Pediatric Advance Care Planning: A Scoping Review
Abstract
1. Introduction
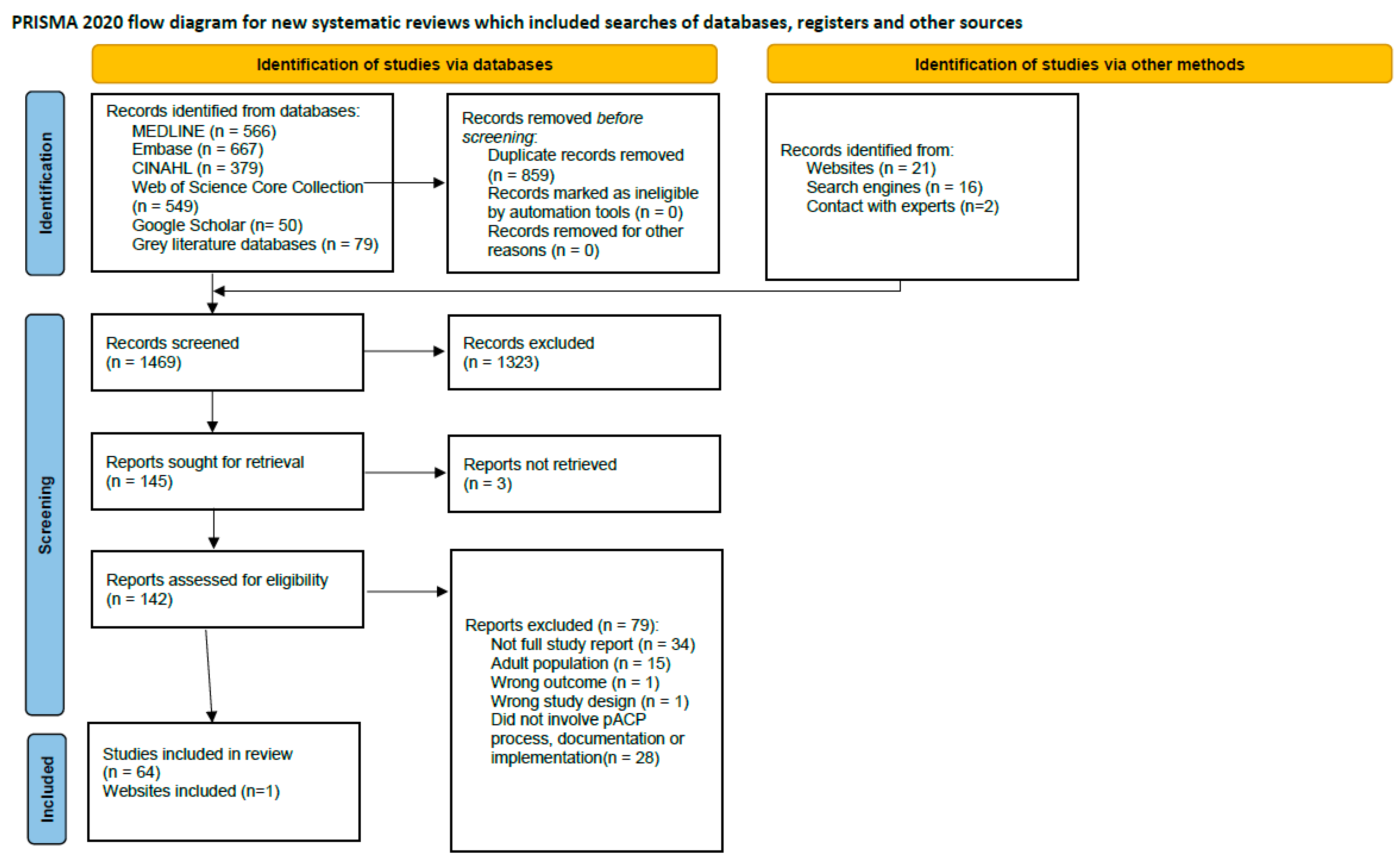
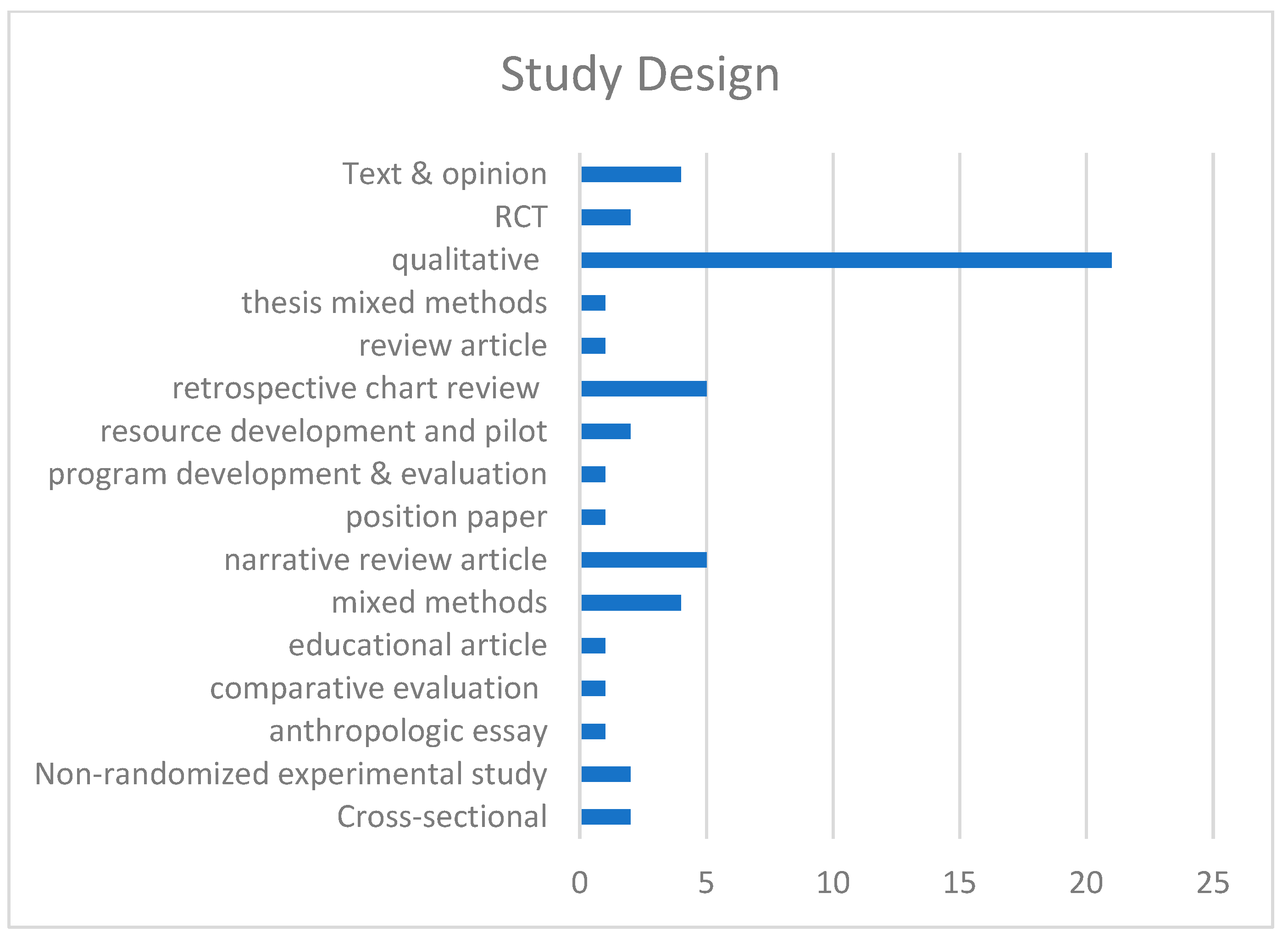
2. Materials and Methods
2.1. pACP Process
2.1.1. Inclusion Criteria
2.1.2. Information Sources and Search Strategy
2.1.3. Study Selection
2.1.4. Data Extraction
- Number of participants;
- Age range;
- Country;
- Study design;
- Person who conducts the ACP conversation (e.g., GP, specialist, paramedic);
- Characteristics of ACP forms.
3. Results
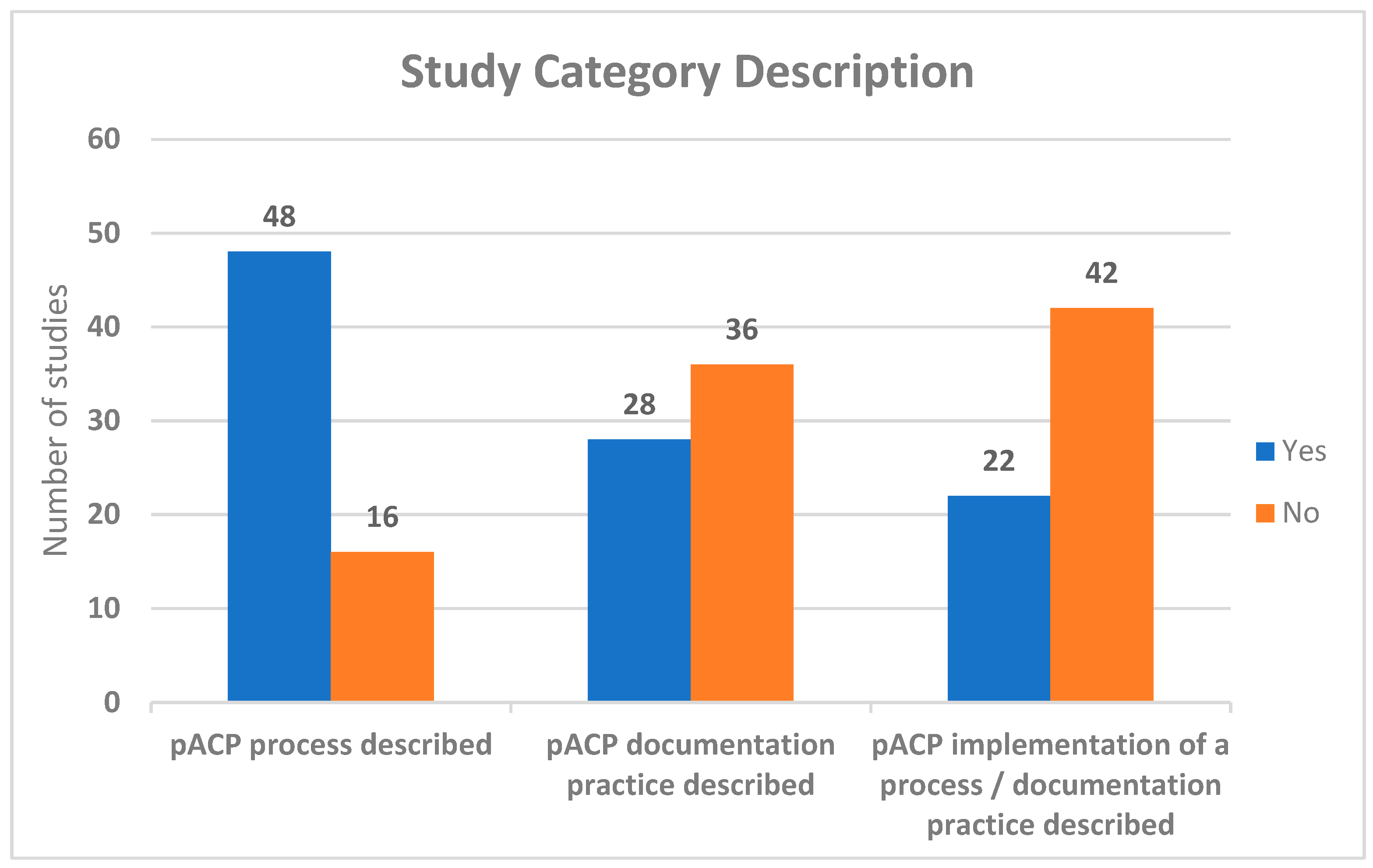
3.1. pACP Process
3.2. pACP Documentation
3.3. pACP Process and Documentation Implementation Practices
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Full Search Strategies for All Databases and List of All Grey Literature Sources
|
| * Including the asterix symbol retrieves every potential suffix variations of the word. |
|
| * Including the asterix symbol retrieves every potential suffix variations of the word. |
| S21 | S11 AND S18 AND S19 | Narrow by Language:—English Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 379 |
| S20 | S11 AND S18 AND S19 | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 387 |
| (pediatric * or paediatric * or child * or newborn * or congenital * or infan * or baby or babies or neonat * or “pre-term” or preterm or “premature birth *” or NICU or preschool * or “pre-school *” or kindergarten * or “elementary school *” or “nursery school *” or schoolchild * or toddler * or boy or boys or girl * or “middle school *” or pubescen * or juvenile * or teen * or youth * or “high school *” or adolesc *or prepubesc * or “pre-pubesc *” or (MH “Child+”) OR (MH “Adolescence+”) OR (MH “Minors (Legal)”) or “(MH “Child Abuse, Sexual”) OR (MH “Child Behavior Disorders+”) OR (MH “Child, Medically Fragile”) OR (MH “Child Day Care”) OR (MH “Child Behavior+”) OR (MH “Child Mortality”) OR (MH “Child Passenger Safety”) OR (MH “Child Development Disorders, Pervasive+”) OR (MH “Child Custody”) OR (MH “Child Abuse+”) OR (MH “Child Nutritional Physiology+”) OR (MH “Child Behavior Checklist”)) OR SO (child * or pediatric * or paediatric * or adolescent *) | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 1,441,871 | |
| S18 | S12 OR S13 OR S14 OR S15 OR S16 OR S17 | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 1,242,469 |
| S17 | TI implement * OR AB implement * | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 213,540 |
| S16 | TI form # OR AB form # | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 164,869 |
| S15 | TI develop * OR AB develop * | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 845,306 |
| S14 | TI (create or creation) OR AB (create or creation) | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 67,912 |
| S13 | TI document * OR AB document * | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 123,651 |
| S12 | (MH “Documentation”) | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 33,410 |
| S11 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 14,185 |
| S10 | TI (“do not attempt resuscitation”) OR AB (“do not attempt resuscitation”) | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 167 |
| S9 | TI (“do not resuscitate”) OR AB (“do not resuscitate”) | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 1404 |
| S8 | TI resuscitation order # OR AB resuscitation order # | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 316 |
| S7 | MH “Resuscitation Orders” | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 3149 |
| S6 | TI “living will *” OR AB “living will *” | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 690 |
| S5 | TI (advance # N2 directive #) OR AB (advance # N2 directive#) | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 3346 |
| S4 | TI advance # care planning OR AB advance # care planning | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 3371 |
| S3 | (MH “Living Wills”) | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 999 |
| S2 | (MH “Advance Directives”) | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 5801 |
| S1 | (MH “Advance Care Planning”) | Search modes—Boolean/Phrase | Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—CINAHL Complete | 4160 |
| * Including the asterix symbol retrieves every potential suffix variation of the word. # Including the wildcard number symbol in a particular place retrieves every possible variation of a word where the wildcard is present. | ||||
- TS=(“advance$ care planning”)
- TS=(advance$ NEAR/2 directive$)
- TS=(“living will*”)
- TS=(“resuscitation order$”)
- TS=(“do not resuscitate”)
- TS=(“do not attempt resuscitation”)
- #1 OR #2 OR #3 OR #4 OR #5 OR #6
- TS=(document*)
- TS=(create or creation)
- TS=(develop*)
- TS=(form$)
- TS=(implement*)
- #8 OR #9 OR #10 OR #11 OR #12
- TS=(pediatric* or paediatric* or child* or newborn* or congenital* or infan* or baby or babies or neonat* or pre-term or preterm* or premature birth* or NICU or preschool* or pre- school* or kindergarten* or kindergarden* or elementary school* or nursery school* or (day care* not adult*) or schoolchild* or toddler* or boy or boys or girl* or middle school* or pubescen* or juvenile* or teen* or youth* or high school* or adolesc* or pre-pubesc* or prepubesc*)
- #7 AND #13 AND #14
- #7 AND #13 AND #14 and English (Languages)
- ○
- Speak Up Canada (https://www.advancecareplanning.ca/) (accessed on 16 October 2021).
- ○
- Speakup Canada pediatric resources (https://www.advancecareplanning.ca/national-community-of-practice-for-advance-care-planning-educators/document-library/pediatric-advance-care-planning/) (accessed on 16 October 2021).
- ○
- BC Center for Palliative Care (https://bc-cpc.ca/all-resources/individuals/acp/; https://bc-cpc.ca/all-resources/individuals/acp/acp-resources/) (accessed on 16 October 2021).
- ○
- Healthlink BC (https://www.healthlinkbc.ca/) (accessed on 16 October 2021).
- ○
- Government BC- My Voice (https://www.health.gov.bc.ca/library/publications/year/2013/MyVoice-AdvanceCarePlanningGuide.pdf) (accessed on 16 October 2021).
- ○
- Interior health (https://www.interiorhealth.ca/sites/Partners/palliative/Pages/Clinical-Practice-Supports.aspx) (accessed on 16 October 2021).
- ○
- Vancouver Island Health Authority (https://www.islandhealth.ca/our-services/advance-care-planning/advance-care-planning) (accessed on 16 October 2021).
- ○
- Fraser Health (https://www.fraserhealth.ca/health-topics-a-to-z/advance-care-planning#.YJ1t6KhKhdg) (accessed on 16 October 2021).
- ○
- PHSA (http://www.phsa.ca/health-info/advance-care-planning) (accessed on 16 October 2021).
- ○
- Canadian Virtual Hospice (https://www.virtualhospice.ca/en_US/Main+Site+Navigation/Home.aspx) (accessed on 16 October 2021).
- ○
- Ministry of Children and Family Development (https://www2.gov.bc.ca/gov/content/governments/organizational-structure/ministries-organizations/ministries/children-and-family-development) (accessed on 16 October 2021).
- ○
- Healthlink (https://www.healthlinkbc.ca/health-feature/advance-care-planning) (accessed on 16 October 2021).
- ○
- Other PPC programs across Canada or key PPC programs, including Sick Kids Hospital, Rogers House, Flames House, IWK hospital, Emily’s House, etc.
References
- Downing, J.; Ling, J.; Benini, F.; Payne, S.; Papadatou, D. Core Competencies for Education in Paediatric Palliative Care; Report of the EAPC Children’s Palliative Care Education Taskforce; European Association for Palliative Care (EAPC): Milan, Italy, 2013. [Google Scholar]
- Together for Short Lives. A Core Care Pathway for Children with Life-Limiting and Life-Threatening Condition, 3rd ed.; Together for Short Lives: Bristol, UK, 2013. [Google Scholar]
- Canadian Hospice Palliative Care Association. Pediatric Hospice Palliative Care Guiding Principles and Norms of Practice; Canadian Hospice Palliative Care Association: Ottawa, ON, Canada, 2006. [Google Scholar]
- Kassam, A.; Skiadaresis, J.; Alexander, S.; Wolfe, J. Differences in End-of-Life Communication for Children with Advanced Cancer Who Were Referred to a Palliative Care Team. Pediatr. Blood Cancer 2015, 62, 1409–1413. [Google Scholar] [CrossRef]
- Snaman, J.M.; Kaye, E.C.; Lu, J.J.; Sykes, A.; Baker, J.N. Palliative Care Involvement Is Associated with Less Intensive End-of-Life Care in Adolescent and Young Adult Oncology Patients. J. Palliat. Med. 2017, 20, 509–516. [Google Scholar] [CrossRef]
- Ananth, P.; Melvin, P.; Berry, J.G.; Wolfe, J. Trends in Hospital Utilization and Costs among Pediatric Palliative Care Recipients. J. Palliat. Med. 2017, 20, 946–953. [Google Scholar] [CrossRef] [PubMed]
- DeCourcey, D.D.; Silverman, M.; Oladunjoye, A.; Wolfe, J. Advance Care Planning and Parent-Reported End-of-Life Outcomes in Children, Adolescents, and Young Adults with Complex Chronic Conditions. Crit. Care Med. 2019, 47, 101–108. [Google Scholar] [CrossRef]
- Lotz, J.D.; Jox, R.J.; Borasio, G.D.; Führer, M. Pediatric Advance Care Planning from the Perspective of Health Care Professionals: A Qualitative Interview Study. Palliat. Med. 2015, 29, 212–222. [Google Scholar] [CrossRef] [PubMed]
- Sidgwick, P.; Fraser, J.; Fortune, P.-M.; McCulloch, R. Parallel Planning and the Paediatric Critical Care Patient. Arch. Dis. Child. 2019, 104, 994–997. [Google Scholar] [CrossRef]
- Lotz, J.D.; Daxer, M.; Jox, R.J.; Borasio, G.D.; Führer, M. “Hope for the Best, Prepare for the Worst”: A Qualitative Interview Study on Parents’ Needs and Fears in Pediatric Advance Care Planning. Palliat. Med. 2017, 31, 764–771. [Google Scholar] [CrossRef] [PubMed]
- Siden, H. Pediatric Palliative Care for Children with Progressive Non-Malignant Diseases. Children 2018, 5, 28. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Chapter 11: Scoping Reviews. In JBI Manual for Evidence Synthesis, 2020 Version; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020; Available online: https://synthesismanual.jbi.global (accessed on 17 September 2021).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Pawliuk, C.; Lusney, N.; van Breemen, C.; Hussein, Z. Documentation, Process and Implementation of Advance Care Planning in the Pediatric Population: A Scoping Review Protocol; OSF Preprints; OSF: Charlottesville, VA, USA, 2021. [Google Scholar] [CrossRef]
- Tjosvold, L.; Campbell, S.M.; Dorgan, M. Filter to Retrieve Pediatric Articles in the OVID Medline Database. John W. Scott Health Sciences Library, University of Alberta. Rev. 14 September 2020. Available online: https://docs.google.com/document/d/1Q3MLfUolWe9q33JdAIzmVK0vi_ieC2Z60e9QvzTgkU8/edit (accessed on 9 October 2021).
- Basu, M.R.; Partin, L.; Revette, A.; Wolfe, J.; DeCourcey, D.D. Clinician Identified Barriers and Strategies for Advance Care Planning in Seriously Ill Pediatric Patients. J. Pain. Symptom Manag. 2021, 62, e100–e111. [Google Scholar] [CrossRef]
- Abbott, D.; Prescott, H.; Forbes, K.; Fraser, J.; Majumdar, A. Men with Duchenne Muscular Dystrophy and End of Life Planning. Neuromuscul. Disord. 2017, 27, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Barrison, P.; Davidson, L.G. Promotion of Advance Care Planning Among Young Adults: A Pilot Study of Health Engagement Workshop Feasibility, Implementation, and Efficacy. Am. J. Hosp. Palliat. Care 2021, 38, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Beecham, E.; Oostendorp, L.; Crocker, J.; Kelly, P.; Dinsdale, A.; Hemsley, J.; Russell, J.; Jones, L.; Bluebond-Langner, M. Keeping All Options Open: Parents’ Approaches to Advance Care Planning. Health Expect. 2017, 20, 675–684. [Google Scholar] [CrossRef] [PubMed]
- Caruso Brown, A.E. Reconceiving Decisions at the End of Life in Pediatrics: Decision-Making as a Form of Ritual. Perspect. Bio Med. 2019, 62, 301–318. [Google Scholar] [CrossRef] [PubMed]
- Copper, T.C.; Jeffe, D.B.; Ahmad, F.A.; Abraham, G.; Yu, F.; Hickey, B.; Schnadower, D. Emergency Information Forms for Children with Medical Complexity: A Qualitative Study. Pediatr. Emerg. Care 2020, 36, e318–e323. [Google Scholar] [CrossRef]
- Coughlin, K. Medical Decision-Making in Paediatrics: Infancy to Adolescence. J. Paediatr. Child. Health 2018, 23, 138–146. [Google Scholar] [CrossRef]
- Curtin, K.B.; Watson, A.E.; Wang, J.; Okonkwo, O.C.; Lyon, M.E. Pediatric Advance Care Planning (PACP) for Teens with Cancer and Their Families: Design of a Dyadic, Longitudinal RCCT. Contemp. Clin. Trials 2017, 62, 121–129. [Google Scholar] [CrossRef]
- Dallas, R.H.; Kimmel, A.; Wilkins, M.L.; Rana, S.; Garcia, A.; Cheng, Y.I.; Wang, J.; Lyon, M.E.; Adolescent Palliative Care Consortium. Acceptability of Family-Centered Advanced Care Planning for Adolescents with HIV. Pediatrics 2016, 138, e20161854. [Google Scholar] [CrossRef]
- de Arruda-Colli, M.N.F.; Sansom-Daly, U.; Dos Santos, M.A.; Wiener, L. Considerations for the Cross-Cultural Adaptation of an Advance Care Planning Guide for Youth with Cancer. Clin. Pract. Pediatr. Psychol. 2018, 6, 341–354. [Google Scholar] [CrossRef]
- DeCourcey, D.D.; Partin, L.; Revette, A.; Bernacki, R.; Wolfe, J. Development of a Stakeholder Driven Serious Illness Communication Program for Advance Care Planning in Children, Adolescents, and Young Adults with Serious Illness. J. Pediatr. 2021, 229, 247–258.e8. [Google Scholar] [CrossRef]
- Dombrecht, L.; Piette, V.; Deliens, L.; Cools, F.; Chambaere, K.; Goossens, L.; Naulaers, G.; Cornette, L.; Beernaert, K.; Cohen, J.; et al. Barriers to and Facilitators of End-of-Life Decision Making by Neonatologists and Neonatal Nurses in Neonates: A Qualitative Study. J. Pain. Symptom Manag. 2020, 59, 599–608.e2. [Google Scholar] [CrossRef]
- Edwards, J.D.; Kun, S.S.; Graham, R.J.; Keens, T.G. End-of-Life Discussions and Advance Care Planning for Children on Long-Term Assisted Ventilation with Life-Limiting Conditions. J. Palliat. Care 2012, 28, 21–27. [Google Scholar] [CrossRef]
- Ekberg, S.; Herbert, A.; Johns, K.; Tarrant, G.; Sansone, H.; Yates, P.; Danby, S.; Bradford, N.K. Finding a Way with Words: Delphi Study to Develop a Discussion Prompt List for Paediatric Palliative Care. Palliat. Med. 2020, 34, 291–299. [Google Scholar] [CrossRef] [PubMed]
- El Sayed, M.F.; Chan, M.; McAllister, M.; Hellmann, J. End-of-Life Care in Toronto Neonatal Intensive Care Units: Challenges for Physician Trainees. Arch. Dis. Child. Fetal Neonatal Ed. 2013, 98, F528–F533. [Google Scholar] [CrossRef] [PubMed]
- Ewing, K.B. Improving Nurses’ Understanding of Pediatric-Focused Advance Directives. Pediat Nurs. 2020, 46, 11–39. [Google Scholar]
- Fahner, J.C.; Tholking, T.W.; Rietjens, J.A.C.; van der Heide, A.; van Delden, J.J.M.; Kars, M.C. Towards Advance Care Planning in Pediatrics: A Qualitative Study on Envisioning the Future as Parents of a Seriously Ill Child. Eur. J. Pediatr. 2020, 179, 1461–1468. [Google Scholar] [CrossRef] [PubMed]
- Fahner, J.; Rietjens, J.; van der Heide, A.; Milota, M.; van Delden, J.; Kars, M. Evaluation Showed That Stakeholders Valued the Support Provided by the Implementing Pediatric Advance Care Planning Toolkit. Acta Paediatr. 2021, 110, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Fraser, J.; Harris, N.; Berringer, A.J.; Prescott, H.; Finlay, F. Advanced Care Planning in Children with Life-Limiting Conditions—The Wishes Document. Arch. Dis. Child. 2010, 95, 79–82. [Google Scholar] [CrossRef]
- Gallagher, A.; Peacock, M.; Arber, A. Helping Young People Who Have Learning Disabilities and Their Families to Plan End of Life Care: The ADVANCE Toolkit. Learn. Disabil. Res. Pract. 2018, 21, 33–41. [Google Scholar] [CrossRef]
- Harmoney, K.; Mobley, E.M.; Gilbertson-White, S.; Brogden, N.K.; Benson, R.J. Differences in Advance Care Planning and Circumstances of Death for Pediatric Patients Who Do and Do Not Receive Palliative Care Consults: A Single-Center Retrospective Review of All Pediatric Deaths from 2012 to 2016. J. Palliat. Med. 2019, 22, 1506–1514. [Google Scholar] [CrossRef]
- Harrop, E.J.; Boyce, K.; Beale, T.; Brombley, K. Fifteen-Minute Consultation: Developing an Advance Care Plan in Partnership with the Child and Family. Arch. Dis. Child. Educ. Pract. Ed. 2018, 103, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Noyes, J.; Hastings, R.P.; Lewis, M.; Hain, R.; Bennett, V.; Hobson, L.; Spencer, L.H. Planning Ahead with Children with Life-Limiting Conditions and Their Families: Development, Implementation and Evaluation of “My Choices. ” BMC Palliat. Care 2013, 12, 5. [Google Scholar] [CrossRef]
- Heckford, E.; Beringer, A.J. Advance Care Planning: Challenges and Approaches for Pediatricians. J. Palliat. Med. 2014, 17, 1049–1053. [Google Scholar] [CrossRef] [PubMed]
- Hein, K.; Knochel, K.; Zaimovic, V.; Reimann, D.; Monz, A.; Heitkamp, N.; Borasio, G.D.; Fuhrer, M. Identifying Key Elements for Paediatric Advance Care Planning with Parents, Healthcare Providers and Stakeholders: A Qualitative Study. Palliat. Med. 2020, 34, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Jack, B.A.; Mitchell, T.K.; O’Brien, M.R.; Silverio, S.A.; Knighting, K. A Qualitative Study of Health Care Professionals’ Views and Experiences of Paediatric Advance Care Planning. BMC Palliat. Care 2018, 17, 93. [Google Scholar] [CrossRef] [PubMed]
- Hughes, B. A Multiple Case Study to Explore the Views and Experiences of Young People, Their Parents and Carers, and Healthcare Professionals of the Advance Care Planning Process; Edge Hill University: Ormskirk, UK, 2019. [Google Scholar]
- Jordan, M.; Keefer, P.M.; Lee, Y.-L.A.; Meade, K.; Snaman, J.M.; Wolfe, J.; Kamal, A.; Rosenberg, A. Top Ten Tips Palliative Care Clinicians Should Know About Caring for Children. J. Palliat. Med. 2018, 21, 1783–1789. [Google Scholar] [CrossRef]
- Katz, N.T.; Sacks, B.H.; Hynson, J.L.; Heywood, M.; Williams, M.; Sokol, J. Improving Paediatric Advance Care Planning: Results of a Learning Needs Analysis and Simulation-Based Education Programme. J. Paediatr. Child. Health 2020, 56, 1898–1905. [Google Scholar] [CrossRef]
- Knochel, K.; Zaimovic, V.; Gatzweiler, B.; Hein, K.K.; Heitkamp, N.; Monz, A.; Reimann, D.; Borasio, G.D.; Fuhrer, M. Participatory Development of a Modular Advance Care Planning Program in Pediatric Palliative Care (MAPPS). J. Pain. Symptom Manag. 2022, 63, 189–198. [Google Scholar] [CrossRef]
- Liberman, D.; Pham, P.; Nager, A. Pediatric Advance Directives: Parents’ Knowledge, Experience, and Preferences. Pediatrics 2014, 134, E436–E443. [Google Scholar] [CrossRef]
- Loeffen, E.A.H.; Tissing, W.J.E.; Schuiling-Otten, M.A.; de Kruiff, C.C.; Kremer, L.C.M.; Verhagen, A.A.E.; Pediatric Palliative Care-Individualized Care Plan Working Group. Individualised Advance Care Planning in Children with Life-Limiting Conditions. Arch. Dis. Child. 2018, 103, 480–485. [Google Scholar] [CrossRef]
- Lord, S.; Moore, C.; Beatty, M.; Cohen, E.; Rapoport, A.; Hellmann, J.; Netten, K.; Amin, R.; Orkin, J. Assessment of Bereaved Caregiver Experiences of Advance Care Planning for Children with Medical Complexity. JAMA Netw. Open 2020, 3, e2010337. [Google Scholar] [CrossRef] [PubMed]
- Lotz, J.D.; Jox, R.J.; Borasio, G.D.; Fuhrer, M. Pediatric Advance Care Planning: A Systematic Review. Pediatrics 2013, 131, e873–e880. [Google Scholar] [CrossRef] [PubMed]
- Lyon, M.E.; Garvie, P.A.; McCarter, R.; Briggs, L.; He, J.; D’Angelo, L.J. Who Will Speak for Me? Improving End-of-Life Decision-Making for Adolescents with HIV and Their Families. Pediatrics 2009, 123, e199–e206. [Google Scholar] [CrossRef]
- Lyon, M.E.; Garvie, P.A.; Briggs, L.; He, J.; McCarter, R.; D’Angelo, L.J. Development, Feasibility, and Acceptability of the Family/Adolescent-Centered (FACE) Advance Care Planning Intervention for Adolescents with HIV. J. Palliat. Med. 2009, 12, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Lyon, M.E.; Garvie, P.A.; Briggs, L.; He, J.; Malow, R.; D’Angelo, L.J.; McCarter, R. Is It Safe? Talking to Teens with HIV/AIDS about Death and Dying: A 3-Month Evaluation of Family Centered Advance Care (FACE) Planning—Anxiety, Depression, Quality of Life. HIV/AIDS 2010, 2, 27–37. [Google Scholar] [CrossRef]
- Lyon, M.E.; Jacobs, S.; Briggs, L.; Cheng, Y.I.; Wang, J. A Longitudinal, Randomized, Controlled Trial of Advance Care Planning for Teens with Cancer: Anxiety, Depression, Quality of Life, Advance Directives, Spirituality. J. Adolesc. Health 2014, 54, 710–717. [Google Scholar] [CrossRef]
- Martin, A.E.; Beringer, A.J. Advanced Care Planning 5 Years on: An Observational Study of Multi-Centred Service Development for Children with Life-Limiting Conditions. Child. Care Health Dev. 2019, 45, 234–240. [Google Scholar] [CrossRef]
- Mitchell, S.; Plunkett, A.; Dale, J. Use of Formal Advance Care Planning Documents: A National Survey of UK Paediatric Intensive Care Units. Arch. Dis. Child. 2014, 99, 327–330. [Google Scholar] [CrossRef]
- Myers, J.; Cosby, R.; Gzik, D.; Harle, I.; Harrold, D.; Incardona, N.; Walton, T. Provider Tools for Advance Care Planning and Goals of Care Discussions: A Systematic Review. Am. J. Hosp. Palliat. Care 2018, 35, 1123–1132. [Google Scholar] [CrossRef]
- Orkin, J.; Beaune, L.; Moore, C.; Weiser, N.; Arje, D.; Rapoport, A.; Netten, K.; Adams, S.; Cohen, E.; Amin, R. Toward an Understanding of Advance Care Planning in Children with Medical Complexity. Pediatrics 2020, 145, e20192241. [Google Scholar] [CrossRef]
- Pao, M.; Mahoney, M.R. “Will You Remember Me?”: Talking with Adolescents About Death and Dying. Child. Adolesc. Psychiatr. Clin. N. Am. 2018, 27, 511–526. [Google Scholar] [CrossRef] [PubMed]
- Rishel, C.J. The Realization of Parental Knowing: End-of-Life Decision Making in Pediatric Blood and Marrow Transplantation; The University of Arizona: Tucson, AZ, USA, 2010. [Google Scholar]
- Smith, S.L. Advance Care Planning Communication for Young Adults: A Role for Simulated Learning. J. Hosp. Palliat. Nurs. 2017, 19, 460–467. [Google Scholar] [CrossRef]
- Snaman, J.M.; Blazin, L.; Holder, R.L.; Wolfe, J.; Baker, J.N. Identifying and Quantifying Adolescent and Young Adult Patient Preferences in Cancer Care: Development of a Conjoint Analysis-Based Decision-Making Tool. J. Adolesc. Young Adult Oncol. 2019, 8, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Stark, Z.; Hynson, J.; Forrester, M. Discussing Withholding and Withdrawing of Life-Sustaining Medical Treatment in Paediatric Inpatients: Audit of Current Practice. J. Paediatr. Child. Health 2008, 44, 399–403. [Google Scholar] [CrossRef]
- Tatterton, M.J. Independent Non-Medical Prescribing in Children’s Hospices in the UK: A Practice Snapshot. Int. J. Palliat. Nurs. 2017, 23, 386–392. [Google Scholar] [CrossRef]
- Thompkins, J.D.; Needle, J.; Baker, J.N.; Briggs, L.; Cheng, Y.I.; Wang, J.; Friebert, S.; Lyon, M.E. Pediatric Advance Care Planning and Families’ Positive Caregiving Appraisals: An RCT. Pediatrics 2021, 147, e2020029330. [Google Scholar] [CrossRef]
- Toce, S.; Collins, M.A. The FOOTPRINTS Model of Pediatric Palliative Care. J. Palliat. Med. 2003, 6, 989–1000. [Google Scholar] [CrossRef] [PubMed]
- Valluzzi, J.L.; Brown, S.E.; Dailey, B. Protecting the Rights of Children with Special Health Care Needs through the Development of Individualized Emergency Response Plans. Infants Young Child. 1997, 10, 66–80. [Google Scholar] [CrossRef]
- van Driessche, A.; De Vleminck, A.; Gilissen, J.; Kars, M.C.; van der Werff Ten Bosch, J.; Deliens, L.; Cohen, J.; Beernaert, K. Advance Care Planning for Adolescents with Cancer and Their Parents: Study Protocol of the BOOST PACP Multi-Centre Randomised Controlled Trial and Process Evaluation. BMC Pediatr. 2021, 21, 376. [Google Scholar] [CrossRef]
- Verberne, L.M.; Fahner, J.C.; Sondaal, S.F.V.; Schouten-van Meeteren, A.Y.N.; de Kruiff, C.C.; van Delden, J.J.M.; Kars, M.C. Anticipating the Future of the Child and Family in Pediatric Palliative Care: A Qualitative Study into the Perspectives of Parents and Healthcare Professionals. Eur. J. Pediatr. 2021, 180, 949–957. [Google Scholar] [CrossRef]
- Wiener, L.; Zadeh, S.; Battles, H.; Baird, K.; Ballard, E.; Osherow, J.; Pao, M. Allowing Adolescents and Young Adults to Plan Their End-of-Life Care. Pediatrics 2012, 130, 897–905. [Google Scholar] [CrossRef] [PubMed]
- Wolff, A.; Browne, J.; Whitehouse, W.P. Personal Resuscitation Plans and End of Life Planning for Children with Disability and Life-Limiting/Life-Threatening Conditions. Arch. Dis. Child. Educ. Pract. Ed. 2011, 96, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.-M.; Huang, I.-C.; Su, H.-L.; Lee, S.-L. Interventions to Support Adolescents with Cancer in Decision-Making: A Systematic Review and Meta-Analysis. Worldviews Evid. Based Nurs. 2021, 18, 339–349. [Google Scholar] [CrossRef]
- Xafis, V.; Gillam, L.; Hynson, J.; Sullivan, J.; Cossich, M.; Wilkinson, D. Caring Decisions: The Development of a Written Resource for Parents Facing End-of-Life Decisions. J. Palliat. Med. 2015, 18, 945–955. [Google Scholar] [CrossRef] [PubMed]
- Moon, Y.J.; Lee, J.; Choo, I.S.; Kang, S.H.; Kim, C.H.; Song, I.G.; Kim, M.S. Development and Application of Advance Care Planning Workbooks to Facilitate Communication with Children and Adolescent Patients: A Pilot Test. J. Hosp. Palliat. Care 2020, 23, 212–227. [Google Scholar] [CrossRef]
- Zaal-Schuller, I.H.; Willems, D.L.; Ewals, F.V.P.M.; van Goudoever, J.B.; de Vos, M.A. Considering Quality of Life in End-of-Life Decisions for Severely Disabled Children. Res. Dev. Disabil. 2018, 73, 67–75. [Google Scholar] [CrossRef]
- Zadeh, S.; Pao, M.; Wiener, L. Opening End-of-Life Discussions: How to Introduce Voicing My CHOiCES TM, an Advance Care Planning Guide for Adolescents and Young Adults. Palliat. Support. Care 2015, 13, 591–599. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Carr, K.; Hasson, F.; McIlfatrick, S.; Downing, J. Initiation of Paediatric Advance Care Planning: Cross-Sectional Survey of Health Professionals Reported Behaviour. Child. Care Health Dev. 2022, 48, 423–434. [Google Scholar] [CrossRef]
- Daxer, M.; Monz, A.; Hein, K.; Heitkamp, N.; Knochel, K.; Borasio, G.D.; Führer, M. How to Open the Door: A Qualitative, Observational Study on Initiating Advance Care Discussions with Parents in Pediatric Palliative Care. J. Palliat. Med. 2022, 25, 562–569. [Google Scholar] [CrossRef]
- Wada, R.K.; Wong, L.; Flohr, A.; Arndt, R.G.; Ing, D.K.; Loos, J.R.; Kaneshige, L.; Teruya, K.; Peterman, K.; Albright, C.L.; et al. Simulation-Based Pediatric Interprofessional Team Training to Facilitate End-of-Life Discussions. Clin. Simul. Nurs. 2023, 78, 27–33. [Google Scholar] [CrossRef]
- Hill, D.L.; Miller, V.; Walter, J.K.; Carroll, K.W.; Morrison, W.E.; Munson, D.A.; Kang, T.I.; Hinds, P.S.; Feudtner, C. Regoaling: A Conceptual Model of How Parents of Children with Serious Illness Change Medical Care Goals. BMC Palliat. Care 2014, 13, 9. [Google Scholar] [CrossRef] [PubMed]
| Description of Participants | Age Range of Participants | Person Conducting ACP |
|---|---|---|
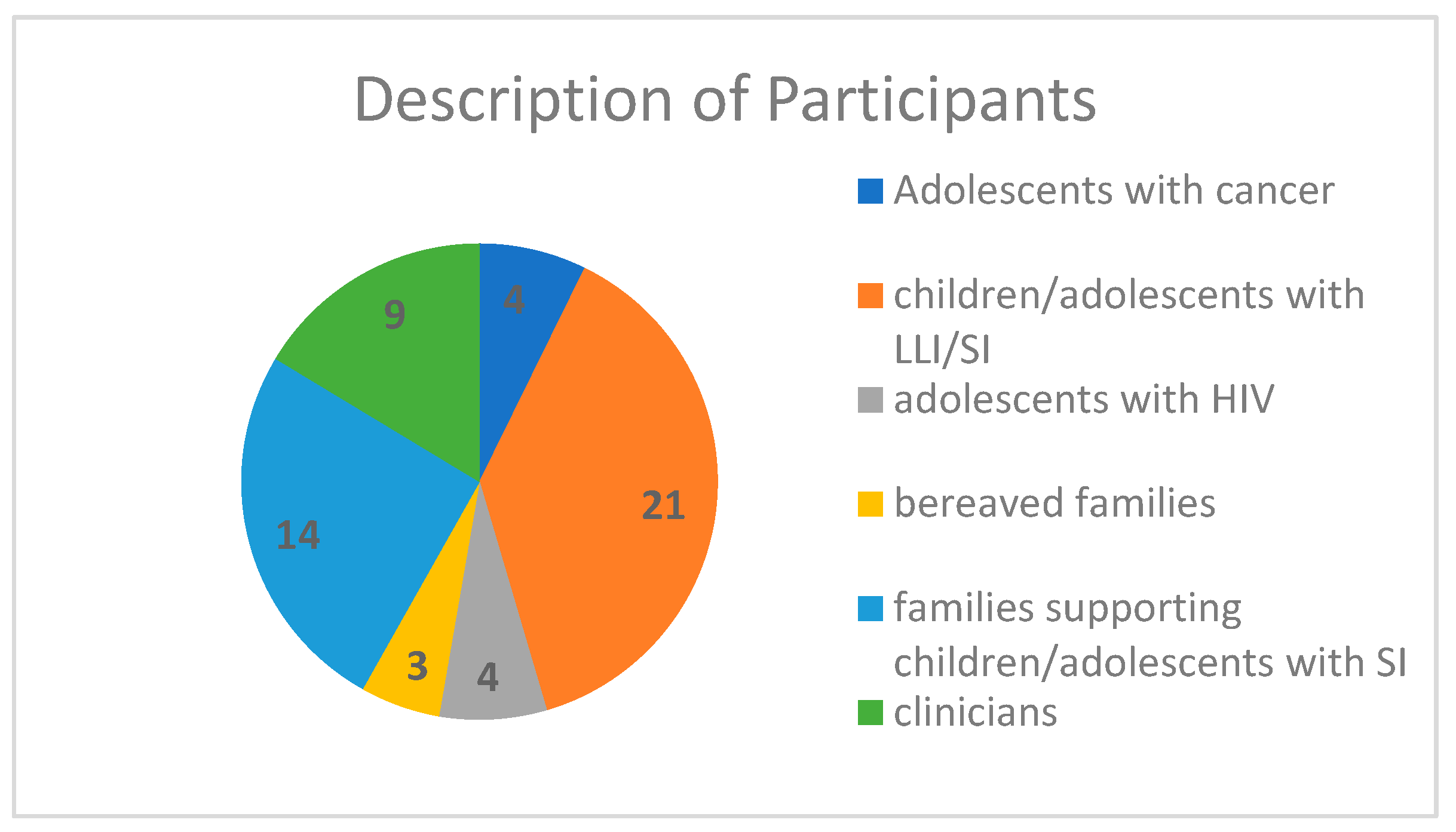
| Adolescents with cancer (n = 4), children/adolescents with LLI/SI (n = 21), adolescents with HIV (n = 4), bereaved families (n = 3), families supporting children/adolescents with SI (n = 14), clinicians (n = 9) | 0–35 (most articles 0–25, one article mentioned the range up to 45 years of age) | Physician, nurse practitioner, families, allied health, nurse, trainee, trained interviewer |
| pACP Documentation Tools/Guides/Strategies |
|---|
| Voicing my Choices, Lyon Advance Care Planning survey, Respecting Choices ACP interview, Five Wishes, My Wishes, Caring Decisions handbook, Statement of treatment preferences, My Choices booklet, Family Centered Pediatric ACP for teens with cancer (FACE-TC), BOOST pACP summary sheet, “My thoughts, my wishes, my voices” document, POLST form, free text in progress notes, Emergency care plans, DNR forms, Pediatric Serious Illness Conversation Guide |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lusney, N.; van Breemen, C.; Lim, E.; Pawliuk, C.; Hussein, Z. Pediatric Advance Care Planning: A Scoping Review. Children 2023, 10, 1179. https://doi.org/10.3390/children10071179
Lusney N, van Breemen C, Lim E, Pawliuk C, Hussein Z. Pediatric Advance Care Planning: A Scoping Review. Children. 2023; 10(7):1179. https://doi.org/10.3390/children10071179
Chicago/Turabian StyleLusney, Nadine, Camara van Breemen, Edlyn Lim, Colleen Pawliuk, and Zahra Hussein. 2023. "Pediatric Advance Care Planning: A Scoping Review" Children 10, no. 7: 1179. https://doi.org/10.3390/children10071179
APA StyleLusney, N., van Breemen, C., Lim, E., Pawliuk, C., & Hussein, Z. (2023). Pediatric Advance Care Planning: A Scoping Review. Children, 10(7), 1179. https://doi.org/10.3390/children10071179






