Continental Umbrella Review and Meta-Analysis of Work-Related Musculoskeletal Disorders Prevalence Among Healthcare Professionals
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Quality Assessment
2.4. Data Extraction
2.5. Overlap Analysis
2.6. Data and Statistical Analysis
3. Results
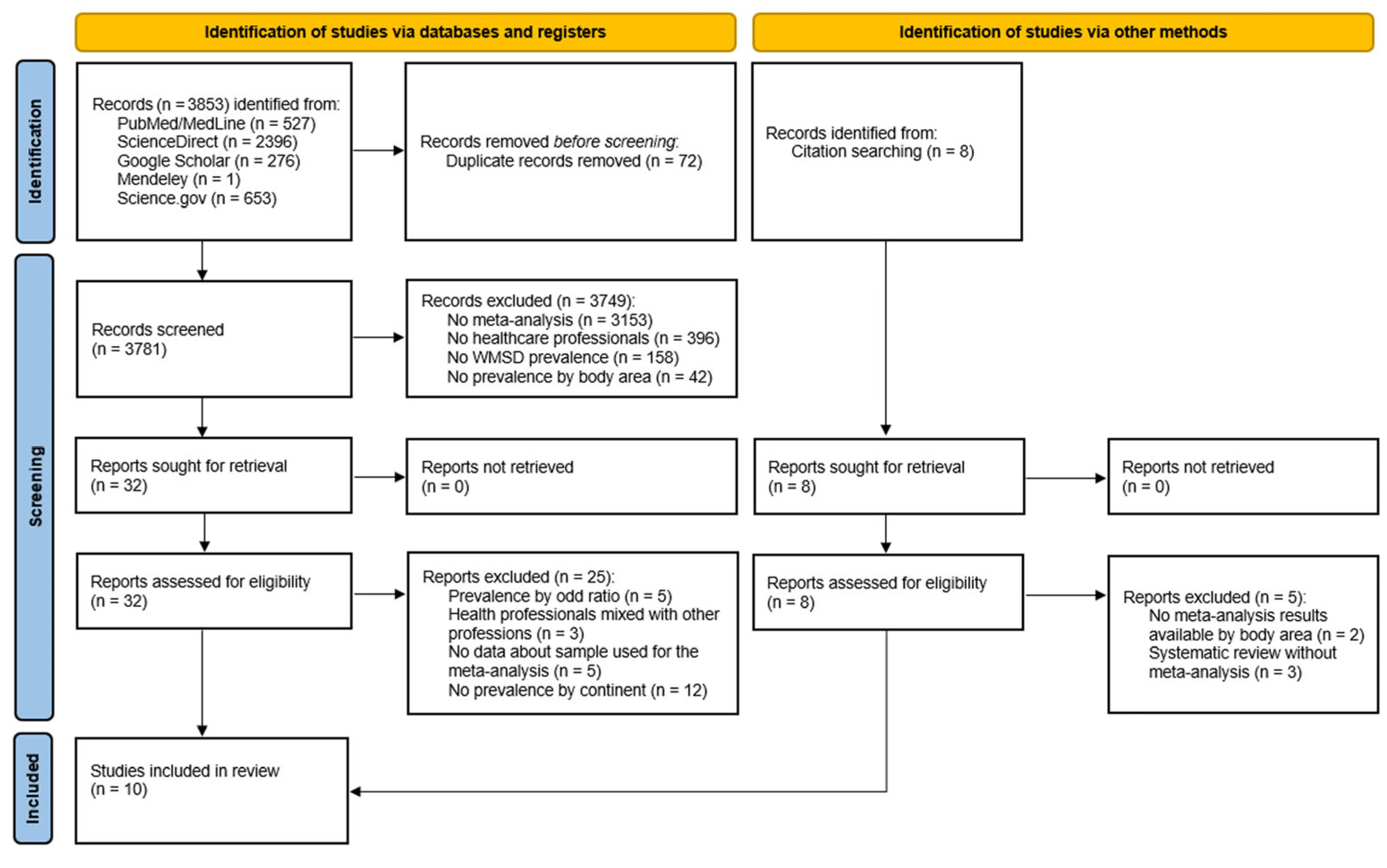
3.1. Database Search Results
3.2. Quality Appraisal
3.3. Study Characteristics
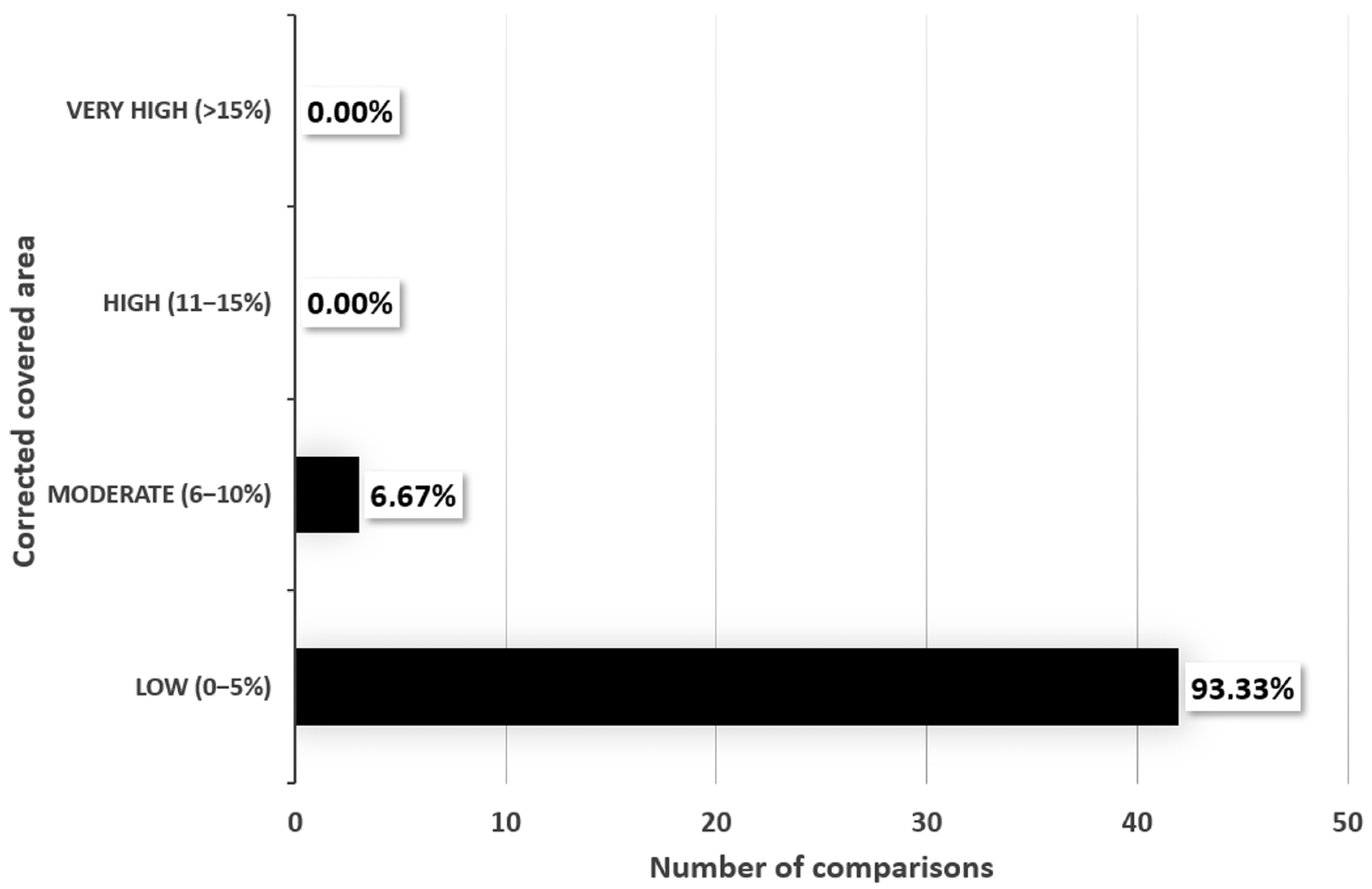
3.4. Overlap Assessment and Study Selection
3.5. Umbrella Review Results
3.5.1. Overall Prevalence
3.5.2. Prevalence by Body Area
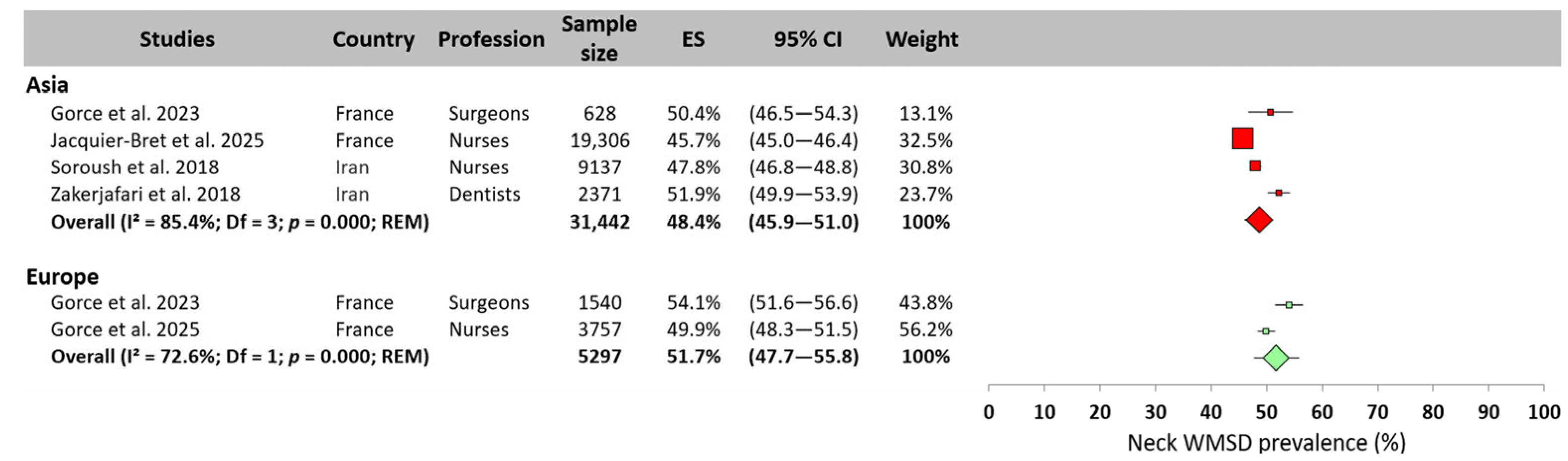
Neck
Upper Back
Lower Back
Shoulder
Elbow
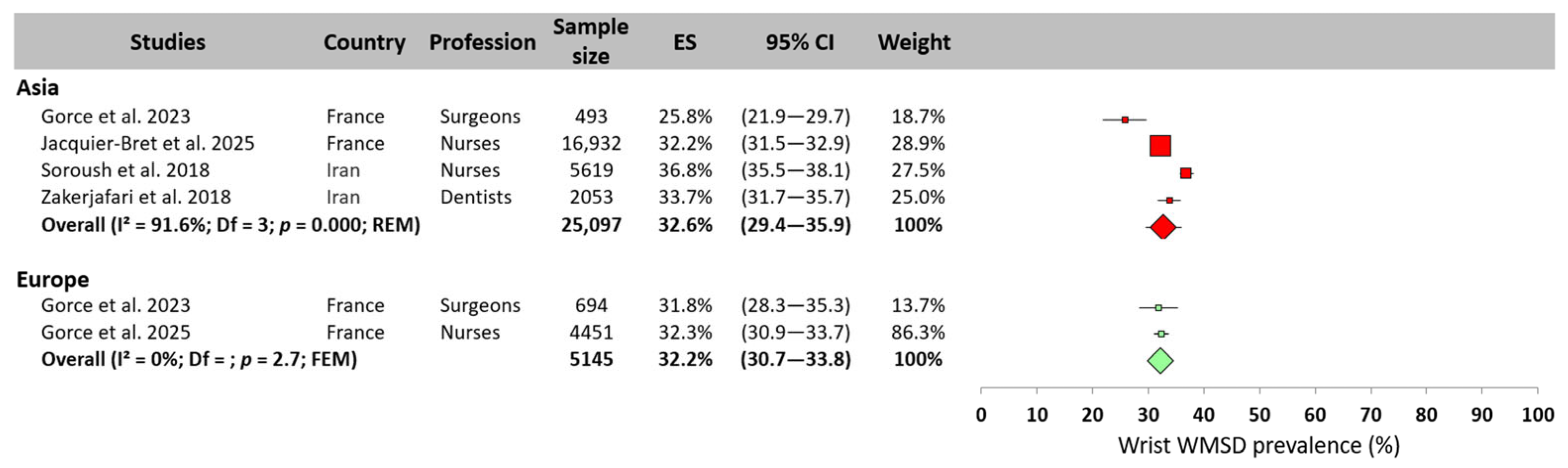
Wrist
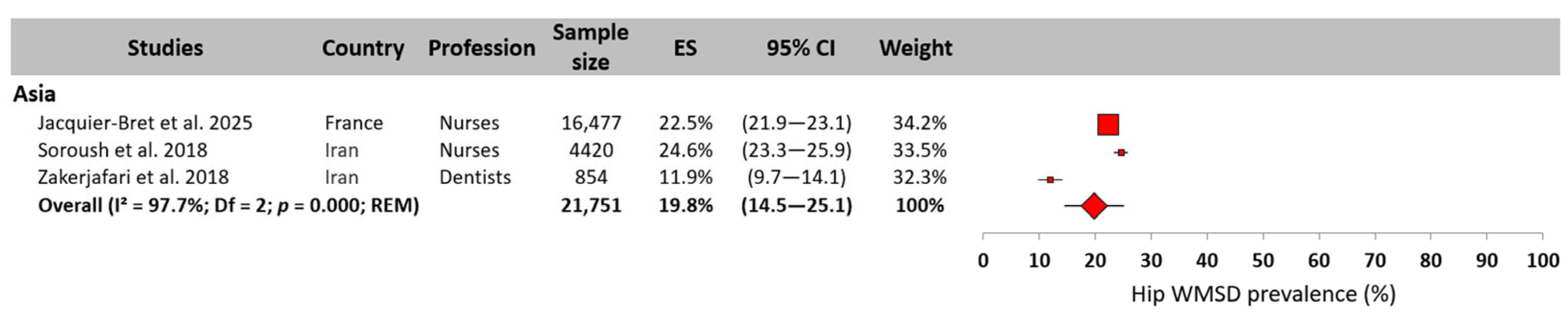
Hip
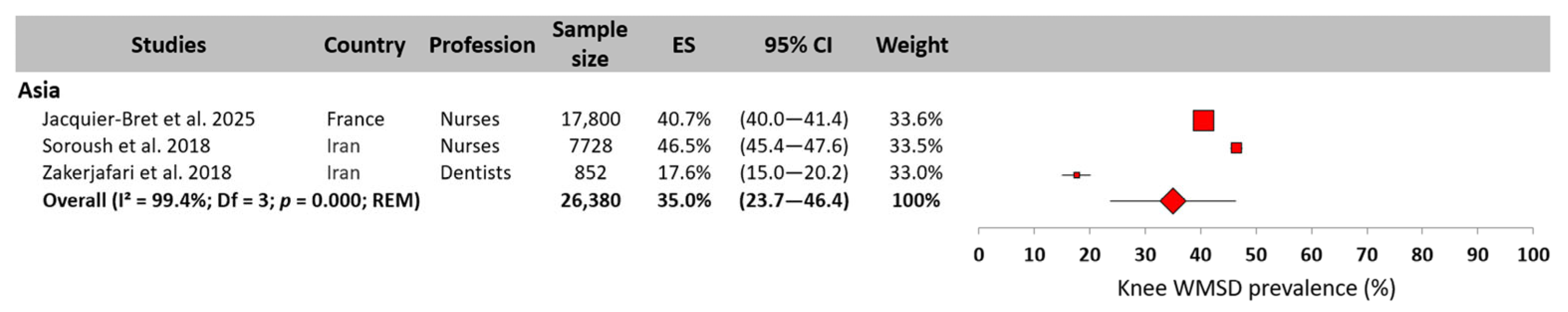
Knee
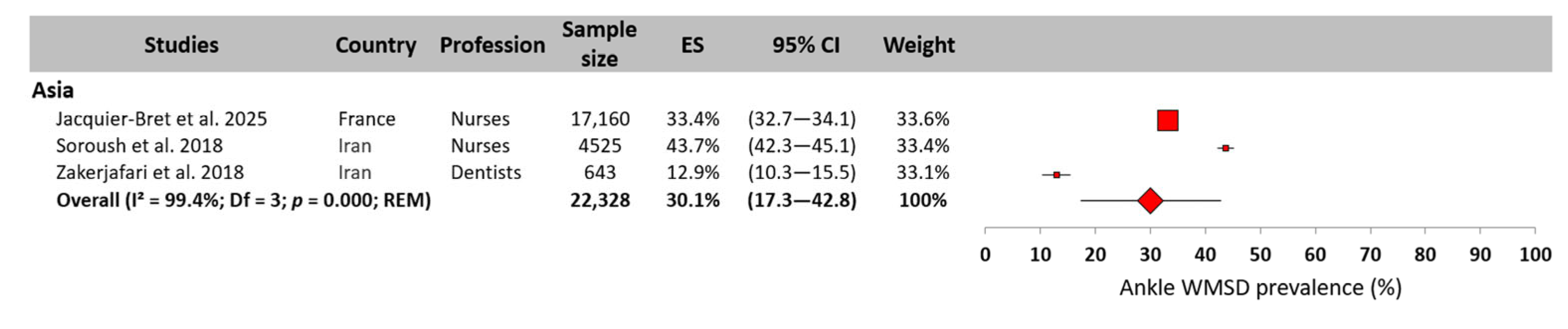
Ankle
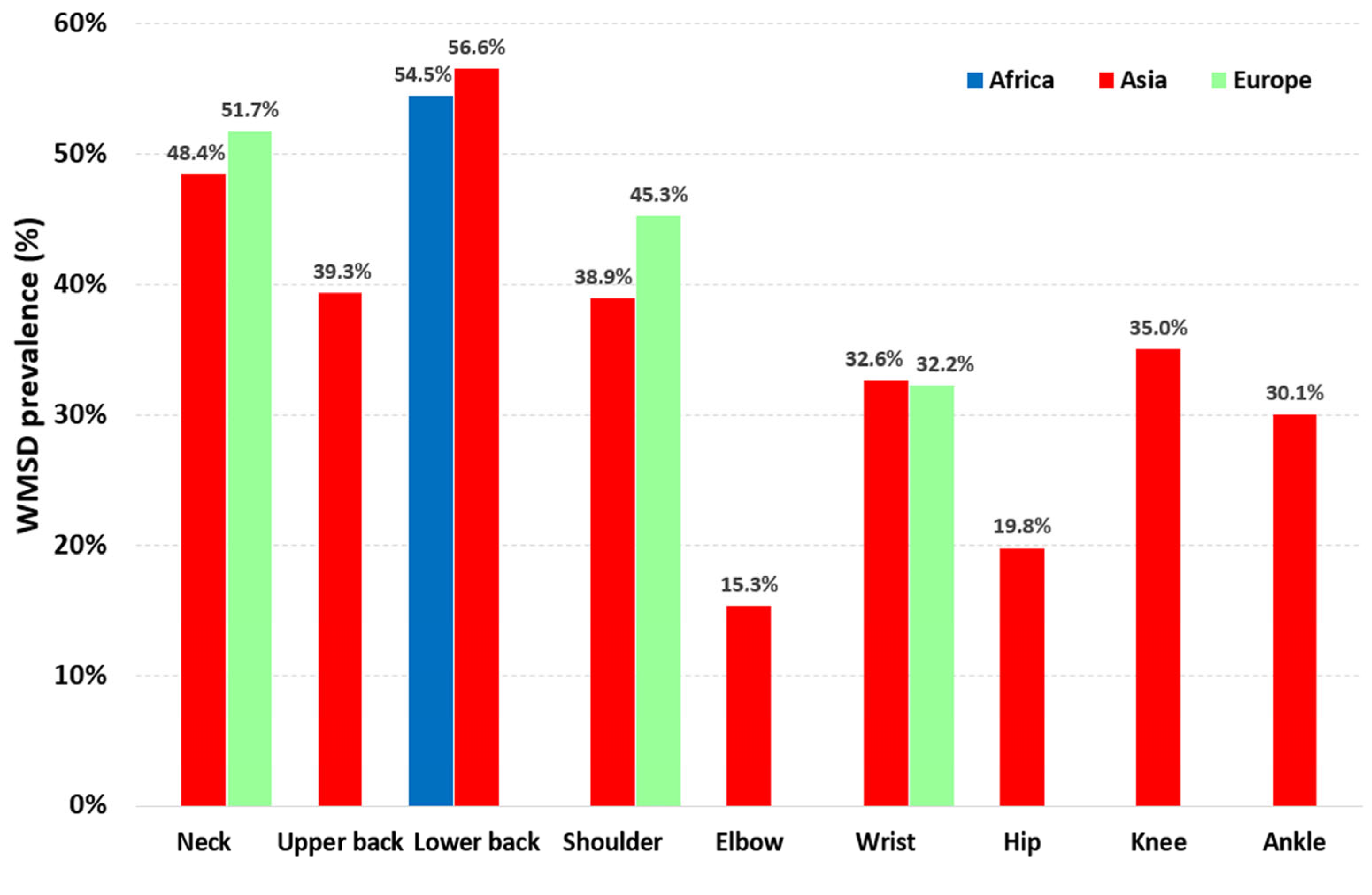
3.5.3. WMSD Prevalence Synthesis
4. Discussion
4.1. WMSD Prevalence—Overall and by Body Area
4.2. Limitations and Recommendations for Future Work
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CCA | Corrected Covered Area |
| FEM | Fixed-Effects Model |
| GROOVE | Graphical Representation of Overlap for Overviews |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| REM | Random-Effects Model |
| WMSDs | Work-Related Musculoskeletal Disorders |
Appendix A
| PRISMA Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10a | 10b | 11 | 12 | 13a | 13b | 13c | 13d | 13e | 13f | 14 | 15 | 16a | 16b |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Al Amer, 2020 [49] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 1 | 2 | 2 | 2 |
| Aremu et al., 2023 [31] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 |
| Gorce et al., 2023 [32] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 |
| Gorce et al., 2025 [28] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 |
| Jacquier-Bret et al., 2025 [29] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 |
| Kasa et al., 2020 [50] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 |
| Saberipour et al., 2019 [51] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 2 |
| Soroush et al., 2018 [26] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 |
| Wang et al., 2024 [27] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Zakerjafari et al., 2018 [52] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 |
| PRISMA Item | 17 | 18 | 19 | 20a | 20b | 20c | 20d | 21 | 22 | 23a | 23b | 23c | 23d | 24a | 24b | 24c | 25 | 26 | 27 | Total Score /84 Points | % | ||
| Al Amer, 2020 [49] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 2 | 2 | 70 | 83.3% | ||
| Aremu et al., 2023 [31] | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 2 | 1 | 1 | 0 | 2 | 2 | 0 | 2 | 2 | 2 | 66 | 78.6% | ||
| Gorce et al., 2023 [32] | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 2 | 1 | 1 | 0 | 2 | 2 | 2 | 68 | 81.0% | ||
| Gorce et al., 2025 [28] | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 74 | 88.1% | ||
| Jacquier-Bret et al., 2025 [29] | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 74 | 88.1% | ||
| Kasa et al., 2020 [50] | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 2 | 2 | 2 | 68 | 81.0% | ||
| Saberipour et al., 2019 [51] | 1 | 1 | 2 | 2 | 2 | 0 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 51 | 60.7% | ||
| Soroush et al., 2018 [26] | 1 | 1 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 61 | 72.6% | ||
| Wang et al., 2024 [27] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 80 | 95.2% | ||
| Zakerjafari et al., 2018 [52] | 2 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 63 | 75.0% | ||
Appendix B
| Al Amer, 2020 [49] | Aremu et al., 2023 [31] | Gorce et al., 2023 [32] | Gorce et al., 2025 [28] | Jacquier-Bret et al., 2025 [29] | Kasa et al., 2020 [50] | Saberipour et al., 2019 [51] | Soroush et al., 2018 [26] | Wang et al., 2024 [27] | |
|---|---|---|---|---|---|---|---|---|---|
| Aremu et al., 2023 [31] | 0.0% | ||||||||
| Gorce et al., 2023 [32] | 0.0% | 0.0% | |||||||
| Gorce et al., 2025 [28] | 0.0% | 0.0% | 0.0% | ||||||
| Jacquier-Bret et al., 2025 [29] | 1.8% | 0.0% | 0.0% | 0.0% | |||||
| Kasa et al., 2020 [50] | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | ||||
| Saberipour et al., 2019 [51] | 0.0% | 0.0% | 0.0% | 0.0% | 7.4% | 0.0% | |||
| Soroush et al., 2018 [26] | 0.0% | 0.0% | 0.0% | 0.0% | 9.3% | 0.0% | 5.6% | ||
| Wang et al., 2024 [27] | 0.0% | 0.0% | 0.0% | 0.0% | 3.3% | 0.0% | 0.0% | 0.0% | |
| Zakerjafari et al., 2018 [52] | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% |
| 45 | Total number of comparisons | ||||||||
| 0 | Very high overlap (CCA ≥ 15%) | ||||||||
| 0 | High overlap (10% ≤ CCA < 15%) | ||||||||
| 3 | Moderate overlap (5% ≤ CCA< 10%) | ||||||||
| 42 | Low overlap (CCA < 5%) | ||||||||
References
- Kee, D. Characteristics of Work-Related Musculoskeletal Disorders in Korea. Int. J. Environ. Res. Public Health 2023, 20, 1024. [Google Scholar] [CrossRef]
- Ibrahim, B.A.; Gaafar, S.E.M. Work-related musculoskeletal complaints: Risk factors and impact on work productivity among university administrative employees. J. Egypt. Public. Health. Assoc. 2024, 99, 10. [Google Scholar] [CrossRef]
- Gorce, P.; Jacquier-Bret, J. A systematic review of work-related musculoskeletal disorders among physical therapists and physiotherapists. J. Bodyw. Mov. Ther. 2024, 38, 350–367. [Google Scholar] [CrossRef] [PubMed]
- da Costa, B.R.; Vieira, E.R. Risk factors for work-related musculoskeletal disorders: A systematic review of recent longitudinal studies. Am. J. Ind. Med. 2010, 53, 285–323. [Google Scholar] [CrossRef] [PubMed]
- Punnett, L.; Wegman, D.H. Work-related musculoskeletal disorders: The epidemiologic evidence and the debate. J. Electromyogr. Kinesiol. 2004, 14, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Epstein, S.; Sparer-Fine, E.; Tran, B.; Ruan, Q.; Dennerlein, J.; Singhal, D.; Lee, B. Prevalence of Work-Related Musculoskeletal Disorders Among Surgeons and Interventionalists: A Systematic Review and Meta-analysis. JAMA Surg. 2017, 153, e174947. [Google Scholar] [CrossRef]
- CCOHS—Canadian Centre for Occupational Health and Safety. Work-Related Musculoskeletal-Disorders (WMSDs). Available online: https://www.ccohs.ca/oshanswers/diseases/rmirsi.html (accessed on 16 May 2025).
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2021, 396, 2006–2017. [Google Scholar] [CrossRef]
- EU-OSHA. Les Troubles Musculo-Squelettiques d’Origine Professionnelle: Faits et Chiffres—Rapport de Synthèse Compilé à Partir de 10 Rapports d’États Membres de l’UE. Available online: https://osha.europa.eu/fr/publications/work-related-musculoskeletal-disorders-facts-and-figures-synthesis-report-10-eu-member/view (accessed on 15 November 2024).
- Bhattacharya, A. Costs of occupational musculoskeletal disorders (MSDs) in the United States. Int. J. Ind. Ergon. 2014, 44, 448–454. [Google Scholar] [CrossRef]
- Jacquier-Bret, J.; Gorce, P. Prevalence of Body Area Work-Related Musculoskeletal Disorders among Healthcare Professionals: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 841. [Google Scholar] [CrossRef]
- Ribeiro, T.; Serranheira, F.; Loureiro, H. Work related musculoskeletal disorders in primary health care nurses. Appl. Nurs. Res. 2017, 33, 72–77. [Google Scholar] [CrossRef]
- Vieira, E.R.; Svoboda, S.; Belniak, A.; Brunt, D.; Rose-St Prix, C.; Roberts, L.; da Costa, B.R. Work-related musculoskeletal disorders among physical therapists: An online survey. Disabil. Rehabil. 2016, 38, 552–557. [Google Scholar] [CrossRef] [PubMed]
- Okuyucu, K.; Gyi, D.; Hignett, S.; Doshani, A. Midwives are getting hurt: UK survey of the prevalence and risk factors for developing musculoskeletal symptoms. Midwifery 2019, 79, 102546. [Google Scholar] [CrossRef] [PubMed]
- Kierklo, A.; Kobus, A.; Jaworska, M.M.; Botuliński, B. Work-related musculoskeletal disorders among dentists—A questionnaire survey. Ann. Agric. Environ. Med. 2011, 18, 79–84. [Google Scholar]
- Szeto, G.P.Y.; Ho, P.; Ting, A.C.W.; Poon, J.T.C.; Cheng, S.W.K.; Tsang, R.C.C. Work-related Musculoskeletal Symptoms in Surgeons. J. Occup. Rehabil. 2009, 19, 175–184. [Google Scholar] [CrossRef] [PubMed]
- McLeod, G.A.; Murphy, M.; Henare, T.M.; Dlabik, B. Work-related musculoskeletal injuries among Australian osteopaths: A preliminary investigation. Int. J. Osteopath. Med. 2018, 27, 14–22. [Google Scholar] [CrossRef]
- Choobineh, A.; Movahed, M.; Tabatabaie, S.H.; Kumashiro, M. Perceived demands and musculoskeletal disorders in operating room nurses of Shiraz city hospitals. Ind. Health 2010, 48, 74–84. [Google Scholar] [CrossRef]
- Liang, C.A.; Levine, V.J.; Dusza, S.W.; Hale, E.K.; Nehal, K.S. Musculoskeletal Disorders and Ergonomics in Dermatologic Surgery: A Survey of Mohs Surgeons in 2010. Dermatol. Surg. 2012, 38, 240–248. [Google Scholar] [CrossRef]
- Cromie, J.E.; Robertson, V.J.; Best, M.O. Work-related musculoskeletal disorders in physical therapists: Prevalence, severity, risks, and responses. Phys. Ther. 2000, 80, 336–351. [Google Scholar] [CrossRef]
- Leggat, P.A.; Smith, D.R. Musculoskeletal disorders self-reported by dentists in Queensland, Australia. Aust. Dent. J. 2006, 51, 324–327. [Google Scholar] [CrossRef]
- Vieira, E.R.; Schneider, P.; Guidera, C.; Gadotti, I.C.; Brunt, D. Work-related musculoskeletal disorders among physical therapists: A systematic review. J. Back Musculoskelet. Rehabil. 2016, 29, 417–428. [Google Scholar] [CrossRef]
- Marciano, F.; Mattogno, P.P.; Codenotti, A.; Cocca, P.; Fontanella, M.M.; Doglietto, F. Work-related musculoskeletal disorders among endoscopic transsphenoidal surgeons: A systematic review of prevalence and ergonomic interventions. Int. J. Occup. Saf. Ergon. 2022, 28, 459–468. [Google Scholar] [CrossRef]
- Halkai, K.R.; Halkai, R.S.; Sulgante, S.; Sanadi, R.M.; Ara, S.A.; Zainab, H.; Kuriadom, S.T.; Munaga, S.; Chitumalla, R. Work-related musculoskeletal disorders among dentists and their prevention through ergonomic interventions—A systematic review. Int. J. Occup. Saf. Health 2022, 12, 125–139. [Google Scholar] [CrossRef]
- Soylar, P.; Ozer, A. Evaluation of the prevalence of musculoskeletal disorders in nurses: A systematic review. Med. Sci. 2018, 7, 1. [Google Scholar] [CrossRef]
- Soroush, A.; Shamsi, M.; Izadi, N.; Heydarpour, B.; Samadzadeh, S.; Shahmohammadi, A. Musculoskeletal Disorders as Common Problems among Iranian Nurses: A Systematic Review and Meta-analysis Study. Int. J. Prev. Med. 2018, 9, 27. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Zeng, X.; Li, J.; Guo, Y.; Wang, Z. The prevalence and risk factors of work-related musculoskeletal disorders among nurses in China: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2024, 157, 104826. [Google Scholar] [CrossRef] [PubMed]
- Gorce, P.; Jacquier-Bret, J. Work-Related Musculoskeletal Disorder Prevalence by Body Area Among Nurses in Europe: Systematic Review and Meta-Analysis. J. Funct. Morphol. Kinesiol. 2025, 10, 66. [Google Scholar] [CrossRef]
- Jacquier-Bret, J.; Gorce, P. Work-Related Musculoskeletal Disorder Prevalence by Body Area Among Nurses in Asia: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2025, 22, 652. [Google Scholar] [CrossRef]
- Kgakge, K.; Hlongwa, M.; Nwagbara, U.I.; Ginindza, T. The distribution of work-related musculoskeletal disorders among nurses in sub-Saharan Africa: A scoping review. Syst. Rev. 2024, 13, 273. [Google Scholar] [CrossRef]
- Aremu, A.B.; Afolabi, I.B.; Odongo, O.A.; Shehzad, S.; Khan, K.S. Prevalence of musculoskeletal disorders among healthcare professionals in Africa: A systematic review and meta-analysis. Available Res. Sq. 2023. [Google Scholar] [CrossRef]
- Gorce, P.; Jacquier-Bret, J. Work-Related Musculoskeletal Disorders Prevalence among American, Asian, and European Surgeons during Robotic/Video-Assisted Surgery. Int. J. Phys. Med. Rehabil. 2023, 11, 689. [Google Scholar]
- Sun, W.; Yin, L.; Zhang, T.; Zhang, H.; Zhang, R.; Cai, W. Prevalence of Work-Related Musculoskeletal Disorders among Nurses: A Meta-Analysis. Iran. J. Public Health 2023, 52, 463–475. [Google Scholar] [CrossRef]
- Chenna, D.; Pentapati, K.C.; Kumar, M.; Madi, M.; Siddiq, H. Prevalence of musculoskeletal disorders among dental healthcare providers: A systematic review and meta-analysis. F1000Res 2022, 16, 1062. [Google Scholar] [CrossRef]
- Gorce, P.; Jacquier-Bret, J. Effect of Assisted Surgery on Work-Related Musculoskeletal Disorder Prevalence by Body Area among Surgeons: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 6419. [Google Scholar] [CrossRef]
- Gorce, P.; Jacquier-Bret, J. Global prevalence of musculoskeletal disorders among physiotherapists: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2023, 24, 265. [Google Scholar] [CrossRef]
- Pan, J.; Wang, M.C.; Zhao, S.Y.; Liu, Q.; Zhai, H.Y. A meta-analysis of the prevalence of work-related musculoskeletal disorders among rehabilitation therapists. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2024, 42, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Morgan, R.L.; Whaley, P.; Thayer, K.A.; Schünemann, H.J. Identifying the PECO: A framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ. Int. 2018, 121, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Erg. 1987, 18, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Hermanson, J.E.; Choi, S.D. Study of musculoskeletal risks of the office-based surgeries. Work 2012, 41, 1940–1943. [Google Scholar] [CrossRef]
- Lunny, C.; Pieper, D.; Thabet, P.; Kanji, S. Managing overlap of primary study results across systematic reviews: Practical considerations for authors of overviews of reviews. BMC Med. Res. Methodol. 2021, 21, 140. [Google Scholar] [CrossRef]
- Hennessy, E.A.; Johnson, B.T. Examining overlap of included studies in meta-reviews: Guidance for using the corrected covered area index. Res. Synth. Methods 2020, 11, 134–145. [Google Scholar] [CrossRef]
- Pieper, D.; Antoine, S.L.; Mathes, T.; Neugebauer, E.A.; Eikermann, M. Systematic review finds overlapping reviews were not mentioned in every other overview. J. Clin. Epidemiol. 2014, 67, 368–375. [Google Scholar] [CrossRef]
- Pérez-Bracchiglione, J.; Meza, N.; Bangdiwala, S.I.; Niño de Guzmán, E.; Urrútia, G.; Bonfill, X.; Madrid, E. Graphical Representation of Overlap for OVErviews: GROOVE tool. Res. Synth. Methods. 2022, 13, 381–388. [Google Scholar] [CrossRef]
- Chys, M.; De Meulemeester, K.; De Greef, I.; Murillo, C.; Kindt, W.; Kouzouz, Y.; Lescroart, B.; Cagnie, B. Clinical Effectiveness of Dry Needling in Patients with Musculoskeletal Pain—An Umbrella Review. J. Clin. Med. 2023, 12, 1205. [Google Scholar] [CrossRef] [PubMed]
- Neyeloff, J.L.; Fuchs, S.C.; Moreira, L.B. Meta-analyses and Forest plots using a microsoft excel spreadsheet: Step-by-step guide focusing on descriptive data analysis. BMC Res. Notes 2012, 5, 52. [Google Scholar] [CrossRef] [PubMed]
- Cochrane Training. Cochrane Handbook for Systematic Reviews of Interventions. Available online: https://training.cochrane.org/handbook/archive/v6/chapter-10#section-10-10-2 (accessed on 2 February 2022).
- Al Amer, H.S. Low back pain prevalence and risk factors among health workers in Saudi Arabia: A systematic review and meta-analysis. J. Occup. Health 2020, 62, e12155. [Google Scholar] [CrossRef]
- Kasa, A.S.; Workineh, Y.; Ayalew, E.; Temesgen, W.A. Low back pain among nurses working in clinical settings of Africa: Systematic review and meta-analysis of 19 years of studies. BMC Musculoskelet. Disord. 2020, 21, 310. [Google Scholar] [CrossRef]
- Saberipour, B.; Ghanbari, S.; Zarea, K.; Gheibizadeh, M.; Zahedian, M. Investigating prevalence of musculoskeletal disorders among Iranian nurses: A systematic review and meta-analysis. Clin. Epidemiol. Glob. Health 2019, 7, 513–518. [Google Scholar] [CrossRef]
- ZakerJafari, H.R.; YektaKooshali, M.H. Work-Related Musculoskeletal Disorders in Iranian Dentists: A Systematic Review and Meta-analysis. Saf. Health Work 2018, 9, 1–9. [Google Scholar] [CrossRef]
- Tahernejad, A.; Makki, F.; Rezaei, E.; Marzban, H.; Tahernejad, S.; Sahebi, A. Musculoskeletal disorders in emergency medi-cal services personnel: A systematic review and meta-analysis. Public Health 2024, 237, 107–115. [Google Scholar] [CrossRef]
- Bozic, A.; Gajdobranski, D.; Brestovacki-Svitlica, B.; Medic-Pericevic, S.; Mikov, M.; Vasovic, V.; Mikov, I. The prevalence of low back pain among nurses in Serbia. Work 2022, 71, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Gaowgzeh, R.A.; Chevidikunnan, M.F.; Al Saif, A.; El-Gendy, S.; Karrouf, G.; Al Senany, S. Prevalence of and risk factors for low back pain among dentists. J. Phys. Ther. Sci. 2015, 27, 2803–2806. [Google Scholar] [CrossRef]
- Takrouni, H.A.; Mousa, G.; Yaseen, K.M.; Alshehri, M.A. Work-Related Low Back Pain Among Physical Therapists in the Makkah Region, Saudi Arabia: A Cross-Sectional Study. Healthcare 2025, 13, 309. [Google Scholar] [CrossRef]
- Mohseni-Bandpei, M.A.; Ahmad-Shirvani, M.; Golbabaei, N.; Behtash, H.; Shahinfar, Z.; Fernández-de-las-Peñas, C. Prevalence and risk factors associated with low back pain in Iranian surgeons. J. Manipulative Physiol. Ther. 2011, 34, 362–370. [Google Scholar] [CrossRef]
- Acharya, H.; Patel, P.; Shetty, G.M.; Shah, M.; Bamb, H.; Nene, A. Prevalence and risk factors of neck pain in spine surgeons - Are we our own patients? J. Clin. Orthop. Trauma 2022, 5, 102012. [Google Scholar] [CrossRef] [PubMed]
- Kawtharani, A.A.; Msheik, A.; Salman, F.; Haj Younes, A.; Chemeisani, A. A Survey of Neck Pain among Dentists of the Lebanese Community. Pain Res. Manag. 2023, 23, 8528028. [Google Scholar] [CrossRef] [PubMed]
- Lövgren, M.; Gustavsson, P.; Melin, B.; Rudman, A. Neck/shoulder and back pain in new graduate nurses: A growth mixture modeling analysis. Int. J. Nurs. Stud. 2014, 51, 625–639. [Google Scholar] [CrossRef] [PubMed]
- Almogbil, I.H.; Alrashidi, L.R.; Alhajlah, R.S.; Alqasim, A.K.; Alharbi, N.S.; Alghamdi, M.A.; Alshahrani, A.H. Prevalence of Shoulder and Neck Pain Among Healthcare Workers in the Central Region of Saudi Arabia. Cureus 2023, 15, e42286. [Google Scholar] [CrossRef]
- Suedbeck, J.R.; O’Connor, T.; Ludwig, E.A.; Bradshaw, B. The effects of static seated and standing positions on posture in dental hygiene students: A pilot study. Can. J. Dent. Hyg. 2023, 57, 172–179. [Google Scholar]
- Toffola, E.D.; Rodigari, A.; Di Natali, G.; Ferrari, S.; Mazzacane, B. Posture and fatigue among surgeons in the operating room. G. Ital. Med. Lav. Ergon. 2009, 31, 414–418. [Google Scholar]
- Chang, H.E.; Cho, S.H. Nurses’ steps, distance traveled, and perceived physical demands in a three-shift schedule. Hum. Resour. Health 2022, 20, 72. [Google Scholar] [CrossRef]





| Database | Search Keyword Combinations | Applied Filters |
|---|---|---|
| Mendeley | musculoskeletal disorder AND (healthcare professional OR surgeon OR nurse OR physiotherapist OR dentist OR midwife OR physical therapist) AND meta-analysis | None |
| PubMed/MedLine | musculoskeletal disorder AND (healthcare professional OR surgeon OR nurse OR physiotherapist OR dentist OR midwife OR physical therapist) AND meta-analysis | Article type: Meta-Analysis Article language: English |
| Science.gov | musculoskeletal disorder AND (healthcare professional OR surgeon OR nurse OR physiotherapist OR dentist OR midwife OR physical therapist) AND meta-analysis | Top results |
| ScienceDirect | musculoskeletal disorder AND (healthcare professional OR surgeon OR nurse OR physiotherapist OR dentist OR midwife OR physical therapist) AND meta-analysis | Article type: Review articles Languages: English |
| Google Scholar | “meta-analysis” prevalence “systematic review”“body area” healthcare OR professional OR surgeon OR nurse OR physiotherapist OR dentist OR midwife OR physical therapist “work-related musculoskeletal disorders” | None |
| Authors | Country | Number of Studies | Sample Size | Healthcare Profession | Age of Participants | Context of this Study | ||
|---|---|---|---|---|---|---|---|---|
| Continent | Number of Studies | Number of Countries | ||||||
| Africa | ||||||||
| Aremu et al., 2023 [31] | Uganda | 18 | 4486 | Healthcare professionals | 30–40 | Africa | 18 | 12 |
| Kasa et al., 2020 [50] | Ethiopia | 19 | 6110 | Nurses | - | Africa | 19 | 11 |
| America | ||||||||
| Gorce et al., 2023 [32] | France | 17 | 4935 | Surgeons | 46.5 ± 4.2 | America | 17 | 2 |
| Asia | ||||||||
| Al Amer 2020 [49] | Saudi Arabia | 18 | 5345 | Healthcare professionals | 23.7 ± 1.6 | Asia | 18 | 1 |
| Gorce et al., 2023 [32] | France | 4 | 628 | Surgeons | 39.9 ± 4.8 | Asia | 4 | 3 |
| Jacquier-Bret et al., 2025 [29] | France | 40 | 19,903 | Nurses | 31.3 ± 3.4 | Asia | 40 | 10 |
| Saberipour et al., 2019 [51] | Iran | 33 | 11,995 | Nurses | - | Asia | 33 | 1 |
| Soroush et al., 2018 [26] | Iran | 41 | 16,350 | Nurses | 33.09 | Asia | 41 | 1 |
| Wang et al., 2024 [27] | China | 23 | 21,042 | Nurses | 22–60 | Asia | 23 | 1 |
| Zakerjafari et al., 2018 [52] | Iran | 23 | 2531 | Dentists | 27.4–42.2 | Asia | 23 | 1 |
| Europe | ||||||||
| Gorce et al., 2023 [32] | France | 12 | 1733 | Surgeons | 44.2 ± 5.9 | Europe | 12 | 9 |
| Gorce et al., 2025 [28] | France | 12 | 5153 | Nurses | 27.9–47.6 | Europe | 12 | 7 |
| Authors | WMSD Prevalence by Body Area | WMSD Overall | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Neck | Upper Back | Lower Back | Shoulder | Elbow | Wrist | Hip | Knee | Ankle | |||
| Africa | |||||||||||
| Aremu et al., 2023 [31] | Prev. (%) | 27.9% | 22.7% | 44.8% | 23.7% | 6.5% | 20.9% | 9.2% | 18.1% | 14.6% | - |
| Nb studies | 17—He | 16—He | 16—He | 17—He | 16—He | 18—He | 17—He | 16—He | 17—He | - | |
| Nb subjects | 4283 | 3930 | 3930 | 4283 | 3930 | 4486 | 3930 | 3930 | 3930 | - | |
| Kasa et al., 2020 [50] | Prev. (%) | - | - | 64.1% | - | - | - | - | - | - | - |
| Nb studies | - | - | 19—He | - | - | - | - | - | - | - | |
| Nb subjects | - | - | 6110 | - | - | - | - | - | - | - | |
| America | |||||||||||
| Gorce et al., 2023 [32] | Prev. (%) | 39.3% | - | - | 36.0% | - | 27.2% | - | - | - | - |
| Nb studies | 17—He | - | - | 13—He | - | 16—He | - | - | - | - | |
| Nb subjects | 4935 | - | - | 3528 | - | 4554 | - | - | - | - | |
| Asia | |||||||||||
| Al Amer 2020 [49] | Prev. (%) | - | - | 65.0% | - | - | - | - | - | - | - |
| Nb studies | - | - | 15—He | - | - | - | - | - | - | - | |
| Nb subjects | - | - | 4032 | - | - | - | - | - | - | - | |
| Gorce et al., 2023 [32] | Prev. (%) | 50.4% | - | - | 35.6% | - | 25.8% | - | - | - | - |
| Nb studies | 4—He | - | - | 4—He | - | 3—He | - | - | - | - | |
| Nb subjects | 628 | - | - | 628 | - | 493 | - | - | - | - | |
| Jacquier-Bret et al., 2025 [29] | Prev. (%) | 45.7% | 34.1% | 58.4% | 43.0% | 14.9% | 32.2% | 22.5% | 40.7% | 33.4% | 84.3% |
| Nb studies | 39—He | 32—He | 38—He | 37—He | 33—He | 32—He | 30—He | 35—He | 33—He | 29—He | |
| Nb subjects | 19,306 | 15,331 | 19,186 | 18,666 | 17,160 | 16,932 | 16,477 | 17,800 | 17,160 | 16,145 | |
| Saberipouret al., 2019 [51] | Prev. (%) | - | - | 60.5% | - | - | - | - | - | - | 84.2% |
| Nb studies | - | - | 31—He | - | - | - | - | - | - | 14—He | |
| Nb subjects | - | - | 11,743 | - | - | - | - | - | - | 4490 | |
| Soroush et al., 2018 [26] | Prev. (%) | 47.8% | 44.6% | 61.0% | 42.8% | 17.5% | 36.8% | 24.6% | 46.5% | 43.7% | - |
| Nb studies | 25—He | 17—He | 38—He | 16—He | 17—He | 16—He | 12—He | 21—He | 13—He | - | |
| Nb subjects | 9137 | 6079 | 15,835 | 5452 | 6555 | 5619 | 4420 | 7728 | 4525 | - | |
| Wang et al., 2024 [27] | Prev. (%) | 58.0% | - | 35.0% | 49.0% | 15.0% | 25.0% | 21.0% | 31.0% | 30.0% | 79.0% |
| Nb studies | 16—He | - | 17—He | 16—He | 16—He | 16—He | 14—He | 16—He | 15—He | 19—He | |
| Nb subjects | - | - | - | - | - | - | - | - | - | 21,042 | |
| Zakerjafariet al., 2018 [52] | Prev. (%) | 51.9% | - | 37.3% | 33.2% | 12.9% | 33.7% | 11.9% | 17.6% | 12.9% | - |
| Nb studies | 21—He | - | 18—He | 17—He | 11—He | 18—He | 11—He | 11—He | 8—He | - | |
| Nb subjects | 2371 | - | 1500 | 1954 | 898 | 2053 | 854 | 852 | 643 | - | |
| Europe | |||||||||||
| Gorce et al., 2023 [32] | Prev. (%) | 54.1% | - | - | 51.4% | - | 31.8% | - | - | - | - |
| Nb studies | 10—He | - | - | 10—He | - | 6—He | - | - | - | - | |
| Nb subjects | 1540 | - | - | 1634 | - | 694 | - | - | - | - | |
| Gorce et al., 2025 [28] | Prev. (%) | 49.9% | 46.3% | 61.4% | 39.3% | 13.4% | 32.3% | 20.8% | 36.6% | 24.7% | 87.8% |
| Nb studies | 11—He | 6—He | 12—He | 12—He | 7—He | 10—He | 6—He | 9—He | 9—He | 10—He | |
| Nb subjects | 3757 | 2778 | 5153 | 5153 | 3070 | 4451 | 2849 | 3526 | 4230 | 3877 | |
| Ranking | Asia | Europe |
|---|---|---|
| 1 | Lower back (56.6%) | Neck (51.7%) |
| 2 | Neck (48.4%) | Shoulder (43.5%) |
| 3 | Upper back (39.3%) | Wrist (32.2%) |
| 4 | Shoulder (38.9%) | |
| 5 | Knee (35.0%) | |
| 6 | Wrist (32.6%) | |
| 7 | Ankle (30.1%) | |
| 8 | Hip (19.8%) | |
| 9 | Elbow (15.3%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gorce, P.; Jacquier-Bret, J. Continental Umbrella Review and Meta-Analysis of Work-Related Musculoskeletal Disorders Prevalence Among Healthcare Professionals. Theor. Appl. Ergon. 2025, 1, 7. https://doi.org/10.3390/tae1010007
Gorce P, Jacquier-Bret J. Continental Umbrella Review and Meta-Analysis of Work-Related Musculoskeletal Disorders Prevalence Among Healthcare Professionals. Theoretical and Applied Ergonomics. 2025; 1(1):7. https://doi.org/10.3390/tae1010007
Chicago/Turabian StyleGorce, Philippe, and Julien Jacquier-Bret. 2025. "Continental Umbrella Review and Meta-Analysis of Work-Related Musculoskeletal Disorders Prevalence Among Healthcare Professionals" Theoretical and Applied Ergonomics 1, no. 1: 7. https://doi.org/10.3390/tae1010007
APA StyleGorce, P., & Jacquier-Bret, J. (2025). Continental Umbrella Review and Meta-Analysis of Work-Related Musculoskeletal Disorders Prevalence Among Healthcare Professionals. Theoretical and Applied Ergonomics, 1(1), 7. https://doi.org/10.3390/tae1010007







