Abstract
Dementia significantly impacts cognitive, behavioral, and functional abilities, creating challenges for both individuals and caregivers. Recent advancements in HCI have introduced innovative technological solutions to support people with dementia (PwD) and their caregivers. This scoping review systematically examines 32 recent publications from leading digital libraries, categorizing technological interventions into four key domains: Assistive and Smart Technology for Daily Life, Social Interaction and Communication, Well-being and Psychological Support, and Caregiver Support and Training. Our analysis highlights how emerging technologies are transforming dementia care. These technologies enhance quality of life by promoting independence, fostering social engagement, and providing emotional and cognitive support. However, the review also identifies critical gaps, particularly in addressing the needs of individuals with early-stage dementia and the lack of individualized support mechanisms. By emphasizing user-centered design, accessibility, and ethical considerations, this paper offers a structured roadmap for future research and practice in dementia care. It bridges the gap between technological innovation and the real-world needs of PwD and their caregivers, providing valuable insights for researchers, practitioners, and policymakers. This review not only synthesizes current advancements but also sets the stage for future HCI-driven innovations in dementia care, aiming to improve outcomes for an aging global population. Findings primarily reflect older adults; implications for early-onset dementia are discussed.
1. Introduction
Dementia, a progressive neurological condition characterized by cognitive decline, behavioral changes, and functional impairments, represents a significant and growing global health challenge [1]. As the global population ages, the prevalence of dementia continues to rise, placing increasing demands on healthcare systems and caregivers. The gradual loss of memory, cognitive abilities, and emotional and social functioning profoundly impacts the daily lives of people with dementia (PwD) and their informal caregivers, significantly diminishing their overall quality of life [2]. While advancing age is a well-established risk factor, it is critical to recognize that dementia is not an inevitable consequence of aging [1]. Instead, it is a complex and multifaceted condition that demands innovative approaches to early detection, care, and support.
Recent advancements in artificial intelligence (AI) and wearable technologies [3] have revolutionized the early-stage diagnosis of dementia. By analyzing diverse patient data, such as brain imaging, speech patterns, facial expressions, movement, and sleep behavior, these technologies offer promising tools for identifying dementia in its initial stages [4,5]. However, the challenges of dementia care extend far beyond diagnosis. Providing effective care for PwD involves addressing their physical, emotional, and social needs while also supporting their caregivers, who often lack the necessary training and resources. Informal caregivers—typically family members—face substantial emotional and financial burdens, underscoring the need for accessible support. In this review, we use carer/caregiver to include both informal (family/friends, unpaid) and formal (paid) carers, and we consider technologies deployed across home/community, residential aged care/long-term care (LTC), outpatient/clinic, and hospital/acute settings.
Assistive technologies, including monitoring systems, cognitive therapies, and daily living support tools, have demonstrated significant potential in enhancing dementia care [6,7]. For instance, wearable devices equipped with advanced sensors enable continuous monitoring of daily activities, providing valuable insights into the behavior and care patterns of PwD [8]. Mobile health applications extend healthcare support, improving the well-being of PwD [9], while interactive entertainment systems foster engagement and independence, enhancing their quality of life [10]. However, the integration of these technologies into dementia care raises important ethical considerations, particularly regarding the stigmatization and disempowerment of PwD. Researchers in human–computer interaction (HCI) emphasize the need for tailored technologies that prioritize the voices and preferences of PwD, rather than viewing dementia solely through a medical lens as a problem to be “solved” [11,12].
While existing review papers, such as those by Dada et al. [13] and Koo et al. [14], have explored smart health technologies and mobile solutions for dementia care, they often focus on specific aspects of technology, such as monitoring or caregiver support. In contrast, this paper adopts a broader perspective, synthesizing advancements across multiple dimensions of dementia care technologies over the past five years (2020–2024). By categorizing these technologies into four thematic areas—Assistive and Smart Technology for Daily Life, Social Interaction and Communication, Well-being and Psychological Support, and Caregiver Support and Training—we aim to provide a comprehensive roadmap for researchers and practitioners in the field.
Furthermore, this review emphasizes the ethical and human-centered considerations in developing technologies for PwD, aligning with the critical dementia perspective [11]. Unlike previous reviews that primarily focus on technological capabilities, this paper focuses specifically on tailoring solutions to the unique needs and preferences of PwD and their caregivers. By systematically mapping the existing literature from authoritative sources such as PubMed, Web of Science (WOS), Scopus, ACM, and IEEE, we offer a nuanced understanding of how technology can bridge gaps in dementia care while addressing the ethical and practical challenges associated with its implementation.
This review paper contributes to the growing body of knowledge on dementia care technologies by providing a holistic and up-to-date synthesis of advancements in the field. It not only builds on existing research but also identifies emerging trends and gaps, offering insights for future innovation. By focusing on both technological advancements and ethical considerations, this paper aims to enrich the experiences of PwD and their caregivers, ultimately improving the quality of dementia care in an aging world. While our corpus predominantly features studies with older adults, we explicitly consider transferability to early-onset/young-onset dementia (EOD/YOD), highlighting where needs diverge (e.g., employment, parenting, stigma) and where evidence is lacking. We mark EOD/YOD coverage in tables and revisit generalizability in the Discussion.
2. Method
Our literature review follows the PICO (Patients, Intervention, Comparison, and Outcome) framework [15], with a focus on individuals with dementia (PwD) and their caregivers. We conducted our search within the PubMed, Web of Science (WOS), Scopus, ACM, and IEEE Digital Libraries, covering research published between 2020 and 2024 to capture the most recent advancements. The Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines [16] informed our process, which consisted of four stages: identification, screening, eligibility, and inclusion. Figure 1 illustrates this selection process, detailing the criteria applied at each stage. In this section, we formulate two research questions to guide our review process. These questions serve as the foundation for our systematic literature search, ensuring alignment with the key aspects of technology in dementia care. Subsequently, we outline our approach to the publication search process, illustrating how it corresponds to these research questions.
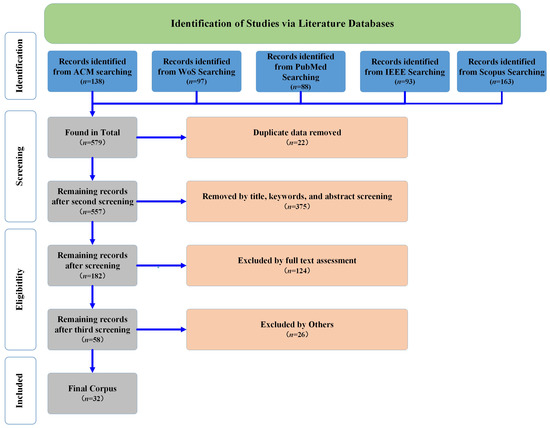
Figure 1.
Overview of review methodology presented on the PRISMA flow chart.
2.1. Reporting Standards and Compliance
This review was carried out according to the PRISMA-ScR guidelines [17], which provide a standardized framework to ensure transparency and reproducibility in scoping reviews. Our review protocol was not prospectively registered with PRISMA, and we explicitly acknowledge this in compliance with reporting requirements. Although the PRISMA methodology informed the identification and selection of relevant studies, the subsequent corpus analysis was primarily guided by thematic analysis and collaborative group discussions, which enabled us to synthesize the findings and establish the thematic categories presented in this review.
To enhance clarity and accessibility, we also provide a graphical abstract (GA) that visually summarizes the scope and methodology of our study. The GA illustrates the central role of technology-based interventions in dementia care, their impact on both people living with dementia (PwD) and their caregivers, and the structured PRISMA-based selection process that guided our literature review. Designed to be self-explanatory, GA allows readers to quickly grasp the core contributions and relevance of our work.
2.2. Research Question
As previously mentioned, dementia care aims to enhance the lives of individuals with dementia and the well-being of their caregivers. To explore how ongoing technologies are employed in the field of dementia care, we formulated the following two research questions:
- RQ1: Which technology-based dementia care strategies can effectively improve the quality of life for people living with dementia?
- RQ2: Which technology-based stress-coping approaches can significantly alleviate the stress and distress experienced by caregivers of people living with dementia?
Integrated dementia care models (e.g., collaborative care [18], case management [19], and memory-clinic–anchored networks [20]) consistently show benefits for people with dementia (PwD) and caregivers, including reduced neuropsychiatric symptoms, improved caregiver burden and quality of life, and fewer avoidable transitions. Notably, integrated care mitigates what health services research calls the diagnostic odyssey—repeated, fragmented consultations across siloed services—thereby reducing time-to-diagnosis, duplicative testing, and “provider ping-pong.” Because “wandering” also denotes a behavioral symptom in dementia, we avoid the term medical wandering to prevent confusion [21]. In this review we therefore treat care integration as a first-order determinant of quality of life and explicitly tag included interventions by their integration level (e.g., single-point vs networked care), reporting quality of life and utilization outcomes when available.
Emerging technologies, such as AI [22], wearable devices [23], and robotics [24,25], hold promise in revolutionizing dementia care and support. To address RQ1, we explored keywords such as “technology-based,” “dementia care,” “older people with dementia,” and “quality of life” in our literature searches. We extracted whether each study incorporated cross-organizational coordination (e.g., shared care plans, case management) and, when reported, any effects on time-to-diagnosis, service duplication, or unplanned utilization.
Our exploration also extends to technologies that provide essential assistance to caregivers, who often bear significant emotional and financial burdens. To address RQ2, we used keywords such as “dementia caregivers” and “technology-based” to identify innovative ways of supporting and empowering this population.
2.3. Search Strategy
In our literature research strategy, we operationalized the PICO framework [15] using conventional Boolean and controlled-vocabulary (MeSH/Emtree) strategies [15]. Term lists for the population, intervention and outcomes were developed collaboratively through coauthor brainstorming, manual review of sentinel articles, and thesaurus consultation. We then used AI tools (GPT-4o) solely to suggest additional English-language synonyms and phrasings for our predefined PICO concepts; all AI suggestions were manually vetted before inclusion. No AI was used for translation, similarity search, screening, or data extraction. Searches were complemented by hand snowballing (backward/forward citation chasing), de-duplication via DOI/PMID and manual title checks, and dual-reviewer screening with consensus resolution. The final query strings and the PRISMA flow diagram are as follows.
- ■
- Person/Population (P): This category included keywords related to the elderly population, such as “Elderly”, “Seniors”, “Older Adults”, “Older People”, “Older Population”, “Geriatric”, and “Aging Population”. These terms ensured that our review captured literature specifically addressing the dementia healthcare needs of older adults, particularly those living with dementia.
- ■
- Intervention/Indicator (I): This category focused on keywords related to interactive technologies. We used terms such as “Technology-based interventions”, “Assistive technology”, “Digital health tools”, “Smart home technology”, “Wearable devices”, “Telehealth in dementia care”, “Artificial intelligence in dementia”, “Computer Vision”, “Mobile apps for dementia”, “Virtual reality dementia therapy”, “Robotic”, “Mobile app”, “Virtual reality”, “Telehealth”, “Interactive Technology”, “Digital Health Technologies”, and “Robot*”. These keywords allowed us to capture the wide range of interactive applications designed to support dementia care settings.
- ■
- Comparison/Control/Context (C): To contextualize the role of interactive technologies within healthcare, we used terms such as “dementia care” and “dementia healthcare”. These keywords ensured that our review remained focused on how interactive technologies impact dementia healthcare delivery, care quality, and outcomes for the elderly.
- ■
- Outcome (O): This category focused on keywords related to the enhancement of elderly healthcare. We used terms like “Enhanced Healthcare”, “Healthcare Improvement”, “Health Enhancement”, “Improved Health Outcomes”, “Better Quality of Life”, “Effective Health Monitoring”, and “Cognitive Support”. These terms helped us identify studies that explored how interactive technologies contribute to improving health outcomes and quality of life for PwD.
By organizing our search terms into these four categories, the PICO framework allowed us to conduct a highly focused and efficient literature search. This approach ensured that our review systematically addressed the research questions by covering the relevant population (PwD), interventions (interactive technologies), comparisons (dementia care contexts), and outcomes (improved healthcare and quality of life). As a result, the PICO strategy played a pivotal role in shaping the scope and direction of our literature review, enabling us to identify and analyze the most relevant studies in the field.
2.4. Literature Selection
Our aim is to provide an up-to-date and comprehensive analysis of recent advances in the field of interactive technologies within the context of dementia care, with a particular focus on research published over the past five years (2020–2024). To achieve this objective, we used a scoping review methodology, a robust approach that enables us to synthesize research findings, map the scope and nature of emerging research areas, and identify potential avenues for future investigations [26].
Throughout our literature collection and selection process, we adhered to the Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines [16] and the Meta-Analyzes Extension for Scoping Reviews (PRISMA-ScR) framework [17,27], both widely recognized methodologies for the construction of comprehensive review articles. These frameworks ensured a rigorous, transparent and systematic approach to our review process.
As illustrated in Figure 1, our literature selection process unfolded in four iterative stages: data collection, initial filtering, research question exclusion, and full-text selection. To commence our study, we identified pertinent search terms based on our existing knowledge and executed a systematic query across five esteemed databases—PubMed, Web of Science (WoS), Scopus, ACM Digital Library, and IEEE Xplore. These databases were selected for their extensive repositories of high-quality, peer-reviewed literature, ensuring access to the most relevant and up-to-date research in the field.
2.4.1. Identification
During the identification process, we utilized the aforementioned keywords to search the PubMed, WoS, Scopus, ACM, and IEEE libraries. These repositories were chosen for their comprehensive collections of literature relevant to our research objectives. Focusing on the years 2020–2024 ensured that our search yielded the most current and relevant publications. Our search retrieved 138 publications from ACM, 97 from WOS, 88 from PubMed, 93 from IEEE, and 163 from Scopus, resulting in a total of 579 relevant pieces of literature.
2.4.2. Screening
Two reviewers independently screened titles/abstracts; potentially eligible articles underwent full-text assessment against the criteria above. Disagreements were resolved by discussion (third reviewer available). Reasons for exclusion at full text are shown in Figure 1 (PRISMA-ScR flow). Articles were retained for full-text review when they met all of the following inclusion criteria:
- (i)
- Peer-reviewed, full-text article in English.
- (ii)
- Pertains to dementia care.
- (iii)
- Participants or target users include people living with dementia and/or their carers (informal family/friends or formal paid carers).
- (iv)
- Describes, prototypes, or evaluates an HCI technology intended to support daily life (e.g., monitoring, support, social/communication, well-being).
- (v)
- Addresses at least one of our research questions (RQ1 or RQ2).
- Exclusion criteria. We focused on original empirical studies (qualitative, quantitative, or mixed-methods), including lab, field, pilot/feasibility, quasi-experimental, and randomized designs. We excluded:
- Systematic and scoping reviews, meta-analyses, editorials, commentaries, protocols, theses, and patents. However, the reference lists of systematic and scoping reviews and meta-analyses were screened to identify relevant primary studies.
- Papers that did not focus on dementia or on carers of people with dementia.
- Purely technical or algorithmic papers lacking user evaluation or clear relevance to care (e.g., detection-only studies).
- Non-English full-text papers and animal studies, if encountered.
- Screening flow (titles/abstracts). Prior to screening, we removed 22 duplicate records. During screening, we applied the criteria above and pragmatically allowed wording variants in titles/abstracts (e.g., “older adults with memory problems”), provided that the full text explicitly linked the work to dementia care. We excluded 375 records at this stage (including review articles and papers reporting only initial designs, technical developments, or detection algorithms), leaving 182 records for further evaluation.
2.4.3. Eligibility
During the eligibility stage, the same two authors assessed the full text of the remaining papers. We excluded papers that, while mentioning dementia care, primarily focused on unrelated research directions or technical developments. We also evaluated whether the technologies or designs presented could benefit PwD or their caregivers. Short papers, such as those from CHI Late-Breaking Work, were included if they addressed RQ1 or RQ2 and involved relevant participants. A total of 124 papers were excluded during this stage, resulting in 58 records.
The final corpus consisted of 32 papers, each thoroughly reviewed and aligned with our research objectives. To ensure consistency, the authors exchanged their assigned tasks and held regular discussions to resolve any uncertainties. This collaborative approach ensured a rigorous and unbiased selection process.
Additionally, in this paper, we use carer/caregiver to refer to both informal carers (family members or friends) and formal carers (care workers, nurses, allied health professionals). Throughout, “healthcare” denotes services delivered across home/community, residential aged care/long-term caring, outpatient/clinic, and hospital/acute, or mixed settings. Moreover, we treated quality of life as a multidimensional, person-centred construct comprising psychological well-being, social connection, functional autonomy, and symptom burden. Where available, we recorded validated instruments (e.g., QoL-AD, DEMQOL/QUALID) and mapped proxy measures (e.g., engagement, affect) to these dimensions.
2.4.4. Corpus Management Under Heavy-Tailed Growth
Digital-health and HCI outputs are expanding rapidly and are dispersed across many venues. To keep the synthesis contemporary and tractable, we restricted inclusion to the five most recent publication years (2020–2024). We combined broad database queries with forward and backward citation chasing from sentinel papers. We monitored diminishing returns during screening and halted snowballing when ten consecutive newly identified records yielded no additional eligible studies. We also reviewed the mix of included studies by outlet and publication year qualitatively to avoid unintended clustering toward a small set of venues. Moreover, we treated quality of life as a multidimensional, person-centred construct encompassing psychological well-being, social connection, functional autonomy, and symptom burden. Where available, we recorded validated instruments (e.g., QoL-AD, DEMQOL/QUALID) and mapped proxy measures (engagement, affect) to these dimensions.
2.5. Data Extraction and Synthesis
Data extraction was performed manually using a standardized template piloted on a small subset of papers. Two authors independently extracted study-level fields (participants, setting, technology, study design, outcomes, and care-integration features), compared results, and resolved discrepancies by discussion; a third author adjudicated unresolved cases. We maintained an audit trail of extraction decisions. No AI systems were used for data extraction, coding, clustering, or analysis.
To synthesize and analyze the included literature, we employed reflexive thematic analysis [28]. Rather than maintaining a fixed a priori codebook, we used an iterative framework-matrix and analytic memoing workflow: initial open codes were generated independently by two co-authors, consolidated through calibration meetings, and then organized into a living framework matrix that captured working code labels, operational notes, anchor examples, and inclusion/exclusion rules. The matrix evolved alongside the analysis and was versioned to preserve an audit trail.
The coding followed a hybrid strategy:
- Descriptive coding: Capture of study attributes, including technology type (e.g., conversational agents, robotics, sensing), participant groups (e.g., people with dementia, caregivers, clinicians), study context (e.g., home, long-term care, clinic), and study design (e.g., pilot, randomized trial, field deployment).
- Analytical coding: Development of higher-order themes such as modes of human–technology interaction, care domains addressed (e.g., cognitive support, safety, caregiver support), reported outcomes (e.g., quality of life, independence, caregiver burden), and cross-cutting considerations (usability, trust, privacy, ethics).
- Pattern checking: Constant comparison across studies and iterative memoing to consolidate overlapping codes and ensure themes were coherent, distinct, and aligned with our research questions; the framework matrix was updated after each cycle to reflect decisions and rationales.
Ambiguities in codes or classifications were resolved through iterative discussion until consensus. We then organized the agreed codes into broader thematic categories that characterize the current research landscape in dementia-care technologies, allowing us to (1) map the distribution of technologies and interaction paradigms, (2) identify dominant trends and emerging areas, (3) examine how outcomes are operationalized and measured, and (4) surface under-explored issues such as ethical risks, accessibility barriers, and long-term deployment challenges. A de-identified version of the final framework matrix and the memo log is provided in the Supplementary Materials for transparency and reproducibility.
3. Results
In this section, our primary focus is to present the results of our analysis, with an emphasis on recent technological advancements in the domain of dementia care. Grounded in these contemporary technologies, we have systematically categorized our findings into six distinct and coherent themes. These thematic categories are Assistive and Smart Technology for Daily Life, Social Interaction and Communication, Caregiver Support and Training, and Well-being and Psychological Support. By categorizing our findings into these four research themes, we aim to offer a structured and insightful panorama of the current technological milieu within dementia care.
3.1. Results of Literature Search
Our research review was conducted across several comprehensive databases, including PubMed, Web of Science (WOS), Scopus, ACM, and IEEE, culminating in the selection of 32 highly relevant publications. To visually represent our findings and the evolving landscape of dementia care technology, we employ histograms, as illustrated in Figure 2. This figure depicts the distribution of research publications over the years, categorized by publishers such as ACM, IEEE, PubMed, Scopus, and Web of Science. The histogram reveals a growing research interest in dementia care technologies, particularly in recent years. Notably, ACM has consistently led in the number of publications, followed closely by IEEE, highlighting the pivotal role of computing and engineering communities in advancing dementia care technologies. The inclusion of PubMed and Scopus indicates a rise in interdisciplinary collaborations, merging healthcare insights with technological innovations.
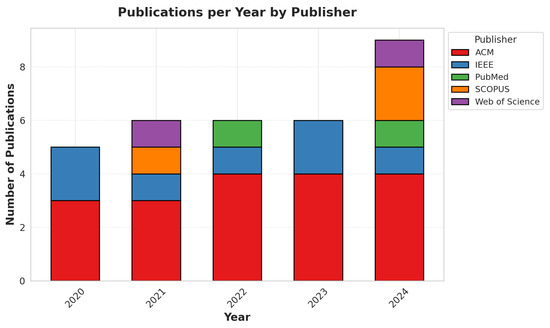
Figure 2.
Number of publications by year and publisher.
Figure 3 showcases the evolution of research themes over time, focusing on key categories such as Assistive and Smart Technology for Daily Life, Caregiver Support and Training, Social Interaction and Communication, and Well-being and Psychological Support. The data reveals a steady increase in research dedicated to well-being and psychological support, underscoring the growing emphasis on emotional and cognitive interventions in dementia care. Additionally, technologies aimed at enhancing social interaction and communication have seen a progressive rise, reflecting the importance of digital and robotic solutions in fostering engagement for individuals with dementia. Fluctuations in research on caregiver support and assistive technologies suggest ongoing exploration and refinement in these areas.
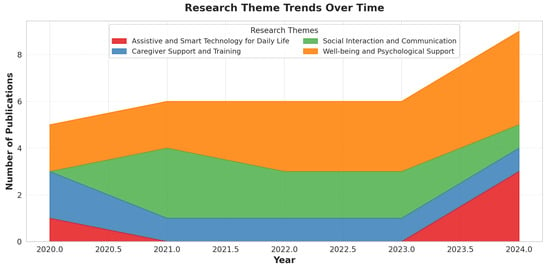
Figure 3.
Trends in technology categories over time.
Figure 4 provides a comprehensive overview of the proportion of research dedicated to various thematic areas. Well-being and psychological support dominate the landscape, emphasizing their central role in dementia care innovations. Social interaction and communication also represent a significant portion, highlighting the relevance of conversational agents, robotics, and digital engagement platforms in supporting both dementia patients and caregivers. While caregiver support and training, along with daily life assistance technologies, remain critical, they occupy a smaller share of the research, pointing to potential areas for further exploration and development. This distribution underscores the need for a holistic approach that integrates cognitive, emotional, social, and functional support in dementia care technology.
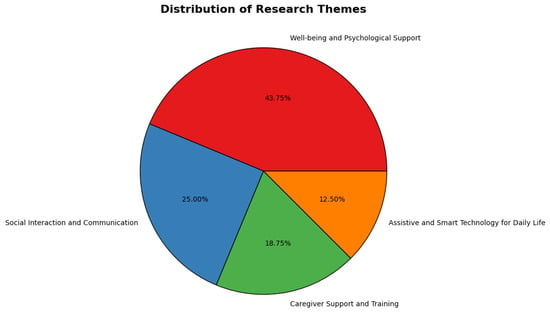
Figure 4.
Distribution of categories.
3.2. Thematic Analysis of Dementia Care Technologies
To systematically categorize and analyze research trends in dementia care technologies, we conducted a thematic analysis following Braun and Clarke’s [28] six-step framework. This approach enabled us to identify patterns across the selected literature and group studies based on their technological contributions. We began by thoroughly reviewing 33 selected research papers, extracting key insights regarding their objectives, methodologies, and the role of technology in dementia care. Through an iterative coding process, we identified recurring themes related to assistive technologies, social engagement, caregiver support, and well-being enhancement. Each paper was assigned multiple descriptive labels to capture its core technological focus before consolidating them into broader themes.
After the initial coding, we categorized the studies into four primary themes based on the nature of their technological intervention: (1) Assistive and Smart Technology for Daily Life, which includes solutions that aid activities of daily living (ADLs) and promote independence; (2) Social Interaction and Communication, encompassing robotic and digital tools designed to facilitate engagement and companionship for individuals with dementia; (3) Caregiver Support and Training, which includes training programs, mobile applications, and robotic assistants aimed at reducing caregiver burden and improving skill development; and (4) Well-being and Psychological Support, comprising interventions such as music therapy, reminiscence-based applications, and virtual reality experiences that focus on emotional and cognitive well-being. Each theme was refined iteratively to ensure clear distinctions while addressing overlaps in studies that spanned multiple domains.
The thematic analysis results provided valuable insights into the distribution and trends of dementia care technologies. We observed a significant focus on social interaction and well-being enhancement, reflecting the increasing importance of engagement-based interventions. The findings also highlighted a growing interest in robotic and AI-driven solutions, particularly in social and caregiver-support domains. By structuring the thematic analysis in this way, we were able to map the technological landscape, highlight key advancements, and identify research gaps in dementia care. The categorized themes serve as a foundation for discussing how technology can further evolve to meet the holistic needs of people with dementia and their caregivers.
3.3. Review Topics of Current Technologies in Dementia Care
Table 1 provides an overview of the selected relevant papers and their corresponding categories. Through the thematic analysis of the data material, as previously discussed, we have identified and categorized technology into four distinct areas aimed at enhancing the lives of individuals with dementia: (1) technologies for Social Interaction and Communication, (2) technologies for Well-being and Psychological Support, (3) technologies for Caregiver Support and Training, and (4) Assistive and Smart Technology for Daily Life. In this section, we present each of these categories in detail.

Table 1.
The distribution of technology categorization to dementia care in the corpus.
3.3.1. Technologies for Social Interaction and Communication
Social isolation and communication difficulties are among the most significant challenges faced by individuals with dementia, leading to emotional distress, depression, and reduced cognitive function. Technologies designed for social interaction and communication aim to enhance engagement, foster meaningful relationships, and provide PwD with a sense of connectedness [33,34,35,36,37,38,39,40]. Conversational agents, robotic companions, digital memory-sharing platforms, and cooperative gaming have emerged as effective solutions to counteract loneliness and cognitive decline. Xygkou et al. [33] introduced AI-powered conversational agents that help PwD engage in interactive dialogues, improving their cognitive stimulation and social interaction. Similarly, Lee et al. [34] demonstrated how social robots could bridge intergenerational gaps by facilitating shared activities between PwD and younger family members.
In addition to robotic and AI-driven solutions, digital communication tools play an essential role in promoting social engagement and memory recall. Munoz et al. [38] examined how cooperative digital games could enhance the visiting experience of PwD living in care homes, making interactions with visitors more engaging and meaningful. Similarly, memory-sharing platforms such as RelivRing [61] allow PwD to relive cherished memories through personalized audio recordings from family members, strengthening emotional bonds. Other studies highlight the importance of robotic pet therapy and virtual social platforms in alleviating social isolation, showing that digital and robotic companions can significantly improve mood, engagement, and cognitive well-being in PwD. The integration of these technologies into dementia care environments has the potential to reshape how PwD connect with their surroundings, caregivers, and loved ones, fostering greater emotional stability and quality of life.
Although conversational agents (CAs) and socially assistive robots (SARs) are widely available on mobile and home platforms, their effectiveness depends on communication capacity and disease severity. Across included studies, the most consistent benefits were reported in mild–to–moderate cohorts [33,39,40,62], whereas work with advanced dementia highlights barriers related to language production/comprehension, apathy/fatigue, sensory loss, and dysexecutive symptoms [35]. To reduce the common “light-case” bias in digital health, we recommend reporting staging (e.g., MMSE/MoCA bands; CDR), analyzing outcomes by severity strata, and documenting sensory baselines (hearing/vision aids). Design measures that help preserve usability across stages include multimodal I/O (speech with live captions, large-type text, simple pictograms), partnered use modes that let a care-partner co-pilot interactions (consistent with family-centred communication tools and care-partner roles in HCI) [34,36], and failure-tolerant dialogue with graceful fallback from free speech to small, menu-based choices when recognition confidence is low. Observational findings that residents may treat zoomorphic robots more as appliances than companions further underscore the need for low-load, predictable routines and clear affordances in late-stage contexts [37]. Finally, because recent CA deployments increasingly use LLM back-ends, systems should disclose language/dialect coverage and provide localized phrase sets to mitigate majority-language bias [33].
3.3.2. Technologies for Well-Being and Psychological Support
Ensuring the emotional well-being of individuals with dementia is just as crucial as addressing their cognitive and physical needs. Various sensory-based, music-based, and interactive cognitive therapies have been developed to enhance mood, reduce anxiety, and provide engaging experiences for PwD [47,48,49,50,51,52,53,54,55,56,57,58,59,60]. Nicol et al. [47] explored music therapy interventions, demonstrating how duet-playing technology encouraged active participation and emotional expression in PwD. Similarly, Collingham et al. [48] developed a multi-sensory interactive platform that stimulates vision, hearing, and touch, enhancing overall emotional well-being. These approaches align with research showing that music and multi-sensory engagement can trigger positive emotions, improve social interactions, and reduce agitation in PwD.
Other studies have examined the role of virtual reality (VR), robotics, and reminiscence therapy in enhancing well-being. Baumann et al. [49] developed VR-based reminiscence therapy, allowing PwD to relive past experiences through immersive digital environments. Schweiger et al. [51] investigated robot-assisted emotion regulation, where interactive robotic pets and humanoid robots provided comfort and companionship, reducing feelings of loneliness. Additionally, sensory-based experiences, such as ambient soundscapes and AI-driven mood enhancement systems, have shown promise in stabilizing emotions and reducing stress levels. These studies highlight the need for holistic approaches in dementia care, ensuring PwD experience meaningful engagement, comfort, and joy throughout their journey.
3.3.3. Assistive and Smart Technology for Daily Life
Assistive and smart technologies are becoming indispensable tools in dementia care, providing individuals with dementia (PwD) with greater independence in their daily activities while reducing caregiver burden. These technologies encompass wearable devices, sensor-based monitoring systems, robotic assistants, and smart home environments that help PwD navigate their daily routines safely and effectively [29,30,31,32]. For example, Ballester et al. [29] introduced a depth-based interactive system designed to assist PwD with mobility challenges by detecting their presence and providing real-time guidance. Similarly, Yuan et al. [30] explored robot-assisted self-care technologies, which help PwD with dressing, grooming, and hygiene tasks, enabling them to maintain dignity and independence. The adoption of these smart technologies contributes to a safer and more structured living environment, mitigating risks such as falls, forgetting daily routines, or failing to take prescribed medications.
Beyond physical assistance, automated and AI-driven technologies are being integrated into dementia care to optimize daily life interactions. Mirkovic et al. [31] developed a multimodal AI-driven system that adapts to the cognitive state of PwD, providing personalized reminders and interactive guidance throughout the day. Smart home environments embedded with Internet of Things (IoT) sensors are particularly useful for monitoring cognitive and physical decline over time, allowing caregivers and healthcare professionals to intervene proactively when necessary. Additionally, robotic assistants are playing an increasingly important role in promoting routine-based independence, assisting PwD in performing daily tasks while offering companionship and emotional support. The continued advancement of assistive and smart technologies holds the potential to transform home-based and institutional dementia care, enhancing quality of life while alleviating the pressures placed on caregivers and medical professionals.
3.3.4. Technologies for Caregiver Support and Training
Caring for individuals with dementia is a demanding task, often leading to burnout, emotional exhaustion, and high stress levels among caregivers. To address these challenges, various technology-assisted caregiver support systems have been developed, focusing on training, remote monitoring, and robotic assistance [41,42,43,44,45,46]. Wu et al. [41] explored the effectiveness of virtual reality (VR)-based dementia training programs for professional caregivers, revealing that immersive simulations improved their understanding of dementia symptoms, patient behavior, and caregiving techniques. Similarly, Shen et al. [42] introduced an augmented reality (AR)-based dementia education platform to provide interactive training modules, allowing caregivers to practice different caregiving scenarios in a safe and controlled virtual setting. These technologies equip caregivers with the skills and confidence needed to handle complex dementia care situations, ultimately enhancing the quality of care provided to PwD.
Beyond training, remote monitoring systems and robotic caregiver support have become essential in reducing workload and improving caregiving efficiency. Yuan et al. [43] examined robot-assisted psychoeducation programs, demonstrating that robotic technology could provide emotional and psychological support to caregivers by engaging PwD in cognitive and physical activities. Hiramatsu et al. [45] developed an AI-driven monitoring system that continuously tracks the health and safety of PwD at home, sending real-time alerts to caregivers when necessary. These advancements bridge the gap between professional and informal caregiving, offering caregivers greater flexibility, reduced stress, and improved job satisfaction. Future research should continue refining these technological caregiving solutions, ensuring they are user-friendly, scalable, and accessible to a broader caregiver population.
4. Discussion
Our review underscores the dynamic evolution of technological interventions in dementia care, spanning assistive and smart technologies, social interaction tools, caregiver support, and psychological well-being enhancements. The synthesis of existing literature reveals substantial progress in these areas, yet it also highlights critical gaps and opportunities for future advancements. This discussion contextualizes the findings within broader dementia care paradigms, reflecting on their implications for both individuals with dementia (PwD) and caregivers.
4.1. Consideration of Dementia Progression
While many technologies aim to enhance the lives of people with dementia, such as intelligent assistive technologies [13], mobile-based solutions [14,63], ambient-assisted living technologies [64], and smart health technologies [65], etc., they often predominantly focus on individuals with later onset dementia, typically diagnosed after the age of 65. This focus leaves a notable gap in research and care for those with early onset dementia, also known as young onset dementia. Early onset dementia affects individuals who are diagnosed at a younger age, and addressing their specific needs and challenges is of paramount importance [53]. Due to its rarity, dementia in young individuals is frequently misdiagnosed or ignored, in contrast to that in older adults [66]. Early diagnosis is essential for obtaining appropriate support services and therapies. Younger individuals may have different care needs compared to older adults with dementia [67]. They may require services tailored to their age group, such as vocational rehabilitation, educational support, and assistance with maintaining social connections. Furthermore, young individuals with dementia frequently want to preserve their independence and sense of self for as long as feasible [68]. Support services should focus on keeping people active and involved in things they love, as well as assisting them with difficult chores. Additionally, unlike seniors, young people with dementia are more likely to be employed, have dependent children, and be physically active. Consequently, the stress of dealing with dementia tends to affect younger people more than older individuals due to career and financial concerns [68], as well as family and caregiver responsibilities [69]. Moreover, younger people with dementia may experience social isolation and stigma because of their age, and support groups and social activities created for older individuals may not be appropriate for them. In terms of health needs, young-onset dementia may have distinct underlying causes and progressions than dementia in older people, therefore health management and care measures should be tailored accordingly. However, some researchers have underscored the importance of addressing the unique requirements of individuals with early onset dementia and advocated for the implementation of dementia care technologies tailored to this demographic [53]. The distinct experiences and challenges faced by individuals diagnosed at a younger age necessitate innovative approaches to technology-driven care and support. The predominance of late-onset cohorts in HCI studies limits generalizability to EOD/YOD. Where possible, we note interventions with plausible portability (e.g., speech-based assessments, family-centric support) and identify design gaps unique to working-age adults.
Moreover, it is essential to recognize that dementia manifests across various stages, each of which presents different cognitive, physical, and emotional challenges. The progression of dementia can significantly influences how individuals interact with technology, and this aspect deserves further exploration. While technology has the potential to improve the quality of life for PwD at different stages of dementia, it should be designed with an understanding of the unique needs and capabilities associated with each stage. Incorporating technology into dementia care for early onset cases and tailoring solutions to different stages of dementia will not only address existing gaps in research but also contribute to more effective and compassionate care for individuals across the entire dementia spectrum. Future research should prioritize the development of technologies designed specifically for younger individuals with early-onset dementia, addressing challenges such as work-life balance and family responsibilities. Additionally, adaptive systems that respond to varying cognitive stages could significantly enhance the utility of technology across the entire dementia spectrum.
Additionally, beyond conventional scales, several digitally captured measures now show analytic and clinical validation signals for tracking Alzheimer’s disease (AD) progression. First, augmented-reality (AR) IADL tasks have demonstrated group discrimination (healthy vs. preclinical vs. prodromal AD), associations with cognitive/functional tests, and at-home feasibility with test–retest analyses [70]. Second, longitudinal speech composites combining acoustic and linguistic features detect change over 6–18 months and correlate with clinical endpoints (e.g., CDR-SB, ADAS-Cog), supporting sensitivity to progression [71]. Third, multi-sensor remote monitoring technologies (wearables, smartphone tasks, sleep and gait metrics) show stage-wise differences and machine-learning discrimination in multicentre cohorts (e.g., RADAR-AD) [72]. These tools increasingly report clinimetric properties (test–retest, learning effects, AUC, responsiveness). However, broad regulatory qualification and pathway-linked triggers (i.e., how changes prompt care actions) remain limited; studies should therefore report the validation level (analytic, clinical, longitudinal), population/stage, and context of use to clarify readiness for routine care.
4.2. Emerging Technologies and Future Trends
4.2.1. Research Trends and Opportunities
Recent HCI work for people with dementia (PwD) has increasingly emphasized well-being (Figure 1), shifting focus toward tools that support everyday life and relationships. Alongside conventional approaches, interventions such as virtual reality and mindfulness apps are being explored to improve mood, engagement, and self-efficacy. In parallel, advances in sensors and wearables have accelerated progress in Daily Life Monitoring and Daily Life Support: smart-home systems and assistive devices simplify routines and may reduce caregiver burden [73]. Natural-language technologies are also moving the field toward richer social interaction and communication, with personalized voice assistants and socially assistive robots providing companionship, prompting, and dyadic support [74,75].
Several adjacent HCI innovations outline plausible near-term pathways for translation into dementia care. Rewind demonstrates memory cueing from self-tracked location traces [76]; NeuralGaitillustrates passive, smartphone-based gait assessment relevant to brain health [77]; and everyday platforms (smartphones, voice assistants, social media) continue to be appropriated for health-related use [78]. To maximize real-world impact, future studies should prioritize longitudinal, in-home evaluations, report acceptability for both PwD and care partners, and address privacy, accessibility, and equity from the outset.
4.2.2. Digital Biomarkers for Assessment
Digital biomarkers for dementia assessment extend beyond cognitive apps to four main classes: (i) speech and language(acoustic/linguistic features associated with severity and longitudinal change); (ii) motor activity, gait, and mobility derived from wearables and smartphones; (iii) sleep and circadian patterns (e.g., fragmentation, REM-related metrics); and (iv) ecologically grounded IADL performance via AR/VR tasks or structured smartphone interactions. Recent reviews and scoping analyses highlight their potential for continuous, objective, and sensitive endpoints—especially in early Alzheimer’s disease—while stressing transparent reporting and external validation [79,80,81]. Representative validation studies include AR-based IADL assessment with clinic/home feasibility and group discrimination [70], longitudinal speech composites that track progression [71], and multicentre evaluations of remote-monitoring technologies across disease stages [72]. We therefore recommend reporting capture burden, data-quality controls, clinimetric properties (test–retest reliability, minimal detectable change, responsiveness), privacy footprint, and—critically—predefined thresholds that trigger clinical follow-up (e.g., review, referral, or care-plan adjustment).
4.3. Limitations
Despite the valuable insights gained from this review, several limitations should be acknowledged. First, to keep the synthesis contemporary and tractable, we restricted inclusion to the five most recent publication years (2020–2024) and searched major academic databases (PubMed, Web of Science, Scopus, ACM, IEEE). This scope may exclude relevant grey literature, non-indexed outlets, and earlier foundational work, introducing potential publication bias toward positive findings [41]. In a field with rapid, heavy-tailed growth and dispersion across venues, some relevant studies may still have been missed even though we complemented database queries with forward/backward citation chasing and halted snowballing when ten consecutive newly identified records yielded no additional eligible studies (see Section 2.4.4). Searches and screening were conducted in English, which may under-represent non-English records.
Second, while we categorized dementia-care technologies into themes such as social interaction, assistive technologies, caregiver support, and well-being enhancement, the boundaries between categories are sometimes fluid, leading to possible overlaps in classification [42,49]. Heterogeneity in study designs, participant characteristics, settings, and outcome measures limited direct comparisons and precluded quantitative synthesis in many cases, particularly for long-term efficacy [45,47]. Moreover, most studies were conducted in controlled environments (care facilities or hospitals) rather than real-world home settings, which may affect ecological validity [46]. Finally, the evidence base is weighted toward older adults; generalizability to early/young-onset dementia remains uncertain. Future work should prioritize longitudinal, real-world evaluations across diverse settings and dementia stages to assess sustained impact and equity of benefit [36,40].
5. Conclusions
In this work, we have explored the landscape of dementia care technologies by analyzing literature published in PubMed, Web of Science (WOS), Scopus, ACM, and IEEE from 2020 to 2024. Our literature review approach, guided by the PICO process and PRISMA guidelines, led us to a final selection of 32 relevant papers. These papers shed light on the current state of technologies designed to enhance dementia care. Our exploration of these selected papers allowed us to categorize existing dementia care technologies into four distinct categories: Assistive and Smart Technology for Daily Life, Social Interaction and Communication, Caregiver Support and Training, and Well-being and Psychological Support. Each category represents a vital aspect of dementia care, addressing the diverse needs of both patients and caregivers, while also providing answers to our aforementioned research questions. Furthermore, we have provided a glimpse into the research agenda for each of these categories, showcasing the ongoing advancements and innovations in the field. Wearable devices, mobile applications, robotic technologies, and more have been at the forefront of research, offering promising solutions to improve the lives of those affected by dementia. Looking ahead, we have discussed potential future technologies that could revolutionize dementia care. These technologies, ranging from wearable devices to Human–Computer Interaction (HCI)-driven solutions, hold the promise of enhancing the quality of life for dementia patients and alleviating the burdens faced by caregivers. In conclusion, our work serves as a valuable guide for future research in dementia care. By synthesizing the wealth of knowledge within this critical domain, we hope to inspire and inform researchers, caregivers, and healthcare professionals alike, ultimately advancing the care and support available to individuals living with dementia.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jdad2040041/s1. Supplement S1. Full search strategies (replication). Supplement S2. PRISMA-ScR Checklist (completed).
Author Contributions
Conceptualization, Y.M., Y.Z. and O.E.N.; methodology, Y.M., Y.Z. and O.E.N.; validation, Y.M., Y.Z., O.E.N., A.R., M.B. and M.F.; formal analysis, Y.M., Y.Z. and O.E.N.; investigation, Y.M., Y.Z. and O.E.N.; resources, Y.M. and O.E.N.; data curation, Y.M. and O.E.N.; writing—original draft preparation, Y.M. and Y.Z.; writing—review and editing, Y.M., Y.Z., O.E.N., A.R., M.B. and M.F.; visualization, Y.M. and Y.Z.; supervision, A.R., M.B. and M.F.; project administration, A.R., M.B. and M.F.; funding acquisition, A.R., M.B. and M.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially supported by the Research Council of Norway under project number 326907.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Dening, T.; Sandilyan, M.B. Dementia: Definitions and types. Nurs. Stand. (2014+) 2015, 29, 37. [Google Scholar] [CrossRef]
- Potkin, S.G. The ABC of Alzheimer’s disease: ADL and improving day-to-day functioning of patients. Int. Psychogeriatr. 2002, 14, 7–26. [Google Scholar] [CrossRef] [PubMed]
- Xia, H.; Zhang, Y.; Rajabi, N.; Taleb, F.; Yang, Q.; Kragic, D.; Li, Z. Shaping high-performance wearable robots for human motor and sensory reconstruction and enhancement. Nat. Commun. 2024, 15, 1760. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Wang, X.; Lawler, K.; Garg, S.; Bai, Q.; Alty, J. Applications of artificial intelligence to aid early detection of dementia: A scoping review on current capabilities and future directions. J. Biomed. Inform. 2022, 127, 104030. [Google Scholar] [CrossRef]
- Ma, Y.; Nordberg, O.E.; Zhang, Y.; Rongve, A.; Bachinski, M.; Fjeld, M. Understanding dementia speech: Towards an adaptive voice assistant for enhanced communication. In Companion Proceedings of the 16th ACM SIGCHI Symposium on Engineering Interactive Computing Systems, Cagliari, Italy, 24–28 June 2024; Association for Computing Machinery: New York, NY, USA, 2024; pp. 15–21. [Google Scholar]
- Pappadà, A.; Chattat, R.; Chirico, I.; Valente, M.; Ottoboni, G. Assistive technologies in dementia care: An updated analysis of the literature. Front. Psychol. 2021, 12, 644587. [Google Scholar] [CrossRef]
- Ma, Y.; Zhang, Y.; Fu, D.; Jahanshahikhabisi, M.; Matviienko, A.; Bachinski, M.; Fjeld, M.; Kragic, D. HAID: Human-AI interaction for dementia care. In Adjunct Proceedings of the 2024 Nordic Conference on Human-Computer Interaction, Uppsala, Sweden, 13–16 October 2024; Association for Computing Machinery: New York, NY, USA, 2024; pp. 1–4. [Google Scholar]
- Yang, P.; Bi, G.; Qi, J.; Wang, X.; Yang, Y.; Xu, L. Multimodal wearable intelligence for dementia care in healthcare 4.0: A survey. Inf. Syst. Front. 2021, 27, 197–214. [Google Scholar] [CrossRef]
- Yousaf, K.; Mehmood, Z.; Saba, T.; Rehman, A.; Munshi, A.M.; Alharbey, R.; Rashid, M. Mobile-health applications for the efficient delivery of health care facility to people with dementia (PwD) and support to their carers: A survey. BioMed Res. Int. 2019, 2019, 7151475. [Google Scholar] [CrossRef]
- Alm, N.; Astell, A.; Gowans, G.; Dye, R.; Ellis, M.; Vaughan, P.; Newell, A.F. An interactive entertainment system usable by elderly people with dementia. In Proceedings of the Universal Access in Human-Computer Interaction. Ambient Interaction: 4th International Conference on Universal Access in Human-Computer Interaction, UAHCI 2007 Held as Part of HCI International 2007, Beijing, China, 22–27 July 2007; Proceedings, Part II 4; Springer: Berlin/Heidelberg, Germany, 2007; pp. 617–623. [Google Scholar]
- Lazar, A.; Edasis, C.; Piper, A.M. A critical lens on dementia and design in HCI. In Proceedings of the Chi, Denver, CO, USA, 6–11 May 2017; pp. 2175–2188. [Google Scholar]
- Ma, Y.; Nordberg, O.E.; Hubbers, J.; Zhang, Y.; Rongve, A.; Bachinski, M.; Fjeld, M. Bridging the gap: Advancements in technology to support dementia care–a scoping review. arXiv 2024, arXiv:2404.09685. [Google Scholar]
- Dada, S.; Van der Walt, C.; May, A.A.; Murray, J. Intelligent assistive technology devices for persons with dementia: A scoping review. Assist. Technol. 2021, 36, 338–351. [Google Scholar] [CrossRef]
- Koo, B.M.; Vizer, L.M. Examining mobile technologies to support older adults with dementia through the lens of personhood and human needs: Scoping review. JMIR MHealth UHealth 2019, 7, e15122. [Google Scholar] [CrossRef]
- Eriksen, M.B.; Frandsen, T.F. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: A systematic review. J. Med. Libr. Assoc. JMLA 2018, 106, 420. [Google Scholar] [CrossRef] [PubMed]
- Selçuk, A.A. A guide for systematic reviews: PRISMA. Turk. Arch. Otorhinolaryngol. 2019, 57, 57. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; Moher, D. Evaluations of the uptake and impact of the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) Statement and extensions: A scoping review. Syst. Rev. 2017, 6, 263. [Google Scholar] [CrossRef] [PubMed]
- Heintz, H.; Monette, P.; Epstein-Lubow, G.; Smith, L.; Rowlett, S.; Forester, B.P. Emerging collaborative care models for dementia care in the primary care setting: A narrative review. Am. J. Geriatr. Psychiatry 2020, 28, 320–330. [Google Scholar] [CrossRef]
- Minkman, M.M.; Ligthart, S.A.; Huijsman, R. Integrated dementia care in The Netherlands: A multiple case study of case management programmes. Health Soc. Care Community 2009, 17, 485–494. [Google Scholar] [CrossRef]
- Clevenger, C.K.; Cellar, J.; Kovaleva, M.; Medders, L.; Hepburn, K. Integrated memory care clinic: Design, implementation, and initial results. J. Am. Geriatr. Soc. 2018, 66, 2401–2407. [Google Scholar] [CrossRef]
- Cipriani, G.; Lucetti, C.; Nuti, A.; Danti, S. Wandering and dementia. Psychogeriatrics 2014, 14, 135–142. [Google Scholar] [CrossRef]
- Kameyama, M.; Umeda-Kameyama, Y. Applications of artificial intelligence in dementia. Geriatr. Gerontol. Int. 2024, 24, 25–30. [Google Scholar] [CrossRef]
- Lin, C.C.; Yang, C.T.; Su, P.L.; Hsu, J.L.; Shyu, Y.I.L.; Hsu, W.C. Implementation difficulties and solutions for a smart-clothes assisted home nursing care program for older adults with dementia or recovering from hip fracture. BMC Med. Inform. Decis. Mak. 2024, 24, 71. [Google Scholar] [CrossRef]
- Koh, W.Q.; Heins, P.; Flynn, A.; Mahmoudi Asl, A.; Garcia, L.; Malinowsky, C.; Brorsson, A. Bridging gaps in the design and implementation of socially assistive technologies for dementia care: The role of occupational therapy. Disabil. Rehabil. Assist. Technol. 2024, 19, 595–603. [Google Scholar] [CrossRef]
- Zhang, Y.; Ma, Y.; Kragic, D. Vision beyond boundaries: An initial design space of domain-specific large vision models in human-robot interaction. In Adjunct Proceedings of the 26th International Conference on Mobile Human-Computer Interaction, Melbourne, VIC, Australia, 30 September–3 October 2024; Association for Computing Machinery: New York, NY, USA, 2024; pp. 1–8. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’brien, K.; Colquhoun, H.; Kastner, M.; Levac, D.; Ng, C.; Sharpe, J.P.; Wilson, K.; et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med. Res. Methodol. 2016, 16, 15. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Rajabi, N.; Taleb, F.; Matviienko, A.; Ma, Y.; Björkman, M.; Kragic, D. Mind meets robots: A review of EEG-based brain-robot interaction systems. Int. J. Hum.–Comput. Interact. 2025, 41, 12784–12815. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Ballester, I.; Gall, M.; Münzer, T.; Kampel, M. Depth-based interactive assistive system for dementia care. J. Ambient Intell. Humaniz. Comput. 2024, 15, 3901–3912. [Google Scholar] [CrossRef]
- Yuan, F.; Bray, R.; Oliver, M.; Duzan, J.; Crane, M.; Zhao, X. A social robot-facilitated performance assessment of self-care skills for people with alzheimer’s: A preliminary study. Int. J. Soc. Robot. 2024, 16, 2065–2078. [Google Scholar] [CrossRef]
- Mirkovic, N.; Wolff, C. Multimodal interaction in an adaptive dementia exercise robot. In Proceedings of the 2024 IEEE First International Conference on Artificial Intelligence for Medicine, Health and Care (AIMHC), Laguna Hills, CA, USA, 5–7 February 2024; pp. 201–208. [Google Scholar]
- Carros, F.; Meurer, J.; Löffler, D.; Unbehaun, D.; Matthies, S.; Koch, I.; Wieching, R.; Randall, D.; Hassenzahl, M.; Wulf, V. Exploring human-robot interaction with the elderly: Results from a ten-week case study in a care home. In Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020; pp. 1–12. [Google Scholar]
- Xygkou, A.; Ang, C.S.; Siriaraya, P.; Kopecki, J.P.; Covaci, A.; Kanjo, E.; She, W.J. MindTalker: Navigating the Complexities of AI-Enhanced Social Engagement for People with Early-Stage Dementia. In Proceedings of the 2024 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 11–16 May 2024; pp. 1–15. [Google Scholar]
- Lee, H.R.; Sun, F.; Iqbal, T.; Roberts, B. Reimagining robots for dementia: From robots for care-receivers/giver to robots for carepartners. In Proceedings of the 2023 ACM/IEEE International Conference on Human-Robot Interaction, Stockholm, Sweden, 13–16 March 2023; pp. 475–484. [Google Scholar]
- Raß, E.; Unbehaun, D.; Wulf, V.; Lüssem, J.; Eilers, H.; Lenz, G.; Tandler, J.; Afzali, S.N.; Eroglu, B. Investigating the potential and impacts of social robots to engage people with advanced dementia and their caregivers: Early insights from an exploratory ethnographic study within a protected care environment. In Proceedings of the 16th International Conference on Pervasive Technologies Related to Assistive Environments, Corfu, Greece, 5–7 July 2023; pp. 272–278. [Google Scholar]
- Thoolen, M.; Toso, F.; TM Peek, S.; Lu, Y.; Brankaert, R. LivingMoments: Bespoke social communication for people living with dementia and their relatives. In Proceedings of the 2022 CHI Conference on Human Factors in Computing Systems, New Orleans, LA, USA, 30 April–5 May 2022; pp. 1–18. [Google Scholar]
- Marchetti, E.; Grimme, S.; Hornecker, E.; Kollakidou, A.; Graf, P. Pet-robot or appliance? Care home residents with dementia respond to a zoomorphic floor washing robot. In Proceedings of the 2022 CHI Conference on Human Factors in Computing Systems, New Orleans, LA, USA, 30 April–5 May 2022; pp. 1–21. [Google Scholar]
- Muñoz, D.; Favilla, S.; Pedell, S.; Murphy, A.; Beh, J.; Petrovich, T. Evaluating an app to promote a better visit through shared activities for people living with dementia and their families. In Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems, Virtual, 8–13 May 2021; pp. 1–13. [Google Scholar]
- Taylor, L.; Downing, A.; Noury, G.A.; Masala, G.; Palomino, M.; McGinn, C.; Jones, R. Exploring the applicability of the socially assistive robot Stevie in a day center for people with dementia. In Proceedings of the 2021 30th IEEE International Conference on Robot & Human Interactive Communication (RO-MAN), Vancouver, BC, Canada, 8–12 August 2021; pp. 957–962. [Google Scholar]
- Khosla, R.; Chu, M.T.; Khaksar, S.M.S.; Nguyen, K.; Nishida, T. Engagement and experience of older people with socially assistive robots in home care. Assist. Technol. 2021, 33, 57–71. [Google Scholar] [CrossRef]
- Wu, J.; Igarashi, A.; Suzuki, H.; Matsumoto, H.; Kugai, H.; Takaoka, M.; Yamamoto-Mitani, N. Effects of a dementia educational programme using virtual reality on nurses in an acute care hospital: A pre-post comparative study. Int. J. Older People Nurs. 2024, 19, e12616. [Google Scholar] [CrossRef]
- Shen, X.; Pai, Y.S.; Kiuchi, D.; Bao, K.; Aoki, T.; Meguro, H.; Oishi, K.; Wang, Z.; Wakisaka, S.; Minamizawa, K. Dementia eyes: Co-Design and Evaluation of a dementia education augmented reality experience for medical workers. In Proceedings of the 2023 CHI Conference on Human Factors in Computing Systems, Hamburg, Germany, 23–29 April 2023; pp. 1–18. [Google Scholar]
- Yuan, F.; Bowland, S.; Proctor, L.; Blackburn, J.; Mukherjee, N.; Bray, R.; Lopez, R.P.; Wick, K.; Zhao, X. Robot-assisted psycho-education to enhance Alzheimer’s caregiver health. In Proceedings of the 2022 IEEE/ACM Conference on Connected Health: Applications, Systems and Engineering Technologies (CHASE), Arlington, VA, USA, 17–19 November 2022; pp. 57–65. [Google Scholar]
- Zubatiy, T.; Vickers, K.L.; Mathur, N.; Mynatt, E.D. Empowering dyads of older adults with mild cognitive impairment and their care partners using conversational agents. In Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems, Virtual, 8–13 May 2021; pp. 1–15. [Google Scholar]
- Hiramatsu, T.; Kamei, M.; Inoue, D.; Kawamura, A.; An, Q.; Kurazume, R. Development of dementia care training system based on augmented reality and whole body wearable tactile sensor. In Proceedings of the 2020 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Las Vegas, Nevada, USA, 25–29 October 2020; pp. 4148–4154. [Google Scholar]
- Lv, H.; Yang, G.; Zhou, H.; Huang, X.; Yang, H.; Pang, Z. Teleoperation of collaborative robot for remote dementia care in home environments. IEEE J. Transl. Eng. Health Med. 2020, 8, 1400510. [Google Scholar]
- Nicol, J.; Loehr, J.; Christensen, J.; Lang, J.; Peacock, S. Duet playing in dementia care: A new therapeutic music technology. Disabil. Rehabil. Assist. Technol. 2024, 19, 3139–3152. [Google Scholar] [CrossRef]
- Collingham, H.; Wallace, J.; Crawshaw, P.; Hunt, L. Mariana’s Song: Materializing Personhood through Non-Linear Multisensory Experiences Designed for People Living with Advanced Dementia. In Proceedings of the 2024 ACM Designing Interactive Systems Conference, Copenhagen, Denmark, 1–5 July 2024; pp. 819–843. [Google Scholar]
- Baumann, A.; Shaw, P.; Trotter, L.; Clinch, S.; Davies, N. Mnemosyne-Supporting Reminiscence for Individuals with Dementia in Residential Care Settings. In Proceedings of the 2024 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 11–16 May 2024; pp. 1–17. [Google Scholar]
- Vidas, D.; Thompson, Z.; Kelly, R.M.; Waycott, J.; Tamplin, J.; Vieira Sousa, T.; Kulik, L.; Lampit, A.; Lautenschlager, N.T.; Baker, F.A. Family caregiver experiences of using a mobile app for music-based training to support dementia care. In Proceedings of the 2024 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 11–16 May 2024; pp. 1–16. [Google Scholar]
- Schweiger, N.; Wolff, C. Robotic Support for Haptic Dementia Exercises. In Proceedings of the 2023 IEEE 11th International Conference on Serious Games and Applications for Health (SeGAH), Athens, Greece, 28–30 August 2023; pp. 1–7. [Google Scholar]
- Houben, M.; van Berlo, M.; Antonissen, F.; Wouters, E.; Brankaert, R. Switch2Move: Designing a tangible interface with people living with dementia for initiating and engaging in music-supported exercises at home. In Proceedings of the 2023 ACM Designing Interactive Systems Conference, Pittsburgh, PA, USA, 10–14 July 2023; pp. 1457–1471. [Google Scholar]
- Yuan, F.; Boltz, M.; Bilal, D.; Jao, Y.L.; Crane, M.; Duzan, J.; Bahour, A.; Zhao, X. Cognitive Exercise for Persons with Alzheimer’s Disease and Related Dementia Using a Social Robot. IEEE Trans. Robot. 2023, 39, 3332–3346. [Google Scholar] [CrossRef]
- Houben, M.; Brankaert, R.; Dhaeze, E.; Kenning, G.; Bongers, I.; Eggen, B. Enriching everyday lived experiences in dementia care. In Proceedings of the Sixteenth International Conference on Tangible, Embedded, and Embodied Interaction, Daejeon, Republic of Korea, 13–16 February 2022; pp. 1–13. [Google Scholar]
- Houben, M.; Brankaert, R.; Kenning, G.; Bongers, I.; Eggen, B. Designing for everyday sounds at home with people with dementia and their partners. In Proceedings of the 2022 CHI Conference on Human Factors in Computing Systems, New Orleans, LA, USA, 30 April–5 May 2022; pp. 1–15. [Google Scholar]
- Flynn, A.; Barry, M.; Qi Koh, W.; Reilly, G.; Brennan, A.; Redfern, S.; Casey, D. Introducing and familiarising older adults living with dementia and their caregivers to virtual reality. Int. J. Environ. Res. Public Health 2022, 19, 16343. [Google Scholar] [CrossRef] [PubMed]
- Karaosmanoglu, S.; Rings, S.; Kruse, L.; Stein, C.; Steinicke, F. Lessons learned from a human-centered design of an immersive exergame for people with dementia. Proc. ACM Hum.-Comput. Interact. 2021, 5, 1–27. [Google Scholar] [CrossRef]
- Kang, J.M.; Kim, N.; Lee, S.Y.; Woo, S.K.; Park, G.; Yeon, B.K.; Park, J.W.; Youn, J.H.; Ryu, S.H.; Lee, J.Y.; et al. Effect of cognitive training in fully immersive virtual reality on visuospatial function and frontal-occipital functional connectivity in predementia: Randomized controlled trial. J. Med. Internet Res. 2021, 23, e24526. [Google Scholar] [CrossRef] [PubMed]
- Houben, M.; Brankaert, R.; Bakker, S.; Kenning, G.; Bongers, I.; Eggen, B. The role of everyday sounds in advanced dementia care. In Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020; pp. 1–14. [Google Scholar]
- Cruz-Sandoval, D.; Morales-Tellez, A.; Sandoval, E.B.; Favela, J. A social robot as therapy facilitator in interventions to deal with dementia-related behavioral symptoms. In Proceedings of the 2020 ACM/IEEE International Conference on Human-Robot Interaction, Cambridge, UK, 23–26 March 2020; pp. 161–169. [Google Scholar]
- van Rijen, K.; Cobbenhagen, T.; Janssen, R.; Olsen, M.; Brankaert, R.; Houben, M.; Lu, Y. RelivRing: Reliving social activities for people with dementia. In Proceedings of the Extended Abstracts of the 2020 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020; pp. 1–8. [Google Scholar]
- Muñoz, D.; Pedell, S.; Sterling, L. Evaluating Engagement in Technology-Supported Social Interaction by People Living with Dementia in Residential Care. ACM Trans. Comput.-Hum. Interact. 2022, 29, 1–31. [Google Scholar] [CrossRef]
- Ye, B.; Chu, C.H.; Bayat, S.; Babineau, J.; How, T.V.; Mihailidis, A. Researched Apps Used in Dementia Care for People Living with Dementia and Their Informal Caregivers: Systematic Review on App Features, Security, and Usability. J. Med. Internet Res. 2023, 25, e46188. [Google Scholar] [CrossRef]
- Gettel, C.J.; Chen, K.; Goldberg, E.M. Dementia care, fall detection, and ambient-assisted living technologies help older adults age in place: A scoping review. J. Appl. Gerontol. 2021, 40, 1893–1902. [Google Scholar] [CrossRef]
- Guisado-Fernández, E.; Giunti, G.; Mackey, L.M.; Blake, C.; Caulfield, B.M. Factors influencing the adoption of smart health technologies for people with dementia and their informal caregivers: Scoping review and design framework. JMIR Aging 2019, 2, e12192. [Google Scholar] [CrossRef]
- Sullivan, M.P.; Williams, V.; Grillo, A.; McKee-Jackson, R.; Camic, P.M.; Windle, G.; Stott, J.; Brotherhood, E.; Crutch, S.J.; Rare Dementia Support (RDS) research team. Peer support for people living with rare or young onset dementia: An integrative review. Dementia 2022, 21, 2700–2726. [Google Scholar] [CrossRef]
- Hancock, G.A.; Woods, B.; Challis, D.; Orrell, M. The needs of older people with dementia in residential care. Int. J. Geriatr. Psychiatry J. Psychiatry Late Life Allied Sci. 2006, 21, 43–49. [Google Scholar] [CrossRef]
- Greenwood, N.; Smith, R. The experiences of people with young-onset dementia: A meta-ethnographic review of the qualitative literature. Maturitas 2016, 92, 102–109. [Google Scholar] [CrossRef]
- Cabote, C.J.; Bramble, M.; McCann, D. Family caregivers’ experiences of caring for a relative with younger onset dementia: A qualitative systematic review. J. Fam. Nurs. 2015, 21, 443–468. [Google Scholar] [CrossRef]
- Muurling, M.; de Boer, C.; Vairavan, S.; Harms, R.L.; Chadha, A.S.; Tarnanas, I.; Luis, E.V.; Religa, D.; Gjestsen, M.T.; Galluzzi, S.; et al. Augmented reality versus standard tests to assess cognition and function in early Alzheimer’s disease. npj Digit. Med. 2023, 6, 234. [Google Scholar] [CrossRef] [PubMed]
- Robin, J.; Xu, M.; Balagopalan, A.; Novikova, J.; Kahn, L.; Oday, A.; Hejrati, M.; Hashemifar, S.; Negahdar, M.; Simpson, W.; et al. Automated detection of progressive speech changes in early Alzheimer’s disease. Alzheimer’s Dementia Diagn. Assess. Dis. Monit. 2023, 15, e12445. [Google Scholar] [CrossRef] [PubMed]
- Lentzen, M.; Vairavan, S.; Muurling, M.; Alepopoulos, V.; Atreya, A.; Boada, M.; de Boer, C.; Conde, P.; Curcic, J.; Frisoni, G.; et al. RADAR-AD: Assessment of multiple remote monitoring technologies for early detection of Alzheimer’s disease. Alzheimer’s Res. Ther. 2025, 17, 29. [Google Scholar] [CrossRef]
- Lazarou, I.; Karakostas, A.; Stavropoulos, T.G.; Tsompanidis, T.; Meditskos, G.; Kompatsiaris, I.; Tsolaki, M. A novel and intelligent home monitoring system for care support of elders with cognitive impairment. J. Alzheimer’s Dis. 2016, 54, 1561–1591. [Google Scholar] [CrossRef]
- Li, J.; Maharjan, B.; Xie, B.; Tao, C. A personalized voice-based diet assistant for caregivers of Alzheimer disease and related dementias: System development and validation. J. Med. Internet Res. 2020, 22, e19897. [Google Scholar] [CrossRef]
- Striegl, J.; Gollasch, D.; Loitsch, C.; Weber, G. Designing vuis for social assistance robots for people with dementia. In Proceedings of the Mensch und Computer 2021, Ingolstadt, Germany, 5–8 September 2021; pp. 145–155. [Google Scholar]
- Tan, N.A.H.; Sha, H.; Celen, E.; Tran, P.; Wang, K.; Cheung, G.; Hinch, P.; Huang, J. Rewind: Automatically Reconstructing Everyday Memories with First-Person Perspectives. Proc. ACM Interactive Mobile Wearable Ubiquitous Technol. 2018, 2, 1–20. [Google Scholar] [CrossRef]
- Li, H.; Chen, H.; Xu, C.; Li, Z.; Zhang, H.; Qian, X.; Li, D.; Huang, M.c.; Xu, W. NeuralGait: Assessing Brain Health Using Your Smartphone. Proc. ACM Interactive Mobile Wearable Ubiquitous Technol. 2023, 6, 1–28. [Google Scholar] [CrossRef]
- Shu, S.; Woo, B.K. Use of technology and social media in dementia care: Current and future directions. World J. Psychiatry 2021, 11, 109. [Google Scholar] [CrossRef]
- Qi, W.; Zhu, X.; Wang, B.; Shi, Y.; Dong, C.; Shen, S.; Li, J.; Zhang, K.; He, Y.; Zhao, M.; et al. Alzheimer’s disease digital biomarkers multidimensional landscape and AI model scoping review. npj Digit. Med. 2025, 8, 366. [Google Scholar] [CrossRef]
- Iulita, M.F.; Streel, E.; Harrison, J. Digital biomarkers: Redefining clinical outcomes and the concept of meaningful change. Alzheimer’s Dementia Transl. Res. Clin. Interv. 2025, 11, e70114. [Google Scholar] [CrossRef]
- Gramkow, M.H.; Gleerup, H.S.; Simonsen, A.H.; Waldemar, G.; Frederiksen, K.S. Digital biomarkers in early Alzheimer’s disease from wearable or portable technology: A scoping review. medRxiv 2025. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).