Evaluation of Orthodontic Mini-Implants’ Stability Based on Insertion and Removal Torques: An Experimental Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Sample Preparation
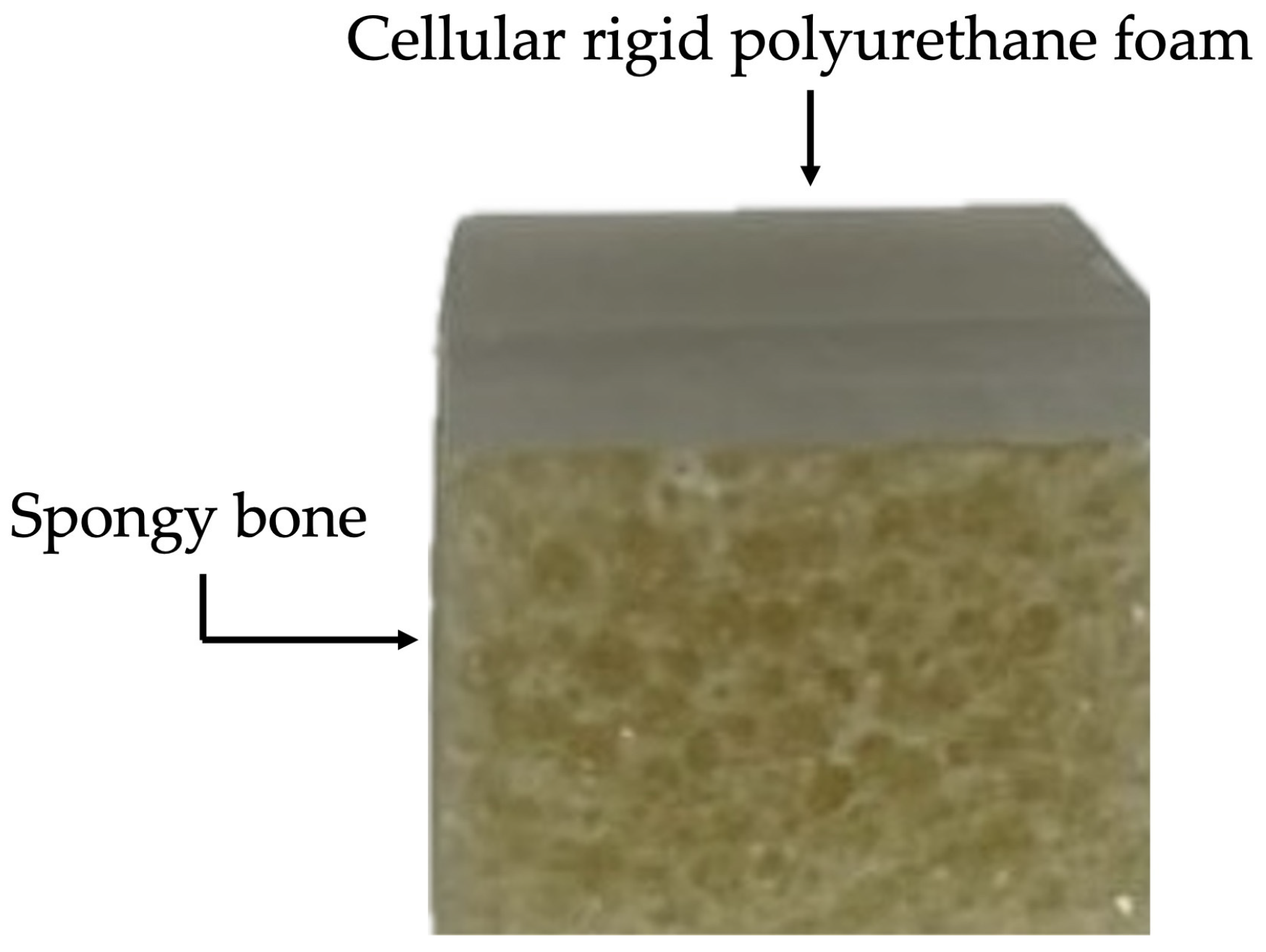
2.2.2. Elaboration of Artificial Bone Block
2.2.3. Insertion of MIs into Artificial Bone
2.2.4. Ageing of MIs in Saliva and Removal from the Artificial Bone
2.2.5. Maximum Insertion and Removal Torque Measurements
2.2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wilmes, B.; Panayotidis, A.; Drescher, D. Fracture resistance of orthodontic mini-implants: A biomechanical in vitro study. Eur. J. Orthod. 2011, 33, 396–401. [Google Scholar] [CrossRef] [PubMed]
- da Nova, M.F.P.; Carvalho, F.R.; Elias, C.N.; Artese, F. Avaliação do torque para inserção, remoção e fratura de diferentes mini-implantes ortodônticos. Rev. Dent. Press Ortodon. Ortop. Facial 2008, 13, 76–87. [Google Scholar] [CrossRef]
- Elias, C.N.; Guimarães, G.S.; Muller, C.A. Torque de inserção e de remoção de miniparafusos ortodônticos. Rev. Bras. Implant. 2005, 11, 5–8. [Google Scholar]
- Takaki, T.; Tamura, N.; Yamamoto, M.; Takano, N.; Shibahara, T.; Yasumura, T.; Nishii, Y.; Sueishi, K. Clinical Study of Temporary Anchorage Devices for Orthodontic Treatment. Bull. Tokyo Dent. Coll. 2010, 51, 151–163. [Google Scholar] [CrossRef]
- Assad-Loss, T.F.; Kitahara-Céia, F.M.F.; Silveira, G.S.; Elias, C.N.; Mucha, J.N. Fracture strength of orthodontic mini-implants. Dental Press J. Orthod. 2017, 22, 47–54. [Google Scholar] [CrossRef]
- Barros, S.E.; Janson, G.; Chiqueto, K.; Garib, D.G.; Janson, M. Effect of mini-implant diameter on fracture risk and self-drilling efficacy. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 181–192. [Google Scholar] [CrossRef]
- Pithon, M.M.; Nojima, M.G.; Nojima, L.I. In vitro evaluation of insertion and removal torques of orthodontic mini-implants. Int. J. Oral Maxillofac. Surg. 2011, 40, 80–85. [Google Scholar] [CrossRef]
- Deguchi, T.; Takano-Yamamoto, T.; Kanomi, R.; Hartsfield, J.K.; Roberts, W.E.; Garetto, L.P. The Use of Small Titanium Screws for Orthodontic Anchorage. J. Dent. Res. 2003, 82, 377–381. [Google Scholar] [CrossRef]
- Huja, S.S.; Litsky, A.S.; Beck, F.M.; Johnson, K.A.; Larsen, P.E. Pull-out strength of monocortical screws placed in the maxillae and mandibles of dogs. Am. J. Orthod. Dentofac. Orthop. 2005, 127, 307–313. [Google Scholar] [CrossRef]
- Chen, F.; Terada, K.; Hanada, K.; Saito, I. Anchorage effect of osseointegrated vs nonosseointegrated palatal implants. Angle Orthod. 2006, 76, 660–665. [Google Scholar]
- Melsen, B.; Costa, A. Immediate loading of implants used for orthodontic anchorage. Clin. Orthod. Res. 2000, 3, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Wilmes, B.; Rademacher, C.; Olthoff, G.; Drescher, D. Parameters affecting primary stability of orthodontic mini-implants. J. Orofac. Orthop. 2006, 67, 162–174. [Google Scholar] [CrossRef] [PubMed]
- Vinodh, S.; Sangamesh, B.; Neelakantha, P.V.; Ahmed, S.; Venkat, N.B. Fracture Resistance of Commonly Used Self-drilling Mini-implants of Various Diameters. J. Indian Orthod. Soc. 2020, 54, 31–38. [Google Scholar] [CrossRef]
- Kim, S.H.; Cho, J.H.; Chung, K.R.; Kook, Y.A.; Nelson, G. Removal torque values of surface-treated mini-implants after loading. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 36–43. [Google Scholar] [CrossRef]
- Proffit, W.R.; Fields, H.W.; Larson, B.; Sarver, D.M. Contemporary Orthodontics, 6th ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2019; p. 828. [Google Scholar]
- Dilek, O.; Tezulas, E.; Dincel, M. Required minimum primary stability and torque values for immediate loading of mini dental implants: An experimental study in nonviable bovine femoral bone. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 105, 20–27. [Google Scholar] [CrossRef]
- Brown, R.N.; Sexton, B.E.; Chu, T.M.G.; Katona, T.R.; Stewart, K.T.; Kyung, H.M.; Liu, S.S.Y. Comparison of stainless steel and titanium alloy orthodontic miniscrew implants: A mechanical and histologic analysis. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 496–504. [Google Scholar] [CrossRef]
- Bicudo, P.; Reis, J.; Deus, A.M.; Reis, L.; Vaz, M.F. Performance evaluation of dental implants: An experimental and numerical simulation study. Theor. Appl. Fract. Mech. 2016, 85 Pt A, 74–83. [Google Scholar] [CrossRef]
- Reynders, R.A.M.; Ronchi, L.; Ladu, L.; Etten-Jamaludin, F.V.; Bipat, S. Insertion torque and success of orthodontic mini-implants: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 596–614. [Google Scholar] [CrossRef]
- Best Anatomical Medical Training Models Company|Sawbones. Available online: https://www.sawbones.com (accessed on 19 June 2024).
- Sousa-Santos, S.; Silva, A.S.; Sousa-Santos, P.; Vale, T.; Mendes, J.M. The Influence of Saliva pH on the Fracture Resistance of Two Types of Implant-Supported Bis-Acrylic Resin Provisional Crowns—An In Vitro Study. J. Funct. Biomater. 2023, 14, 62. [Google Scholar] [CrossRef]
- ISO 9001:2015; Quality Management Systems Requirements. International Standard ISO (International Organization for Standardization): Geneva, Switzerland, 2015.
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2023. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: London, UK, 1988. [Google Scholar]
- Gracco, A.; Giagnorio, C.; Siciliani, G. Structure and mechanical properties of orthodontic miniscrew implants. In Skeletal Anchorage in Orthodontic Treatment of Class II Malocclusion; Elsevier: Maryland Heights, MO, USA, 2015; pp. 39–47. [Google Scholar] [CrossRef]
- Walter, A.; Winsauer, H.; Marcé-Nogué, J.; Mojal, S.; Puigdollers, A. Design characteristics, primary stability and risk of fracture of orthodontic miniimplants: Pilot scan electron microscope and mechanical studies. Med. Oral Patol. Oral Cir. Bucal. 2013, 18, 804–810. [Google Scholar] [CrossRef]
- Melsen, B. Mini-implants: Where are we? J. Clin. Orthod. 2005, 39, 539–547. [Google Scholar] [PubMed]
- Palissery, V.; Taylor, M.; Browne, M. Fatigue characterization of a polymer foam to use as a cancellous bone analog material in the assessment of orthopaedic devices. J. Mater. Sci. Mater. Med. 2004, 15, 61–67. [Google Scholar] [CrossRef] [PubMed]
- ASTM F1839-08(2021); Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopedic Devices and Instruments. ASTM: West Conshohocken, PA, USA, 2021.
- Elias, C.N.; Rocha, F.A.; Nascimento, A.L.; Coelho, P.G. Influence of implant shape, surface morphology, surgical technique and bone quality on the primary stability of dental implants. J. Mech. Behav. Biomed. Mater. 2012, 16, 169–180. [Google Scholar] [CrossRef]
- Liu, C.; Tsai, M.T.; Huang, H.L.; Chen, M.Y.C.; Hsu, J.T.; Su, K.C.; Chang, C.H.; Wu, A.Y.J. Relation between insertion torque and bone-implant contact percentage: An artificial bone study. Clin. Oral Investig. 2012, 16, 1679–1684. [Google Scholar] [CrossRef]
- Sousa-Santos, C.; Sousa-Santos, S.; Mendes, J.; Coelho, C.; Aroso, C.; Sousa-Santos, P.; Mendes, J.M. The Influence of the Diameter of Orthodontic Mini-Implants on Primary Stability: Bending Tests—An In Vitro Study. Materials 2024, 17, 3149. [Google Scholar] [CrossRef]
- Tseng, Y.C.; Wu, J.H.; Chen, H.S.; Chen, C.M.; Ting, C.C. Evaluation of mechanical strengths of three types of mini-implants in artificial bones. Kaohsiung J. Med. Sci. 2017, 33, 578–583. [Google Scholar] [CrossRef]
- Trisi, P.; Perfetti, G.; Baldoni, E.; Berardi, D.; Colagiovanni, M.; Scogna, G. Implant micromotion is related to peak insertion torque and bone density. Clin. Oral Implants Res. 2009, 20, 467–471. [Google Scholar] [CrossRef]
- Motoyoshi, M.; Hirabayashi, M.; Uemura, M.; Shimizu, N. Recommended placement torque when tightening an orthodontic mini-implant. Clin. Oral Implants Res. 2005, 17, 109–114. [Google Scholar] [CrossRef]
- Motoyoshi, M.; Matsuoka, M.; Shimizu, N. Application of orthodontic mini-implants in adolescents. Int. J. Oral Maxillofac. Surg. 2007, 36, 695–699. [Google Scholar] [CrossRef]
- Motoyoshi, M.; Yoshida, T.; Ono, A.; Shimizu, N. Effect of cortical bone thickness and implant placement torque on stability of orthodontic mini-implants. Int. J. Oral Maxillofac. Implants 2007, 22, 779–784. [Google Scholar]
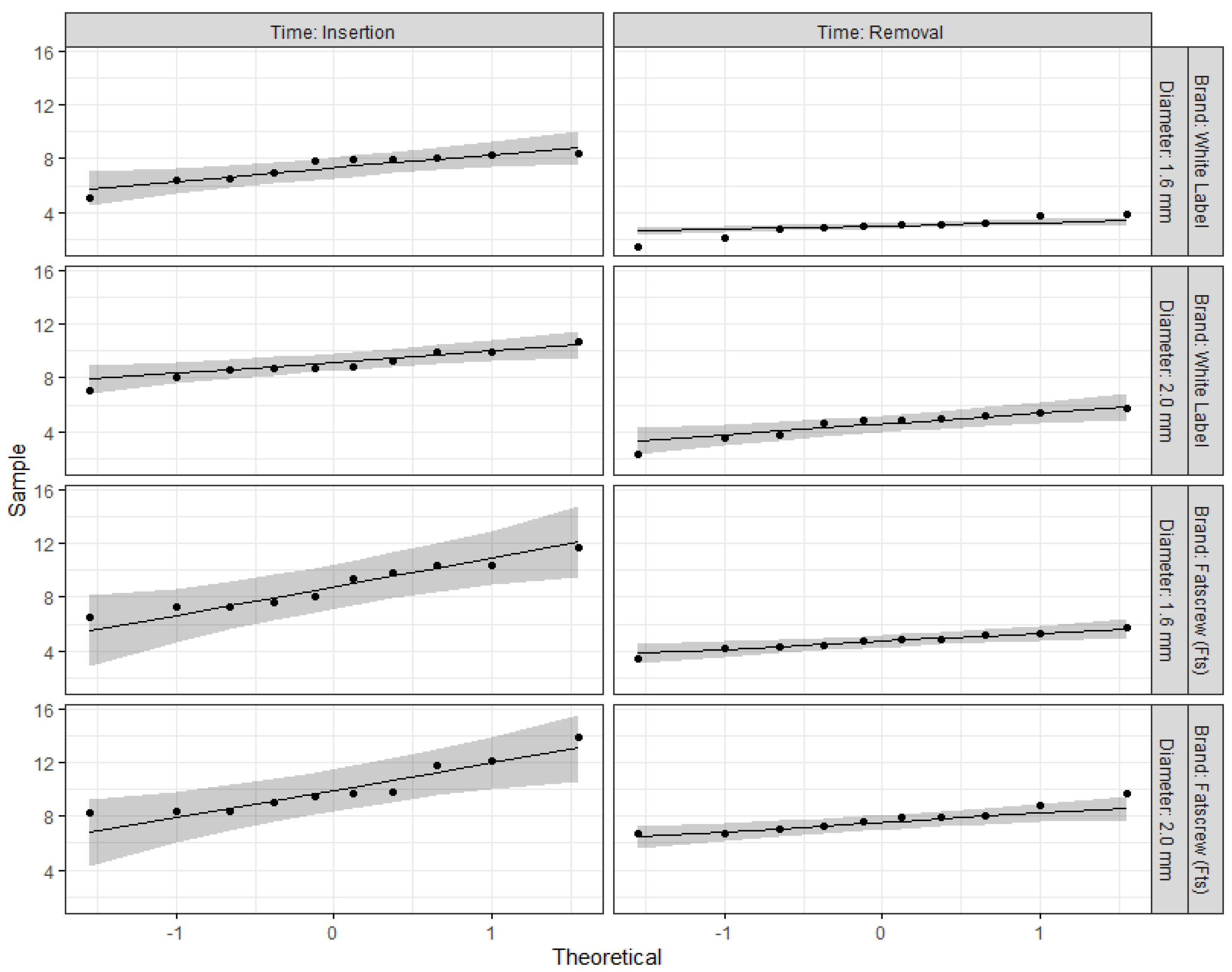


| F-Test(1,9) | p-Value | η2g | |
|---|---|---|---|
| Three-way effects | |||
| Brand | 67.13 | <0.001 *** | 0.41 |
| Diameter | 60.10 | <0.001 *** | 0.41 |
| Time | 211.08 | <0.001 *** | 0.74 |
| Brand vs. diameter | 0.47 | 0.512 | 0.011 |
| Brand vs. time | 7.87 | 0.021 * | 0.07 |
| Diameter vs. time | 2.72 | 0.133 | 0.04 |
| Brand vs. diameter vs. time | 2.27 | 0.166 | 0.04 |
| Two-way effects (stratified by brand) | |||
| Brand: White label | |||
| Diameter | 13.90 | 0.005 ** | 0.44 |
| Time | 632.00 | <0.001 *** | 0.85 |
| Diameter vs. time | 0.01 | 0.936 | 0.00 |
| Brand: Fatscrew (Fts) | |||
| Diameter | 19.10 | 0.002 ** | 0.40 |
| Time | 51.50 | <0.001 *** | 0.59 |
| Diameter vs. time | 3.44 | 0.097 | 0.11 |
| Simple effects (stratified by brand: diameter) | |||
| White label: 1.6 mm | 131.00 | <0.001 *** | 0.87 |
| White label: 2.0 mm | 181.00 | <0.001 *** | 0.84 |
| Fts: 1.6 mm | 40.60 | <0.001 *** | 0.74 |
| Fts: 2.0 mm | 11.20 | 0.009 ** | 0.40 |
| Insertion Torque (Ncm) | Removal Torque (Ncm) | |
|---|---|---|
| Brand | ||
| White label | 8.16 (0.33) | 3.73 (0.20) |
| Fatscrew (Fts) | 9.45 (0.33) | 6.23 (0.20) |
| Overall | 8.81 (0.23) | 4.98 (0.13) |
| Diameter | ||
| 1.6 mm | 8.09 (0.33) | 3.81 (0.19) |
| 2.0 mm | 9.53 (0.33) | 6.15 (0.19) |
| Overall | 8.81 (0.23) | 4.98 (0.13) |
| Brand: White label | ||
| Diameter: 1.6 mm | 7.34 (0.47) | 2.93 (0.27) |
| Diameter: 2.0 mm | 8.99 (0.47) | 4.52 (0.27) |
| Brand: Fts | ||
| Diameter: 1.6 mm | 8.83 (0.47) | 4.69 (0.27) |
| Diameter: 2.0 mm | 10.07 (0.47) | 7.77 (0.27) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sousa-Santos, P.; Sousa-Santos, S.; Oliveira, A.C.; Queirós, C.; Mendes, J.; Aroso, C.; Mendes, J.M. Evaluation of Orthodontic Mini-Implants’ Stability Based on Insertion and Removal Torques: An Experimental Study. Bioengineering 2025, 12, 549. https://doi.org/10.3390/bioengineering12050549
Sousa-Santos P, Sousa-Santos S, Oliveira AC, Queirós C, Mendes J, Aroso C, Mendes JM. Evaluation of Orthodontic Mini-Implants’ Stability Based on Insertion and Removal Torques: An Experimental Study. Bioengineering. 2025; 12(5):549. https://doi.org/10.3390/bioengineering12050549
Chicago/Turabian StyleSousa-Santos, Primavera, Sofia Sousa-Santos, Ana Catarina Oliveira, Cíntia Queirós, Joana Mendes, Carlos Aroso, and José Manuel Mendes. 2025. "Evaluation of Orthodontic Mini-Implants’ Stability Based on Insertion and Removal Torques: An Experimental Study" Bioengineering 12, no. 5: 549. https://doi.org/10.3390/bioengineering12050549
APA StyleSousa-Santos, P., Sousa-Santos, S., Oliveira, A. C., Queirós, C., Mendes, J., Aroso, C., & Mendes, J. M. (2025). Evaluation of Orthodontic Mini-Implants’ Stability Based on Insertion and Removal Torques: An Experimental Study. Bioengineering, 12(5), 549. https://doi.org/10.3390/bioengineering12050549










