The Burden of Survivorship on Hematological Patients—Long-Term Analysis of Toxicities after Total Body Irradiation and Allogeneic Stem Cell Transplantation
Abstract
:Simple Summary
Abstract
1. Introduction
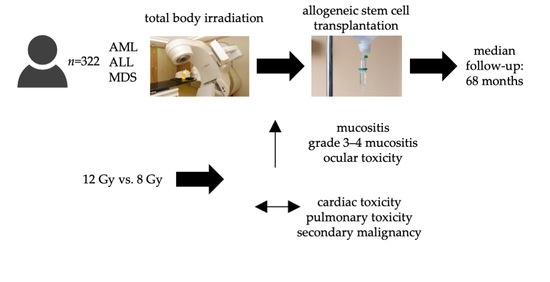
2. Materials and Methods
2.1. Clinical Data
2.2. Radiation Treatment
2.3. Statistical Analysis
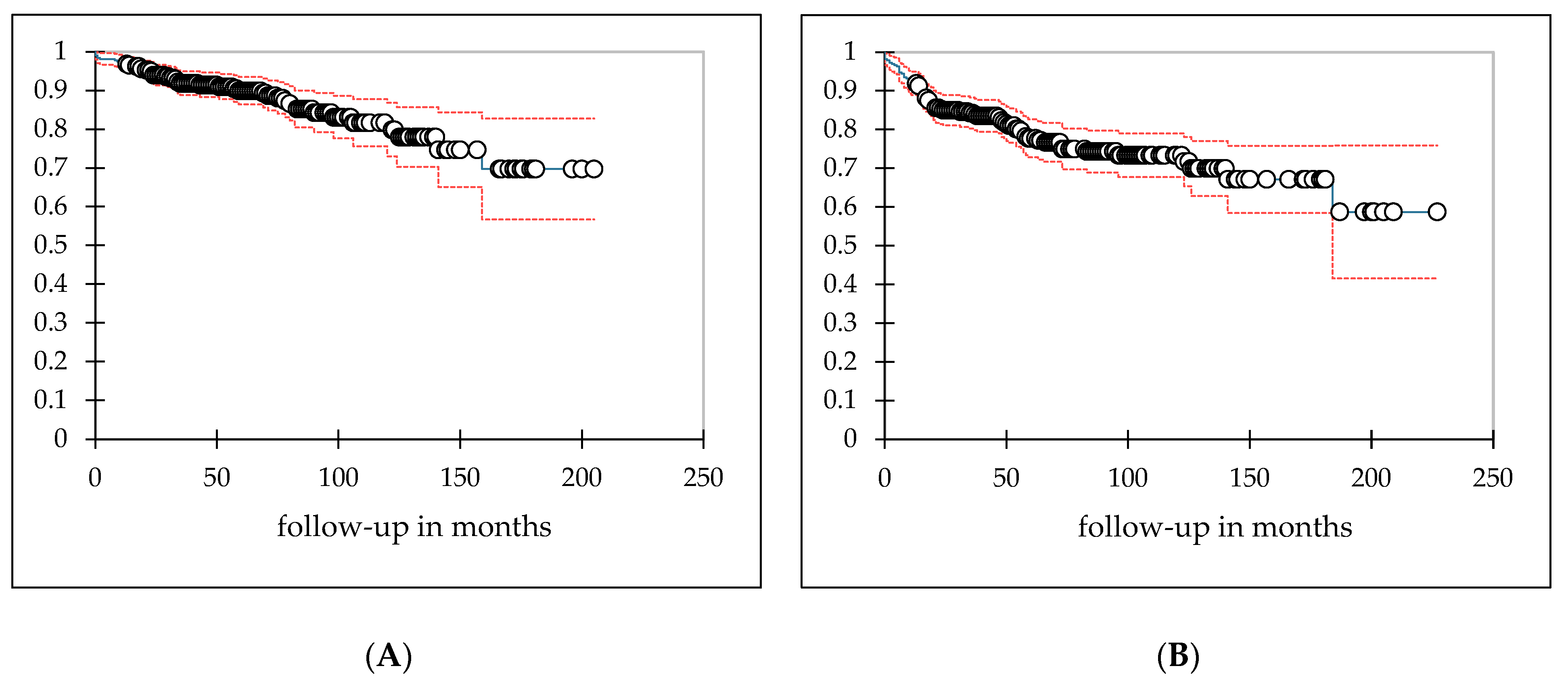
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Paix, A.; Antoni, D.; Waissi, W.; Ledoux, M.-P.; Bilger, K.; Fornecker, L.; Noel, G. Total Body Irradiation in Allogeneic Bone Marrow Transplantation Conditioning Regimens: A Review. Crit. Rev. Oncol. Hematol. 2018, 123, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.Y.C.; Filippi, A.R.; Dabaja, B.S.; Yahalom, J.; Specht, L. Total Body Irradiation: Guidelines from the International Lymphoma Radiation Oncology Group (ILROG). Int. J. Radiat. Oncol. Biol. Phys. 2018, 101, 521–529. [Google Scholar] [CrossRef]
- Wong, J.Y.C.; Filippi, A.R.; Scorsetti, M.; Hui, S.; Muren, L.P.; Mancosu, P. Total Marrow and Total Lymphoid Irradiation in Bone Marrow Transplantation for Acute Leukaemia. Lancet Oncol. 2020, 21, e477–e487. [Google Scholar] [CrossRef]
- Hoeller, U.; Borgmann, K.; Oertel, M.; Haverkamp, U.; Budach, V.; Eich, H.T. Late Sequelae of Radiotherapy—the Effect of Technical and Conceptual Innovations in Radiation Oncology. Dtsch. Aerzteblatt Online 2021, 118, 205–212. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0; U.S. Department of Health and Human Services: Washington, DC, USA, 2017.
- Ozsahin, M.; Belkacémi, Y.; Pène, F.; Laporte, J.; Rio, B.; Leblond, V.; Korbas, D.; Touboul, E.; Gorin, N.C.; Schlienger, M.; et al. Interstitial Pneumonitis Following Autologous Bone-Marrow Transplantation Conditioned with Cyclophosphamide and Total-Body Irradiation. Int. J. Radiat. Oncol. Biol. Phys. 1996, 34, 71–77. [Google Scholar] [CrossRef]
- Cosset, J.M.; Baume, D.; Pico, J.L.; Shank, B.; Girinski, T.; Benhamou, E.; Briot, E.; Malaise, E.; Hayat, M.; Dutreix, J. Single Dose versus Hyperfractionated Total Body Irradiation before Allogeneic Bone Marrow Transplantation: A Non-Randomized Comparative Study of 54 Patients at the Institut Gustave-Roussy. Radiother. Oncol. 1989, 15, 151–160. [Google Scholar] [CrossRef]
- Socie, G.; Devergie, A.; Girinsky, T.; Reiffers, J.; Vernant, J.P.; Le Bourgeois, J.P.; Herve, P.; Guyotat, D.; Maraninchi, D.; Rio, B. Influence of the Fractionation of Total Body Irradiation on Complications and Relapse Rate for Chronic Myelogenous Leukemia. The Groupe d’Etude Des Greffes de Moelle Osseuse (GEGMO). Int. J. Radiat. Oncol. Biol. Phys. 1991, 20, 397–404. [Google Scholar] [CrossRef]
- Chiang, Y.; Tsai, C.-H.; Kuo, S.-H.; Liu, C.-Y.; Yao, M.; Li, C.-C.; Huang, S.-Y.; Ko, B.-S.; Lin, C.-T.; Hou, H.-A.; et al. Reduced Incidence of Interstitial Pneumonitis after Allogeneic Hematopoietic Stem Cell Transplantation Using a Modified Technique of Total Body Irradiation. Sci. Rep. 2016, 6, 36730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Byun, H.K.; Yoon, H.I.; Cho, J.; Kim, H.J.; Min, Y.H.; Lyu, C.J.; Cheong, J.-W.; Kim, J.S.; Kim, H.S.; Kim, S.-J.; et al. Factors Associated with Pulmonary Toxicity after Myeloablative Conditioning Using Fractionated Total Body Irradiation. Radiat. Oncol. J. 2017, 35, 257–267. [Google Scholar] [CrossRef]
- Abugideiri, M.; Nanda, R.H.; Butker, C.; Zhang, C.; Kim, S.; Chiang, K.-Y.; Butker, E.; Khan, M.K.; Haight, A.E.; Chen, Z.; et al. Factors Influencing Pulmonary Toxicity in Children Undergoing Allogeneic Hematopoietic Stem Cell Transplantation in the Setting of Total Body Irradiation-Based Myeloablative Conditioning. Int. J. Radiat. Oncol. Biol. Phys. 2016, 94, 349–359. [Google Scholar] [CrossRef]
- Durie, E.; Nicholson, E.; Anthias, C.; Dunne, E.M.; Potter, M.; Ethell, M.; Messiou, C.; Brennan, J.; Eagle, S.; Talbot, J.; et al. Determining the Incidence of Interstitial Pneumonitis and Chronic Kidney Disease Following Full Intensity Haemopoetic Stem Cell Transplant Conditioned Using a Forward-Planned Intensity Modulated Total Body Irradiation Technique. Radiother. Oncol. 2021, 158, 97–103. [Google Scholar] [CrossRef]
- Latini, P.; Aristei, C.; Aversa, F.; Checcaglini, F.; Maranzano, E.; Panizza, B.M.; Perrucci, E.; Carotti, A.; Martelli, M.F. Interstitial Pneumonitis after Hyperfractionated Total Body Irradiation in HLA-Matched T-Depleted Bone Marrow Transplantation. Int. J. Radiat. Oncol. Biol. Phys. 1992, 23, 401–405. [Google Scholar] [CrossRef]
- Latini, P.; Aristei, C.; Aversa, F.; Checcaglini, F.; Maranzano, E.; Raymondi, C.; Panizza, B.M.; Perrucci, E.; Martelli, M.F. Lung Damage Following Bone Marrow Transplantation after Hyperfractionated Total Body Irradiation. Radiother. Oncol. 1991, 22, 127–132. [Google Scholar] [CrossRef]
- Gao, R.W.; Weisdorf, D.J.; DeFor, T.E.; Ehler, E.; Dusenbery, K.E. Influence of Total Body Irradiation Dose Rate on Idiopathic Pneumonia Syndrome in Acute Leukemia Patients Undergoing Allogeneic Hematopoietic Cell Transplantation. Int. J. Radiat. Oncol. Biol. Phys. 2019, 103, 180–189. [Google Scholar] [CrossRef]
- Oya, N.; Sasai, K.; Tachiiri, S.; Sakamoto, T.; Nagata, Y.; Okada, T.; Yano, S.; Ishikawa, T.; Uchiyama, T.; Hiraoka, M. Influence of Radiation Dose Rate and Lung Dose on Interstitial Pneumonitis after Fractionated Total Body Irradiation: Acute Parotitis May Predict Interstitial Pneumonitis. Int. J. Hematol. 2006, 83, 86–91. [Google Scholar] [CrossRef]
- Shinde, A.; Yang, D.; Frankel, P.; Liu, A.; Han, C.; Del Vecchio, B.; Schultheiss, T.; Cheng, J.; Li, R.; Kim, D.; et al. Radiation-Related Toxicities Using Organ Sparing Total Marrow Irradiation Transplant Conditioning Regimens. Int. J. Radiat. Oncol. Biol. Phys. 2019, 105, 1025–1033. [Google Scholar] [CrossRef]
- Thomas, O.; Mahé, M.; Campion, L.; Bourdin, S.; Milpied, N.; Brunet, G.; Lisbona, A.; Le Mevel, A.; Moreau, P.; Harousseau, J.; et al. Long-Term Complications of Total Body Irradiation in Adults. Int. J. Radiat. Oncol. Biol. Phys. 2001, 49, 125–131. [Google Scholar] [CrossRef]
- Bölling, T.; Kreuziger, D.C.; Ernst, I.; Elsayed, H.; Willich, N. Retrospective, Monocentric Analysis of Late Effects after Total Body Irradiation (TBI) in Adults. Strahlenther. Onkol. 2011, 187, 311–315. [Google Scholar] [CrossRef]
- Marnitz, S.; Zich, A.; Martus, P.; Budach, V.; Jahn, U.; Neumann, O.; Arnold, R. Long-Term Results of Total Body Irradiation in Adults with Acute Lymphoblastic Leukemia. Strahlenther. Onkol. 2014, 190, 453–458. [Google Scholar] [CrossRef]
- Belkacémi, Y.; Pène, F.; Touboul, E.; Rio, B.; Leblond, V.; Gorin, N.C.; Laugier, A.; Gemici, C.; Housset, M.; Ozsahin, M. Total-Body Irradiation before Bone Marrow Transplantation for Acute Leukemia in First or Second Complete Remission. Results and Prognostic Factors in 326 Consecutive Patients. Strahlenther. Onkol. 1998, 174, 92–104. [Google Scholar] [CrossRef]
- DE Felice, F.; Grapulin, L.; Musio, D.; Pomponi, J.; DI Felice, C.; Iori, A.P.; Bertaina, A.; Tombolini, V. Treatment Complications and Long-Term Outcomes of Total Body Irradiation in Patients with Acute Lymphoblastic Leukemia: A Single Institute Experience. Anticancer Res. 2016, 36, 4859–4864. [Google Scholar] [CrossRef] [Green Version]
- Barrett, A.; Depledge, M.H.; Powles, R.L. Interstitial Pneumonitis Following Bone Marrow Transplantation after Low Dose Rate Total Body Irradiation. Int. J. Radiat. Oncol. Biol. Phys. 1983, 9, 1029–1033. [Google Scholar] [CrossRef]
- Kelsey, C.R.; Horwitz, M.E.; Chino, J.P.; Craciunescu, O.; Steffey, B.; Folz, R.J.; Chao, N.J.; Rizzieri, D.A.; Marks, L.B. Severe Pulmonary Toxicity After Myeloablative Conditioning Using Total Body Irradiation: An Assessment of Risk Factors. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, 812–818. [Google Scholar] [CrossRef]
- Molls, M.; Quast, U.; Schaefer, U.W.; Szy, D.; Beelen, D.W.; Quabeck, K.; Graeven, U.; Sayer, H.G.; Bamberg, M.; Sack, H. Clinical Results and the Essen Concept of TBI. Radiother. Oncol. 1990, 18 (Suppl. S1), 121–124. [Google Scholar] [CrossRef]
- Oertel, M.; Kittel, C.; Martel, J.; Mikesch, J.-H.; Glashoerster, M.; Stelljes, M.; Eich, H.T. Pulmonary Toxicity after Total Body Irradiation—An Underrated Complication? Estimation of Risk via Normal Tissue Complication Probability Calculations and Correlation with Clinical Data. Cancers 2021, 13, 2946. [Google Scholar] [CrossRef]
- Hanania, A.N.; Mainwaring, W.; Ghebre, Y.T.; Hanania, N.A.; Ludwig, M. Radiation-Induced Lung Injury: Assessment and Management. Chest 2019, 156, 150–162. [Google Scholar] [CrossRef]
- Gogna, N.K.; Morgan, G.; Downs, K.; Atkinson, K.; Biggs, J. Lung Dose Rate and Interstitial Pneumonitis in Total Body Irradiation for Bone Marrow Transplantation. Australas. Radiol. 1992, 36, 317–320. [Google Scholar] [CrossRef]
- Lawton, C.A.; Barber-Derus, S.; Murray, K.J.; Casper, J.T.; Ash, R.C.; Gillin, M.T.; Frank Wilson, J. Technical Modifications in Hyperfractionated Total Body Irradiation for T-Lymphocyte Deplete Bone Marrow Transplant. Int. J. Radiat. Oncol. Biol. Phys. 1989, 17, 319–322. [Google Scholar] [CrossRef]
- Carruthers, S.A.; Wallington, M.M. Total Body Irradiation and Pneumonitis Risk: A Review of Outcomes. Br. J. Cancer 2004, 90, 2080–2084. [Google Scholar] [CrossRef]
- Borg, M.; Hughes, T.; Horvath, N.; Rice, M.; Thomas, A.C. Renal Toxicity after Total Body Irradiation. Int. J. Radiat. Oncol. Biol. Phys. 2002, 54, 1165–1173. [Google Scholar] [CrossRef]
- Sampath, S.; Schultheiss, T.E.; Wong, J. Dose Response and Factors Related to Interstitial Pneumonitis after Bone Marrow Transplant. Int. J. Radiat. Oncol. Biol. Phys. 2005, 63, 876–884. [Google Scholar] [CrossRef]
- Livesey, S.J.; Holmes, J.A.; Whittaker, J.A. Ocular Complications of Bone Marrow Transplantation. Eye 1989, 3 Pt 3, 271–276. [Google Scholar] [CrossRef]
- Belkacémi, Y.; Ozsahin, M.; Pène, F.; Rio, B.; Laporte, J.P.; Leblond, V.; Touboul, E.; Schlienger, M.; Gorin, N.C.; Laugier, A. Cataractogenesis after Total Body Irradiation. Int. J. Radiat. Oncol. Biol. Phys. 1996, 35, 53–60. [Google Scholar] [CrossRef]
- Bautista Juanes, J.A.; Theischen, M.; Beelen, D.W.; Pauleikhoff, D.; Koch, J.M.; Waubke, T.N.; Wessing, A. Ocular complications of long-term survival of bone marrow transplantation. A prospective study with 21 patients. Klin. Mon. Augenheilkd. 1993, 202, 110–115. [Google Scholar]
- Rodriguez, T.E. Neurologic Complications of Bone Marrow Transplantation. Handb. Clin. Neurol. 2014, 121, 1295–1304. [Google Scholar] [CrossRef]
- Darby, S.C.; Ewertz, M.; McGale, P.; Bennet, A.M.; Blom-Goldman, U.; Brønnum, D.; Correa, C.; Cutter, D.; Gagliardi, G.; Gigante, B.; et al. Risk of Ischemic Heart Disease in Women after Radiotherapy for Breast Cancer. N. Engl. J. Med. 2013, 368, 987–998. [Google Scholar] [CrossRef] [Green Version]
- Cutter, D.J.; Schaapveld, M.; Darby, S.C.; Hauptmann, M.; van Nimwegen, F.A.; Krol, A.D.G.; Janus, C.P.M.; van Leeuwen, F.E.; Aleman, B.M.P. Risk of Valvular Heart Disease after Treatment for Hodgkin Lymphoma. J. Natl. Cancer Inst. 2015, 107, djv008. [Google Scholar] [CrossRef]
- Miralbell, R.; Bieri, S.; Mermillod, B.; Helg, C.; Sancho, G.; Pastoors, B.; Keller, A.; Kurtz, J.M.; Chapuis, B. Renal Toxicity after Allogeneic Bone Marrow Transplantation: The Combined Effects of Total-Body Irradiation and Graft-versus-Host Disease. J. Clin. Oncol. 1996, 14, 579–585. [Google Scholar] [CrossRef]
- Delgado, J.; Cooper, N.; Thomson, K.; Duarte, R.; Jarmulowicz, M.; Cassoni, A.; Kottaridis, P.; Peggs, K.; Mackinnon, S. The Importance of Age, Fludarabine, and Total Body Irradiation in the Incidence and Severity of Chronic Renal Failure after Allogeneic Hematopoietic Cell Transplantation. Biol. Blood Marrow Transplant. 2006, 12, 75–83. [Google Scholar] [CrossRef] [Green Version]
- Zuro, D.; Vagge, S.; Broggi, S.; Agostinelli, S.; Takahashi, Y.; Brooks, J.; Leszcynska, P.; Liu, A.; Zucchetti, C.; Saldi, S.; et al. Multi-Institutional Evaluation of MVCT Guided Patient Registration and Dosimetric Precision in Total Marrow Irradiation: A Global Health Initiative by the International Consortium of Total Marrow Irradiation. Radiother. Oncol. 2019, 141, 275–282. [Google Scholar] [CrossRef]
| Patient Characteristics | n (% or Range) |
|---|---|
| Number of patients | 322 |
| Median age at transplantation | 47 (18–74) |
| Sex | |
| Male | 182 (56.5) |
| Female | 140 (43.5) |
| Diseases | |
| AML | 213 (66.1) |
| ALL | 91 (28.3) |
| MDS | 15 (4.7) |
| Biphenotypic leukemia | 2 (0.6) |
| T-PLL | 1 (0.3) |
| Graft-versus-host disease | |
| None | 121 (37.6) |
| Acute only | 70 (21.7) |
| Chronic | 128 (39.8) |
| No information | 3 (0.9) |
| TBI dose | |
| <8 Gy | 4 (1.2) |
| 8 Gy | 236 (73.3) |
| 12 Gy | 82 (25.5) |
| Conditioning regimens | |
| Fludarabine-8 Gy | 137 (42.5) |
| Melphalan-Fludarabine-8 Gy | 93 (28.9) |
| Cyclophosphamide-12 Gy | 68 (21.1) |
| Etoposide-12 Gy | 9 (2.8) |
| Other | 15 (4.7) |
| Previous cranial radiation | |
| Yes | 52 (16.1) |
| No | 267 (82.9) |
| No information | 3 (0.9) |
| Toxicity and Grade | n * (%) | TBI Dose | p-Value | |
|---|---|---|---|---|
| 8 Gy | 12 Gy | |||
| VOD | 2 (0.6) | 2 (0.8) | 0 | >0.99 |
| Mucositis ** | 251 (86.3) | 188 (85.1) | 62 (92.5) | <0.001 |
| Grades 1 and 2 | 99 (39.4) | 88 (46.8) | 10 (16.1) | |
| Grades 3–4 | 152 (60.6) | 100 (53.2) | 52 (83.9) | |
| Pulmonary | 77 (23.9) | 56 (23.7) | 19 (23.2) | 0.82 |
| Pneumonia | 42 (13.4) | 30 (12.2) | 11 (11.8) | |
| Bronchial obstruction | 20 (6.2) | 14 (5.9) | 6 (7.3) | |
| Dyspnea | 9 (2.8) | 8 (3.4) | 1 (1.2) | |
| Pleural effusion | 7 (2.2) | 5 (2.1) | 1 (1.2) | |
| ARDS | 2 (0.6) | 1 (0.4) | 1 (1.2) | |
| Other | 4 (1.2) | 4 (1.6) | 0 | |
| Grades 1 and 2 | 50 (64.9) | 40 (71.4) | 10 (55.5) | |
| Grades 3–5 | 27 (35.1) | 16 (28.6) | 9 (44.5) | |
| Cardiac | 45 (14.0) | 31 (13.1) | 13 (15.9) | 0.58 |
| Heart failure | 12 (3.7) | 10 (4.0) | 1 (1.1) | |
| Pericardial effusion | 8 (2.5) | 5 (2.0) | 3 (3.3) | |
| Atrial fibrillation | 7 (2.2) | 5 (2.0) | 2 (2.2) | |
| Other cardiac arrhythmias | 6 (1.9) | 3 (1.3) | 3 (3.3) | |
| Valve disease | 6 (1.9) | 5 (2.0) | 1 (1.1) | |
| Coronary heart disease | 5 (1.6) | 5 (2.0) | 0 | |
| Myocarditis | 3 (0.9) | 2 (0.8) | 1 (1.1) | |
| Other | 4 (1.2) | 2 (0.8) | 2 (2.2) | |
| Grades 1 and 2 | 28 (70.0) | 22 (84.6) | 6 (46.2) | |
| Grades 3–5 *** | 12 (30.0) | 4 (15.4) | 7 (53.8) | |
| Ocular | 76 (23.6) | 45 (19.1) | 30 (36.6) | 0.013 |
| Sicca-Syndrome | 52 (16.1) | 28 (11.4) | 23 (24.7) | |
| Cataract | 20 (6.2) | 11 (4.5) | 9 (9.6) | |
| Other | 13 (4.0) | 9 (3.7) | 4 (4.3) | |
| Grades 1 and 2 | 52 (80.0) | 30 (76.9) | 21 (84.0) | |
| Grades 3–5 **** | 13 (20.0) | 9 (23.1) | 4 (16.0) | |
| Neurological | 77 (23.9) | 59 (25.0) | 17 (20.7) | 0.78 |
| Polyneuropathy | 63 (19.6) | 49 (20.0) | 14 (15.0) | |
| Concentration impairment | 15 (6.1) | 13 (5.3) | 2 (2.2) | |
| Leukoencephalopathy | 2 (0.6) | 0 | 1 (1.1) | |
| Grades 1 and 2 | 67 (87.0) | 53 (89.8) | 14 (82.3) | |
| Grades 3–5 | 10 (13.0) | 6 (10.2) | 3 (17.6) | |
| Renal | 65 (20.2) | 57 (24.2) | 7 (8.5) | 0.002 |
| Grades 1 and 2 | 58 (89.2) | 52 (91.2) | 5 (71.4) | |
| Grades 3–5 | 7 (10.8) | 5 (8.8) | 2 (28.6) | |
| Secondary neoplasia | 17 (5.3) | 13 (5.5) | 4 (3.9) | 0.96 |
| Toxicity | Variable | Comparison | Univariate Analysis | Multivariate Analysis | Multivariate Analysis | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Step One | Step Two | ||||||||||
| RR | Range | p | RR | Range | p | RR | Range | p | |||
| Disease | ALL vs. AML | 0.71 | 0.34–1.50 | 0.371 | |||||||
| MDS vs. AML | 1.46 | 0.45–4.77 | 0.533 | ||||||||
| Cardiac | TBI dose | 12 Gy vs. 8 Gy | 0.73 | 0.36–1.47 | 0.373 | ||||||
| Sex | male vs. female | 1.32 | 0.72–2.41 | 0.378 | |||||||
| Age at SCT | 1.03 | 1.00–1.05 | 0.048 | ||||||||
| Disease | ALL vs. AML | 1.04 | 0.63–1.71 | 0.886 | |||||||
| MDS vs. AML | 0.81 | 0.25–2.61 | 0.729 | ||||||||
| TBI dose | 12 Gy vs. 8 Gy | 0.75 | 0.44–1.29 | 0.301 | |||||||
| Pulmonary | Conditioning | flu vs. cy | 1.79 | 0.98–3.30 | 0.060 | ||||||
| chemotherapy | |||||||||||
| Sex | male vs. female | 0.90 | 0.57–1.42 | 0.641 | |||||||
| Age at SCT | 1.01 | 1.00–1.03 | 0.139 | ||||||||
| Disease | ALL vs. AML | 0.25 | 0.11–0.56 | 0.001 | 0.32 | 0.13–0.78 | 0.012 | 0.31 | 0.13–0.74 | 0.008 | |
| MDS vs. AML | 1.07 | 0.33–3.50 | 0.910 | 0.99 | 0.30–3.32 | 0.991 | 1.00 | 0.30–3.34 | 0.997 | ||
| Renal | TBI dose | 12 Gy vs. 8 Gy | 0.29 | 0.13–0.67 | 0.004 | 0.90 | 0.35–2.33 | 0.826 | |||
| Sex | male vs. female | 0.94 | 0.55–1.63 | 0.836 | |||||||
| Age at SCT | 1.06 | 1.03–1.09 | <0.001 | 1.06 | 1.03–1.09 | <0.001 | 1.06 | 1.03–1.09 | <0.001 | ||
| Disease | ALL vs. AML | 1.23 | 0.70–2.17 | 0.471 | |||||||
| MDS vs. AML | 1.25 | 0.38–4.10 | 0.713 | ||||||||
| Neurological | TBI dose | 12 Gy vs. 8 Gy | 0.94 | 0.81–1.10 | 0.436 | ||||||
| Sex | male vs. female | 0.63 | 0.37–1.07 | 0.089 | |||||||
| Age at SCT | 1.02 | 1.00–1.04 | 0.147 | ||||||||
| Disease | ALL vs. AML | 1.27 | 0.72–2.23 | 0.417 | |||||||
| MDS vs. AML | 1.77 | 0.58–5.42 | 0.320 | ||||||||
| TBI dose | 12 Gy vs. 8 Gy | 2.45 | 1.41–4.26 | 0.002 | 2.29 | 1.22–4.30 | 0.010 | 2.60 | 1.49–4.54 | 0.001 | |
| Ocular | Sex | male vs. female | 1.33 | 0.79–2.26 | 0.285 | ||||||
| Age at SCT | 1.00 | 0.99–1.02 | 0.689 | ||||||||
| Previous cranial | yes vs. no | 2.12 | 1.12–4.00 | 0.020 | 1.38 | 0.67–2.85 | 0.387 | ||||
| irradiation | |||||||||||
| Disease | ALL vs. AML | 0.90 | 0.28–2.92 | 0.865 | |||||||
| Secondary | MDS vs. AML | 3.28 | 0.70–15.33 | 0.130 | |||||||
| neoplasia | TBI dose | 12 Gy vs. 8 Gy | 0.44 | 0.14–1.42 | 0.168 | ||||||
| Sex | male vs. female | 1.80 | 0.62–5.21 | 0.278 | |||||||
| Age at SCT | 1.04 | 1.00–1.08 | 0.078 | ||||||||
| Study | n | Age (y) | FU (M) | TBI Dose | Pulmo. | Card | Renal | Ocular | Neuro. | 2nd Mal. |
|---|---|---|---|---|---|---|---|---|---|---|
| Belkacémi, 1998 [21] | 326 (118 alloSCT) | 3–63 (median 30) | 68 | 10 Gy/1 fx 12 Gy/6 fx | 19% * | n.a. | n.a. | cataract: 8% * | n.a. | n.a. |
| Bölling, 2011 [19] | 120 | 18–70 (mean 46.1) | 23 | 4–12 Gy/2–6 fx | 20.4% (8.6%) ** | n.a. | 12.8% | cataract: 8.6% | n.a. | 5.8% |
| De Felice, 2016 [22] | 211 (48 adults) | 3–53 (median 14) | 40 | 12 Gy/6 fx | 9% (adults: 8.3%) | n.a. | n.a. | cataract: 12.8% (adults: 10.4%) | n.a. | 0% |
| Marnitz, 2014 [20] | 110 (62 alloSCT) | 17–54 (mean 34) | 68 | n.a. | 15.5% * | n.a. | n.a. | 28% * | n.a. | 0% |
| Thomas, 2001 [18] | 186 (42% alloSCT) | 15–60 (median 36.5) | 55 | 10 Gy/1 fx 12–13.5 Gy/6 fx | 19% * | n.a. | n.a. | 28% * (15% cataract) | n.a. | n.a. |
| Present study | 322 | 18–74 (median 47) | 68 | 8–12 Gy/4–6 fx | 23.9% | 14.0% | 20.2% | 23.6% (6.2% cataract) | 23.9% | 5.3% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oertel, M.; Martel, J.; Mikesch, J.-H.; Scobioala, S.; Reicherts, C.; Kröger, K.; Lenz, G.; Stelljes, M.; Eich, H.T. The Burden of Survivorship on Hematological Patients—Long-Term Analysis of Toxicities after Total Body Irradiation and Allogeneic Stem Cell Transplantation. Cancers 2021, 13, 5640. https://doi.org/10.3390/cancers13225640
Oertel M, Martel J, Mikesch J-H, Scobioala S, Reicherts C, Kröger K, Lenz G, Stelljes M, Eich HT. The Burden of Survivorship on Hematological Patients—Long-Term Analysis of Toxicities after Total Body Irradiation and Allogeneic Stem Cell Transplantation. Cancers. 2021; 13(22):5640. https://doi.org/10.3390/cancers13225640
Chicago/Turabian StyleOertel, Michael, Jonas Martel, Jan-Henrik Mikesch, Sergiu Scobioala, Christian Reicherts, Kai Kröger, Georg Lenz, Matthias Stelljes, and Hans Theodor Eich. 2021. "The Burden of Survivorship on Hematological Patients—Long-Term Analysis of Toxicities after Total Body Irradiation and Allogeneic Stem Cell Transplantation" Cancers 13, no. 22: 5640. https://doi.org/10.3390/cancers13225640
APA StyleOertel, M., Martel, J., Mikesch, J.-H., Scobioala, S., Reicherts, C., Kröger, K., Lenz, G., Stelljes, M., & Eich, H. T. (2021). The Burden of Survivorship on Hematological Patients—Long-Term Analysis of Toxicities after Total Body Irradiation and Allogeneic Stem Cell Transplantation. Cancers, 13(22), 5640. https://doi.org/10.3390/cancers13225640