Testing Surgical Face Masks in an Emergency Context: The Experience of Italian Laboratories during the COVID-19 Pandemic Crisis
Abstract
1. Introduction
1.1. The Covid-19 Outbreak in Italy and the Emergency Context
1.2. The Market Dynamics of Surgical Face Masks and the Request to Set Up Testing Laboratories at Italian Universities
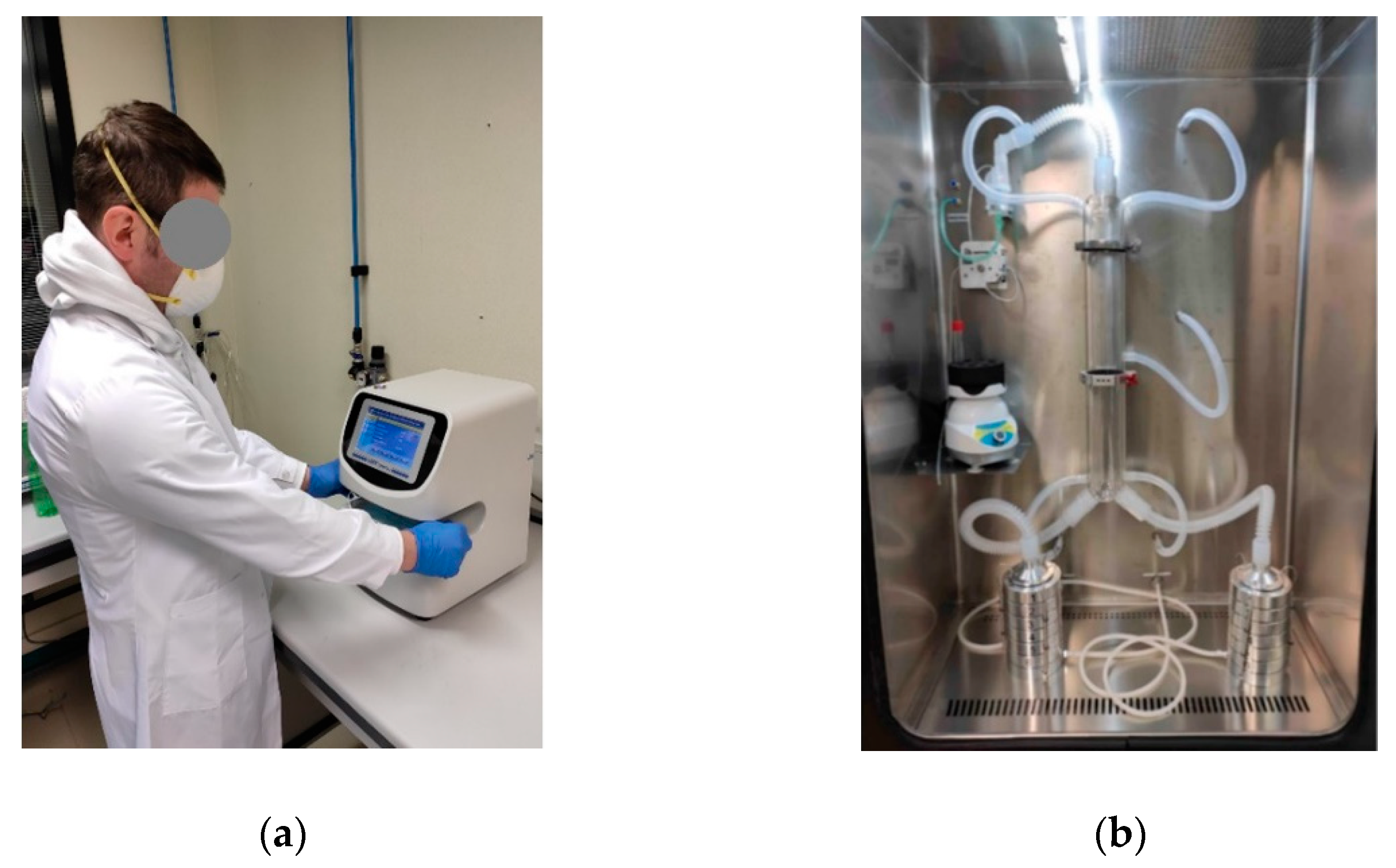
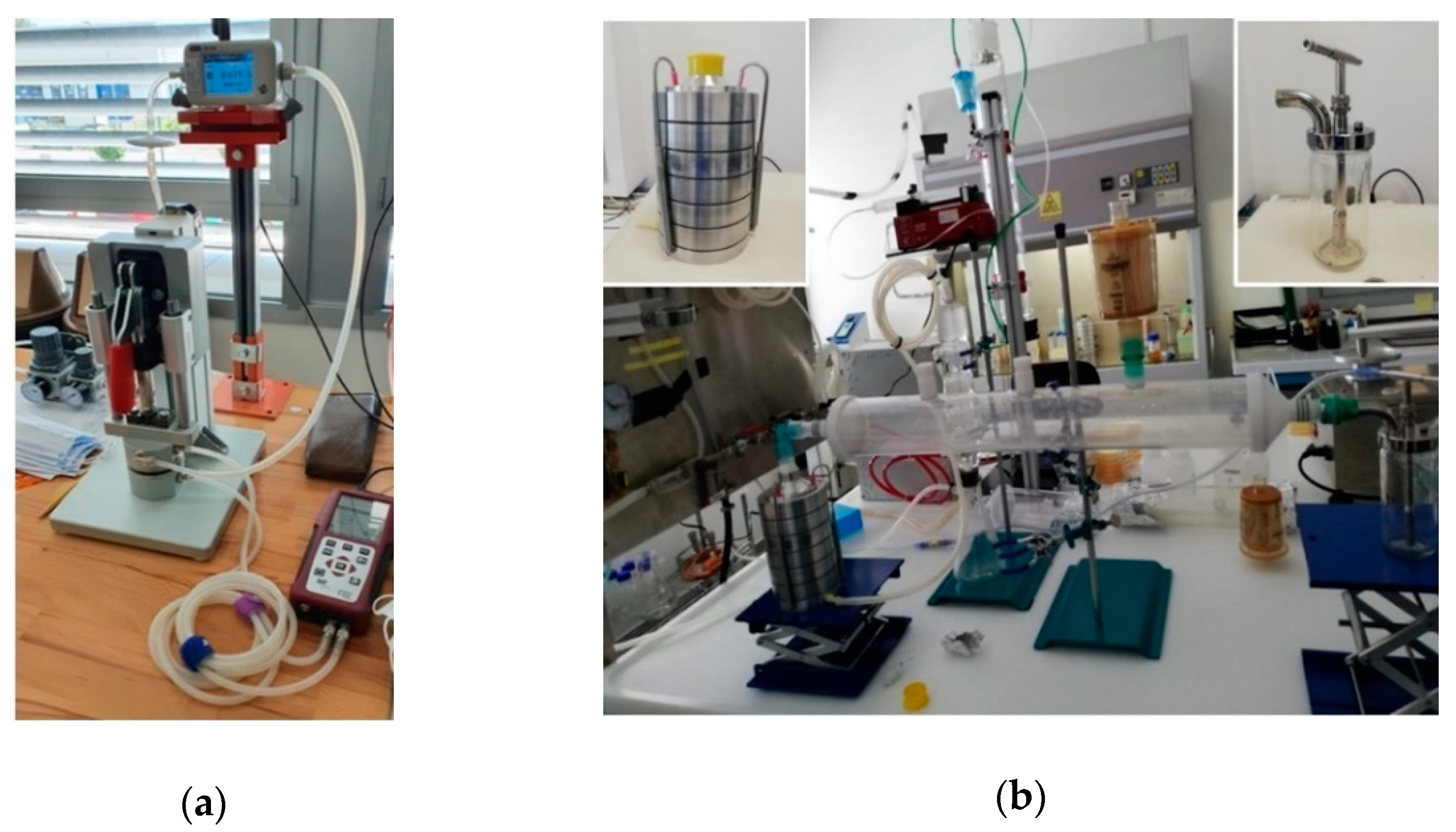
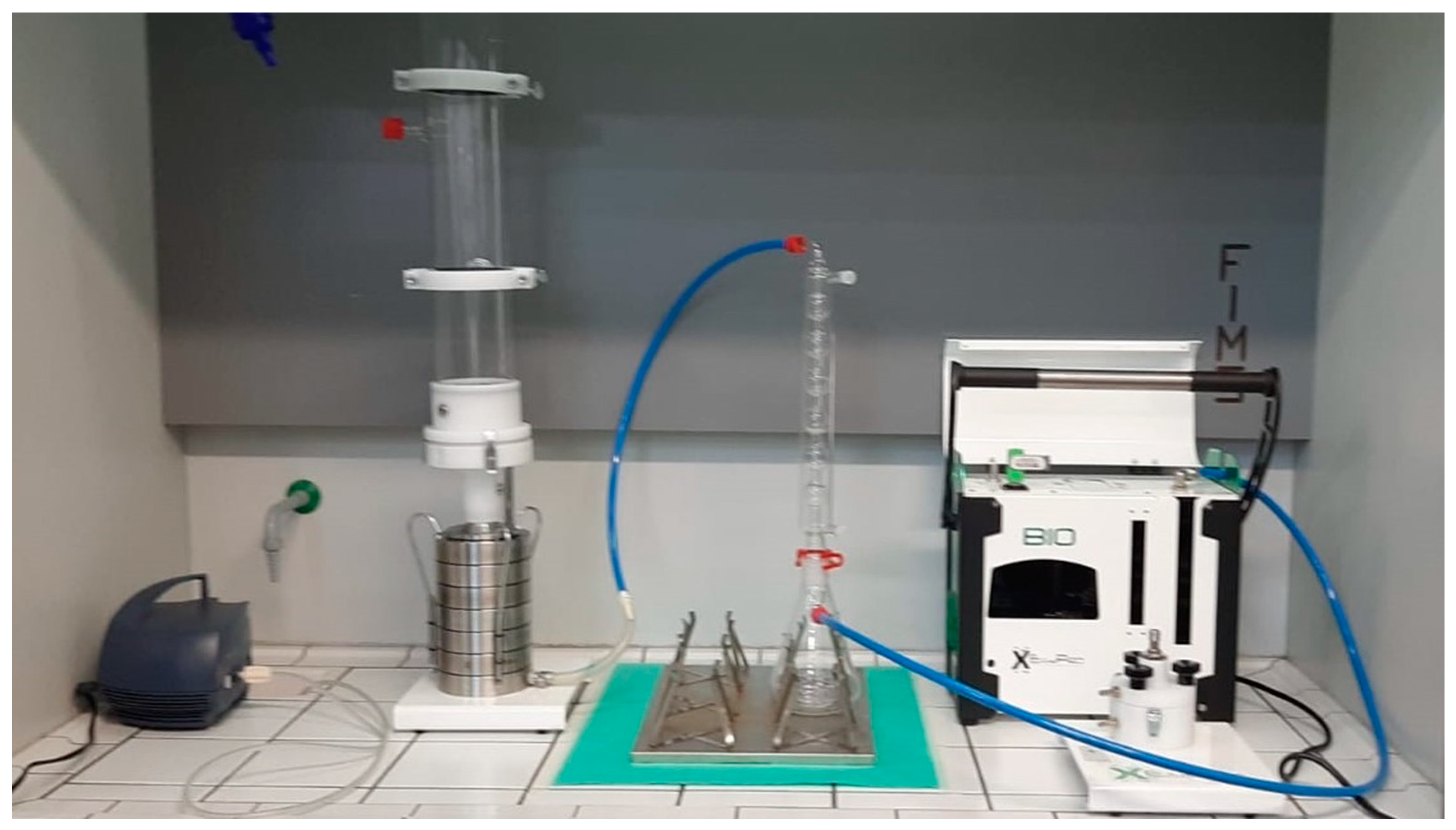
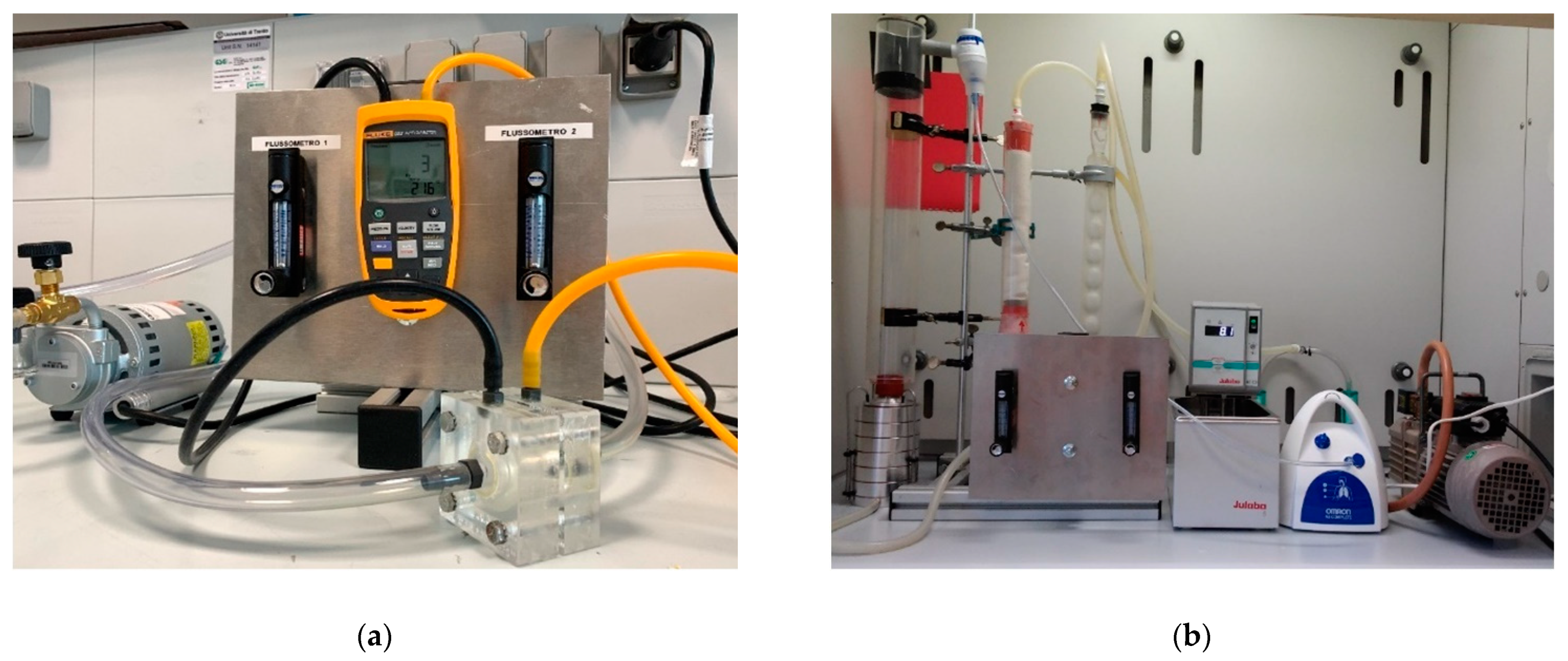
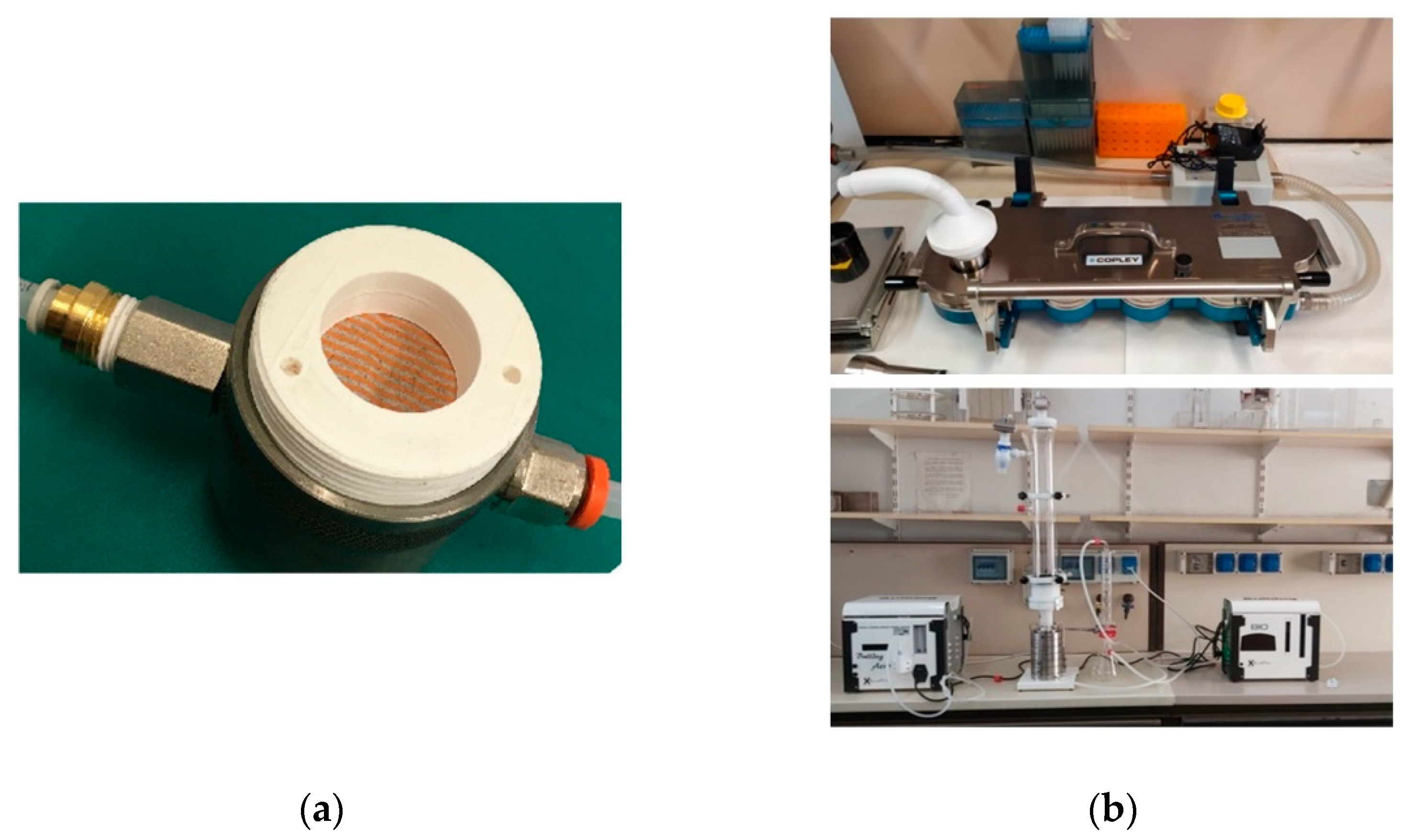
2. Materials and Methods
2.1. The Standard EN 14683:2019+AC
- the aerosol should be mixed with air in a cylinder with an 80 mm diameter and 600 mm length;
- the air flow in the system should be generated and kept constant by a vacuum pump at a rate of 28.3 L/min;
- the aerosol should be obtained from a bacterial suspension grown in tryptic soy broth and then diluted in peptone water up to a concentration of 5 × 105 CFU/mL (CFU stands for Colony Forming Units);
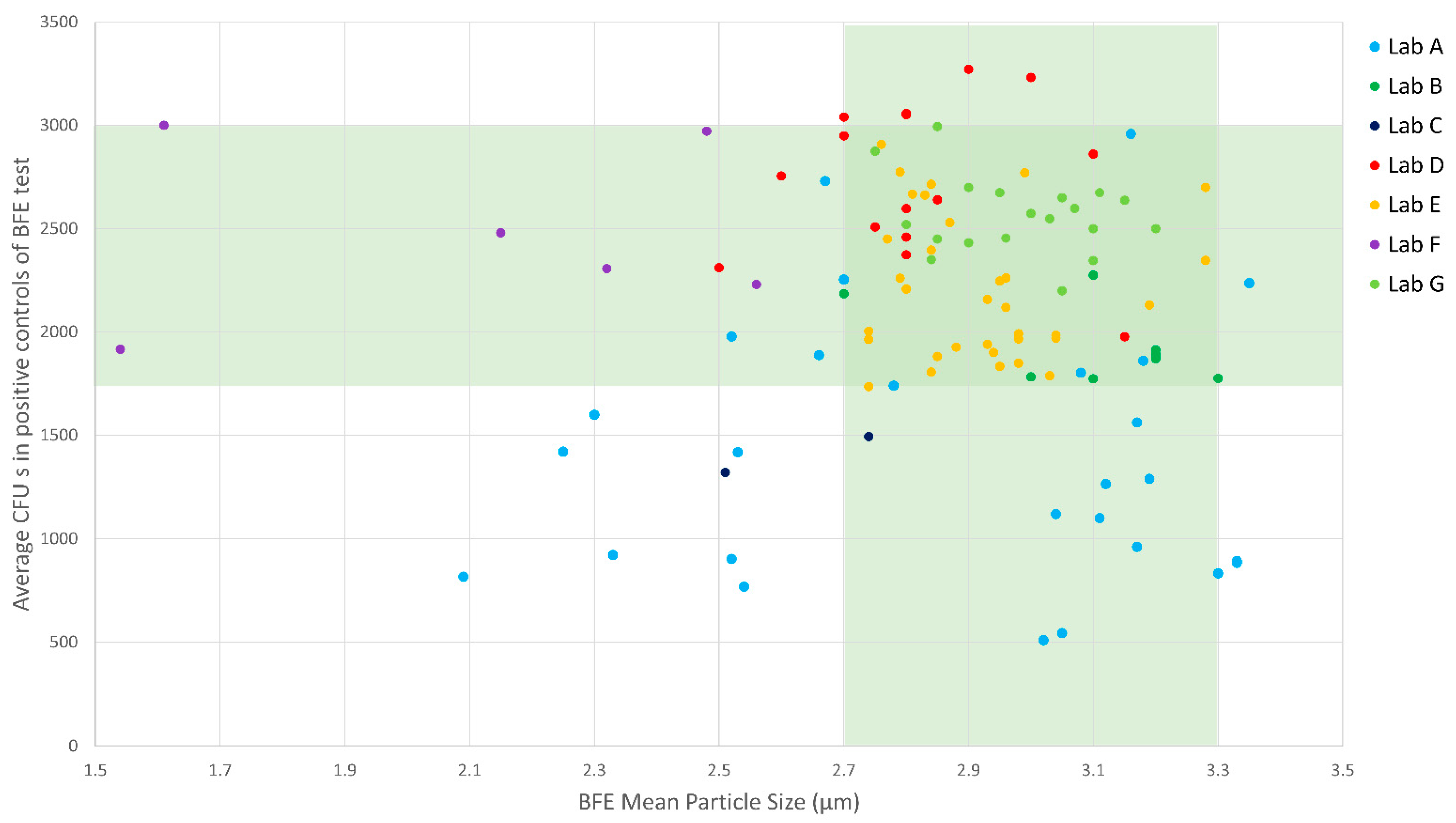
- the Mean Particle Size (MPS) of the aerosol should be in the range from 2.7 µm to 3.3 µm;
- the average number of CFUs in the two positive controls (tests without mask) should be between 1700 and 3000.
2.2. The Set-Up of Laboratory Facilities at the Universities in the Emergency Period
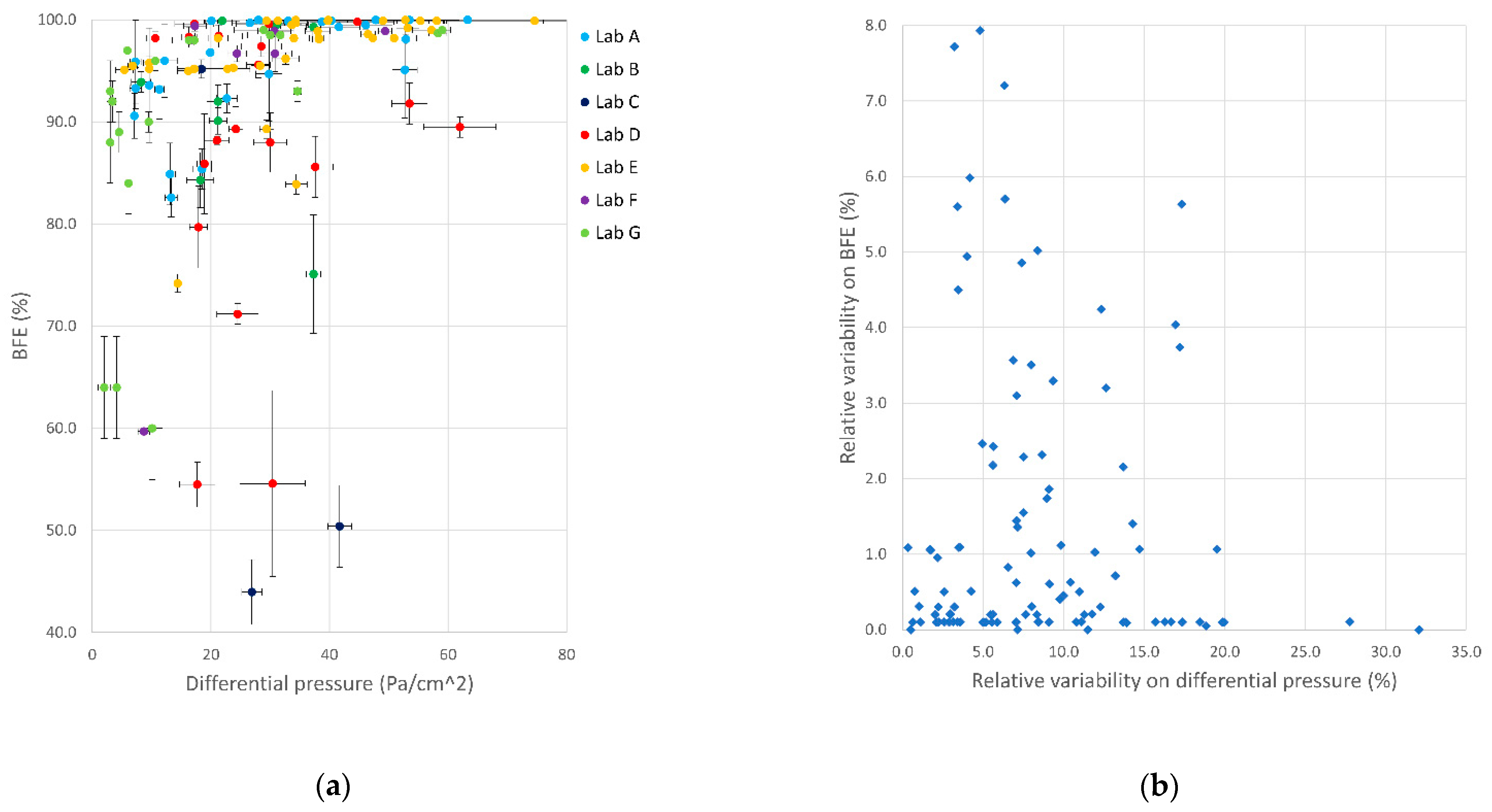
3. Results and Discussion
3.1. Laboratories’ Activity Report
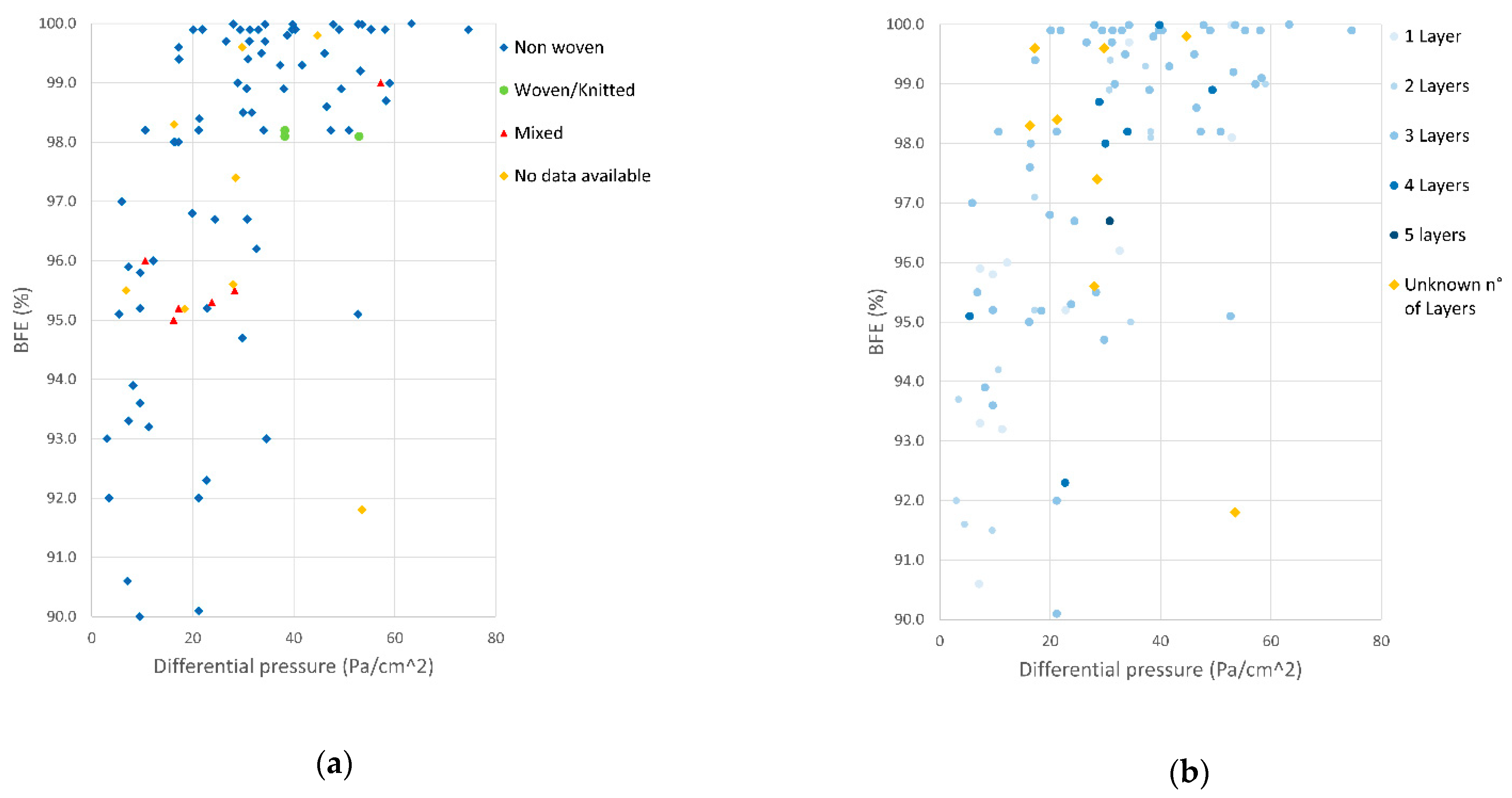
3.2. Mask Performances
3.3. Laboratories’ Adherence to Standards Specifications
3.4. The Organizational Strategies: An Example of University Third Mission in an Emergency
- two step procedure (UNICAM, UNIVPM, UNIMORE, UNITN, UNICA), performing tests in sequence, starting from DP test, and proceeding to BFE with a 6-stage Andersen impactor only if DP requirements were satisfied;
- three step procedure with simplified BFE (UNICT), performing tests in sequence, starting from DP test, and proceeding to a simplified BFE (impactor with reduced number of stages or full number of stages, but no sample replicates) only if DP requirements were satisfied, then proceeding to a complete BFE analysis with the 6-stage Andersen impactor only in case the simplified BFE provides a positive result;
- four step procedure with cross-check testing (UNINA), performing tests in go/no go stages. Stage 1: measure of DP and particle filtration; Stage 2: Aerosol filtration efficiency; Stage 3: Complete BFE, Stage 4: other testing for conformity to EN 14683:2019+AC (e.g., microbial load, splash resistance) and EN 10993-1:2010 (biocompatibility tests).
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Advice on the Use of Masks in the Community, during Home Care and in Healthcare Settings in the Context of the Novel Coronavirus (COVID-19) Outbreak. Available online: https://www.who.int/publications-detail-redirect/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak (accessed on 9 November 2020).
- CEN Workshop Agreement CWA 17553:2020 E, “Community Face Coverings—Guide to Minimum Requirements, Methods of Testing and Use”; European Committee for Standardisation: Bruxelles, Belgium, 2020.
- European Center for Disease Prevention and Control. Using Face Masks in the Community, ECDC-European Center for Disease Prevention and Control, Technical Report. Available online: https://www.ecdc.europa.eu/en/publications-data/using-face-masks-community-reducing-covid-19-transmission (accessed on 3 February 2021).
- Gazzetta Ufficiale dell Repubblica Italiana. Decreto Legge n.9 Del 2 Marzo 2020 (Art. 34, Comma 3); Istituto Poligrafico e Zecca dello Stato S.p.A.: Roma, Italy, 2020. [Google Scholar]
- Gazzetta Ufficiale dell Repubblica Italiana. Decreto Legge Del 17 Marzo 2020 n.18 (Art. 15); Istituto Poligrafico e Zecca dello Stato S.p.A.: Roma, Italy, 2020. [Google Scholar]
- World Health Organization. Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19) and Considerations during Severe Shortages—Interim Guidance 2020. Available online: https://www.who.int/publications/i/item/rational-use-of-personal-protective-equipment-for-coronavirus-disease-(covid-19)-and-considerations-during-severe-shortages (accessed on 3 February 2021).
- The Organisation for Economic Co-operation and Development. The Face Mask Global Value Chain in the COVID-19 Outbreak: Evidence and Policy Lessons. Available online: http://www.oecd.org/coronavirus/policy-responses/the-face-mask-global-value-chain-in-the-covid-19-outbreak-evidence-and-policy-lessons-a4df866d/ (accessed on 9 November 2020).
- Yu, J.; Lu, Y.; Muñoz-Justicia, J. Analyzing Spanish News Frames on Twitter during COVID-19—A Network Study of El País and El Mundo. Int. J. Environ. Res. Public Health 2020, 17, 5414. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, W.; Vidal-Alaball, J.; Lopez Segui, F.; Moreno-Sánchez, P.A. A Social Network Analysis of Tweets Related to Masks during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 8235. [Google Scholar] [CrossRef] [PubMed]
- Istituto Superiore di Sanità. Procedure per Richiesta Produzione Mascherine—ISS. Available online: https://www.iss.it/procedure-per-richiesta-produzione-mascherine (accessed on 9 November 2020).
- European Committee for Standardization. EN 14683:2019+AC Medical Face Masks—Requirements and Test Methods 2019; European Standard: Bruxelles, Belgium, 2019. [Google Scholar]
- International Standard Organization. ISO 10993-1:2018 Biological Evaluation of Medical Devices—Part 1: Evaluation and Testing within a Risk Management Process 2018; International Organization for Standardization: Geneva, Switzerland, 2018. [Google Scholar]
- Marple, V.A. History of Impactors—The First 110 Years. Aerosol Sci. Technol. 2004, 38, 247–292. [Google Scholar] [CrossRef]
- Andersen, A.A. New Sampler for the Collection, Sizing, and Enumeration of Viable Airborn Particles. J. Bacteriol. 1958, 76, 471–484. [Google Scholar] [CrossRef] [PubMed]
- Macii, D.; Petri, D. Guidelines to Manage Measurement Uncertainty in Conformance Testing Procedures. IEEE Trans. Instrum. Meas. 2009, 58, 33–40. [Google Scholar] [CrossRef]
- del Wacher-Rodarte, M.C.; Trejo-Muñúzuri, T.P.; Montiel-Aguirre, J.F.; Drago-Serrano, M.E.; Gutiérrez-Lucas, R.L.; Castañeda-Sánchez, J.I.; Sainz-Espuñes, T. Antibiotic Resistance and Multidrug-Resistant Efflux Pumps Expression in Lactic Acid Bacteria Isolated from Pozol, a Nonalcoholic Mayan Maize Fermented Beverage. Food Sci. Nutr. 2016, 4, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Treangen, T.J.; Maybank, R.A.; Enke, S.; Friss, M.B.; Diviak, L.F.; Karaolis, D.K.R.; Koren, S.; Ondov, B.; Phillippy, A.M.; Bergman, N.H.; et al. Complete Genome Sequence of the Quality Control Strain Staphylococcus Aureus Subsp. Aureus ATCC 25923. Genome Announc. 2014, 2, e01110-14. [Google Scholar] [CrossRef] [PubMed]
- European Committee for Standardization. EN 149:2009+A1 Respiratory Protective Devices—Filtering Half Masks to Protect against Particles—Requirements, Testing, Marking 2009; European Standard: Bruxelles, Belgium, 2009. [Google Scholar]
- D’Anna, A.; Di Natale, F.; De Falco, G.; Di Maio, E.; Tammaro, D.; Quaglia, F.; Ungaro, F.; Cassiano, C.; Salvatore, P.; Colicchio, R.; et al. Validazione di maschere chirurgiche nella fase di emergenza COVID19: L’esperienza dell’Università degli Studi di Napoli Federico II. G. Ital. Med. Lav. Ergon 2020, 42, 73–81. [Google Scholar] [PubMed]
- Arcuri, D.D. Ordinanza n. 11 /2020; Presidenza del Consiglio dei Ministri: Roma, Italy, 2020. [Google Scholar]
- Aydin, O.; Emon, B.; Cheng, S.; Hong, L.; Chamorro, L.P.; Saif, M.T.A. Performance of Fabrics for Home-Made Masks against the Spread of COVID-19 through Droplets: A Quantitative Mechanistic Study. Extreme Mech. Lett. 2020, 40, 100924. [Google Scholar] [CrossRef] [PubMed]
- Shakya, K.M.; Noyes, A.; Kallin, R.; Peltier, R.E. Evaluating the Efficacy of Cloth Facemasks in Reducing Particulate Matter Exposure. J. Expo. Sci. Environ. Epidemiol. 2017, 27, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-P.; Yip, J.; Kan, C.-W.; Chiou, J.-C.; Yung, K.-F. Reusable Face Masks as Alternative for Disposable Medical Masks: Factors That Affect Their Wear-Comfort. Int. J. Environ. Res. Public Health 2020, 17, 6623. [Google Scholar] [CrossRef] [PubMed]
- Shaw, K.; Butcher, S.; Ko, J.; Zello, G.A.; Chilibeck, P.D. Wearing of Cloth or Disposable Surgical Face Masks Has No Effect on Vigorous Exercise Performance in Healthy Individuals. Int. J. Environ. Res. Public Health 2020, 17, 8110. [Google Scholar] [CrossRef] [PubMed]
- Machida, M.; Nakamura, I.; Saito, R.; Nakaya, T.; Hanibuchi, T.; Takamiya, T.; Odagiri, Y.; Fukushima, N.; Kikuchi, H.; Amagasa, S.; et al. Incorrect Use of Face Masks during the Current COVID-19 Pandemic among the General Public in Japan. Int. J. Environ. Res. Public Health 2020, 17, 6484. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Saiki, D.; Kandiah, J. Masks, Gloves, and the COVID-19 Pandemic: Rapid Assessment of Public Behaviors in the United States. Epidemiologia 2020, 1, 4. [Google Scholar] [CrossRef]
- Compagnucci, L.; Spigarelli, F. The Third Mission of the University: A Systematic Literature Review on Potentials and Constraints. Technol. Forecast. Soc. Chang. 2020, 161, 120284. [Google Scholar] [CrossRef]
- Berghaeuser, H.; Hoelscher, M. Reinventing the Third Mission of Higher Education in Germany: Political Frameworks and Universities’ Reactions. Tert. Educ. Manag. 2020, 26, 57–76. [Google Scholar] [CrossRef]
- Lass-Tn-Covid-19, Progetto Mascherine, Dipartimento Di Ingegneria Industriale, Università Di Trento. Available online: https://www.dii.unitn.it/1208/progetto-mascherine (accessed on 22 January 2021).
- LABC19—Centro di ricerca e servizio per l’emergenza Covid-19—Università Politecnica delle Marche. Available online: https://labc19.univpm.org/ (accessed on 22 January 2021).
- Tecnopolo Mario Veronesi Mirandola. Available online: https://tpm.bio/ (accessed on 22 January 2021).
- Safe S.r.l, Analisi Chimico Biologich. Available online: https://www.laboratoriosafe.it/ (accessed on 22 January 2021).
- Anti_Covid-Lab, Laboratorio per Il Test Di Tessuti per Dpi, Università Degli Studi Di Catania. Available online: http://www.brit.unict.it/ (accessed on 22 January 2021).
- Laboratorio Emergenza Covid-19—Laboratorio DPI, Center of Advanced Metrology and Technology Services, Università di Napoli Federico II. Available online: http://www.cesma.unina.it/laboratori/presidio-tecnico-scientifico-per-l-emergenza-covid-19/presidio-tecnico-scientifico-per-l-emergenza-covid-19-laboratori-aree-di-intervento/laboratorio-emergenza-covid-19-laboratorio-dpi (accessed on 22 January 2021).
- Laboratorio Di Certificazione Delle Mascherine, Area Ricerca, Trasferimento Tecnologico e Gestione Progetti Università Di Camerino. Available online: https://aripro.unicam.it/content/laboratorio-di-certificazione-delle-mascherine (accessed on 22 January 2021).



| Mask Type | Bacterial Filtration Efficiency (BFE) % | Differential Pressure (DP) Pa/cm2 |
|---|---|---|
| I | ≥95 | <40 |
| II | ≥98 | <40 |
| II R | ≥98 | <60 |
| Mask Material 1 | Mask Design | |||||
|---|---|---|---|---|---|---|
| 1 Layer | 2 Layers | 3 Layers | 4 Layers | 5 Layers | No. of Layers N.A. 2 | |
| Polypropylene | 11 | 15 | 42 | 7 | 2 | 2 |
| Polyamide | 2 | - | - | - | - | - |
| Polyester | - | - | 1 | - | - | - |
| Cellulose | - | 1 | - | - | - | - |
| Polypropylene/Polyester | - | - | 6 | - | - | - |
| Polypropylene/Polyurethane | - | - | 1 | - | - | - |
| Polypropylene/Polyamide | - | - | 1 | - | - | - |
| Polypropylene/Polyethylene | - | - | 1 | - | - | - |
| Polypropylene/Cotton | 1 | - | 3 | - | - | - |
| Polypropylene/Polyamide/Cotton | - | - | 1 | - | - | - |
| Polypropylene/Polyester/Cotton | - | - | 1 | - | - | - |
| Polyamide/polyurethane | 1 | - | - | - | - | - |
| Polyamide/Polypropylene/Cotton | - | - | 2 | - | - | - |
| Polyester/Polyurethane | - | 1 | - | - | - | - |
| Polyester/Cotton | - | 1 | 1 | - | - | - |
| Polyester/Cellulose | 1 | - | - | - | - | - |
| Polyurethane/Cotton | - | 2 | - | - | - | - |
| Material N.A. 2 | - | 1 | 1 | - | - | 11 |
| Fiber Structure 1 | Number of Masks |
|---|---|
| Nonwoven | 89 |
| Woven/Knitted | 7 |
| Mix of woven/fabric and nonwoven layers | 11 |
| Structure information N.A. 2 | 13 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tessarolo, F.; Nollo, G.; Maniglio, D.; Rigoni, M.; Benedetti, L.; Helfer, F.; Corradi, I.; Rovati, L.; Ferrari, A.; Piccini, M.; et al. Testing Surgical Face Masks in an Emergency Context: The Experience of Italian Laboratories during the COVID-19 Pandemic Crisis. Int. J. Environ. Res. Public Health 2021, 18, 1462. https://doi.org/10.3390/ijerph18041462
Tessarolo F, Nollo G, Maniglio D, Rigoni M, Benedetti L, Helfer F, Corradi I, Rovati L, Ferrari A, Piccini M, et al. Testing Surgical Face Masks in an Emergency Context: The Experience of Italian Laboratories during the COVID-19 Pandemic Crisis. International Journal of Environmental Research and Public Health. 2021; 18(4):1462. https://doi.org/10.3390/ijerph18041462
Chicago/Turabian StyleTessarolo, Francesco, Giandomenico Nollo, Devid Maniglio, Marta Rigoni, Luca Benedetti, Fabrizia Helfer, Ivan Corradi, Luigi Rovati, Alberto Ferrari, Mattia Piccini, and et al. 2021. "Testing Surgical Face Masks in an Emergency Context: The Experience of Italian Laboratories during the COVID-19 Pandemic Crisis" International Journal of Environmental Research and Public Health 18, no. 4: 1462. https://doi.org/10.3390/ijerph18041462
APA StyleTessarolo, F., Nollo, G., Maniglio, D., Rigoni, M., Benedetti, L., Helfer, F., Corradi, I., Rovati, L., Ferrari, A., Piccini, M., Accorsi, L., Veronesi, E., Cuoghi, A., Baglio, S., Tuccitto, N., Stefani, S., Stracquadanio, S., Caraci, F., Terrasi, A., ... Paone, N. (2021). Testing Surgical Face Masks in an Emergency Context: The Experience of Italian Laboratories during the COVID-19 Pandemic Crisis. International Journal of Environmental Research and Public Health, 18(4), 1462. https://doi.org/10.3390/ijerph18041462















