 2025, 13, 208. https://doi.org/10.3390/dj13050208
Tanellari O, Alushi A, Toti C, Balcos C, Armencia AO, Panaite T, Zetu I. Screening for Obstructive Sleep Apnea Among the Adult Population in the Northeastern Region of Romania. Dentistry Journal. 2025; 13(5):208. https://doi.org/10.3390/dj13050208
Chicago/Turabian StyleTanellari, Olja, Adela Alushi, Celiana Toti, Carina Balcos, Adina Oana Armencia, Tinela Panaite, and Irina Zetu. 2025. "Screening for Obstructive Sleep Apnea Among the Adult Population in the Northeastern Region of Romania" Dentistry Journal 13, no. 5: 208. https://doi.org/10.3390/dj13050208
APA StyleTanellari, O., Alushi, A., Toti, C., Balcos, C., Armencia, A. O., Panaite, T., & Zetu, I. (2025). Screening for Obstructive Sleep Apnea Among the Adult Population in the Northeastern Region of Romania. Dentistry Journal, 13(5), 208. https://doi.org/10.3390/dj13050208








