Relationship between Empowerment and Functioning and Disability in Older Japanese Patients: A Covariance Structure Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.1.1. Inclusion Criteria
- (1)
- The patients or their families consented to participate in this study at the time of admission.
- (2)
- The patients were able to understand the questions (a Mini-Mental State Examination [MMSE] score of 11 or above [13]).
2.1.2. Exclusion Criteria
- (1)
- The patients had a risk of deterioration of their medical condition owing to participation in the survey, as determined by the attending physician.
- (2)
- The patients were unable to understand the questions owing to a decreased level of consciousness or mental function.
2.2. Survey Items
2.2.1. Selection of Survey Items
2.2.2. Inclusion Criteria
- (1)
- Previous studies have shown the association with empowerment.
- (2)
- The surveys, measurement, and collection of information from the medical records of older patients in the hospital environment and daily care situations were possible.
- (3)
- Those considered necessary for the promotion of health and care of older patients.
2.2.3. Exclusion Criteria
- (1)
- The evaluation/measurement placed a physical and emotional burden on the
- (2)
- Older patient.
- (3)
- The evaluation/measurement may have placed the patient at risk for disease exacerbation.
- (4)
- There was an excessive financial burden for conducting the survey.
2.2.4. Collection of Items
2.2.5. Medical Information
2.2.6. Individual Patient Characteristics
2.2.7. Evaluation and Measurement Items
2.2.8. Empowerment
2.2.9. Cognitive Function
2.2.10. Muscle Strength
2.2.11. Pain
2.2.12. Activities of Daily Living
2.2.13. Physical Activity
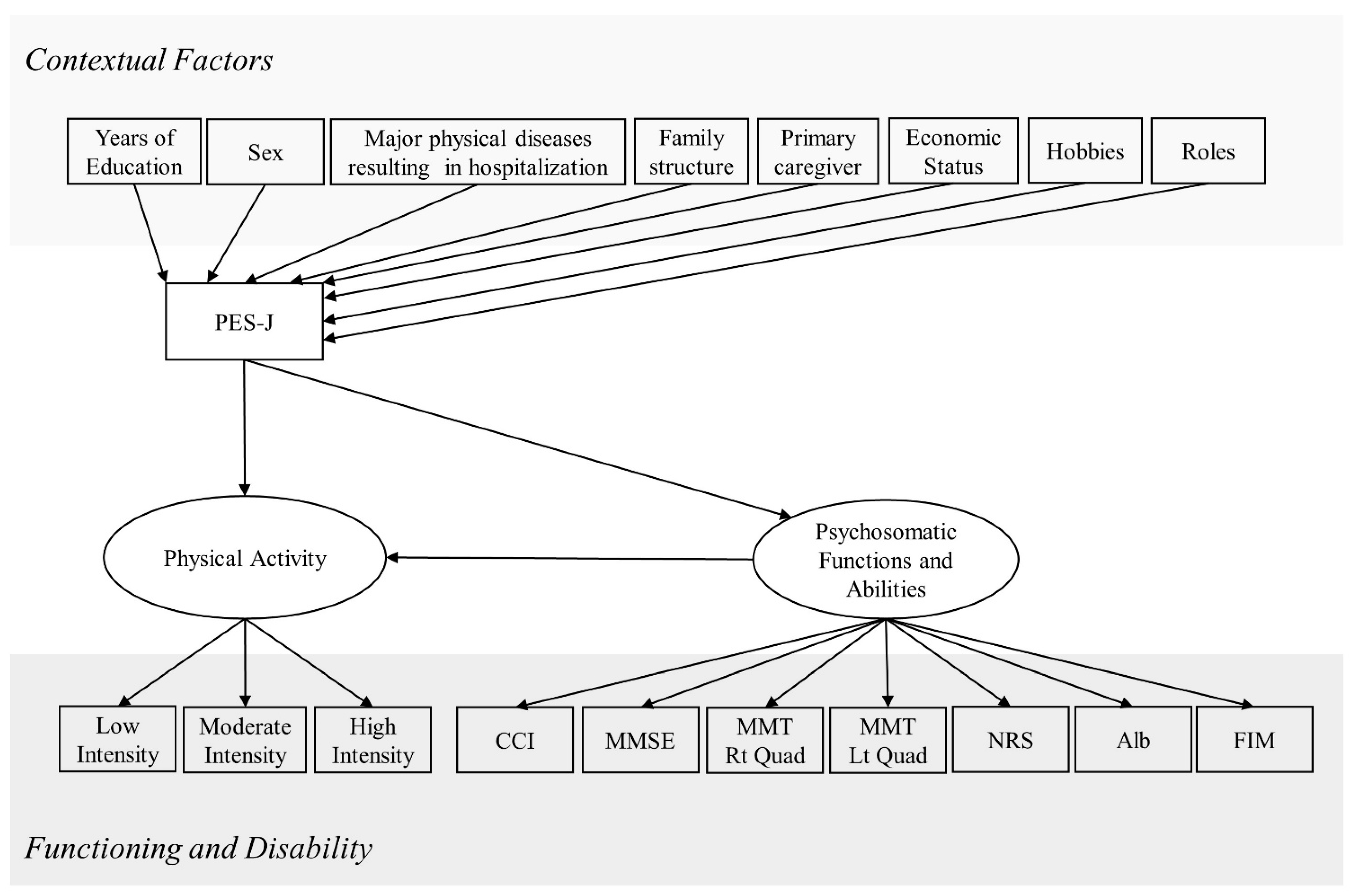
2.3. Data Analytical Strategy
3. Results
3.1. Participant Characteristics
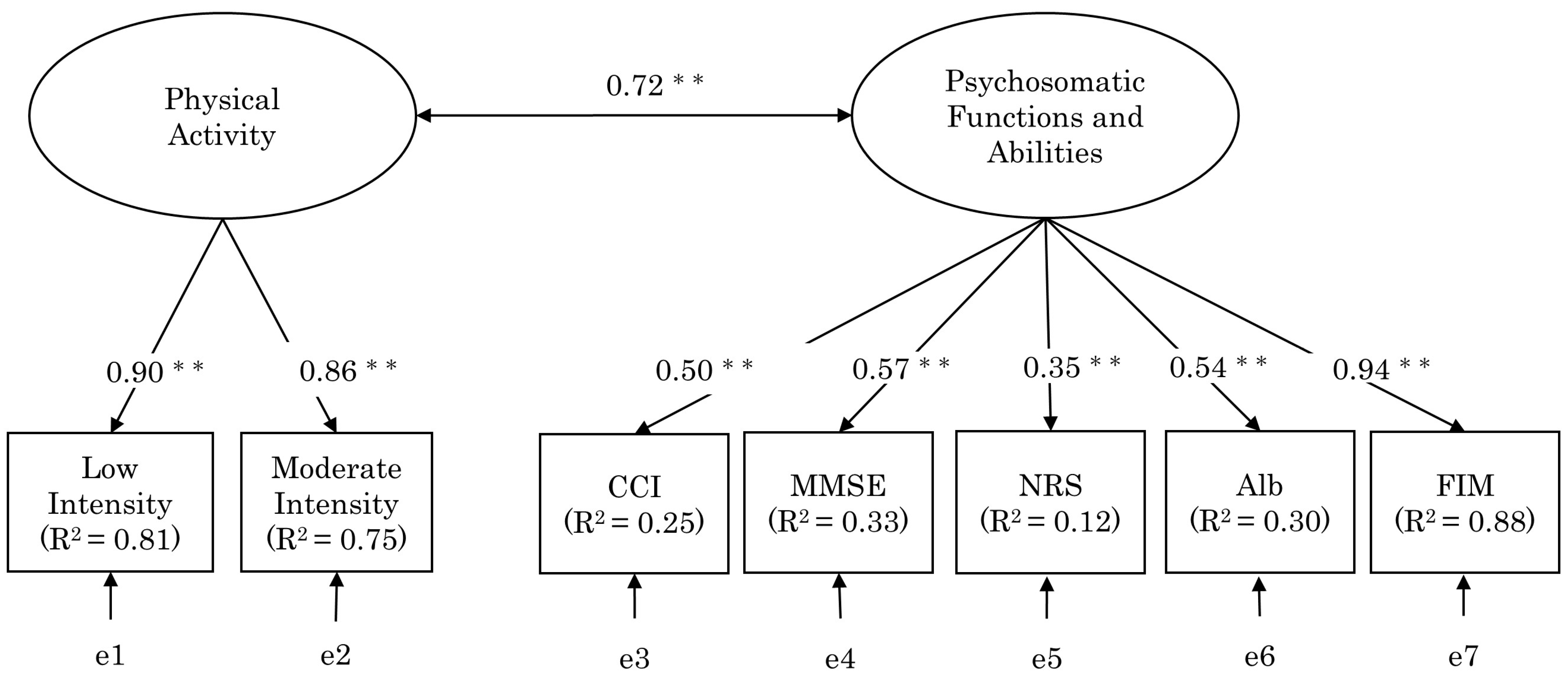
3.2. Process for Selecting the Items Constituting the Structural Model
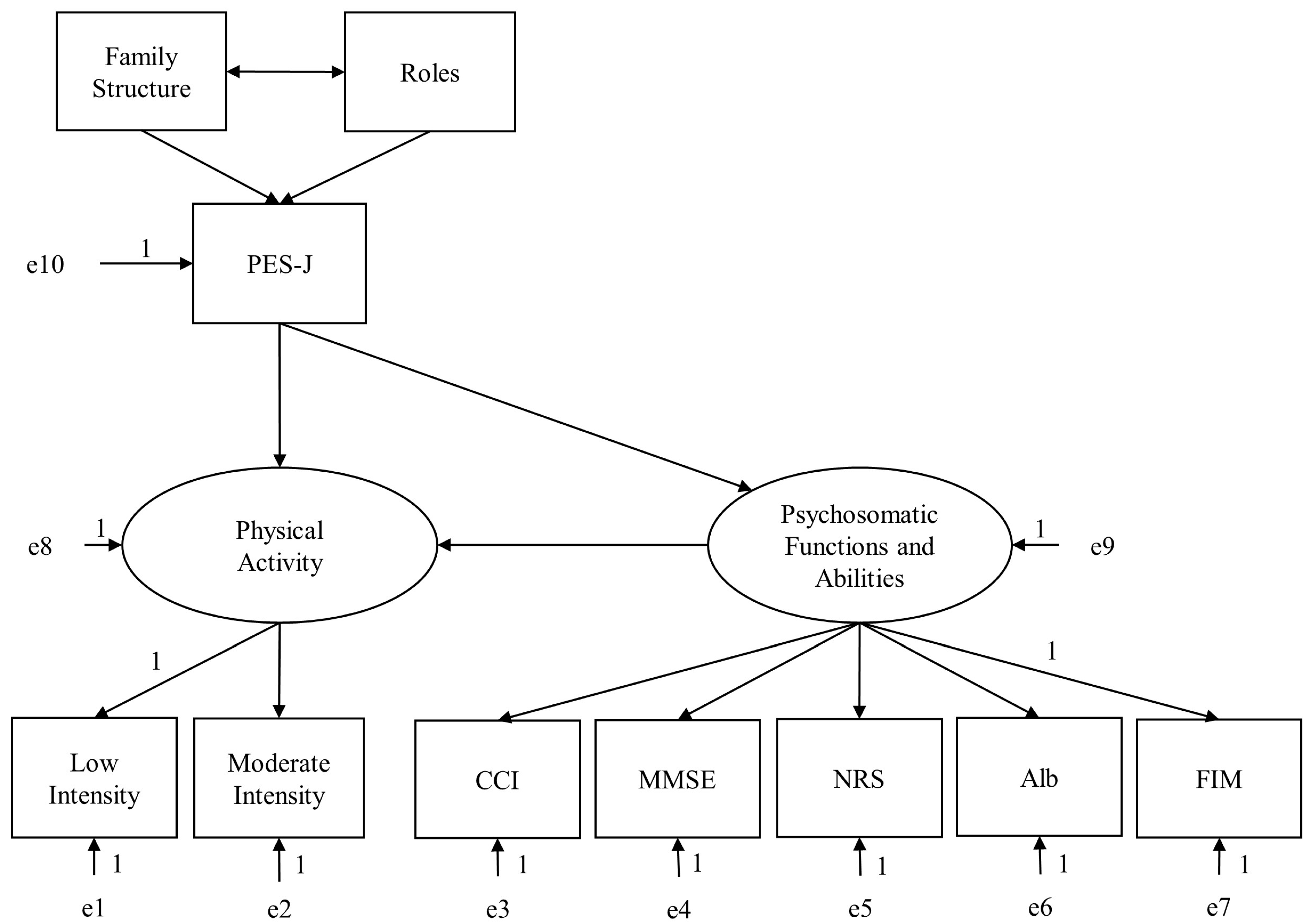
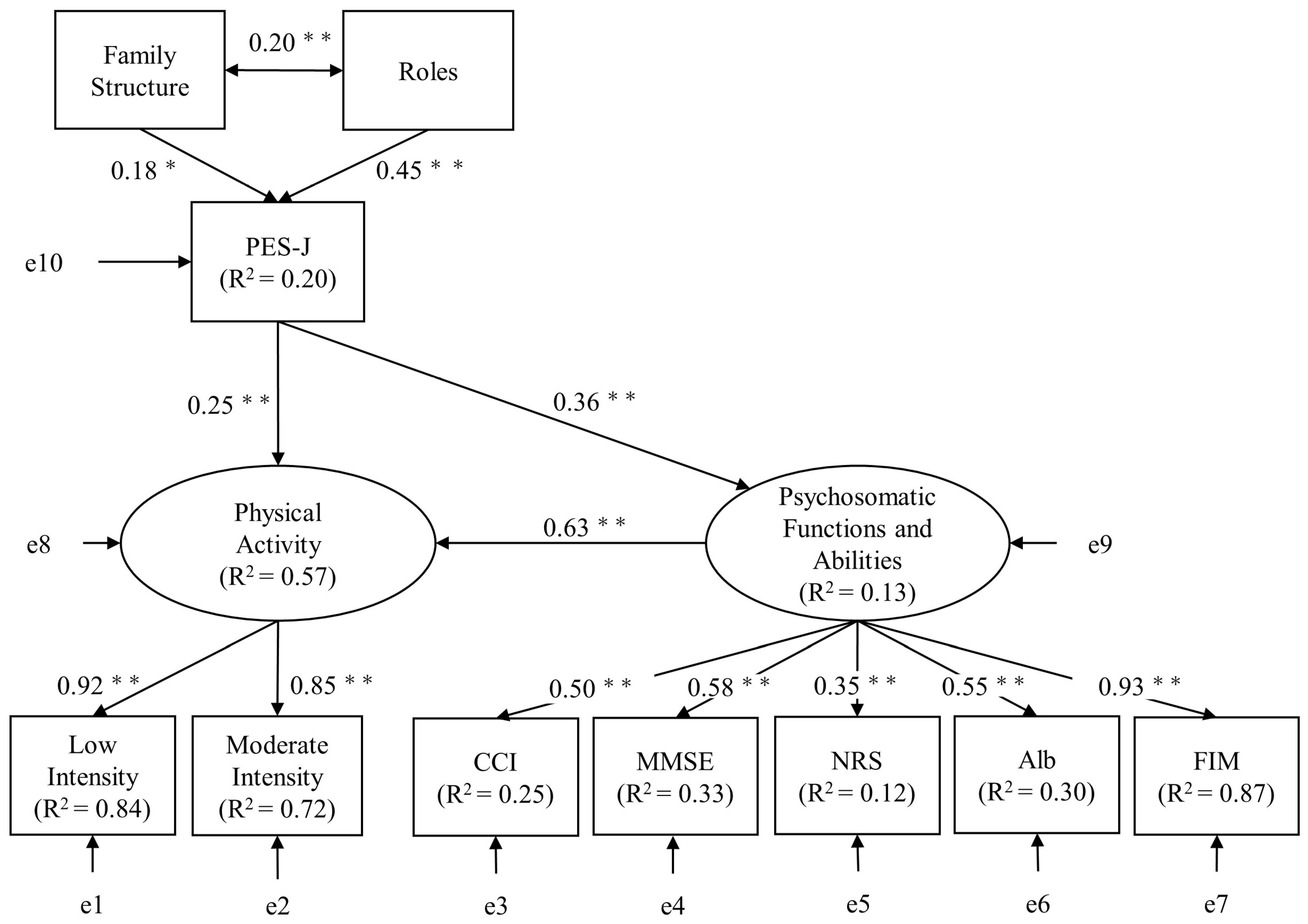
3.3. Relationship between Factor Structure in Functioning and Disability and Empowerment
4. Discussion
4.1. Contextual Factors Affecting Empowerment
4.2. Impact of Empowerment on Functioning and Disability
4.3. The Application of Empowerment in Older Adults’ Healthcare
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Greenwood, N.; Smith, R. The experiences of people with young-onset dementia: A meta-ethnographic review of the qualitative literature. Maturitas 2016, 92, 102–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giacomini, M.; DeJean, D.; Simeonov, D.; Smith, A. Experiences of living and dying with COPD: A systematic review and synthesis of the qualitative empirical literature. Ont. Health Technol. Assess. Ser. 2012, 12, 1–47. [Google Scholar] [PubMed]
- Hussain, J.A.; Flemming, K.; Murtagh, F.E.; Johnson, M.J. Patient and Health Care Professional Decision-Making to Commence and Withdraw from Renal Dialysis: A Systematic Review of Qualitative Research. Clin. J. Am. Soc. Nephrol. 2015, 10, 1201–1215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Momose, Y. Koureisya herusupuromōsyon ni okeru enpawāmento syakudo no kaihatsu [Development of the empowerment scale for the elderly (ESE) in health promotion]. J. Phys. Educ. Med. 2007, 8, 21–32. [Google Scholar] [CrossRef]
- Miyanaga, R.; Poudyal, H. Participation of nurses and care workers in the decision-making process for people with dementia in Japan: Discussion paper. Int. J. Nurs. Stud. 2019, 96, 91–98. [Google Scholar] [CrossRef]
- Bravo, P.; Edwards, A.; Barr, P.J.; Scholl, I.; Elwyn, G.; McAllister, M.; Cochrane Healthcare Quality Research Group; Cardiff University. Conceptualising patient empowerment: A mixed methods study. BMC Health Serv. Res. 2015, 15, 252. [Google Scholar] [CrossRef] [Green Version]
- Gibson, C.H. A concept analysis of empowerment. J. Adv. Nurs. 1991, 16, 354–361. [Google Scholar] [CrossRef]
- Tsubouchi, Y.; Yorozuya, K.; Tainosyo, A.; Naito, Y. A conceptual analysis of older adults’ empowerment in contemporary japanese culture. BMC Geriatr. 2021, 21, 672. [Google Scholar] [CrossRef]
- Mora, M.A.; Sparud-Lundin, C.; Moons, P.; Bratt, E.-L. Definitions, instruments and correlates of patient empowerment: A descriptive review. Patient Educ. Couns. 2022, 105, 346–355. [Google Scholar] [CrossRef]
- Castro, E.M.; Van Regenmortel, T.; Vanhaecht, K.; Sermeus, W.; Van Hecke, A. Patient empowerment, patient participation and patient-centeredness in hospital care: A concept analysis based on a literature review. Patient Educ. Couns. 2016, 99, 1923–1939. [Google Scholar] [CrossRef]
- Stichler, J.F.; Pelletier, L.R. Psychometric Testing of a Patient Empowerment, Engagement, and Activation Survey. J. Nurs. Care Qual. 2020, 35, E49–E57. [Google Scholar] [CrossRef]
- Zimmerman, M.A. Psychological empowerment: Issues and illustrations. Am. J. Community Psychol. 1995, 23, 581–599. [Google Scholar] [CrossRef] [Green Version]
- Logsdon, R.G.; Gibbons, L.E.; McCurry, S.M.; Teri, L. Assessing Quality of Life in Older Adults with Cognitive Impairment. Psychosom. Med. 2002, 64, 510–519. [Google Scholar] [CrossRef] [PubMed]
- Cabinet Office. Summary of the FY. Revision of Medical Fees (Inpatient Care). 2020. Available online: https://www.mhlw.go.jp/content/12400000/000691039.pdf (accessed on 9 March 2021).
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Tsubouchi, Y.; Tainosho, A.; Shimomura, K.; Yorozuya, K.; Kou, M.; Tsubouchi, R.; Tanaka, H.; Naito, Y. Reliability and Validation of the Japanese Version of the Patient Empowerment Scale. Healthcare 2022, 10, 1151. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-Mental State”. A Practical Method for Grading the Cognitive State of Patients for the Clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Shigemori, K.; Ohgi, S.; Okuyama, E.; Shimura, T.; Schneider, E. The factorial structure of the mini mental state examination (MMSE) in Japanese dementia patients. BMC Geriatr. 2010, 10, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugishita, M.; Hemmi, I.; JADNI. MMSE-J (seishin jyoutai tanzikan kensa nihongoban) no datousei to shinraisei ni tsuite: A preliminary report [validity and reliability of the Mini-Mental State Examination (MMSE-J): A preliminary report]. Ninchi Shinkei Kagaku [Jpn. J. Cogn. Neurosci.] 2010, 12, 186–190. (In Japanese) [Google Scholar] [CrossRef]
- Avers, D.; Brown, M. Daniels and Worthingham’s Muscle Testing: Techniques of Manual Examination and Performance Testing, 10th ed.; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Rodriguez, C.S. Pain measurement in the elderly: A review. Pain Manag. Nurs. 2001, 2, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Tsuji, T.; Sonoda, S.; Domen, K.; Saitoh, E.; Liu, M.; Chino, N. ADL structure for stroke patients in japan based on the functional independence measure. Am. J. Phys. Med. Rehabil. 1995, 74, 432–438. [Google Scholar] [CrossRef]
- Gibbs, B.B.; Hergenroeder, A.L.; Katzmarzyk, P.T.; Lee, I.-M.; Jakicic, J.M. Definition, Measurement, and Health Risks Associated with Sedentary Behavior. Med. Sci. Sports Exerc. 2015, 47, 1295–1300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matthews, C.; Ainsworth, B.E.; Thompson, R.W.; Bassett, D.R. Sources of variance in daily physical activity levels as measured by an accelerometer. Med. Sci. Sports Exerc. 2002, 34, 1376–1381. [Google Scholar] [CrossRef] [PubMed]
- Finney, S.J.; Distefano, C. Non-normal and Categorical Data in Structural Equation Modelling. Structural Equation Modelling: A Second Course; Information Age Publishing: Charlotte, NC, USA, 2006; pp. 269–314. [Google Scholar]
- Morrison, T.G.; Morrison, M.A.; McCutcheon, J.M. Best Practice Recommendations for Using Structural Equation Modelling in Psychological Research. Psychology 2017, 08, 1326–1341. [Google Scholar] [CrossRef] [Green Version]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Equation modelling: Guidelines for determining model fit. Electron. J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar] [CrossRef]
- Yoshimura, T.; Kitayama, A. Satoyama no kurashi ni okeru sōsyarukyapitaru no tokuchou. [Characteristics of social capital in satoyama life]. Nihon Rūraru Nāshingu Gakkaishi [Jpn. J. Rural. Remote Area Nurs.] 2013, 8, 1–15. (In Japanese) [Google Scholar]
- Sakanashi, S.; Fujita, K. Empowerment of family caregivers of adults and elderly persons: A concept analysis. Int. J. Nurs. Pr. 2017, 23, e12573. [Google Scholar] [CrossRef]
- Sepúlveda-Loyola, W.; Rodríguez-Sánchez, I.; Pérez-Rodríguez, P.; Ganz, F.; Torralba, R.; Oliveira, D.V.; Rodríguez-Mañas, L. Impact of social isolation due to COVID-19 on health in older people: Mental and physical effects and recommendations. J. Nutr. Health Aging 2020, 24, 938–947. [Google Scholar] [CrossRef]
- Faulkner, M. A measure of patient empowerment in hospital environments catering for older people. J. Adv. Nurs. 2001, 34, 676–686. [Google Scholar] [CrossRef]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Whitehall, L.; Rush, R.; Górska, S.; Forsyth, K. The General Self-Efficacy of Older Adults Receiving Care: A Systematic Review and Meta-Analysis. Gerontologist 2020, 61, e302–e317. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M.; On Behalf of SBRN Terminology Consensus Project Participants. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inoue, K.; Okamoto, M.; Shibato, J.; Lee, M.C.; Matsui, T.; Rakwal, R.; Soya, H. Long-Term Mild, rather than Intense, Exercise Enhances Adult Hippocampal Neurogenesis and Greatly Changes the Transcriptomic Profile of the Hippocampus. PLoS ONE 2015, 10, e0128720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Copeland, J.L.; Ashe, M.C.; Biddle, S.J.; Brown, W.J.; Buman, M.P.; Chastin, S.; A Gardiner, P.; Inoue, S.; Jefferis, B.J.; Oka, K.; et al. Sedentary time in older adults: A critical review of measurement, associations with health, and interventions. Br. J. Sports Med. 2017, 51, 1539. [Google Scholar] [CrossRef] [Green Version]
- Inoue, M.; Iso, H.; Yamamoto, S.; Kurahashi, N.; Iwasaki, M.; Sasazuki, S.; Tsugane, S.; Japan Public Health Center-Based Prospective Study Group. Daily Total Physical Activity Level and Premature Death in Men and Women: Results from a Large-Scale Population-Based Cohort Study in Japan (JPHC Study). Ann. Epidemiology 2008, 18, 522–530. [Google Scholar] [CrossRef]
- Buchman, A.S.; Boyle, P.A.; Wilson, R.S.; Fleischman, D.A.; Leurgans, S.; Bennett, D.A. Association Between Late-Life Social Activity and Motor Decline in Older Adults. Arch. Intern. Med. 2009, 169, 1139–1146. [Google Scholar] [CrossRef]
| Item | N = 151 | Skewness | Kurtosis | |
|---|---|---|---|---|
| Age (years) | 81.75 | −7.15 | −0.35 | −0.15 |
| Years of education | 11.2 | −1.81 | 0.45 | 0.5 |
| Sex (no. of people) | ||||
| Male | 54 | 35.76% | −0.76 | −1.45 |
| Female | 97 | 64.24% | ||
| Major physical diseases resulting in hospitalization (no. of people) | ||||
| Central nervous system diseases | 33 | 21.85% | ||
| Orthopedic diseases | 79 | 52.32% | −0.05 | −0.89 |
| Disuse syndromes associated with medical diseases | 39 | 25.83% | ||
| CCI | 1.56 | −1.31 | 0.83 | 0.92 |
| MMSE | 22.09 | −5.31 | −0.4 | −0.77 |
| MMT | ||||
| Right quadriceps | 3.79 | −0.71 | −0.5 | 1.11 |
| Left quadriceps | 3.69 | −0.6 | 0.07 | −0.37 |
| NRS | 3.48 | −2.2 | 0.31 | −0.96 |
| Alb (g/dL) | 3.74 | −0.39 | −0.11 | −0.53 |
| FIM | 73.22 | −20.91 | 0.06 | −0.53 |
| Activity time per intensity (minute) | ||||
| Low intensity | 13.6 | −12.14 | 1.02 | 0.19 |
| Moderate intensity | 4.31 | −5.3 | 1.9 | 3.79 |
| High intensity | 0.59 | −0.99 | 4.08 | 23.33 |
| Family structure (no. of people) | ||||
| Lone parent | 59 | 39.07% | ||
| Married couple | 23 | 15.23% | 0.19 | −1.39 |
| Two-parent household | 52 | 34.44% | ||
| Three or more-person household | 17 | 11.26% | ||
| Primary caregiver (no. of people) | ||||
| Spouse of child | 26 | 17.22% | ||
| Daughter/Son | 96 | 63.58% | 0.95 | 0.07 |
| Sibling | 2 | 1.32% | ||
| Spouse | 27 | 17.88% | ||
| Economic status (no. of people) | ||||
| Independent | 84 | 55.63% | ||
| Family support | 58 | 38.41% | 0.79 | −0.34 |
| Public support | 9 | 5.96% | ||
| Hobbies (no. of people) | ||||
| Affected | 95 | 62.91% 37.09% | 0.54 | −1.73 |
| Unaffected | 56 | |||
| Roles (no. of people) | ||||
| Affected | 85 | 56.29% | 0.26 | −1.96 |
| Unaffected | 66 | 43.71% | ||
| Independent Variable | B | SE B | β | t Value | f 2 |
|---|---|---|---|---|---|
| Years of education | −0.13 | 0.72 | −0.01 | −0.17 | <0.01 |
| Sex | −3.25 | 2.77 | −0.10 | −1.17 | <0.01 |
| Major physical diseases resulting in hospitalization | −0.40 | 1.89 | −0.02 | −0.21 | <0.01 |
| Family structure | 2.68 | 1.16 | 0.18 * | 2.32 | <0.01 |
| Primary caregiver | −0.13 | 1.41 | −0.01 | −0.09 | <0.01 |
| Economic status | −0.79 | 2.15 | −0.03 | −0.37 | <0.01 |
| Hobbies | −3.23 | 2.69 | −0.10 | −1.20 | <0.01 |
| Roles | −13.26 | 2.39 | −0.41 ** | −5.54 | 0.20 |
| Dependent Variable | B | SE B | β | t Value | f 2 |
|---|---|---|---|---|---|
| CCI | −0.64 | 0.18 | −0.29 ** | −3.64 | 0.09 |
| MMSE | 0.07 | 0.03 | 0.22 ** | 2.75 | 0.05 |
| MMT | |||||
| Right quadriceps | <0.01 | <0.01 | 0.04 | 0.49 | <0.01 |
| Left quadriceps | <0.01 | <0.01 | 0.11 | 1.30 | <0.01 |
| NRS | −0.02 | 0.01 | −0.17 * | −2.04 | 0.03 |
| Alb | 0.01 | <0.01 | 0.30 ** | 3.89 | 0.10 |
| FIM | 0.41 | 0.10 | 0.32 ** | 4.06 | 0.11 |
| Activity time per intensity | |||||
| Low intensity | 0.34 | 0.06 | 0.45 ** | 6.19 | 0.27 |
| Moderate intensity | 0.13 | 0.03 | 0.38 ** | 5.00 | 0.16 |
| PES-J | CCI | MMSE | NRS | Alb | FIM | Low-Intensity Activity Time | Moderate-Intensity Activity Time | |
|---|---|---|---|---|---|---|---|---|
| PES-J | 1 | |||||||
| CCI | −0.25 ** | 1 | ||||||
| MMSE | 0.20 * | −0.20 ** | 1 | |||||
| NRS | −0.16 * | 0.11 | −0.19 * | 1 | ||||
| Alb | 0.32 ** | −0.23 ** | 0.31 ** | −0.25 ** | 1 | |||
| FIM | 0.34 ** | −0.38 ** | 0.53 ** | −0.36 ** | 0.54 ** | 1 | ||
| Low-intensity activity time | 0.45 ** | −0.27 ** | 0.40 ** | −0.27 ** | 0.34 ** | 0.63 ** | 1 | |
| Moderate-intensity activity time | 0.35 ** | −0.26 ** | 0.44 ** | −0.30 ** | 0.30 ** | 0.64 ** | 0.85 ** | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsubouchi, Y.; Tainosho, A.; Shimomura, K.; Kou, M.; Yorozuya, K.; Nakashima, D.; Naito, Y. Relationship between Empowerment and Functioning and Disability in Older Japanese Patients: A Covariance Structure Analysis. Healthcare 2023, 11, 44. https://doi.org/10.3390/healthcare11010044
Tsubouchi Y, Tainosho A, Shimomura K, Kou M, Yorozuya K, Nakashima D, Naito Y. Relationship between Empowerment and Functioning and Disability in Older Japanese Patients: A Covariance Structure Analysis. Healthcare. 2023; 11(1):44. https://doi.org/10.3390/healthcare11010044
Chicago/Turabian StyleTsubouchi, Yoshihito, Akiyoshi Tainosho, Koudai Shimomura, Motoasa Kou, Kyosuke Yorozuya, Daiki Nakashima, and Yasuo Naito. 2023. "Relationship between Empowerment and Functioning and Disability in Older Japanese Patients: A Covariance Structure Analysis" Healthcare 11, no. 1: 44. https://doi.org/10.3390/healthcare11010044





