An Early, Universal Mediterranean Diet-Based Intervention in Pregnancy Reduces Cardiovascular Risk Factors in the “Fourth Trimester”
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Data Collection
2.2.1. Clinical Data
2.2.2. Outcomes Measures
2.2.3. Lifestyle Assessment
2.2.4. Biochemical Analysis
2.4. Statistical Analysis
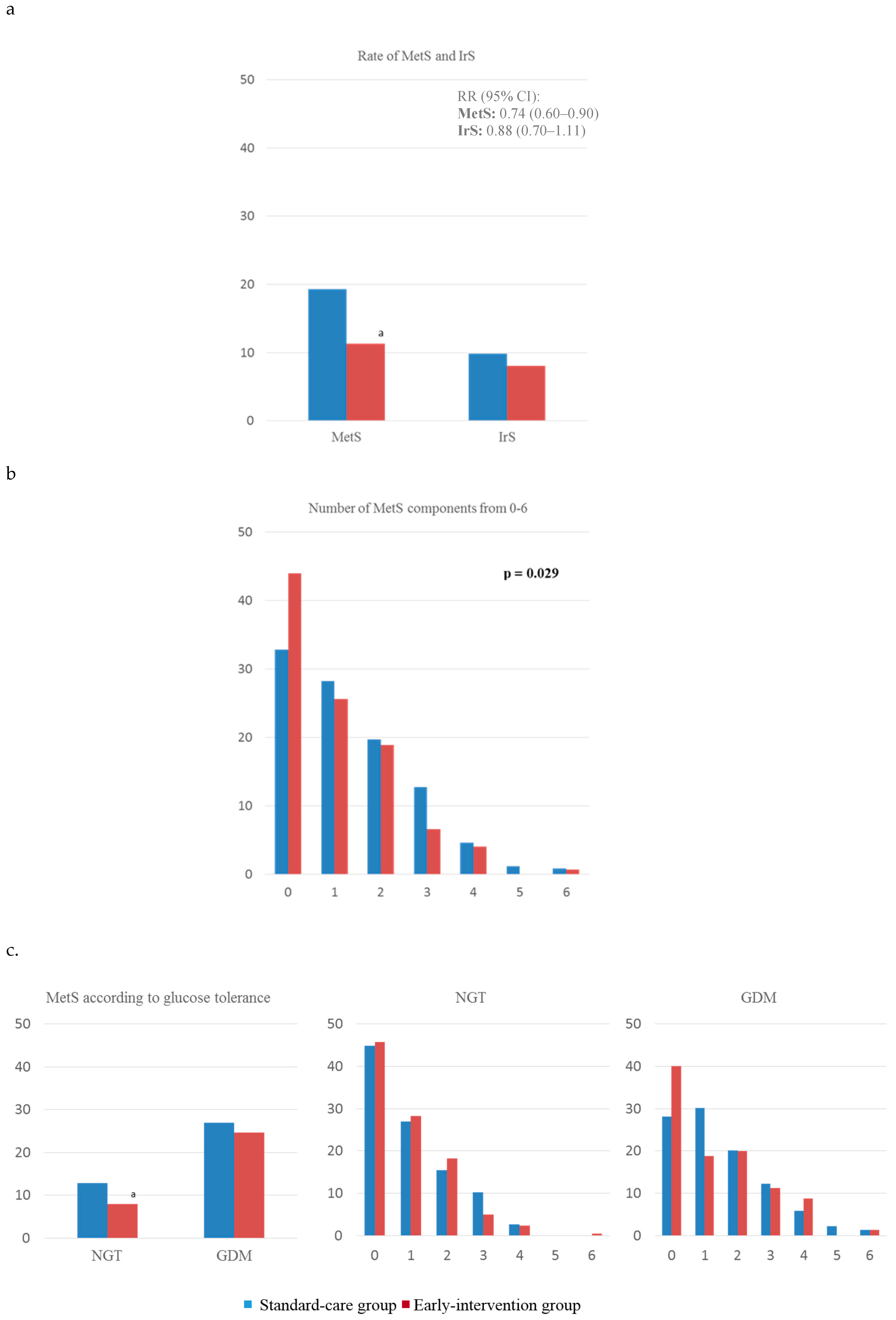
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kramer, C.K.; Campbell, S.; Retnakaran, R. Gestational diabetes and the risk of cardiovascular disease in women: A systematic review and meta-analysis. Diabetologia 2019, 62, 905–914. [Google Scholar] [CrossRef] [PubMed]
- Kitzmiller, J.L.; Dang-Kilduff, L.; Taslimi, M.M. Gestational Diabetes After Delivery: Short-term management and long-term risks. Diabetes Care 2007, 30, S225–S235. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 736. Obstet. Gynecol. 2018, 131, e140–e150. [Google Scholar] [CrossRef] [PubMed]
- Spelke, B.; Werner, E. The Fourth Trimester of Pregnancy: Committing to Maternal Health and Well-Being Postpartum. R. I. Med. J. 2018, 101, 30–33. [Google Scholar]
- Noctor, E.; Crowe, C.; Carmody, L.A.; Kirwan, B.; O’Dea, A.; Glynn, L.G.; McGuire, B.E.; O’Shea, P.M.; Dunne, F.P. ATLANTIC-DIP: Prevalence of metabolic syndrome and insulin resistance in women with previous gestational diabetes mellitus by International Association of Diabetes in Pregnancy Study Groups criteria. Acta Diabetol. 2015, 52, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Nouhjah, S.; Shahbazian, H.; Shahbazian, N.; Jahanfar, S.; Jahanshahi, A.; Cheraghian, B.; Mohammadi, Z.D.; Ghodrati, N.; Houshmandi, S. Early postpartum metabolic syndrome in women with or without gestational diabetes: Results from Life after Gestational Diabetes Ahvaz cohort study. Diabetes Metab. Syndr. Clin. Res. Rev. 2018, 12, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Assaf-Balut, C.; García de la Torre, N.; Durán, A.; Fuentes, M.; Bordiú, E.; del Valle, L.; Familiar, C.; Ortolá, A.; Jiménez, I.; Herraiz, M.A.; et al. A Mediterranean diet with additional extra virgin olive oil and pistachios reduces the incidence of gestational diabetes mellitus (GDM): A randomized controlled trial: The St. Carlos GDM prevention study. PLoS ONE 2017, 12, e0185873. [Google Scholar] [CrossRef]
- Assaf-Balut, C.; García de la Torre, N.; Fuentes, M.; Durán, A.; Bordiú, E.; del Valle, L.; Valerio, J.; Jiménez, I.; Herraiz, M.; Izquierdo, N.; et al. A High Adherence to Six Food Targets of the Mediterranean Diet in the Late First Trimester is Associated with a Reduction in the Risk of Materno-Foetal Outcomes: The St. Carlos Gestational Diabetes Mellitus Prevention Study. Nutrients 2018, 11, 66. [Google Scholar] [CrossRef]
- Assaf-Balut, C.; García de la Torre, N.; Duran, A.; Fuentes, M.; Bordiú, E.; del Valle, L.; Familiar, C.; Valerio, J.; Jiménez, I.; Herraiz, M.A.; et al. A Mediterranean Diet with an Enhanced Consumption of Extra Virgin Olive Oil and Pistachios Improves Pregnancy Outcomes in Women Without Gestational Diabetes Mellitus: A Sub-Analysis of the St. Carlos Gestational Diabetes Mellitus Prevention Study. Ann. Nutr. Metab. 2019, 74, 69–79. [Google Scholar] [CrossRef]
- Salas-Salvadó, J.; Guasch-Ferré, M.; Lee, C.-H.; Estruch, R.; Clish, C.B.; Ros, E. Protective Effects of the Mediterranean Diet on Type 2 Diabetes and Metabolic Syndrome. J. Nutr. 2015, 146, 920S–927S. [Google Scholar] [CrossRef]
- Huvinen, E.; Koivusalo, S.B.; Meinilä, J.; Valkama, A.; Tiitinen, A.; Rönö, K.; Stach-Lempinen, B.; Eriksson, J.G. Effects of a Lifestyle Intervention During Pregnancy and First Postpartum Year: Findings From the RADIEL Study. J. Clin. Endocrinol. Metab. 2018, 103, 1669–1677. [Google Scholar] [CrossRef] [PubMed]
- Assaf-Balut, C.; Garcia de la Torre, N.; Durán, A.; Fuentes, M.; Bordiú, E.; del Valle, L.; Valerio, J.; Familiar, C.; Jiménez, I.; Herraiz, M.A.; et al. Medical nutrition therapy for gestational diabetes mellitus based on Mediterranean Diet principles: A subanalysis of the St Carlos GDM Prevention Study. BMJ Open Diabetes Res. Care 2018, 6, e000550. [Google Scholar] [CrossRef] [PubMed]
- García de la Torre, N.; Assaf-Balut, C.; Jiménez Varas, I.; del Valle, L.; Durán, A.; Fuentes, M.; del Prado, N.; Bordiú, E.; Valerio, J.J.; Herraiz, M.A.; et al. Effectiveness of Following Mediterranean Diet Recommendations in the Real World in the Incidence of Gestational Diabetes Mellitus (GDM) and Adverse Maternal-Foetal Outcomes: A Prospective, Universal, Interventional Study with a Single Group. The St Carlos Study. Nutrients 2019, 11, 1210. [Google Scholar] [CrossRef]
- Ruiz-Gracia, T.; Duran, A.; Fuentes, M.; Rubio, M.A.; Runkle, I.; Carrera, E.F.; Torrejón, M.J.; Bordiú, E.; del Valle, L.; García de la Torre, N.; et al. Lifestyle patterns in early pregnancy linked to gestational diabetes mellitus diagnoses when using IADPSG criteria. The St Carlos gestational study. Clin. Nutr. 2016, 35, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Marcuello, C.; Calle-Pascual, A.L.; Fuentes, M.; Runkle, I.; Rubio, M.A.; Montañez, C.; Rojo-Martinez, G.; Soriguer, F.; Bordiu, E.; Goday, A.; et al. Prevalence of the metabolic syndrome in Spain using regional cutoff points for waist circumference: The di@bet.es study. Acta Diabetol. 2013, 50, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Larrad, M.T.; Fernández-Pérez, C.; Corbatón-Anchuelo, A.; Gabriel, R.; Lorenzo, C.; Serrano-Ríos, M. Revised waist circumference cut-off points for the criteria of abdominal obesity in the Spanish population: Multicenter nationwide Spanish population based study. Av. Diabetol. 2011, 27, 168–174. [Google Scholar] [CrossRef]
- Retnakaran, R.; Qi, Y.; Connelly, P.W.; Sermer, M.; Zinman, B.; Hanley, A.J.G. Glucose intolerance in pregnancy and postpartum risk of metabolic syndrome in young women. J. Clin. Endocrinol. Metab. 2010, 95, 670–677. [Google Scholar] [CrossRef]
- Nouhjah, S.; Shahbazian, H.; Jahanfar, S.; Shahbazian, N.; Jahanshahi, A.; Cheraghian, B.; Hardanipasand, L.; Moradi, M. Early Postpartum Lipid Profile in Women with and Without Gestational Diabetes Mellitus: Results of a Prospective Cohort Study. Iran. Red Crescent Med. J. 2017, 19. [Google Scholar] [CrossRef]
- Ferrara, A.; Hedderson, M.M.; Albright, C.L.; Ehrlich, S.F.; Quesenberry, C.P.; Peng, T.; Feng, J.; Ching, J.; Crites, Y. A Pregnancy and Postpartum Lifestyle Intervention in Women With Gestational Diabetes Mellitus Reduces Diabetes Risk Factors: A feasibility randomized control trial. Diabetes Care 2011, 34, 1519–1525. [Google Scholar] [CrossRef]
- Linné, Y.; Dye, L.; Barkeling, B.; Rössner, S. Long-Term Weight Development in Women: A 15-Year Follow-up of the Effects of Pregnancy. Obes. Res. 2004, 12, 1166–1178. [Google Scholar] [CrossRef]
- Moran, L.J.; Flynn, A.C.; Louise, J.; Deussen, A.R.; Dodd, J.M. The effect of a lifestyle intervention on pregnancy and postpartum dietary patterns determined by factor analysis. Obesity 2017, 25, 1022–1032. [Google Scholar] [CrossRef] [PubMed]
- Kieffer, E.C.; Sinco, B.; Kim, C. Health Behaviors Among Women of Reproductive Age With and Without a History of Gestational Diabetes Mellitus. Diabetes Care 2006, 29, 1788–1793. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, B.; Razurel, C. Determinants of postpartum physical activity, dietary habits and weight loss after gestational diabetes mellitus. J. Nurs. Manag. 2013, 21, 58–69. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Hsu-Hage, B.; Zhang, H.; Zhang, C.; Zhang, Y.; Zhang, C. Women with impaired glucose tolerance during pregnancy have significantly poor pregnancy outcomes. Diabetes Care 2002, 25, 1619–1624. [Google Scholar] [CrossRef] [PubMed]


| Variables | Standard-Care Group (n = 676) | Early-Intervention Group (n = 999) | p Value |
|---|---|---|---|
| Age (years) | 33.54 ± 5.11 | 33.32 ± 4.78 | 0.369 |
| Race/Ethnicity n (%) | |||
| Caucasian | 467 (69.3) | 676(67.7) | 0.275 |
| Hispanic | 185 (27.4) | 303 (30.4) | |
| Others | 24 (1.9) | 20 (1.9) | |
| Family history >1 component of MetS | 216 (32.0) | 455 (45.5) | 0.001 |
| Miscarriage | 178 (26.4) | 335 (33.5) | 0.006 |
| Number of pregnancies n (%) | |||
| Primiparous | 292 (43.8) | 447 (44.8) | 0.998 |
| Second pregnancy | 208 (31.2) | 301 (30.1) | |
| >2 pregnancies | 176 (26.0) | 251 (25.1) | |
| Prepregnancy BW (kg) | 63.3 ± 12.4 | 61.6 ± 11.1 | 0.003 |
| Prepregnancy BMI (kg/m2) | 24.2 ± 4.3 | 23.3 ± 4.0 | 0.001 |
| BW at 12–14 GW (kg) | 64.1 ± 11.7 | 63.5 ± 11.2 | 0.421 |
| BW gain at 12–14 GW (kg) | 2.0 ± 3.1 | 1.9 ± 3.1 | 0.338 |
| BW gain at 24–28 GW | 7.6 ± 3.8 | 7.0 ± 4.2 | 0.05 |
| BW gain at 36–38 GW | 11.4 ± 5.17 | 11.8 ± 6.4 | |
| University Degree | 442 (65.4) | 709 (71.0) | 0.209 |
| Employed | 543 (80.6) | 632 (82.1) | 0.089 |
| Smoker | |||
| Never | 421 (62.6) | 582 (58.3) | 0.006 |
| Current | 142 (21.2) | 166 (16.6) | |
| GDM at 24–28 GW | 304 (49.5) | 199 (19.9) | 0.001 |
| Variables | Standard-Care Group | Early-Intervention Group | ||||
|---|---|---|---|---|---|---|
| All | Glucose Tolerance | All | Glucose Tolerance | |||
| NGT | GDM | NGT | GDM | |||
| Pregestational | ||||||
| Nutrition Score | 1.2 ± 3.4 | 0.4 ± 3.1 | 1.9 ± 3.5 | 0.5 ± 3.2 *** | 0.5 ± 3.1 | 0.7 ± 2.8 *** |
| MedDiet Score | 5.1 ± 1.8 | 5.0 ± 1.8 | 5.1 ± 1.7 | 5.4 ± 1.7 ** | 5.3 ± 1.7 * | 5.5 ± 1.7 |
| 36–38 GW | ||||||
| Nutrition Score | 3.8 ± 3.6 | 2.6 ± 3.1 | 6.9 ± 2.9 | 4.7 ± 3.6 ** | 3.9 ± 3.3 *** | 7.7 ± 3.0 |
| MD (95% CI) | 3.2 (2.7-3.8) c | 2.2 (1.6-2.8) c | 6.1 (5.1-7.1) c | 4.2 (3.9-4.5) c | 3.4 (3.2-3.7) c | 7.0 (6.4-7.6) c |
| MedDiet Score | 5.8 ± 1.8 | 5.1 ± 1.4 | 7.7 ± 1.4 | 6.4 ± 2.0 *** | 5.9 ± 1.8 *** | 8.1 ± 1.9 |
| MD (95% CI) | 0.8(0.4–1.1) c | 0.0 (−0.3–0.4) | 2.8 (2.3–3.4) c | 1.0 (0.9–1.2) c | 0.7 (0.5–0.8) c | 2.6 (2.2–3.0) |
| Postpartum | ||||||
| Nutrition Score | 2.6 ± 3.6 | 2.4 ± 3.7 | 3.3 ± 3.5 | 3.1 ± 3.7 | 2.8 ± 3.7* | 3.9 ± 3.5 |
| MD (95% CI) | 2.0 (1.5–2.6) c | 2.0 (1.4–2.6) c | 2.1 (1.1–3.1) c | 2.6 (2.3–2.8) c | 2.4 (2.1–2.7) c | 3.2 (2.6–3.8) c |
| MedDiet Score | 5.5 ± 1.6 | 5.5 ± 1.7 | 5.6 ± 1.5 | 6.0 ± 1.7 *** | 5.8 ± 1.7 * | 6.6 ± 1.7 ** |
| MD (95% CI) | 0.5 (0.1-0.8) b | 0.5 (0.1–0.8) a | 0.4 (−0.2–1.0) | 0.6 (0.5–0.8) c | 0.5 (0.4–0.7) c | 1.0 (0.6–1.3) c |
| Clinical and Biochemical Parameters | Variables | Standard-Care Group | Early-Intervention Group | ||||
| All | Glucose Tolerance | All | Glucose Tolerance | ||||
| NGT | GDM | NGT | GDM | ||||
| N (%) | 676 | 372 (55.0) | 304 (45.0) | 999 | 800 (80.1) | 199 (19.9) | |
| Age (year) | 33.5 ± 5.1 | 32.3 ± 5.3 | 34.3 ± 4.9 | 33.3 ± 4.8 | 33.0 ± 4.8 | 34.3 ± 4.5 | |
| Anthropometric parameters | Pregestational BW (kg) | 63.3 ± 12.4 | 60.7 ± 10.2 | 65.2 ± 13.1 | 61.6 ± 11.1 ** | 60.6 ± 11.1 | 65.1 ± 12.7 |
| Pregestational BMI (kg/m2) | 24.2 ± 4.3 | 23.0 ± 3.9 | 24.9 ± 4.4 | 23.3 ± 4.0 *** | 22.9 ± 3.6 | 24.9 ± 4.6 | |
| Postpartum BW (kg) | 67.7 ± 12.8 | 65.5 ± 12.2 | 68.7 ± 13.2 | 66.3 ± 11.3 | 65. 5 ± 10.8 | 68.6 ± 11.9 | |
| Postpartum BMI (kg/m2) | 25.8 ± 4.5 | 24.9 ± 4.4 | 26.3 ± 4.6 | 25.1 ± 4.2 * | 24.7 ± 4.0 | 26.3 ± 4.5 | |
| BW change (kg) | 4.8 ± 6.0 | 5.2 ± 4.8 | 3.0 ± 5.4 | 3.7 ± 5.4 ** | 5.3 ± 5.9 | 3.3 ± 5.2 | |
| WC (cm) | 85.7 ± 10.3 | 84.2 ± 9.2 | 89.5 ± 8.6 | 85.8 ± 9.1 | 84.6 ± 9.1 | 86.8 ± 10.2 * | |
| Glucose regulation | Fasting glucose (mg/dL) | 87.3 ± 9.1 | 84.2 ± 9.2 | 89.0 ± 8.6 | 84.4 ± 7.6 *** | 83.7 ± 7.4 | 87.1 ± 7.8 * |
| HbA1c-IFCC % | 5.4 ± 0.3 | 5.3 ± 0.3 | 5.4 ± 0.3 | 5.3 ± 0.3 *** | 5.2 ± 0.3 | 5.3 ± 0.3 *** | |
| Fasting insulin (mcUI/mL) | 6.9 ± 6.0 | 7.4 ± 6.2 | 6.9 ± 5.6 | 6.5 ± 5.9 | 6.4 ± 5.9 * | 6.9 ± 6.0 | |
| HOMA-IR | 1.7 ± 1.4 | 1.8 ± 1.6 | 1.7 ± 1.3 | 1.6 ± 1.4 | 1.6 ± 1.4 | 1.7 ± 1.4 | |
| Blood pressure | sBP (mm Hg) | 116 ± 14 | 111 ± 13 | 121 ± 14 | 111 ± 12 *** | 110 ± 12 | 114 ± 12 *** |
| dBP (mm Hg) | 73 ± 10 | 71 ± 11 | 76 ± 11 | 71 ± 10 * | 70 ± 9 | 73 ± 9 * | |
| Lipid panel | Total cholesterol (mg/dL) | 211 ± 42 | 202 ± 38 | 214 ± 42 | 197 ± 37 *** | 195 ± 36 * | 203 ± 38 ** |
| HDL cholesterol (mg/dL) | 63 ± 14 | 64 ± 13 | 62 ± 13 | 67 ± 18 *** | 64 ± 19 | 68 ± 15 *** | |
| LDL cholesterol (mg/dL) | 130 ± 36 | 124 ± 31 | 130 ± 37 | 116 ± 30 *** | 114 ± 29 *** | 123 ± 33 | |
| Triglycerides (g/L) | 88 ± 45 | 82 ± 41 | 89 ± 45 | 82 ± 47 ** | 80 ± 47 | 85 ± 47 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Assaf-Balut, C.; Garcia de la Torre, N.; Durán, A.; Bordiu, E.; del Valle, L.; Familiar, C.; Valerio, J.; Jimenez, I.; Herraiz, M.A.; Izquierdo, N.; et al. An Early, Universal Mediterranean Diet-Based Intervention in Pregnancy Reduces Cardiovascular Risk Factors in the “Fourth Trimester”. J. Clin. Med. 2019, 8, 1499. https://doi.org/10.3390/jcm8091499
Assaf-Balut C, Garcia de la Torre N, Durán A, Bordiu E, del Valle L, Familiar C, Valerio J, Jimenez I, Herraiz MA, Izquierdo N, et al. An Early, Universal Mediterranean Diet-Based Intervention in Pregnancy Reduces Cardiovascular Risk Factors in the “Fourth Trimester”. Journal of Clinical Medicine. 2019; 8(9):1499. https://doi.org/10.3390/jcm8091499
Chicago/Turabian StyleAssaf-Balut, Carla, Nuria Garcia de la Torre, Alejandra Durán, Elena Bordiu, Laura del Valle, Cristina Familiar, Johanna Valerio, Inés Jimenez, Miguel Angel Herraiz, Nuria Izquierdo, and et al. 2019. "An Early, Universal Mediterranean Diet-Based Intervention in Pregnancy Reduces Cardiovascular Risk Factors in the “Fourth Trimester”" Journal of Clinical Medicine 8, no. 9: 1499. https://doi.org/10.3390/jcm8091499
APA StyleAssaf-Balut, C., Garcia de la Torre, N., Durán, A., Bordiu, E., del Valle, L., Familiar, C., Valerio, J., Jimenez, I., Herraiz, M. A., Izquierdo, N., Runkle, I., de Miguel, M. P., Montañez, C., Barabash, A., Cuesta, M., Rubio, M. A., & Calle-Pascual, A. L. (2019). An Early, Universal Mediterranean Diet-Based Intervention in Pregnancy Reduces Cardiovascular Risk Factors in the “Fourth Trimester”. Journal of Clinical Medicine, 8(9), 1499. https://doi.org/10.3390/jcm8091499





