Successful Correction of Crossbite with Multi-Segment Le Fort I Osteotomy in a Patient with Cleft Lip and Palate
Abstract
1. Introduction
2. Patient History
3. Clinical Findings
3.1. Initial Facial Findings (Figure 1A)

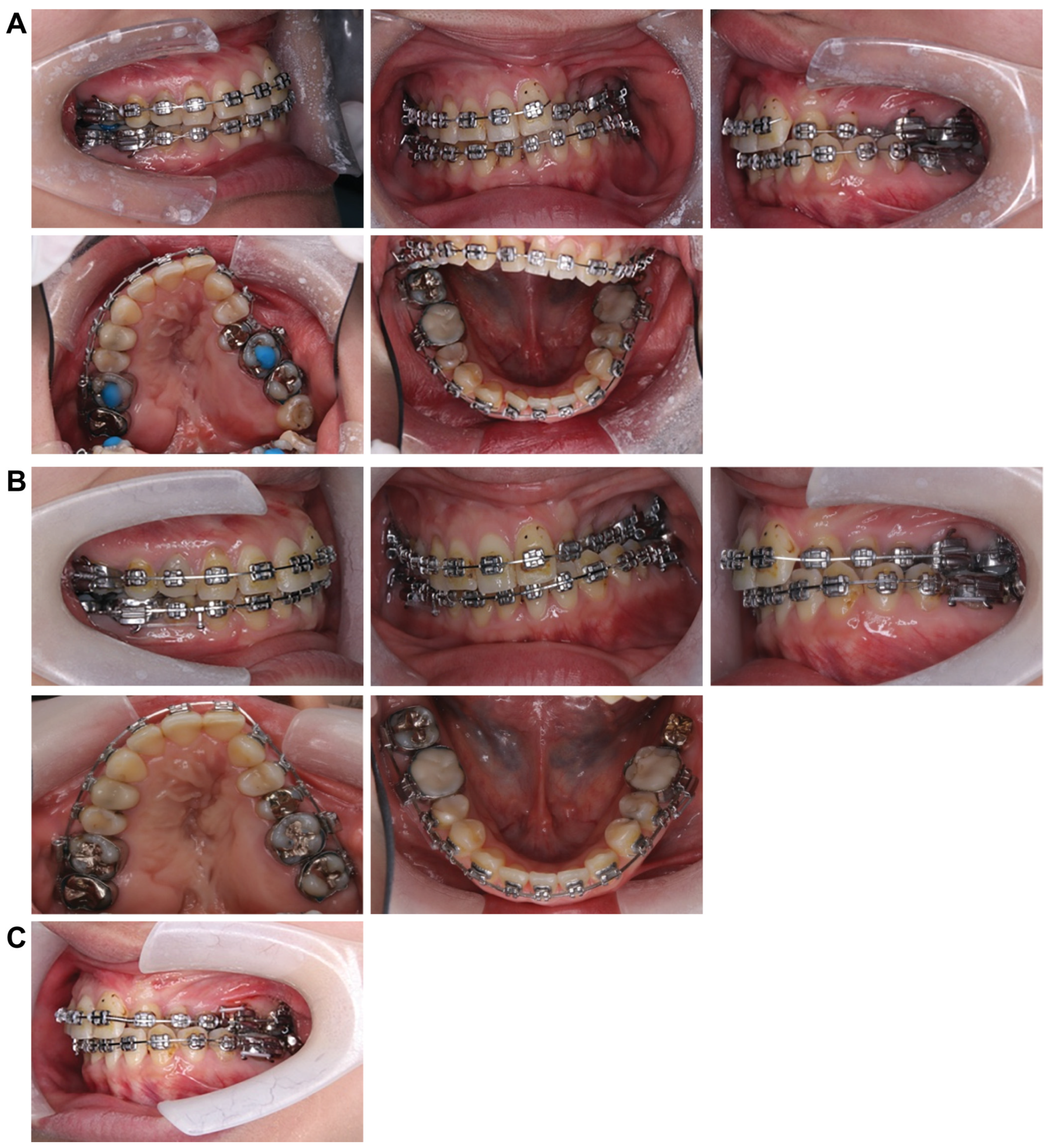
3.2. Intraoral Photo at First Visit (Figure 1B)
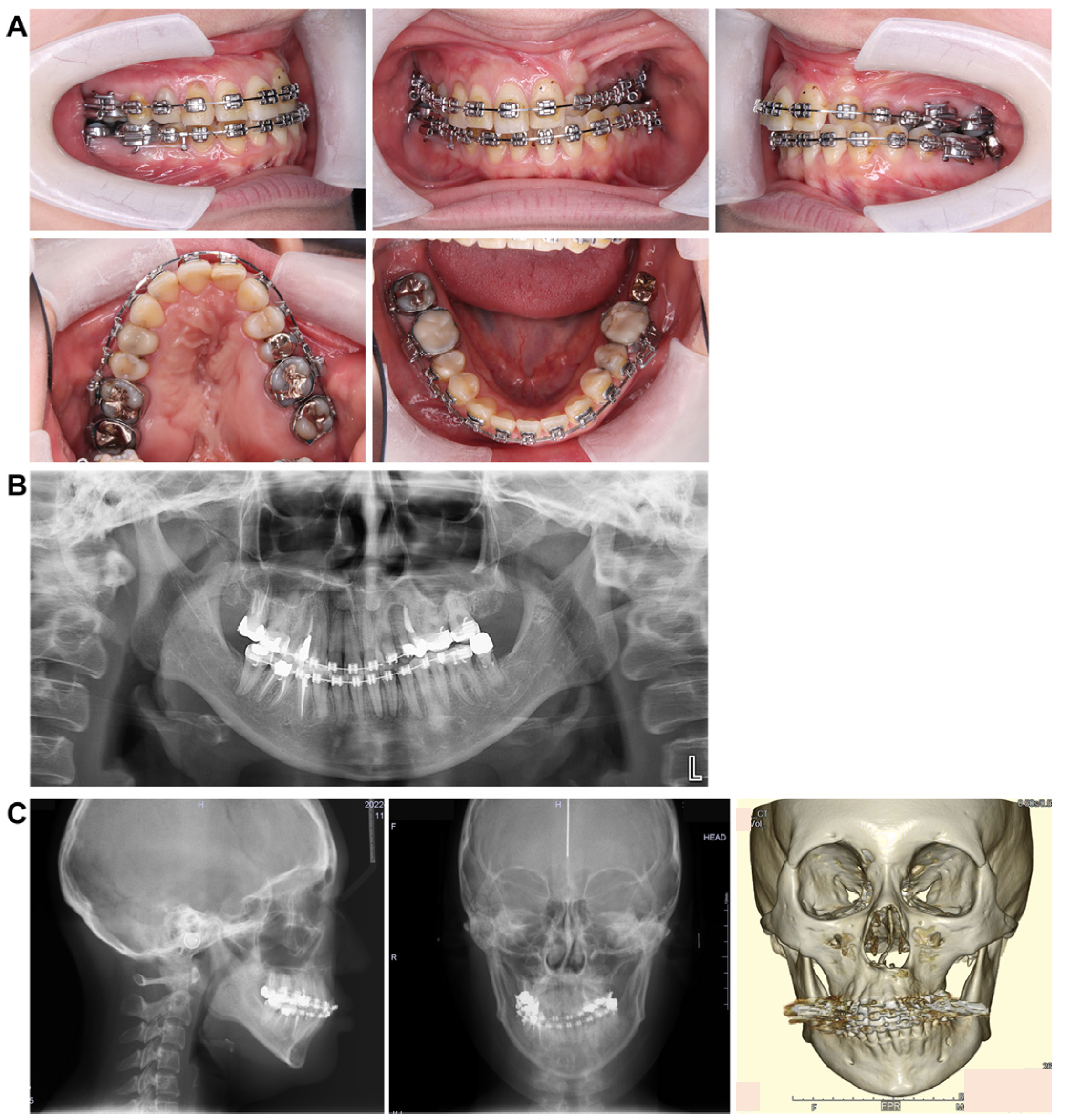
3.3. Panoramic Cephalometric Radiograph (Figure 2A)

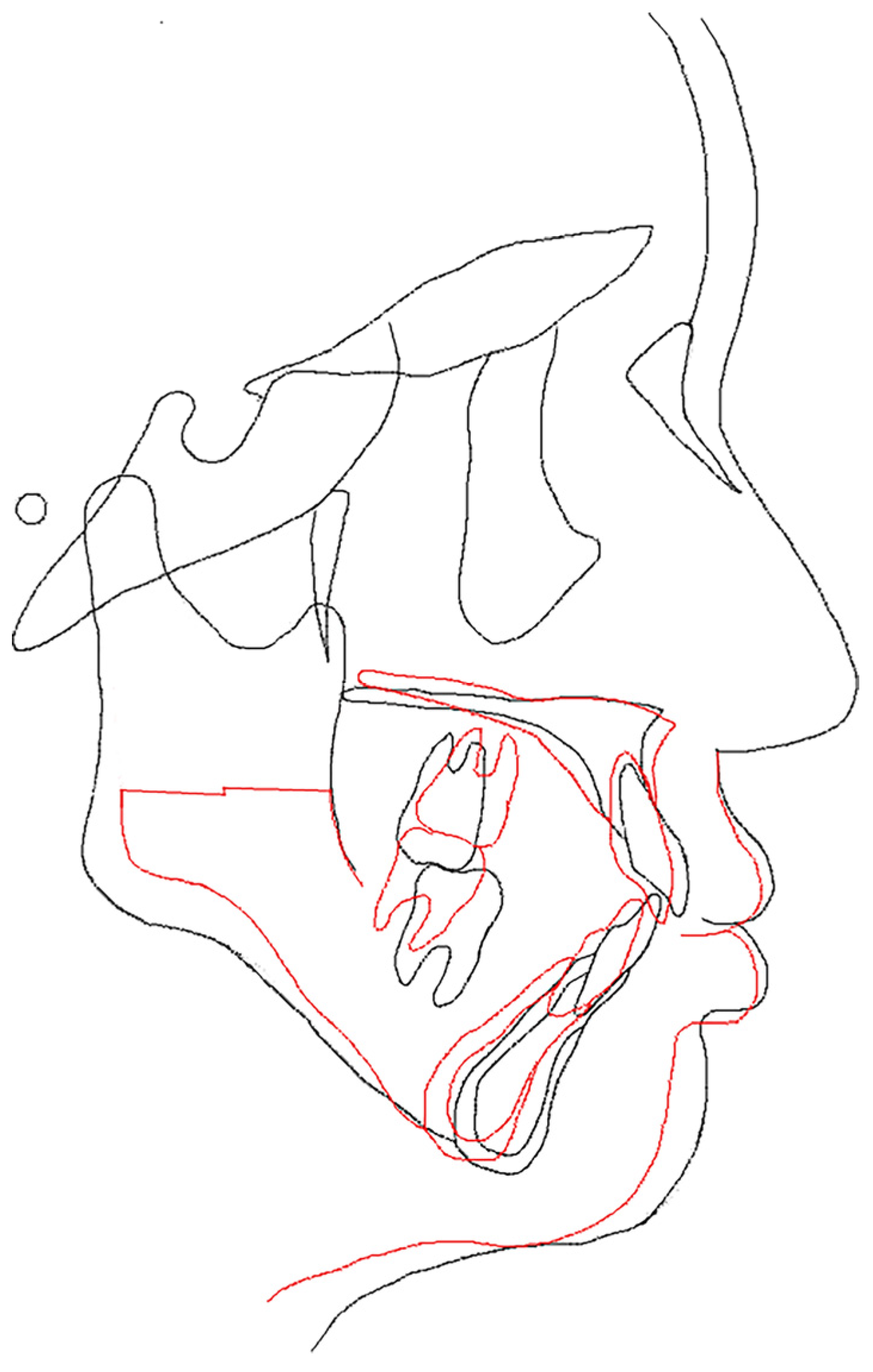
3.4. Lateral and Frontal Cephalometric Radiographs (Figure 2B)
3.5. Initial Examination of the Temporomandibular Joint
4. Diagnosis/Treatment Approach
5. Treatment Results
5.1. Facial Appearance Findings (Figure 9A)

5.2. Intraoral Findings (Figure 9B,C)
5.3. Panoramic Cephalometric Radiograph (Figure 9D)
5.4. Lateral and Frontal Cephalometric Radiographs (Figure 9E)
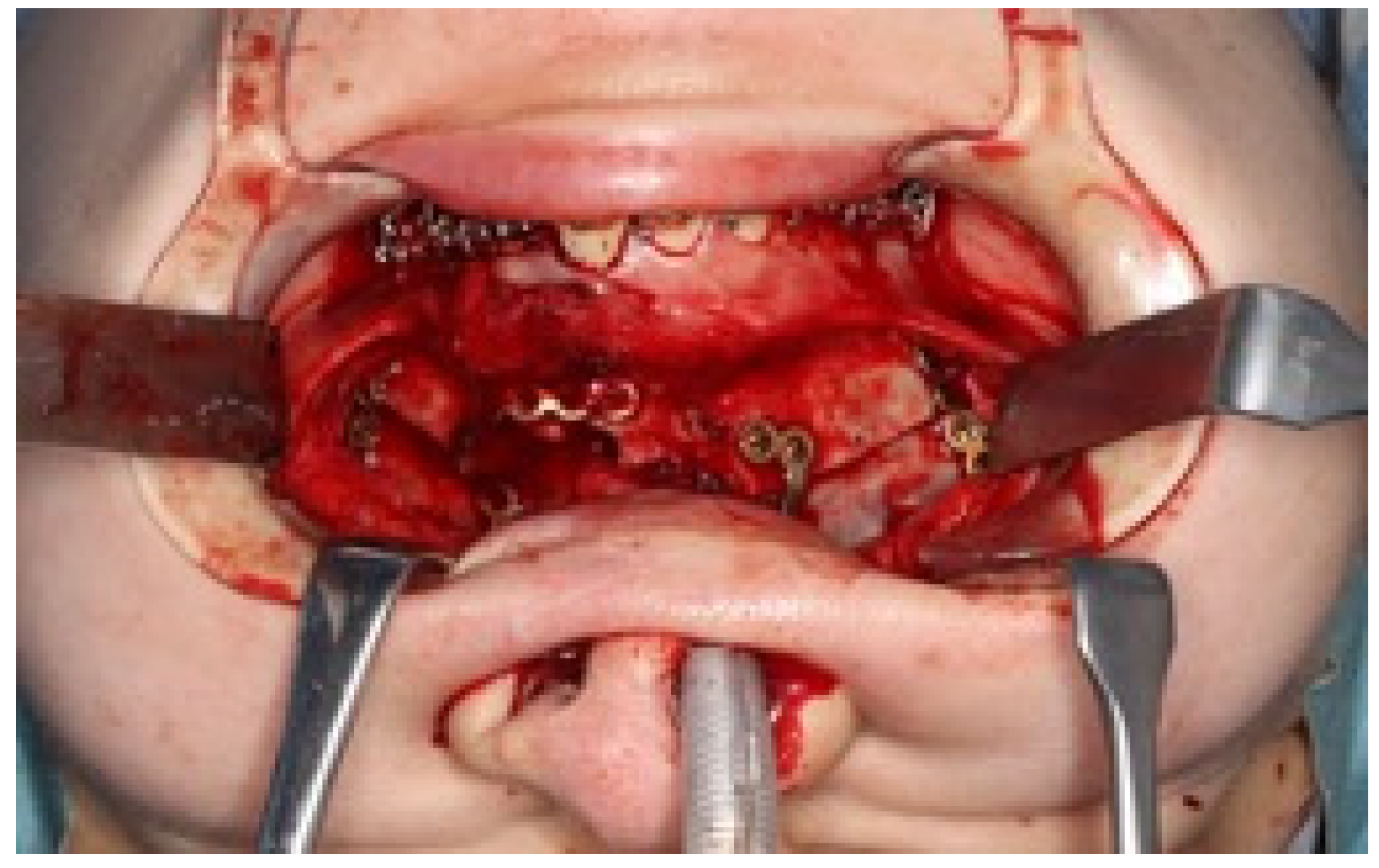
5.5. Treatment Progress
6. Discussion
6.1. Regarding the Treatment Plan
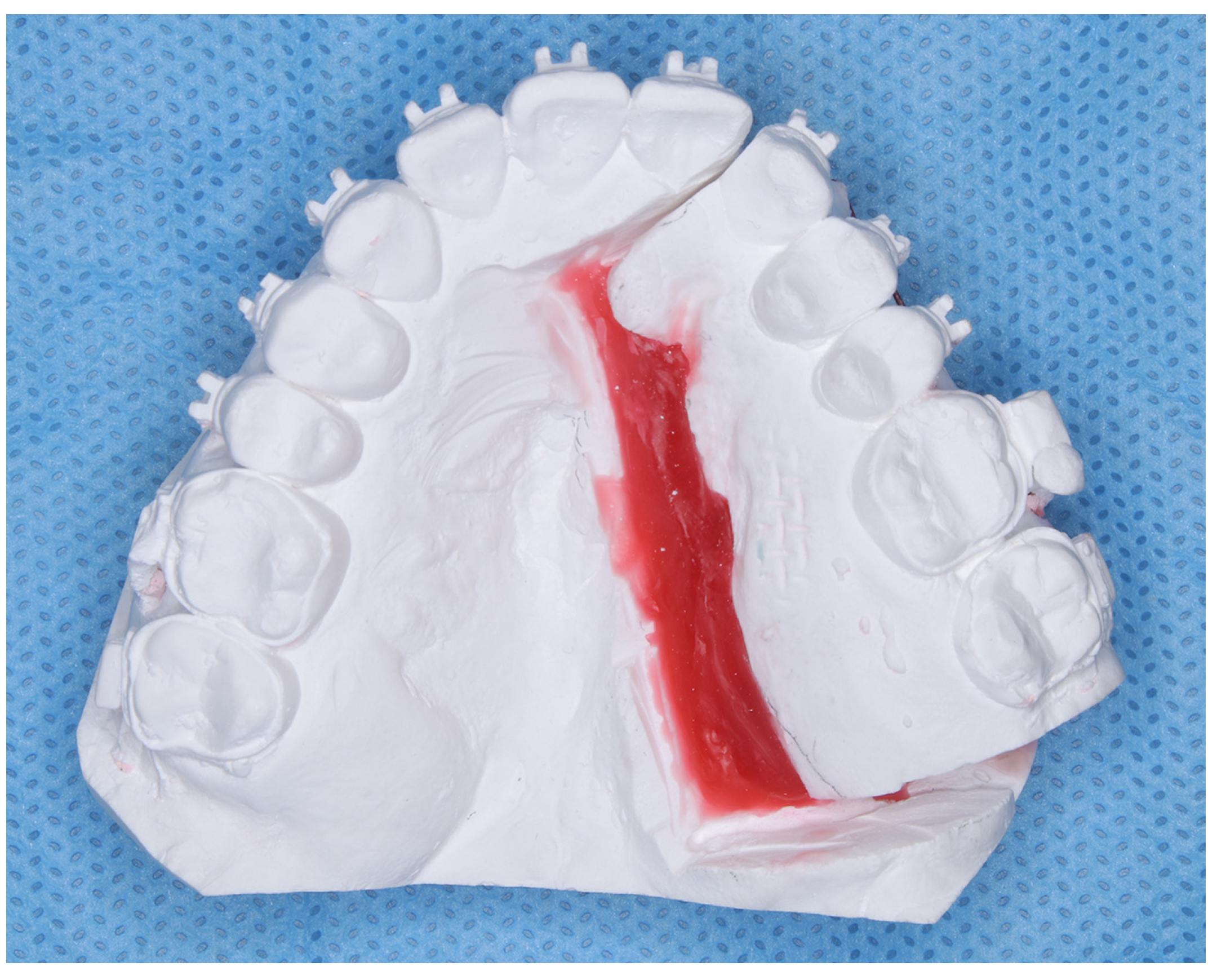
6.2. Lateral Expansion of the Maxillary Dental Arch
7. Research Limitations
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MARPE | Miniscrew-Assisted Rapid Palatal Expansion |
| SARPE | Surgically Assisted Rapid Palatal Expansion |
| SSRO | Sagittal Split Ramus Osteotomies |
References
- Paradowska-Stolarz, A.; Mikulewicz, M.; Duś-Ilnicka, I. Current concepts and challenges in the treatment of cleft lip and palate patients—A comprehensive review. J. Pers. Med. 2022, 12, 2089. [Google Scholar] [CrossRef] [PubMed]
- Ko, S.; Furutani, M.; Togo, Y.; Arimoto, A.; Hashikawa, N. Segmental Le Fort I osteotomy combined with horseshoe osteotomy for maxillary expansion. Jpn. J. Jaw Deform. 2023, 33, 1–9. [Google Scholar] [CrossRef]
- Yoshiaki, S.; Shuichi, Y.; Toru, O.; Takaaki, Y.; Toru, I.; Jyunichiro, I.; Yasuo, U.; Koichi, O.; Osamu, T.; Noboru, O.; et al. Study on disharmony of maxillary basal bone width and diameter and molar tooth axis in patients with jaw deformity. J. Jpn. Jaw Deform. Soc. 2001, 11, 21–28. [Google Scholar]
- Kusayama, M.; Motohashi, N.; Kuroda, T. Relationship between trans- verse dental anormalies and skeletal asymmetry. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 329–337. [Google Scholar] [CrossRef]
- Graber, T.M. Changing philosophies in cleft palate management. J. Pediatr. 1950, 37, 400–415. [Google Scholar] [CrossRef]
- Yudai, I.; Hidesato, H.; Teruhiko, F.; Hideyoshi, T.; Ryo, N.; Hiroshi, Y.; Haruhisa, N. Long-Term Management Case of Left-Sided Cleft Lip and Palate with Undergrowth of the Maxilla. J. Showa Acad. Società 2024, 84, 452–462. Available online: https://www.jstage.jst.go.jp/article/jshowaunivsoc/84/5/84_452/_pdf (accessed on 20 December 2024).
- Lagravere, M.O.; Major, P.W.; Flores-Mir, C. Long-term skeletal changes with rapid maxillary expansion: A systematic review. Angle Orthod. 2005, 75, 1046–1052. [Google Scholar] [CrossRef]
- Koudstaal, M.J.; Poort, L.J.; van der Wal, K.G.H.; Wolvius, E.B.; Prahl-Andersen, B.; Schulten, A.J.M. Surgically assisted rapid maxillary expansion (SARME): A review of the literature. Int. J. Oral. Maxillofac. Surg. 2005, 34, 709–714. [Google Scholar] [CrossRef]
- Yao, W.; Bekmezian, S.; Hardy, D.; Kushner, H.W.; Miller, A.J.; Huang, J.C.; Lee, J.S. Cone-beam computed tomographic comparison of surgically assisted rapid palatal expansion and multipiece Le Fort 1 osteotomy. J. Oral. Maxillofac. Surg. 2015, 73, 499–508. [Google Scholar] [CrossRef]
- Seeberger, R.; Gander, E.; Hoffmann, J.; Engel, M. Surgical management of crossbites in orthognathic surgery: Surgically assisted rapid maxillary expansion (SARPE) versus two-piece maxilla. J. Craniomaxillofac. Surg. 2015, 43, 1109–1112. [Google Scholar] [CrossRef]
- Marchetti, C.; Pironi, M.; Bianchi, A.; Musci, A. Surgically assisted rapid palatal expansion vs. segmental Le FortIosteotomy: Transverse stability over a 2-year period. J. Craniomaxillofac. Surg. 2009, 37, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Yuka, Y.; Itoh, S.; Inubushi, T.; Yokoyama, M.; Miyagawa, K.; Seki, S.; Susumu, T.; Aikawa, T.; Yamashiro, T. A case of skeletal class II open bite with narrow maxillary arch and CO-CR discrepancy treated by segmental Le. Fort, I osteotomy and sagittal split ramus osteotomy. J. Jpn. Jaw Deform. Soc. 2023, 33, 41–51. [Google Scholar]
- Arisa, O.; Kunihiko, N.; Kanako, M.; Yasushi, N.; Kenji, S.; Akira, W.; Masato, N.; Nobuo, T.; Ken, I. Comprehensive dental treatment of adult cleft lip and palate cases using SARPE. Dent. Rep. 2017, 117, 221–230. [Google Scholar]
- Kahnberg, K.E.; Vannas-Löfqvist, L.; Zellin, G. Complications associated with segmentation of the maxilla: A retrospective radiographic follow up of 82 patients. Int. J. Oral. Maxillofac. Surg. 2005, 34, 840–845. [Google Scholar] [CrossRef] [PubMed]
- Ochiai, S.; Kuroyanagi, N.; Sakuma, H.; Sakuma, H.; Miyachi, H.; Shimozato, K. Endoscopic-assisted resection of peripheral osteoma using piezosurgery. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2012, 115, 16–20. [Google Scholar] [CrossRef]
- Robiony, M.; Polini, F.; Costa, F.; Zerman, N.; Politi, M. Ultrasonic bone cutting for surgically assisted rapid maxillary expansion (SARPE) under local anaesthesia. Int. J. Oral. Maxillofac. Surg. 2007, 36, 267–269. [Google Scholar] [CrossRef]
- Passeri, L.A.; Bento, A.M.; Vanni, T. Resorbable versus titanium fixation of le Fort I osteotomy. J. Craniofac. Surg. 2020, 31, 934–939. [Google Scholar] [CrossRef]
- Yuko, F.; Hiroyoshi, I.; Yasuki, H. Absorbable plastic from infection after reduction of tibial fracture.1 case requiring removal of wound. J. Jpn. Jaw Deform. Soc. 2021, 12, 66–69. [Google Scholar]
- Chen, Y.R.; Yeow, V.K. Multiple-segment osteotomy in maxillofacial surgery. Plast. Reconstr. Surg. 1999, 104, 381–388. [Google Scholar] [CrossRef]
- Ryoichi, G.; Yoshishio, K. Lips, jaws, dentition of cleft palate patients, research on palate morphology, dentition after palatal flap posterior movement surgery. Characteristics of palate morphology. Jpn. J. Palate 1983, 8, 67–84. [Google Scholar]
- Hiroto; Otubo, H.I.; Kayomi, T.; Keiei, Y.; Nobuyuki, O.; Ryuichi, T.; Yosuke, A.; Hideki, O.; Koichi, M.; Ryo, N.; et al. Regression after expansion of the maxillary dental arch in patients with unilateral cleft lip and palate. Res. Hokkai Orthod. 1990, 18, 35–42. [Google Scholar]
- Hiroyasu, H.; Hisao, S.; Masakatsu, F.; Mai, F.; Kai, S.; Mikiko, M.; Naoto, S.; Hideaki, S.; Shinji, Y. After maxillary lengthening for patients with cleft lip and palate with marked maxillary undergrowth. A case of two-jaw surgery. J. Meikai Dent. Med. 2022, 51, 109–118. [Google Scholar]
- Ishikawa, H.; Nakamura, S.; Misaki, K.; Kudoh, M.; Fukuda, H.; Yoshida, S. Scar tissue distribution on palates and its relation to maxillary dental arch form. Cleft Palate Craniofac. J. 1998, 35, 313–319. [Google Scholar] [CrossRef] [PubMed]


| SNA | SNB | ANB | McNamara to A | McNamara to Pog | Mand.P | Gonial.A | U1 to FH | L1 to Mand.P | IIA | |
|---|---|---|---|---|---|---|---|---|---|---|
| At initial examination | 73.0 | 72.0 | +1.0 | −3.0 | −14.0 | 35.0 | 125.0 | 104.0 | 86.5 | 135.0 |
| At completion of preoperative orthodontics | 73.0 | 72.0 | +1.0 | −3.0 | −14.0 | 35.0 | 125.0 | 113.0 | 82.0 | 126.0 |
| At the completion of dynamic treatment | 75.0 | 70.0 | +5.0 | +1.0 | −19.0 | 37.0 | 131.0 | 108.0 | 85.0 | 125.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nemoto, N.; Kawanabe, H.; Oyama, A. Successful Correction of Crossbite with Multi-Segment Le Fort I Osteotomy in a Patient with Cleft Lip and Palate. Dent. J. 2025, 13, 131. https://doi.org/10.3390/dj13030131
Nemoto N, Kawanabe H, Oyama A. Successful Correction of Crossbite with Multi-Segment Le Fort I Osteotomy in a Patient with Cleft Lip and Palate. Dentistry Journal. 2025; 13(3):131. https://doi.org/10.3390/dj13030131
Chicago/Turabian StyleNemoto, Naoko, Hitoshi Kawanabe, and Akihiko Oyama. 2025. "Successful Correction of Crossbite with Multi-Segment Le Fort I Osteotomy in a Patient with Cleft Lip and Palate" Dentistry Journal 13, no. 3: 131. https://doi.org/10.3390/dj13030131
APA StyleNemoto, N., Kawanabe, H., & Oyama, A. (2025). Successful Correction of Crossbite with Multi-Segment Le Fort I Osteotomy in a Patient with Cleft Lip and Palate. Dentistry Journal, 13(3), 131. https://doi.org/10.3390/dj13030131





