The Association between Nonalcoholic Fatty Liver Disease and Stroke: Results from the Korean Genome and Epidemiology Study (KoGES)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Data Collection
2.3. Measurement of Fatty Liver Index (FLI) and Definition of NAFLD
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
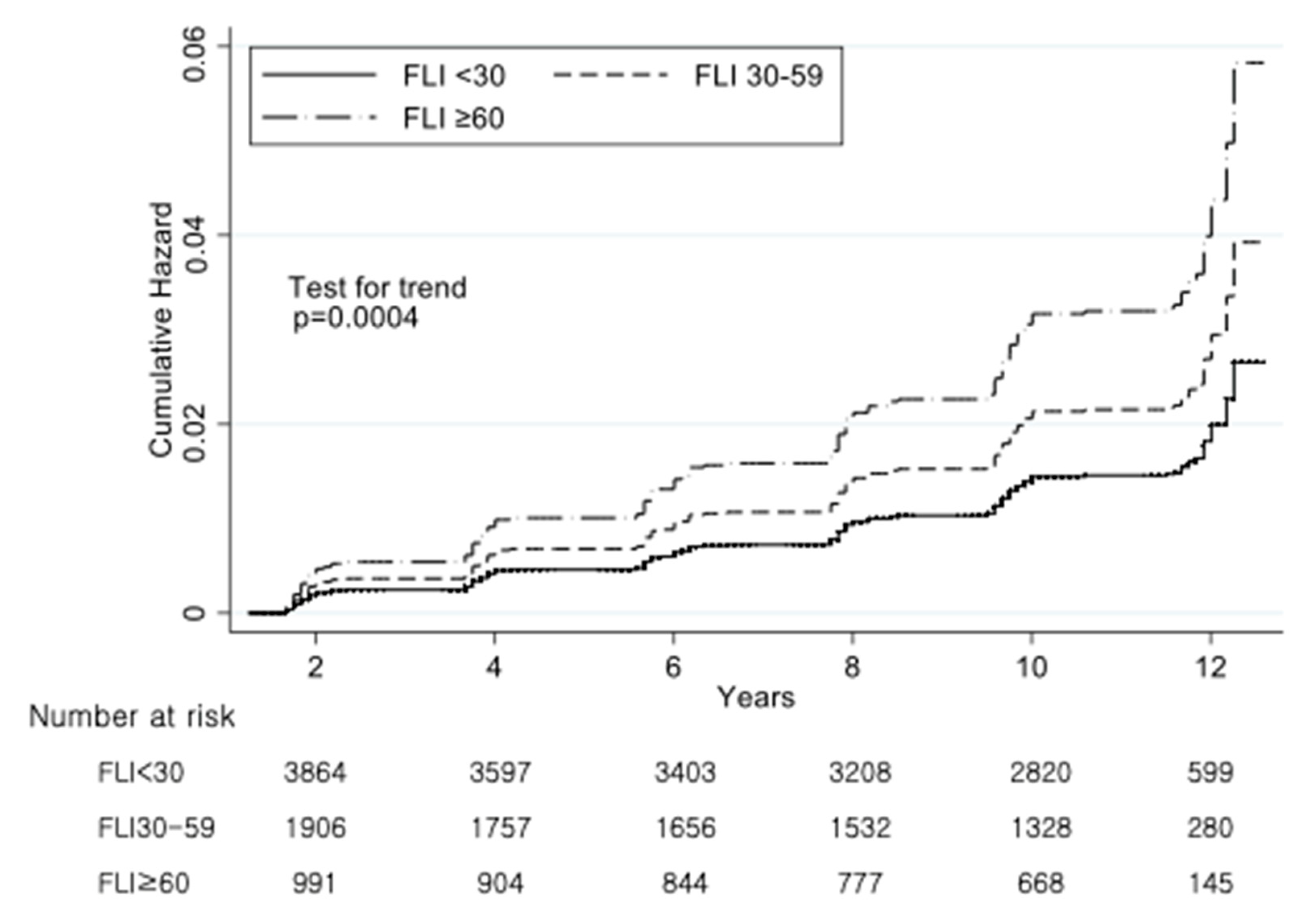
3.2. Incidence and Hazard Ratios of Stroke According to the FLI Group
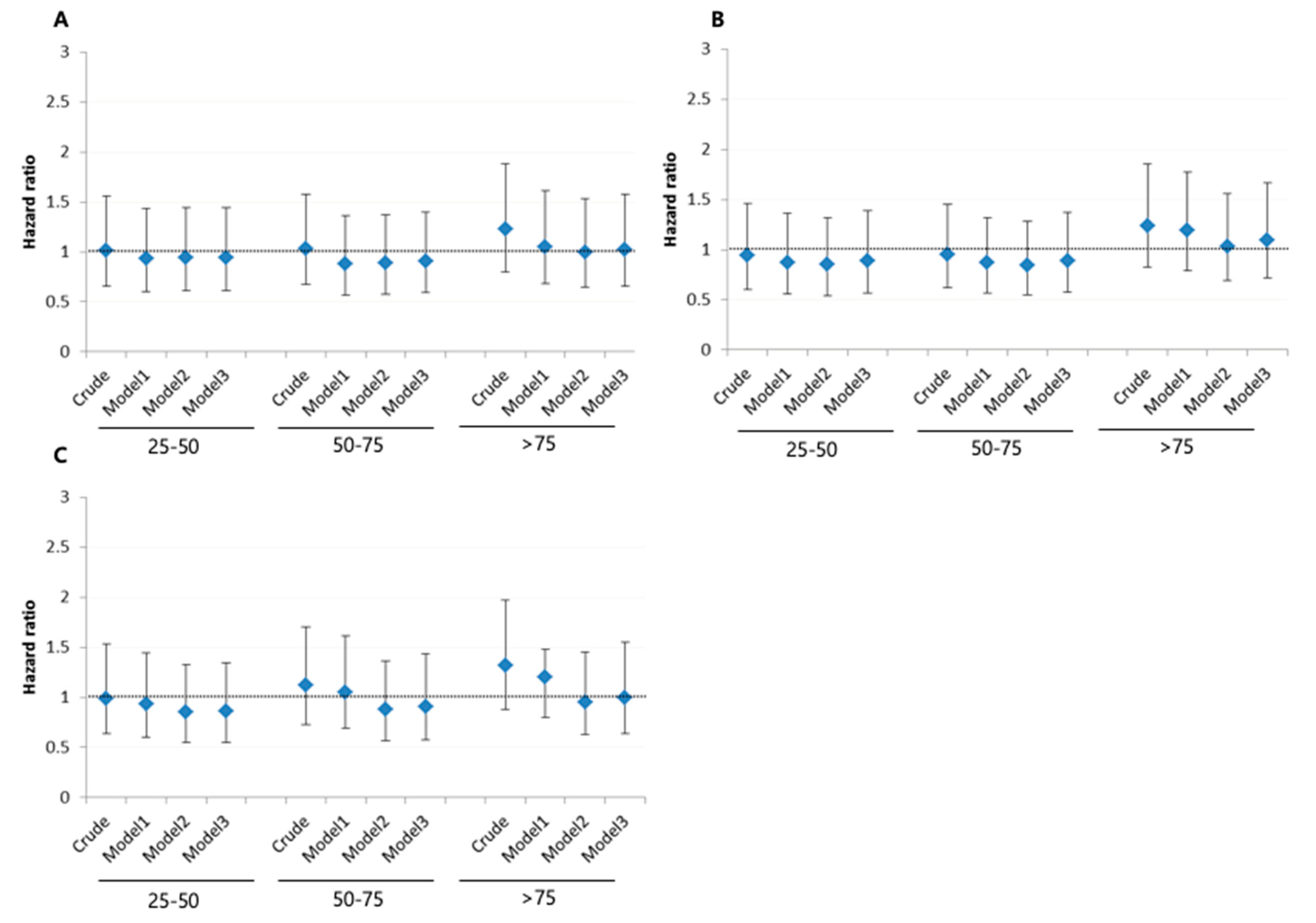
3.3. Incidence and Hazard Ratios of Stroke According to AST, ALT, and GGT
4. Discussions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; de Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef] [PubMed]
- Feigin, V.L.; Roth, G.A.; Naghavi, M.; Parmar, P.; Krishnamurthi, R.; Chugh, S.; Mensah, G.A.; Norrving, B.; Shiue, I.; Ng, M.; et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016, 15, 913–924. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Venketasubramanian, N.; Yoon, B.W.; Pandian, J.; Navarro, J.C. Stroke Epidemiology in South, East, and South-East Asia: A Review. J. Stroke 2017, 19, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.Y.; Jung, K.H.; Mo, H.; Lee, C.H.; Kim, T.J.; Park, J.M.; Oh, M.; Lee, J.S.; Kim, B.J.; Kim, J.T.; et al. Characteristics and management of stroke in Korea: 2014-2018 data from Korean Stroke Registry. Int. J. Stroke 2019. [Google Scholar] [CrossRef]
- Hong, K.S.; Bang, O.Y.; Kang, D.W.; Yu, K.H.; Bae, H.J.; Lee, J.S.; Heo, J.H.; Kwon, S.U.; Oh, C.W.; Lee, B.C.; et al. Stroke statistics in Korea: Part I. Epidemiology and risk factors: A report from the korean stroke society and clinical research center for stroke. J. Stroke 2013, 15, 2–20. [Google Scholar] [CrossRef]
- Hopewell, J.C.; Clarke, R. Emerging Risk Factors for Stroke: What Have We Learned From Mendelian Randomization Studies? Stroke 2016, 47, 1673–1678. [Google Scholar] [CrossRef] [Green Version]
- An, S.J.; Kim, T.J.; Yoon, B.W. Epidemiology, Risk Factors, and Clinical Features of Intracerebral Hemorrhage: An Update. J. Stroke 2017, 19, 3–10. [Google Scholar] [CrossRef] [Green Version]
- Arboix, A. Cardiovascular risk factors for acute stroke: Risk profiles in the different subtypes of ischemic stroke. World J. Clin. Cases 2015, 3, 418–429. [Google Scholar] [CrossRef]
- Alkagiet, S.; Papagiannis, A.; Tziomalos, K. Associations between nonalcoholic fatty liver disease and ischemic stroke. World J. Hepatol. 2018, 10, 474–478. [Google Scholar] [CrossRef]
- Bouziana, S.D.; Tziomalos, K. Inhibition of apoptosis in the management of nonalcoholic fatty liver disease. World J. Gastrointest. Pharmacol. Ther. 2013, 4, 4–8. [Google Scholar] [CrossRef]
- Papagianni, M.; Tziomalos, K. Non-alcoholic fatty liver disease: An emerging predictor of stroke risk, severity and outcome. Eur. J. Neurol. 2018, 25, 610–611. [Google Scholar] [CrossRef] [PubMed]
- Abdeldyem, S.M.; Goda, T.; Khodeir, S.A.; Abou Saif, S.; Abd-Elsalam, S. Nonalcoholic fatty liver disease in patients with acute ischemic stroke is associated with more severe stroke and worse outcome. J. Clin. Lipidol. 2017, 11, 915–919. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Xu, Y.; He, Z.; Zhang, H.; Lian, X.; Zhu, T.; Liang, C.; Li, J. Increased risk of cerebrovascular accident related to non-alcoholic fatty liver disease: A meta-analysis. Oncotarget 2018, 9, 2752–2760. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parikh, N.S.; VanWagner, L.B.; Elkind, M.S.V.; Gutierrez, J. Association between nonalcoholic fatty liver disease with advanced fibrosis and stroke. J. Neurol. Sci. 2019, 407, 116524. [Google Scholar] [CrossRef] [PubMed]
- Tu, S.; Zhao, R.; Fang, H.; Wang, L.; Shao, A.; Sheng, J. Association between Non-Alcoholic Fatty Liver Disease and Intracerebral Hemorrhage. Cell Transplant. 2019, 28, 1033–1038. [Google Scholar] [CrossRef] [PubMed]
- Baik, M.; Kim, S.U.; Nam, H.S.; Heo, J.H.; Kim, Y.D. The Paradoxical Protective Effect of Liver Steatosis on Severity and Functional Outcome of Ischemic Stroke. Front. Neurol. 2019, 10, 375. [Google Scholar] [CrossRef]
- An, S.J.; Jung, M.H.; Ihm, S.H.; Yang, Y.J.; Youn, H.J. Effect of physical activity on the cardiometabolic profiles of non-obese and obese subjects: Results from the Korea National Health and Nutritional Examination Survey. PLoS ONE 2019, 14, e0208189. [Google Scholar] [CrossRef] [Green Version]
- Alexander, K.S.; Zakai, N.A.; Lidofsky, S.D.; Callas, P.W.; Judd, S.E.; Tracy, R.P.; Cushman, M. Non-alcoholic fatty liver disease, liver biomarkers and stroke risk: The Reasons for Geographic and Racial Differences in Stroke cohort. PLoS ONE 2018, 13, e0194153. [Google Scholar] [CrossRef]
- Kim, Y.; Han, B.G.; KoGES group. Cohort Profile: The Korean Genome and Epidemiology Study (KoGES) Consortium. Int. J. Epidemiol. 2017, 46, e20. [Google Scholar] [CrossRef]
- Bedogni, G.; Bellentani, S.; Miglioli, L.; Masutti, F.; Passalacqua, M.; Castiglione, A.; Tiribelli, C. The Fatty Liver Index: A simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006, 6, 33. [Google Scholar] [CrossRef] [Green Version]
- Kwak, M.S.; Kim, K.W.; Seo, H.; Chung, G.E.; Yim, J.Y.; Kim, D. Non-obese fatty liver disease is associated with lacunar infarct. Liver Int. 2018, 38, 1292–1299. [Google Scholar] [CrossRef] [PubMed]
- Wannamethee, S.G.; Lennon, L.; Shaper, A.G. The value of gamma-glutamyltransferase in cardiovascular risk prediction in men without diagnosed cardiovascular disease or diabetes. Atherosclerosis 2008, 201, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Kunutsor, S.K.; Bakker, S.J.L.; Blokzijl, H.; Dullaart, R.P.F. Associations of the fatty liver and hepatic steatosis indices with risk of cardiovascular disease: Interrelationship with age. Clin. Chim. Acta 2017, 466, 54–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, H.; Hu, B.; Wei, L.; Zhou, L.; Zhang, L.; Lin, Y.; Qin, B.; Dai, Y.; Lu, Z. Non-alcoholic fatty liver disease is associated with stroke severity and progression of brainstem infarctions. Eur. J. Neurol. 2018, 25, 577-e34. [Google Scholar] [CrossRef]
- Ying, I.; Saposnik, G.; Vermeulen, M.J.; Leung, A.; Ray, J.G. Nonalcoholic fatty liver disease and acute ischemic stroke. Epidemiology 2011, 22, 129–130. [Google Scholar] [CrossRef]
- Bots, M.L.; Salonen, J.T.; Elwood, P.C.; Nikitin, Y.; Freire de Concalves, A.; Inzitari, D.; Sivenius, J.; Trichopoulou, A.; Tuomilehto, J.; Koudstaal, P.J.; et al. Gamma-glutamyltransferase and risk of stroke: The EUROSTROKE project. J. Epidemiol. Community Health 2002, 56 (Suppl. 1), i25–i29. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.C.; Kang, D.R.; Nam, C.M.; Hur, N.W.; Shim, J.S.; Jee, S.H.; Suh, I. Elevated serum aminotransferase level as a predictor of intracerebral hemorrhage: Korea medical insurance corporation study. Stroke 2005, 36, 1642–1647. [Google Scholar] [CrossRef] [Green Version]
- Weikert, C.; Drogan, D.; di Giuseppe, R.; Fritsche, A.; Buijsse, B.; Nothlings, U.; Willich, S.N.; Berger, K.; Boeing, H. Liver enzymes and stroke risk in middle-aged German adults. Atherosclerosis 2013, 228, 508–514. [Google Scholar] [CrossRef]
- Fraser, A.; Harris, R.; Sattar, N.; Ebrahim, S.; Smith, G.D.; Lawlor, D.A. Gamma-glutamyltransferase is associated with incident vascular events independently of alcohol intake: Analysis of the British Women’s Heart and Health Study and Meta-Analysis. Arterioscler. Thromb. Vasc. Biol. 2007, 27, 2729–2735. [Google Scholar] [CrossRef] [Green Version]
- Matteoni, C.A.; Younossi, Z.M.; Gramlich, T.; Boparai, N.; Liu, Y.C.; McCullough, A.J. Nonalcoholic fatty liver disease: A spectrum of clinical and pathological severity. Gastroenterology 1999, 116, 1413–1419. [Google Scholar] [CrossRef]
- Caldwell, S.H.; Oelsner, D.H.; Iezzoni, J.C.; Hespenheide, E.E.; Battle, E.H.; Driscoll, C.J. Cryptogenic cirrhosis: Clinical characterization and risk factors for underlying disease. Hepatology 1999, 29, 664–669. [Google Scholar] [CrossRef] [PubMed]
- Dixon, J.L.; Ginsberg, H.N. Hepatic synthesis of lipoproteins and apolipoproteins. Semin. Liver Dis. 1992, 12, 364–372. [Google Scholar] [CrossRef]
- Lisman, T.; Porte, R.J. Pathogenesis, prevention, and management of bleeding and thrombosis in patients with liver diseases. Res. Pract. Thromb. Haemost. 2017, 1, 150–161. [Google Scholar] [CrossRef] [PubMed]
- Moshage, H. Cytokines and the hepatic acute phase response. J. Pathol. 1997, 181, 257–266. [Google Scholar] [CrossRef]
- Angulo, P.; Keach, J.C.; Batts, K.P.; Lindor, K.D. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology 1999, 30, 1356–1362. [Google Scholar] [CrossRef] [PubMed]
- Rej, R. Aspartate aminotransferase activity and isoenzyme proportions in human liver tissues. Clin. Chem. 1978, 24, 1971–1979. [Google Scholar] [CrossRef]
- Nathwani, R.A.; Pais, S.; Reynolds, T.B.; Kaplowitz, N. Serum alanine aminotransferase in skeletal muscle diseases. Hepatology 2005, 41, 380–382. [Google Scholar] [CrossRef]
- Whitfield, J.B. Gamma glutamyl transferase. Crit. Rev. Clin. Lab. Sci. 2001, 38, 263–355. [Google Scholar] [CrossRef]
- Rhoads, G.G.; Feinleib, M. Serum triglyceride and risk of coronary heart disease, stroke, and total mortality in Japanese-American men. Arteriosclerosis 1983, 3, 316–322. [Google Scholar] [CrossRef] [Green Version]
- Salonen, J.T.; Puska, P. Relation of serum cholesterol and triglycerides to the risk of acute myocardial infarction, cerebral stroke and death in eastern Finnish male population. Int. J. Epidemiol. 1983, 12, 26–31. [Google Scholar] [CrossRef]
- Machado, M.V.; Cortez-Pinto, H. Non-invasive diagnosis of non-alcoholic fatty liver disease. A critical appraisal. J. Hepatol. 2013, 58, 1007–1019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gastaldelli, A.; Kozakova, M.; Hojlund, K.; Flyvbjerg, A.; Favuzzi, A.; Mitrakou, A.; Balkau, B.; Investigators, R. Fatty liver is associated with insulin resistance, risk of coronary heart disease, and early atherosclerosis in a large European population. Hepatology 2009, 49, 1537–1544. [Google Scholar] [CrossRef] [PubMed]
- Lazo, M.; Clark, J.M. The epidemiology of nonalcoholic fatty liver disease: A global perspective. Semin. Liver Dis. 2008, 28, 339–350. [Google Scholar] [CrossRef] [PubMed]

| Variables | FLI Score | p-Value | ||
|---|---|---|---|---|
| <30 | 30–59 | ≥60 | ||
| Participants, n | 4550 | 2229 | 1185 | |
| Gender, n (%) | <0.001 | |||
| Men | 1561 (34.3) | 1043 (46.79) | 708 (59.75) | |
| Women | 2989 (65.7) | 1186 (53.21) | 477 (40.25) | |
| Age, y | 51.67 ± 0.13 | 53.86 ± 0.18 | 53.06 ± 0.25 | <0.001 |
| BMI, kg/m2 | 23.04 ± 0.04 | 26.02 ± 0.04 | 28.05 ± 0.09 | <0.001 |
| Drinking Status, n(%) | <0.001 | |||
| Never | 2615 (57.5) | 1131 (50.7) | 469 (39.6) | |
| Former | 287 (6.3) | 189 (8.5) | 102 (8.6) | |
| Current | 1648 (36.2) | 909 (40.8) | 614 (51.8) | |
| Smoking Status, n(%) | <0.001 | |||
| Never | 3231 (71.0) | 1346 (60.4) | 563 (47.5) | |
| Former | 516 (11.3) | 353 (15.8) | 244 (20.6) | |
| Current | 803 (17.7) | 530 (23.8) | 378 (31.9) | |
| Physical activity, MET-h/week | 23.25 ± 0.22 | 22.85 ± 0.32 | 22.52 ± 0.44 | 0.267 |
| AST | 25.91 ± 0.12 | 29.31 ± 0.38 | 35.99 ± 0.78 | <0.001 |
| ALT | 21.44 ± 0.15 | 30.26 ± 0.55 | 43.20 ± 1.45 | <0.001 |
| γ-GT | 16.38 ± 0.16 | 33.31 ± 0.73 | 74.41 ± 3.60 | <0.001 |
| Comorbidity, n(%) | ||||
| Hypertension | 1310 (28.9) | 1107 (49.7) | 716 (60.4) | <0.001 |
| Diabetes mellitus | 228 (5.0) | 255 (11.4) | 200 (16.9) | <0.001 |
| Hyperlipidemia | 1668 (36.7) | 1367 (61.3) | 859 (72.5) | <0.001 |
| Coronary artery disease | 23 (0.51) | 29 (1.3) | 13 (1.1) | 0.001 |
| Cancer | 59 (1.3) | 15 (0.7) | 12 (1.0) | 0.064 |
| FLI | p-Value | |||
|---|---|---|---|---|
| <30 (n = 4550) | 30–59.9 (n = 2229) | ≥60 (n = 1185) | ||
| Incident stroke case (n, %) | 76 (1.67) | 56 (2.51) | 36 (3.03) | 0.0004 |
| Crude Hazard ratio | 1.00 | 1.53 (1.08–2.16) | 1.92 (1.29–2.85) | 0.0025 |
| Model 1 | 1.00 | 1.31 (0.92–1.86) | 1.64 (1.10–2.46) | <0.001 |
| Model 2 | 1.00 | 1.42 (0.95–2.14) | 1.97 (1.17–3.32) | <0.001 |
| Model 3 | 1.00 | 1.41 (0.94–2.21) | 1.98 (1.17–3.34) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.-J.; Jung, M.-H.; Jeong, S.-H.; Hong, Y.-P.; Kim, Y.I.; An, S.J. The Association between Nonalcoholic Fatty Liver Disease and Stroke: Results from the Korean Genome and Epidemiology Study (KoGES). Int. J. Environ. Res. Public Health 2020, 17, 9568. https://doi.org/10.3390/ijerph17249568
Yang Y-J, Jung M-H, Jeong S-H, Hong Y-P, Kim YI, An SJ. The Association between Nonalcoholic Fatty Liver Disease and Stroke: Results from the Korean Genome and Epidemiology Study (KoGES). International Journal of Environmental Research and Public Health. 2020; 17(24):9568. https://doi.org/10.3390/ijerph17249568
Chicago/Turabian StyleYang, Yun-Jung, Mi-Hyang Jung, Seok-Hoo Jeong, Yeon-Pyo Hong, Yeong In Kim, and Sang Joon An. 2020. "The Association between Nonalcoholic Fatty Liver Disease and Stroke: Results from the Korean Genome and Epidemiology Study (KoGES)" International Journal of Environmental Research and Public Health 17, no. 24: 9568. https://doi.org/10.3390/ijerph17249568





