Dietary Patterns and Mental Health Across the Lifespan: A Systematic Review of Randomized Clinical Trials
Abstract
1. Introduction
2. Material and Methods
2.1. Systematic Review Aim and Strategy
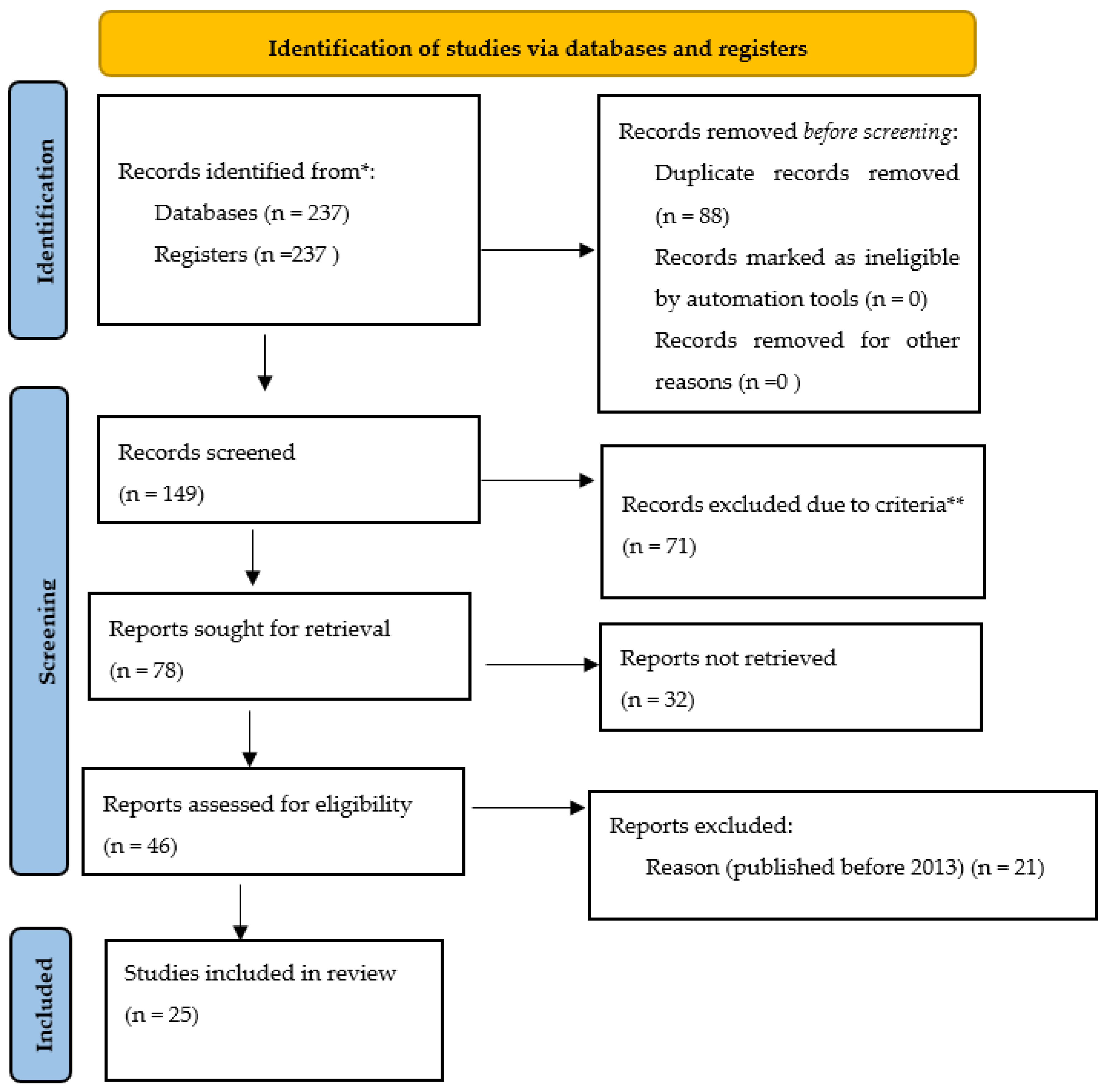
2.2. Literature Search, Study Selection, Eligibility Criteria and Quality Assessment
- -
- Population inclusion criteria: Studies involving individuals across all age groups, from infancy through late adulthood, that had diverse demographic characteristics, such as gender, socio-economic status, and cultural backgrounds, were used.
- -
- Study design: Rigorous research methodologies, including randomized controlled trials (RCTs), cohort studies, cross-sectional studies and systematic reviews were also selected. Further exclusion of case reports, editorials and non-research articles was performed to ensure methodological rigor.
- -
- Intervention and exposure variables: Studies evaluating the impact of nutritional interventions on mental health, exploring dietary factors, including macronutrient and micronutrient intake, dietary patterns and specific food items implicated in dental caries etiology, were additionally selected.
- -
- Outcome measures: Studies reporting relevant outcome measures, such as the incidence, prevalence, severity and progression of mental disorders, were incorporated. Among them, only studies employing standardized diagnostic criteria and assessment tools for dental caries evaluation were finally used.
- -
- Temporal considerations: Studies conducted over varying timeframes to capture longitudinal perspectives on the relationship between nutrition and mental health were also selected.
- -
- Publication characteristics: Additionally, we only considered studies published in peer-reviewed journals to uphold scholarly rigor.
- -
- Geographical variation: We also searched for potential variations in nutritional practices and mental health across different geographical regions; thus, we included studies conducted in diverse global settings to enhance generalizability.
- -
- Finally, only articles written in English and published after 2013 were included.
3. Results
3.1. Mediterranean Diet and Depression
3.2. MIND Diet and Cognitive Health
3.3. Plant-Based Diets and Stress, and Processed Food and Mental Health
4. Discussion
4.1. Main Findings
4.2. Comparison with Previous Research
4.3. Strengths and Limitations
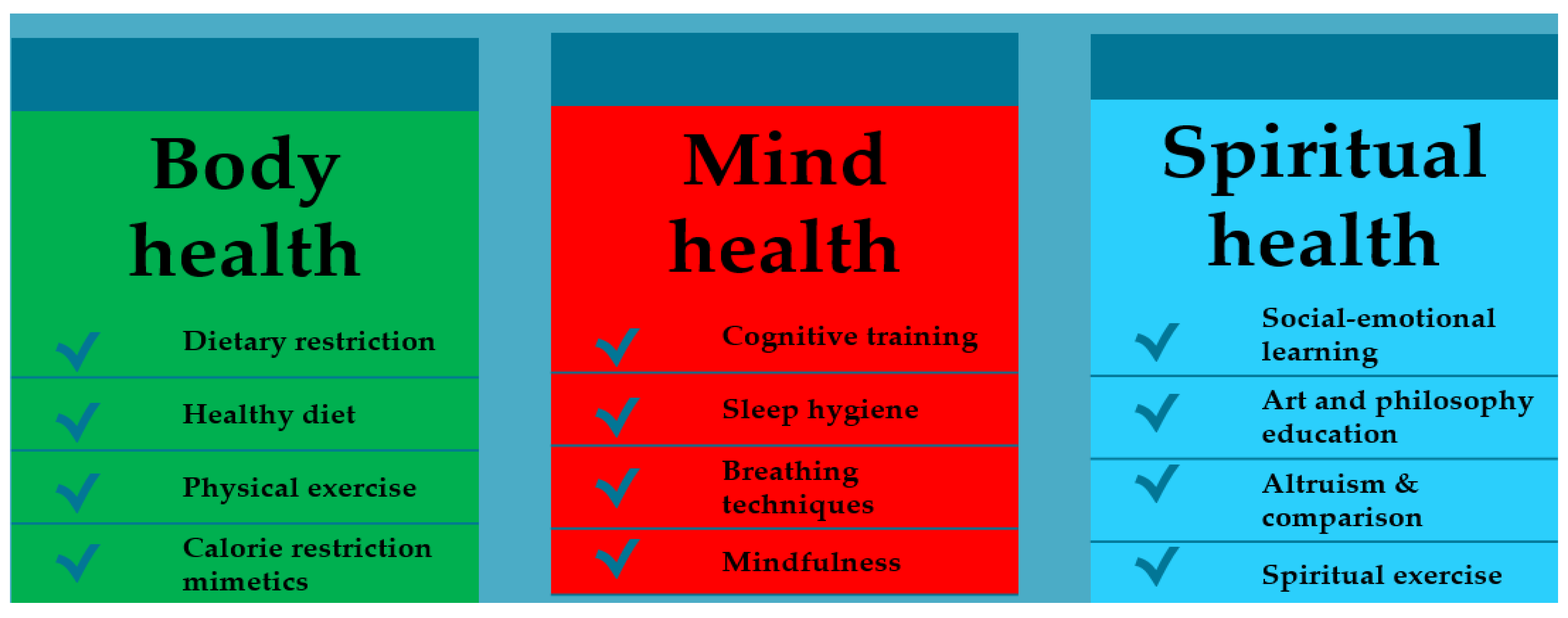
4.4. Practical Implications for Clinicians and Public Health
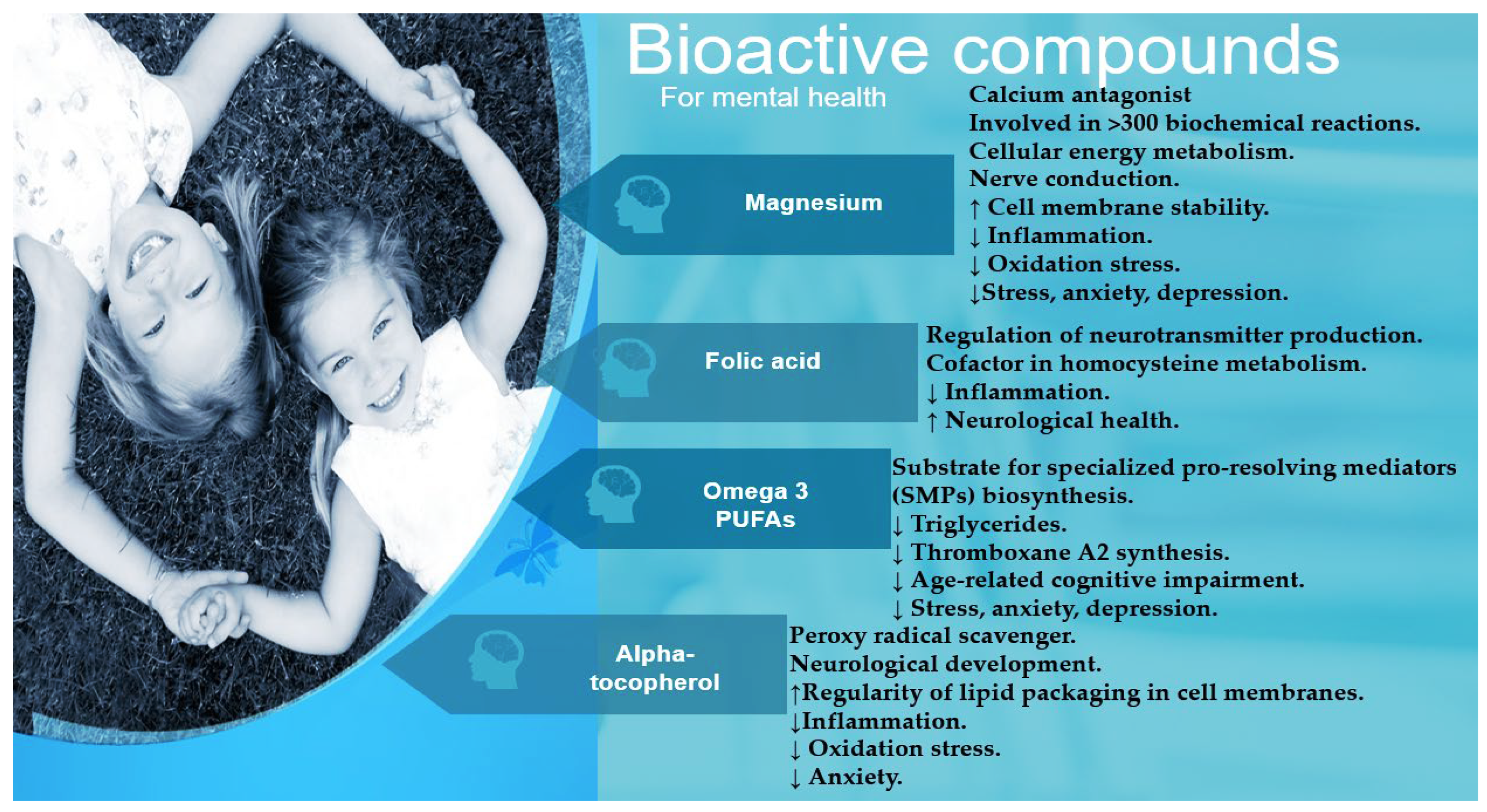
- Fatty fish or fish oil supplements: Omega-3 fatty acids, found in salmon and mackerel, can improve brain function and mood stability (Parletta et al., 2019). Omega-3 treatment improved autism traits such as stereotypic behavior and social communication in children with autism in randomized clinical trials with or without vitamin D supplementation (Doaei et al., 2021; Mazahery et al., 2019).
- Green leafy vegetables (spinach, kale lettuce and collard greens) are rich in folic acid and magnesium, which can help fight depression (Carcelén-Fraile et al., 2024; Sarma & TR, 2024).
- Blueberries or other fruits (watermelon, grape, peach, pomegranate, banana, apple or even dried fig) are rich in antioxidants that can protect the brain from oxidative stress. Bananas also provide vitamin B6 and tryptophan for serotonin production (Kahleova et al., 2020; Tavakkoli-Kakhki et al., 2015).
- Walnuts and almonds contain healthy fats and have been linked to improved cognitive performance (Jacka et al., 2017; Tavakkoli-Kakhki et al., 2015).
- Oats help stabilize blood sugar and can provide long-lasting energy (Carcelén-Fraile et al., 2024). Thyroid hormones influence how the body processes glucose. Thyroid stimulating hormone (TSH) levels of 2 mIU/L promote good sleep and mood; higher levels (5.2 mIU/L) have been associated with fatigue, weight gain and constipation (Munipalli et al., 2022).
- Yoghurt and kefir support gut health through probiotics (Dahiya & Nigam, 2023). Vitamin D supplementation also influences the treatment success for depressive symptoms (Föcker et al., 2018). People with vitamin D levels of 20 ng/mL showed symptoms such as constant fatigue and depressive mood, but higher levels in blood tests (70 mg/mL) were associated with strong immunity and mental health (Munipalli et al., 2022).
- Avocados are rich in healthy fats and mood-boosting B vitamins (Chawla, 2018). In particular, a vitamin B12 level of 650 pg/mL or more than 400 pg/mL helps with brain fog, difficulty concentrating and forgetfulness (Munipalli et al., 2022).
- Dark chocolate contains flavonoids that can improve mood and reduce stress hormones (Chawla, 2018). Several chemical compounds (tyramine, theobromine, phenylalanine, caffeine, etc.) are present in dark chocolate, which are responsible for the stimulating effect on the brain (Samanta et al., 2022).
- Chickpeas and other legumes are a source of fiber, protein and iron (Kahleova et al., 2020). A total protein content of 78 g/L can ensure good recovery and mental health, while a lower content of 61 g/L is associated with fatigue and weakness. Iron stores also play an important role in combating anxiety; a ferritin level of 75 mcg/L can lead to chronic fatigue and brain fog (Munipalli et al., 2022).
- Extra Virgin Olive Oil (EVOO) consumption by patients with mild cognitive impairment attenuates oxidative and nitrative stress, as reflected by reductions in PARP levels and DNA damage (50 mcg/L EVOO for one year) (Tzekaki et al., 2021).
- While sparkling water is not a primary source of lithium, it can be part of a person’s overall fluid intake that contributes to daily lithium consumption. Studies suggest that higher levels of lithium in drinking water, even at trace levels, may be associated with lower suicide rates (Brown et al., 2018).
- Aromatic and therapeutic plants such as basil, coriander, peppermint and dill have revealed preventive effects on depression or its complications (Tavakkoli-Kakhki et al., 2015).
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Section/Topic | # | Checklist Item | Reported on Page |
|---|---|---|---|
| INFORMATION SOURCES AND METHODS | |||
| Database name | 1 | Name each individual database searched, stating the platform for each. | 2–5 |
| Multi-database searching | 2 | If databases were searched simultaneously on a single platform, state the name of the platform, listing all of the databases searched. | 2–5 |
| Study registries | 3 | List any study registries searched. | 3–4 |
| Online resources and browsing | 4 | Describe any online or print source purposefully searched or browsed (e.g., tables of contents, print conference proceedings, web sites), and how this was done. | 3 |
| Citation searching | 5 | Indicate whether cited references or citing references were examined, and describe any methods used for locating cited/citing references (e.g., browsing reference lists, using a citation index, setting up email alerts for references citing included studies). | 3–5 |
| Contacts | 6 | Indicate whether additional studies or data were sought by contacting authors, experts, manufacturers, or others. | 3 |
| Other methods | 7 | Describe any additional information sources or search methods used. | 3 |
| SEARCH STRATEGIES | |||
| Full search strategies | 8 | Include the search strategies for each database and information source, copied and pasted exactly as run. | 2–5 |
| Limits and restrictions | 9 | Specify that no limits were used, or describe any limits or restrictions applied to a search (e.g., date or time period, language, study design) and provide justification for their use. | 2–5 |
| Search filters | 10 | Indicate whether published search filters were used (as originally designed or modified), and if so, cite the filter(s) used. | 3 |
| Prior work | 11 | Indicate when search strategies from other literature reviews were adapted or reused for a substantive part or all of the search, citing the previous review(s). | 3 |
| Updates | 12 | Report the methods used to update the search(es) (e.g., rerunning searches, email alerts). | 3 |
| Dates of searches | 13 | For each search strategy, provide the date when the last search occurred. | 2, 3 |
| PEER REVIEW | |||
| Peer review | 14 | Describe any search peer review process. | 3 |
| MANAGING RECORDS | |||
| Total Records | 15 | Document the total number of records identified from each database and other information sources. | 5 |
| Deduplication | 16 | Describe the processes and any software used to deduplicate records from multiple database searches and other information sources. | 3 |
References
- Adams, J. B., Audhya, T., Geis, E., Gehn, E., Fimbres, V., Pollard, E. L., Mitchell, J., Ingram, J., Hellmers, R., & Laake, D. (2018). Comprehensive nutritional and dietary intervention for autism spectrum disorder—A randomized, controlled 12-month trial. Nutrients, 10(3), 369. [Google Scholar] [CrossRef]
- Adan, R. A., van der Beek, E. M., Buitelaar, J. K., Cryan, J. F., Hebebrand, J., Higgs, S., Schellekens, H., & Dickson, S. L. (2019). Nutritional psychiatry: Towards improving mental health by what you eat. European Neuropsychopharmacology, 29(12), 1321–1332. [Google Scholar] [CrossRef]
- Agarwal, U., Mishra, S., Xu, J., Levin, S., Gonzales, J., & Barnard, N. D. (2015). A multicenter randomized controlled trial of a nutrition intervention program in a multiethnic adult population in the corporate setting reduces depression and anxiety and improves quality of life: The GEICO study. American Journal of Health Promotion, 29(4), 245–254. [Google Scholar] [CrossRef] [PubMed]
- Almuntashiri, S. A., Alsubaie, F. F., & Alotaybi, M. (2025). Plant-based diets and their role in preventive medicine: A systematic review of evidence-based insights for reducing disease risk. Cureus, 17(2), e78629. [Google Scholar] [CrossRef]
- Alzubide, S., & Alhalafi, M. (2024). The gut brain connection. Journal of Behavioral and Brain Science, 14(3), 103–117. [Google Scholar] [CrossRef]
- Arab, A., Khorvash, F., Kazemi, M., Heidari, Z., & Askari, G. (2022). Effects of the Dietary Approaches to Stop Hypertension (DASH) diet on clinical, quality of life and mental health outcomes in women with migraine: A randomised controlled trial. British Journal of Nutrition, 128(8), 1535–1544. [Google Scholar] [CrossRef]
- Arjmand, G., Abbas-Zadeh, M., & Eftekhari, M. H. (2022). Effect of MIND diet intervention on cognitive performance and brain structure in healthy obese women: A randomized controlled trial. Scientific Reports, 12(1), 2871. [Google Scholar] [CrossRef] [PubMed]
- Arnoldy, L., Gauci, S., Young, L. M., Macpherson, H., Civier, O., Scholey, A., Pipingas, A., & White, D. J. (2025). Assessing the association between the Mediterranean, Dietary Approaches to Stop Hypertension and Mediterranean-DASH Intervention for Neurodegenerative Delay dietary patterns, structural connectivity and cognitive function. British Journal of Nutrition, 133, 901–917. [Google Scholar] [CrossRef]
- Barnes, L. L., Dhana, K., Carey, V., Grodstein, F., Tangney, C. C., Aggarwal, N. T., Arfanakis, K., Morris, M. C., & Sacks, F. (2023a). Primary prevention of cognitive decline in older individuals with the MIND diet. Alzheimer’s & Dementia, 19, e078519. [Google Scholar]
- Barnes, L. L., Dhana, K., Liu, X., Carey, V. J., Ventrelle, J., Johnson, K., Hollings, C. S., Bishop, L., Laranjo, N., & Stubbs, B. J. (2023b). Trial of the MIND diet for prevention of cognitive decline in older persons. New England Journal of Medicine, 389(7), 602–611. [Google Scholar] [CrossRef] [PubMed]
- Bayes, J., Schloss, J., & Sibbritt, D. (2022). The effect of a Mediterranean diet on the symptoms of depression in young males (the “AMMEND: A Mediterranean Diet in MEN with Depression” study): A randomized controlled trial. The American Journal of Clinical Nutrition, 116(2), 572–580. [Google Scholar] [CrossRef]
- Bizzozero-Peroni, B., Díaz-Goñi, V., Fernández-Rodríguez, R., Martínez-Vizcaíno, V., Jiménez-López, E., Visier-Alfonso, M. E., Garrido-Miguel, M., & Mesas, A. E. (2025). Plant-based diets and mental and neurocognitive health outcomes: A systematic review with meta-analysis. Nutrition Reviews, nuaf080. [Google Scholar] [CrossRef]
- Brinkworth, G. D., Luscombe-Marsh, N. D., Thompson, C. H., Noakes, M., Buckley, J. D., Wittert, G., & Wilson, C. J. (2016). Long-term effects of very low-carbohydrate and high-carbohydrate weight-loss diets on psychological health in obese adults with type 2 diabetes: Randomized controlled trial. Journal of Internal Medicine, 280(4), 388–397. [Google Scholar] [CrossRef] [PubMed]
- Brown, E. E., Gerretsen, P., Pollock, B., & Graff-Guerrero, A. (2018). Psychiatric benefits of lithium in water supplies may be due to protection from the neurotoxicity of lead exposure. Medical Hypotheses, 115, 94–102. [Google Scholar] [CrossRef]
- Bulkes, N. Z., Davis, K., Kay, B., & Riemann, B. C. (2022). Comparing efficacy of telehealth to in-person mental health care in intensive-treatment-seeking adults. Journal of Psychiatric Research, 145, 347–352. [Google Scholar] [CrossRef]
- Cagigas, M. L., De Ciutiis, I., Masedunskas, A., & Fontana, L. (2025). Dietary and pharmacological energy restriction and exercise for healthspan extension. Trends in Endocrinology & Metabolism, 36(6), 521–545. [Google Scholar] [CrossRef]
- Caprio, M., Moriconi, E., Camajani, E., Feraco, A., Marzolla, V., Vitiello, L., Proietti, S., Armani, A., Gorini, S., & Mammi, C. (2023). Very-low-calorie ketogenic diet vs hypocaloric balanced diet in the prevention of high-frequency episodic migraine: The EMIKETO randomized, controlled trial. Journal of Translational Medicine, 21(1), 692. [Google Scholar] [CrossRef]
- Carcelén-Fraile, M. d. C., Déniz-Ramírez, N. d. P., Sabina-Campos, J., Aibar-Almazán, A., Rivas-Campo, Y., González-Martín, A. M., & Castellote-Caballero, Y. (2024). Exercise and nutrition in the mental health of the older adult population: A randomized controlled clinical trial. Nutrients, 16(11), 1741. [Google Scholar] [CrossRef] [PubMed]
- Casas, I., Nakaki, A., Pascal, R., Castro-Barquero, S., Youssef, L., Genero, M., Benitez, L., Larroya, M., Boutet, M. L., & Casu, G. (2023). Effects of a mediterranean diet intervention on maternal stress, well-being, and sleep quality throughout gestation—The IMPACT-BCN trial. Nutrients, 15(10), 2362. [Google Scholar] [CrossRef] [PubMed]
- Chang de Pinho, I., Giorelli, G., & Oliveira Toledo, D. (2024). A narrative review examining the relationship between mental health, physical activity, and nutrition. Discover Psychology, 4(1), 162. [Google Scholar] [CrossRef]
- Chawla, G. (2018). Boosting mental health through dietary intake. Indian Journal of Health and Wellbeing, 9(2), 312–313. [Google Scholar]
- Chen, H., Cao, Z., Hou, Y., Yang, H., Wang, X., & Xu, C. (2023). The associations of dietary patterns with depressive and anxiety symptoms: A prospective study. BMC Medicine, 21(1), 307. [Google Scholar] [CrossRef]
- Ciappolino, V., Mazzocchi, A., Botturi, A., Turolo, S., Delvecchio, G., Agostoni, C., & Brambilla, P. (2019). The role of docosahexaenoic acid (DHA) on cognitive functions in psychiatric disorders. Nutrients, 11(4), 769. [Google Scholar] [CrossRef]
- Dahiya, D., & Nigam, P. S. (2023). Therapeutic and dietary support for gastrointestinal tract using kefir as a nutraceutical beverage: Dairy-milk-based or plant-sourced kefir probiotic products for vegan and lactose-intolerant populations. Fermentation, 9(4), 388. [Google Scholar] [CrossRef]
- Damiani, F., Cornuti, S., & Tognini, P. (2023). The gut-brain connection: Exploring the influence of the gut microbiota on neuroplasticity and neurodevelopmental disorders. Neuropharmacology, 231, 109491. [Google Scholar] [CrossRef]
- Daneshzad, E., Heshmati, J., Basirat, V., Keshavarz, S.-A., Qorbani, M., Larijani, B., Bellissimo, N., & Azadbakht, L. (2022). The effect of the dietary approaches to stop hypertension (DASH) diet on sleep, mental health, and hormonal changes: A randomized clinical trial in women with type 2 diabetes. Frontiers in Nutrition, 9, 775543. [Google Scholar] [CrossRef] [PubMed]
- De Martinis, M., Sirufo, M. M., Suppa, M., & Ginaldi, L. (2020). New perspectives in food allergy. International Journal of Molecular Sciences, 21(4), 1474. [Google Scholar] [CrossRef] [PubMed]
- Doaei, S., Bourbour, F., Teymoori, Z., Jafari, F., Kalantari, N., Torki, S. A., Ashoori, N., Gorgani, S. N., & Gholamalizadeh, M. (2021). The effect of omega-3 fatty acids supplementation on social and behavioral disorders of children with autism: A randomized clinical trial. Pediatric Endocrinology Diabetes and Metabolism, 27(1), 12–18. [Google Scholar] [CrossRef]
- Dolatkhah, N., Toopchizadeh, V., Barmaki, S., Salekzamani, Y., Najjari, A., Farshbaf-Khalili, A., & Dolati, S. (2023). The effect of an anti-inflammatory in comparison with a low caloric diet on physical and mental health in overweight and obese women with knee osteoarthritis: A randomized clinical trial. European Journal of Nutrition, 62(2), 659–672. [Google Scholar] [CrossRef]
- Fan, Y., Fan, A., Yang, Z., & Fan, D. (2025). Global burden of mental disorders in 204 countries and territories, 1990–2021: Results from the global burden of disease study 2021. BMC Psychiatry, 25(1), 486. [Google Scholar] [CrossRef] [PubMed]
- Firth, J., Gangwisch, J. E., Borsini, A., Wootton, R. E., & Mayer, E. A. (2020). Food and mood: How do diet and nutrition affect mental wellbeing? BMJ, 369, m2382. [Google Scholar] [CrossRef]
- Föcker, M., Antel, J., Grasemann, C., Führer, D., Timmesfeld, N., Öztürk, D., Peters, T., Hinney, A., Hebebrand, J., & Libuda, L. (2018). Effect of an vitamin D deficiency on depressive symptoms in child and adolescent psychiatric patients—A randomized controlled trial: Study protocol. BMC Psychiatry, 18(1), 57. [Google Scholar] [CrossRef]
- Ghalichi, F., Ghaemmaghami, J., Malek, A., & Ostadrahimi, A. (2016). Effect of gluten free diet on gastrointestinal and behavioral indices for children with autism spectrum disorders: A randomized clinical trial. World Journal of Pediatrics, 12(4), 436–442. [Google Scholar] [CrossRef] [PubMed]
- Gheonea, T. C., Oancea, C.-N., Mititelu, M., Lupu, E. C., Ioniță-Mîndrican, C.-B., & Rogoveanu, I. (2023). Nutrition and mental well-being: Exploring connections and holistic approaches. Journal of Clinical Medicine, 12(22), 7180. [Google Scholar] [CrossRef]
- Głąbska, D., Guzek, D., Jílková, A., Kołota-Burdzy, A., Skolmowska, D., & Kouřimská, L. (2025). Influence of lycopene intake on mental health: A systematic review of Randomized Controlled Trials (RCTs). Nutrients, 17(11), 1793. [Google Scholar] [CrossRef]
- Godos, J., Bonaccio, M., Al-Qahtani, W. H., Marx, W., Lane, M. M., Leggio, G. M., & Grosso, G. (2023). Ultra-processed food consumption and depressive symptoms in a Mediterranean cohort. Nutrients, 15(3), 504. [Google Scholar] [CrossRef] [PubMed]
- Godos, J., Currenti, W., Angelino, D., Mena, P., Castellano, S., Caraci, F., Galvano, F., Del Rio, D., Ferri, R., & Grosso, G. (2020). Diet and mental health: Review of the recent updates on molecular mechanisms. Antioxidants, 9(4), 346. [Google Scholar] [CrossRef]
- Gómez-Donoso, C., Sánchez-Villegas, A., Martínez-González, M. A., Gea, A., Mendonça, R. d. D., Lahortiga-Ramos, F., & Bes-Rastrollo, M. (2020). Ultra-processed food consumption and the incidence of depression in a Mediterranean cohort: The SUN Project. European Journal of Nutrition, 59, 1093–1103. [Google Scholar] [CrossRef]
- Grider, H. S., Douglas, S. M., & Raynor, H. A. (2021). The influence of mindful eating and/or intuitive eating approaches on dietary intake: A systematic review. Journal of the Academy of Nutrition and Dietetics, 121(4), 709–727.e701. [Google Scholar] [CrossRef] [PubMed]
- Haghighatdoost, F., Mahdavi, A., Mohammadifard, N., Hassannejad, R., Najafi, F., Farshidi, H., Lotfizadeh, M., Kazemi, T., Karimi, S., & Roohafza, H. (2023). The relationship between a plant-based diet and mental health: Evidence from a cross-sectional multicentric community trial (LIPOKAP study). PLoS ONE, 18(5), e0284446. [Google Scholar] [CrossRef]
- Higgins, J. P. T., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., Savovi’c, J., Schulz, K. F., Weeks, L., & Sterne, J. A. C. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 343, d5928. [Google Scholar] [CrossRef]
- Huberts-Bosch, A., Bierens, M., Rucklidge, J. J., Ly, V., Donders, R., van de Loo-Neus, G. H., Arias-Vasquez, A., Klip, H., Buitelaar, J. K., & van den Berg, S. W. (2025). Effects of an elimination diet and a healthy diet in children with Attention-Deficit/Hyperactivity Disorder: 1-Year prospective follow-up of a two-arm randomized, controlled study (TRACE study). JCPP Advances, 5(1), e12257. [Google Scholar] [CrossRef]
- Hysing, M., Kvestad, I., Kjellevold, M., Kolden Midtbø, L., Graff, I. E., Lie, Ø., Hurum, H., Stormark, K. M., & Øyen, J. (2018). Fatty fish intake and the effect on mental health and sleep in preschool children in FINS-KIDS, a randomized controlled trial. Nutrients, 10(10), 1478. [Google Scholar] [CrossRef]
- Jacka, F. N., O’Neil, A., Opie, R., Itsiopoulos, C., Cotton, S., Mohebbi, M., Castle, D., Dash, S., Mihalopoulos, C., & Chatterton, M. L. (2017). A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Medicine, 15, 23. [Google Scholar] [CrossRef] [PubMed]
- Kahleova, H., Rembert, E., Alwarith, J., Yonas, W. N., Tura, A., Holubkov, R., Agnello, M., Chutkan, R., & Barnard, N. D. (2020). Effects of a low-fat vegan diet on gut microbiota in overweight individuals and relationships with body weight, body composition, and insulin sensitivity. A randomized clinical trial. Nutrients, 12(10), 2917. [Google Scholar] [CrossRef] [PubMed]
- Kamrani, F., Kachouei, A. A., Sobhani, S. R., & Khosravi, M. (2024). Nourishing the mind: How the EAT-Lancet reference diet (ELD) and MIND diet impact stress, anxiety, and depression. BMC Psychiatry, 24(1), 709. [Google Scholar] [CrossRef] [PubMed]
- Kao, L. S., Tyson, J. E., Blakely, M. L., & Lally, K. P. (2008). Clinical research methodology I: Introduction to randomized trials. Journal of the American College of Surgeons, 206(2), 361–369. [Google Scholar] [CrossRef]
- Kuroda, Y., Matsuzaki, K., Wakatsuki, H., Shido, O., Harauma, A., Moriguchi, T., Sugimoto, H., Yamaguchi, S., Yoshino, K., & Hashimoto, M. (2019). Influence of ultra-high hydrostatic pressurizing brown rice on cognitive functions and mental health of elderly Japanese individuals: A 2-year randomized and controlled trial. Journal of Nutritional Science and Vitaminology, 65, S80–S87. [Google Scholar] [CrossRef]
- Lee, M. F., Orr, R., Marx, W., Jacka, F. N., O’Neil, A., Lane, M. M., & Ashtree, D. N. (2025). The association between dietary exposures and anxiety symptoms: A prospective analysis of the Australian longitudinal study on women’s health cohort. Journal of Affective Disorders, 389, 119651. [Google Scholar] [CrossRef]
- Li, S., Chen, K., Liu, C., Bi, J., He, Z., Luo, R., Yu, Y., & Wang, Z. (2021). Dietary diversity and mental health in preschoolers in rural China. Public Health Nutrition, 24(7), 1869–1876. [Google Scholar] [CrossRef]
- Liu, X., Morris, M. C., Dhana, K., Ventrelle, J., Johnson, K., Bishop, L., Hollings, C. S., Boulin, A., Laranjo, N., & Stubbs, B. J. (2021). Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) study: Rationale, design and baseline characteristics of a randomized control trial of the MIND diet on cognitive decline. Contemporary Clinical Trials, 102, 106270. [Google Scholar] [CrossRef]
- Longhitano, C., Finlay, S., Peachey, I., Swift, J.-L., Fayet-Moore, F., Bartle, T., Vos, G., Rudd, D., Shareef, O., & Gordon, S. (2024). The effects of ketogenic metabolic therapy on mental health and metabolic outcomes in schizophrenia and bipolar disorder: A randomized controlled clinical trial protocol. Frontiers in Nutrition, 11, 1444483. [Google Scholar] [CrossRef]
- Mao, Q.-S., Guo, Y.-X., Tian, X.-L., Zhao, H.-L., & Kong, Y.-Z. (2025). Global burden of mental disorders in 204 countries and territories results from the Global Burden of Disease Study 2021. World Journal of Psychiatry, 15(8), 106887. [Google Scholar] [CrossRef]
- Mazahery, H., Conlon, C. A., Beck, K. L., Mugridge, O., Kruger, M. C., Stonehouse, W., Camargo, C. A., Jr., Meyer, B. J., Tsang, B., & Jones, B. (2019). A randomised-controlled trial of vitamin D and omega-3 long chain polyunsaturated fatty acids in the treatment of core symptoms of autism spectrum disorder in children. Journal of Autism and Developmental Disorders, 49(5), 1778–1794. [Google Scholar] [CrossRef]
- Meegan, A. P., Perry, I. J., & Phillips, C. M. (2017). The association between dietary quality and dietary guideline adherence with mental health outcomes in adults: A cross-sectional analysis. Nutrients, 9(3), 238. [Google Scholar] [CrossRef]
- Merino, M., Tornero-Aguilera, J. F., Rubio-Zarapuz, A., Villanueva-Tobaldo, C. V., Martín-Rodríguez, A., & Clemente-Suárez, V. J. (2024). Body perceptions and psychological well-being: A review of the impact of social media and physical measurements on self-esteem and mental health with a focus on body image satisfaction and its relationship with cultural and gender factors. Healthcare, 12(14), 1396. [Google Scholar] [CrossRef] [PubMed]
- Mladenović, M., Astolfi, R., Tomašević, N., Matić, S., Božović, M., Sapienza, F., & Ragno, R. (2023). In vitro antioxidant and in vivo antigenotoxic features of a series of 61 essential oils and quantitative composition–activity relationships modeled through machine learning algorithms. Antioxidants, 12(10), 1815. [Google Scholar] [CrossRef]
- Morris, M. C., Tangney, C. C., Wang, Y., Sacks, F. M., Bennett, D. A., & Aggarwal, N. T. (2015). MIND diet associated with reduced incidence of Alzheimer’s disease. Alzheimer’s & Dementia, 11(9), 1007–1014. [Google Scholar]
- Munipalli, B., Strothers, S., Rivera, F., Malavet, P., Mitri, G., Dabrh, A. M. A., & Dawson, N. L. (2022). Association of vitamin B12, vitamin D, and thyroid-stimulating hormone with fatigue and neurologic symptoms in patients with fibromyalgia. Mayo Clinic Proceedings: Innovations, Quality & Outcomes, 6(4), 381–387. [Google Scholar] [CrossRef]
- Muscaritoli, M. (2021). The impact of nutrients on mental health and well-being: Insights from the literature. Frontiers in Nutrition, 8, 656290. [Google Scholar] [CrossRef] [PubMed]
- Nelson, J. B. (2017). Mindful eating: The art of presence while you eat. Diabetes Spectrum: A Publication of the American Diabetes Association, 30(3), 171–174. [Google Scholar] [CrossRef]
- Nouchi, R., Suiko, T., Kimura, E., Takenaka, H., Murakoshi, M., Uchiyama, A., Aono, M., & Kawashima, R. (2020). Effects of lutein and astaxanthin intake on the improvement of cognitive functions among healthy adults: A systematic review of randomized controlled trials. Nutrients, 12(3), 617. [Google Scholar] [CrossRef]
- Oddo, V. M., Welke, L., McLeod, A., Pezley, L., Xia, Y., Maki, P., Koenig, M. D., Kominiarek, M. A., Langenecker, S., & Tussing-Humphreys, L. (2022). Adherence to a Mediterranean diet is associated with lower depressive symptoms among US adults. Nutrients, 14(2), 278. [Google Scholar] [CrossRef]
- Oddy, W. H., Allen, K. L., Trapp, G. S., Ambrosini, G. L., Black, L. J., Huang, R.-C., Rzehak, P., Runions, K. C., Pan, F., & Beilin, L. J. (2018). Dietary patterns, body mass index and inflammation: Pathways to depression and mental health problems in adolescents. Brain, Behavior, and Immunity, 69, 428–439. [Google Scholar] [CrossRef] [PubMed]
- O’Neil, A., Berk, M., Itsiopoulos, C., Castle, D., Opie, R., Pizzinga, J., Brazionis, L., Hodge, A., Mihalopoulos, C., & Chatterton, M. L. (2013). A randomised, controlled trial of a dietary intervention for adults with major depression (the “SMILES” trial): Study protocol. BMC Psychiatry, 13(1), 114. [Google Scholar] [CrossRef] [PubMed]
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. [Google Scholar] [CrossRef]
- Park, M., Choi, J., & Lee, H.-J. (2020). Flavonoid-rich orange juice intake and altered gut microbiome in young adults with depressive symptom: A randomized controlled study. Nutrients, 12(6), 1815. [Google Scholar] [CrossRef]
- Parletta, N., Zarnowiecki, D., Cho, J., Wilson, A., Bogomolova, S., Villani, A., Itsiopoulos, C., Niyonsenga, T., Blunden, S., & Meyer, B. (2019). A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED). Nutritional Neuroscience, 22(7), 474–487. [Google Scholar] [CrossRef]
- Pearl, R. L., Wadden, T. A., Tronieri, J. S., Berkowitz, R. I., Chao, A. M., Alamuddin, N., Leonard, S. M., Carvajal, R., Bakizada, Z. M., & Pinkasavage, E. (2018). Short-and long-term changes in health-related quality of life with weight loss: Results from a randomized controlled trial. Obesity, 26(6), 985–991. [Google Scholar] [CrossRef] [PubMed]
- Petrut, S.-M., Bragaru, A. M., Munteanu, A. E., Moldovan, A.-D., Moldovan, C.-A., & Rusu, E. (2025). Gut over mind: Exploring the powerful gut–brain Axis. Nutrients, 17(5), 842. [Google Scholar] [CrossRef]
- Piwowarczyk, A., Horvath, A., Pisula, E., Kawa, R., & Szajewska, H. (2020). Gluten-free diet in children with autism spectrum disorders: A randomized, controlled, single-blinded trial. Journal of Autism and Developmental Disorders, 50(2), 482–490. [Google Scholar] [CrossRef]
- Prats-Arimon, M., Puig-Llobet, M., Barceló-Peiró, O., Ribot-Domènech, I., Vilalta-Sererols, C., Fontecha-Valero, B., Heras-Ojeda, M., Agüera, Z., Lluch-Canut, T., & Moreno-Poyato, A. (2024). An interdisciplinary intervention based on prescription of physical activity, diet, and positive mental health to promote healthy lifestyle in patients with obesity: A randomized control trial. Nutrients, 16(16), 2776. [Google Scholar] [CrossRef]
- Pretty, J., Rogerson, M., & Barton, J. (2017). Green mind theory: How brain-body-behaviour links into natural and social environments for healthy habits. International Journal of Environmental Research and Public Health, 14(7), 706. [Google Scholar] [CrossRef]
- Puri, S., Shaheen, M., & Grover, B. (2023). Nutrition and cognitive health: A life course approach. Frontiers in Public Health, 11, 1023907. [Google Scholar] [CrossRef]
- Rondinella, D., Raoul, P. C., Valeriani, E., Venturini, I., Cintoni, M., Severino, A., Galli, F. S., Mora, V., Mele, M. C., & Cammarota, G. (2025). The detrimental impact of ultra-processed foods on the human gut microbiome and gut barrier. Nutrients, 17(5), 859. [Google Scholar] [CrossRef]
- Saghafian, F., Hajishafiee, M., Rouhani, P., & Saneei, P. (2023). Dietary fiber intake, depression, and anxiety: A systematic review and meta-analysis of epidemiologic studies. Nutritional Neuroscience, 26(2), 108–126. [Google Scholar] [CrossRef]
- Samanta, S., Sarkar, T., Chakraborty, R., Rebezov, M., Shariati, M. A., Thiruvengadam, M., & Rengasamy, K. R. (2022). Dark chocolate: An overview of its biological activity, processing, and fortification approaches. Current Research in Food Science, 5, 1916–1943. [Google Scholar] [CrossRef] [PubMed]
- Sarma, U., & TR, B. (2024). Dietary phytonutrients in common green leafy vegetables and the significant role of processing techniques on spinach: A review. Food Production, Processing and Nutrition, 6(1), 10. [Google Scholar] [CrossRef]
- Sánchez-Villegas, A., Henríquez-Sánchez, P., Ruiz-Canela, M., Lahortiga, F., Molero, P., Toledo, E., & Martínez-González, M. A. (2015). A longitudinal analysis of diet quality scores and the risk of incident depression in the SUN Project. BMC Medicine, 13(1), 197. [Google Scholar] [CrossRef] [PubMed]
- Schweren, L. J., Larsson, H., Vinke, P. C., Li, L., Kvalvik, L. G., Arias-Vasquez, A., Haavik, J., & Hartman, C. A. (2021). Diet quality, stress and common mental health problems: A cohort study of 121,008 adults. Clinical Nutrition, 40(3), 901–906. [Google Scholar] [CrossRef]
- Smalls-Mantey, A., Verma, D., Nagarajan, R., Agrawal, A., & Merlo, G. (2025). Nutritional interventions in the prevention and treatment of psychiatric disorders. Psychiatric Annals, 55(7), e170–e175. [Google Scholar] [CrossRef]
- Song, Z., Song, R., Liu, Y., Wu, Z., & Zhang, X. (2023). Effects of ultra-processed foods on the microbiota-gut-brain axis: The bread-and-butter issue. Food Research International, 167, 112730. [Google Scholar] [CrossRef]
- Steffens, D. C. (2024). Treatment-resistant depression in older adults. New England Journal of Medicine, 390(7), 630–639. [Google Scholar] [CrossRef]
- Sterne, J. A. C., Hernán, M. A., Reeves, B. C., Savovi’c, J., Berkman, N. D., Viswanathan, M., Henry, D., Altman, D. G., Ansari, M. T., Boutron, I., Carpenter, J. R., Chan, A., Churchill, R., Deeks, J. J., Hróbjartsson, A., Kirkham, J., Jüni, P., Loke, Y. K., Pigott, T. D., … Higgins, J. P. (2016). ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ, 355, i4919. [Google Scholar] [CrossRef]
- Tardy, A.-L., Pouteau, E., Marquez, D., Yilmaz, C., & Scholey, A. (2020). Vitamins and minerals for energy, fatigue and cognition: A narrative review of the biochemical and clinical evidence. Nutrients, 12(1), 228. [Google Scholar] [CrossRef]
- Tavakkoli-Kakhki, M., Eslami, S., & Motavasselian, M. (2015). Nutrient-rich versus nutrient-poor foods for depressed patients based on Iranian Traditional Medicine resources. Avicenna Journal of Phytomedicine, 5(4), 298–308. [Google Scholar]
- Timlin, D., McCormack, J. M., Kerr, M., Keaver, L., & Simpson, E. E. (2025). The MIND diet, cognitive function, and well-being among healthy adults at midlife: A randomised feasibility trial. BMC Nutrition, 11(1), 59. [Google Scholar] [CrossRef] [PubMed]
- Tussing-Humphreys, L., Lamar, M., Blumenthal, J. A., Babyak, M., Fantuzzi, G., Blumstein, L., Schiffer, L., & Fitzgibbon, M. L. (2017). Building research in diet and cognition: The BRIDGE randomized controlled trial. Contemporary Clinical Trials, 59, 87–97. [Google Scholar] [CrossRef]
- Tzekaki, E. E., Tsolaki, M., Geromichalos, G. D., & Pantazaki, A. A. (2021). Extra Virgin Olive Oil consumption from Mild Cognitive Impairment patients attenuates oxidative and nitrative stress reflecting on the reduction of the PARP levels and DNA damage. Experimental Gerontology, 156, 111621. [Google Scholar] [CrossRef] [PubMed]
- Uscher-Pines, L., Raja, P., Qureshi, N., Huskamp, H. A., Busch, A. B., & Mehrotra, A. (2020). Use of tele–mental health in conjunction with in-person care: A qualitative exploration of implementation models. Psychiatric Services, 71(5), 419–426. [Google Scholar] [CrossRef] [PubMed]
- Vaghef-Mehrabany, E., Maleki, V., Behrooz, M., Ranjbar, F., & Ebrahimi-Mameghani, M. (2020). Can psychobiotics “mood” ify gut? An update systematic review of randomized controlled trials in healthy and clinical subjects, on anti-depressant effects of probiotics, prebiotics, and synbiotics. Clinical Nutrition, 39(5), 1395–1410. [Google Scholar] [CrossRef]
- Venkatesan, A., Rahimi, L., Kaur, M., & Mosunic, C. (2020). Digital cognitive behavior therapy intervention for depression and anxiety: Retrospective study. JMIR Mental Health, 7(8), e21304. [Google Scholar] [CrossRef]
- Wade, A. T., Davis, C. R., Dyer, K. A., Hodgson, J. M., Woodman, R. J., Keage, H. A., & Murphy, K. J. (2019). A Mediterranean diet with fresh, lean pork improves processing speed and mood: Cognitive findings from the MedPork randomised controlled trial. Nutrients, 11(7), 1521. [Google Scholar] [CrossRef]
- Wiss, D. A., & LaFata, E. M. (2024). Ultra-processed foods and mental health: Where do eating disorders fit into the puzzle? Nutrients, 16(12), 1955. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y., Qi, X., Jia, Y., Ye, J., Chu, X., Wen, Y., Cheng, B., Cheng, S., Liu, L., & Liang, C. (2023). Evaluating the interactive effects of dietary habits and human gut microbiome on the risks of depression and anxiety. Psychological Medicine, 53(7), 3047–3055. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N., Ju, Z., & Zuo, T. (2018). Time for food: The impact of diet on gut microbiota and human health. Nutrition, 51, 80–85. [Google Scholar] [CrossRef] [PubMed]


| Database | Keywords | MeSH Terms (PubMed) | Initial Articles | Duplicates Removed | Final Articles for Analysis | Contribution to Study | Reason for Inclusion |
|---|---|---|---|---|---|---|---|
| PubMed | “#Mental health,” #Diet, #Mental disorders, #Psychodietetics,” “#Nutripsychiatry,” “#Depression,” “#Lifestyle,” “#Weight,” and “#Obesity”. | #Diet, #Intervention, #Mental health, #Nutrients, #Nutrition | 190 | 48 | 142 | Provided a broad understanding of the interplay between diet, food consumption, dietary interventions and mental health benefits; MeSH terms ensured precision in the search for relevant literature | Widely recognized as a premier biomedical database, frequently used for systematic reviews in healthcare research |
| Web of Science | “#Diet,” “#Mental disorders,” #Psy-chodietetics,” #Neuropsy-chia-try,” “#De-pression,” “#Life-style,” “#Weight,” “#Obesity, “#Food,” and “#Nutrition,” | N/A (Web of Science does not use MeSH terms) | 5 | 3 | 2 | Enhanced the overall coverage of literature related to dietary interventions, and their impact on mental health | Provides a multidisciplinary approach, covering a wide range of scientific disciplines |
| Scopus | “#Diet,” “#Mental disorders,” “#Psy-chodietetics,” #Neuropsychia-try, “#Depression,” “#Lifestyle,” “#Weight,” and “#Obesity.” | #Diet, #Interventions, #Mental health | 12 | 9 | 3 | Strengthened the evidence base by focusing on diet interventions and their impact on mental health; MeSH terms ensured specificity in selecting relevant literature | Renowned for systematic reviews and emphasizing evidence-based interventions in healthcare research |
| Cochrane Library | “# Diet,” “#Interventions,” “#Nutrition,” “#Mental health”, “#Supplementation” and “#Diet” | #Diet, #Interventions, #Mental health | 30 | 28 | 2 | Strengthened the evidence base by focusing on bioactive compounds in meals and snacks related to evidence-based interventions; MeSH terms ensured specificity in selecting relevant literature | Renowned for systematic reviews and emphasizing evidence-based interventions in healthcare research |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Published in English | Non-original research (such as reviews, case reports and practical guidelines) |
| Randomized controlled trials or cohort studies | Not a human study |
| Participants aged 1–18 years old | No comparator group (i.e., control or alternative dietary intervention) |
| Healthy participants or patients with mental disorders (MD) | |
| Studies with a minimum 3-month follow-up and a minimum of 50 participants | Studies published before 2013 |
| Authors | Year | Population | Intervention 1 | Outcomes and Results 2 | References |
|---|---|---|---|---|---|
| Hysing et al. | 2018 | N = 232 preschoolers | Randomized clinical trial. Duration = 16 weeks. Fish intervention; study kids were randomly assigned to lunch meals with fatty fish (herring/mackerel) or meat (chicken/lamb/beef) three times a week. | There was no significant statistical difference between changes in mental health and sleep for the fish-eating group compared with the meat-eating group, neither in the crude analysis nor after adjusting for intake of fish or meat. | (Hysing et al., 2018) |
| Li et al. | 2021 | N = 1334 preschoolers | A cross-sectional survey. Duration: 3 months. Child dietary diversity was assessed with the dietary diversity score (DDS), which was calculated based on nine food groups using a 24 h recall method. | A higher diet diversity was significantly associated with a lower likelihood of having symptoms of hyperactivity/inattention, peer relationship problems and prosocial behavior problems after adjustment for confounders. | (Li et al., 2021) |
| Adams et al. | 2018 | N = 67 children and adults with autism spectrum disorder (ASD) ages 3–58 years | Randomized clinical trial. Duration = 12 months. Treatment began with a special vitamin/mineral supplement, and additional treatments were added sequentially, including essential fatty acids, Epsom salt baths, carnitine, digestive enzymes, and a healthy gluten-free, casein-free, soy-free (HGCSF) diet. | The positive results of this study suggest that a comprehensive nutritional and dietary intervention is effective at improving nutritional status, non-verbal IQ, autism symptoms and other symptoms in most individuals with ASD. Parents reported that the vitamin/mineral supplements, essential fatty acids and HGCSF diet were the most beneficial. | (Adams et al., 2018) |
| Huberts-Bosch et al. | 2025 | N = 165 children with attention-deficit/hyperactivity disorder. | A prospective follow-up of a two-arm randomized, controlled study (TRACE study). Duration = 1 year. An elimination diet and healthy diet in children with attention-deficit/hyperactivity disorder. | 13–15% of teachers, reported lower inattention, hyperactivity–impulsivity and emotion regulation problems after 5 weeks of the intervention compared to both dietary treatments. | (Huberts-Bosch et al., 2025) |
| Oddy et al. | 2018 | N = 843 adolescents at 14 and 17 years (y) of age. | The Western Australian Pregnancy Cohort (Raine) Study. ‘Healthy’ dietary pattern (high in fruit, vegetables, fish, whole-grains). | A ‘Healthy’ dietary pattern was associated with a minimized risk of mental health problems including depressive symptoms in adolescents, through biologically plausible pathways of adiposity and inflammation. | (Oddy et al., 2018) |
| Pearl et al. | 2018 | N = 137 adults with obesity who had lost ≥ 5% of initial weight in a 14-week intensive lifestyle intervention/low-calorie diet. | A randomized clinical trial. Duration = 52 weeks. A structured 1000 to 1200 kcal/d diet that included the daily consumption of four meal-replacement shakes, combined with an evening meal of a frozen-food (or shelf-stable), a garden salad, and two servings of fruit. | Larger weight losses (≥10% of initial weight) were associated with greater overall improvements in physical function, self-esteem and total well-being in patients | (Pearl et al., 2018) |
| Dolatkhah et al. | 2023 | N = 60 overweight and obese women aged 40 years or older with mild-to-moderate osteoarthritis. | A randomized clinical trial. Duration: 24 weeks. An anti-inflammatory and low-calorie diet. | An anti-inflammatory and low-calorie diet resulted in greater weight loss and greater improvements in pain intensity, functional status, depression, anxiety and some dimensions of QoL. | (Dolatkhah et al., 2023) |
| Carcelén-Fraile et al. | 2024 | N = 116 older adults aged 65 or older | Randomized clinical trial. Duration: 12 weeks. Mediterranean diet (Med Diet) (an experimental group undergoing a combined resistance program and Med Diet program and a control group who did not receive any intervention). | Improvements were observed both within and between groups in anxiety, depression, perceived stress, sleep quality, sleep duration, sleep disturbances, use of medications, and the Pittsburgh Sleep Quality Index (PSQI) total score | (Carcelén-Fraile et al., 2024) |
| Tussing-Humphreys et al. | 2017 | N = 180 obese (BMI ≥ 30 kg/m2 and ≤50.0 kg/m2) older adults (55–85 years of age). | A randomized clinical trial. Duration = 8 months. (1) Typical Diet Control; (2) a Med Diet alone (Med Diet-A) lifestyle program; or (3) a Med Diet with lifestyle program to promote weight loss. | Moderate effect sizes on a composite score of executive function, memory and attention in the combined Med diet and weight management group were observed. | (Tussing-Humphreys et al., 2017) |
| Prats-Arimon et al. | 2024 | N = 141 adults with mild–moderate obesity, i.e., with a Body Mass Index (BMI) of 30–40. | Randomized control clinical trials. Duration = 6 months. Adherence to the Med Diet to promote positive mental health in patients with obesity and physical activity. | No significant differences were observed between the control and intervention groups for the following factors: prosocial attitude, self-control, self-esteem and interpersonal relationship skills. However, significant differences were observed in both groups for personal satisfaction, problem solving and updating, and the overall score of the Positive Mental Health (PMH) scale. | (Prats-Arimon et al., 2024) |
| Bayes et al. | 2022 | N = 72 young males (18–25 y) with depression | A randomized clinical trial. Duration: 12 weeks. Med Diet intervention in the treatment of moderate to severe depression. | Significant increases in Mediterranean Diet Adherence Score (MEDAS), decreases in Beck Depression Inventory—version II (BDI-II) score, and increases in Quality of life (QoL) scores. | (Bayes et al., 2022) |
| Wade et al. | 2019 | N = 55 participants aged between 45 and 80 years and at risk of cardiovascular disease. | A randomized clinical trial. Duration: 24 weeks. The MedPork trial was designed to evaluate the cardiovascular and cognitive effects of a Mediterranean diet supplemented with fresh, lean pork. | The modified Mediterranean diet would lead to greater improvements in cognitive functions associated with aging and dementia compared with the control diet. | (Wade et al., 2019) |
| Casas et al. | 2023 | N = 1221 pregnant women at high risk for stress and anxiety. | A randomized clinical trial. Duration = 34–36 weeks. Med diet intervention, Mindfulness-Based Stress Reduction program, or usual care. | A Mediterranean diet intervention during pregnancy is associated with a significant reduction in maternal anxiety and stress, and improvements in sleep quality throughout gestation. | (Casas et al., 2023) |
| Parletta et al. | 2019 | N = 152 adults with depression. | A randomized clinical trial. Duration = 12 weeks. Med diet intervention supplemented with fish oil can improve mental health in adults suffering depression. | There were some correlations between increased omega-3, decreased omega-6 and improved mental health. | (Parletta et al., 2019) |
| Schweren et al. | 2021 | N = 121.008 adults (age 18–93). | A cohort study. Duration = 3.5 years. Lifelines Diet Score is a food-based assessment of overall diet quality, based on international evidence for diet–disease relations and in line with the 2015 Dutch Dietary Guidelines. | Both stress and neuroticism were associated with diet quality, but diet quality in turn did not predict the development of depression/anxiety. | (Schweren et al., 2021) |
| Barnes et al. | 2023 | N = 604 overweight participants between the ages of 65 and 84 with suboptimal diets who are at risk for dementia. | A cohort study. Duration = 3 years. The effects of the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet on a global measure of cognition based on 12 individual cognitive tests. | Pre-pandemic, researchers observed a significant, positive effect of MIND on change in cognition over two years compared to placebo/usual diet. | (Barnes et al., 2023a) |
| Meegan et al. | 2017 | N = 3043 participants. | Cross-sectional study conducted between 2010 and 2011. The DASH score was calculated to examine potential associations between dietary quality, dietary composition and compliance with food pyramid recommendations with depressive symptoms, anxiety and well-being. | Daily fruit and vegetable consumption was higher among those reporting well-being. Those with high dietary quality were more likely to report well-being. | (Meegan et al., 2017) |
| Daneshzad et al. | 2022 | N = 66 women with type 2 diabetes. | A randomized clinical trial. Duration = 12 weeks. The effect of DASH diet on sleep status, mental health and hormonal changes among Iranian women. | Significantly decreases testosterone, post-prandial glucose responses and advanced glycation end product (AGE) levels, as well as sleep, depression and anxiety scores in women with type 2 diabetes. | (Daneshzad et al., 2022) |
| Jacka et al. | 2017 | N = 166 adults with depression. | A randomized clinical trial. Duration = 12 weeks. A total of 21 were using psychotherapy and pharmacotherapy combined; 9 were exclusively using psychotherapy; and 25 were only using pharmacotherapy. There were 31 in the diet support group and 25 in the social support control group who had complete data at 12 weeks. | The dietary support group demonstrated significantly greater improvement between baseline and 12 weeks on the Montgomery–Åsberg Depression Rating Scale (MADRS). | (Jacka et al., 2017) |
| Arab et al. | 2022 | N = 102 women with migraine (20–50 years). | A randomized clinical trial. Duration = 12 weeks. A total of 51 followed the DASH diet, and 51 participated in the usual dietary advice (control) groups. | The QoL and anxiety outcomes remained comparable, but there were improved migraine health outcomes in reproductive-aged women with the DASH diet. | (Arab et al., 2022) |
| Caprio et al. | 2023 | N = 58 adults with a body mass index > 27 kg/m2. | A randomized clinical trial. Duration: 24 weeks. A very low-calorie ketogenic diet (VLCKD) compared to a hypocaloric balanced diet (HBD). | Inflammatory indexes, namely C-reactive protein (CRP), neutrophil-to-lymphocyte ratio (NLR) and total white blood cell count (WBC), were significantly reduced (p < 0.05) in the VLCKD group at week 12. Aldosterone plasma levels were significantly increased in both groups at week 8. | (Caprio et al., 2023) |
| Longhitano et al. | 2024 | Ν = 100 non-hospitalized adult participants with a diagnosis of bipolar disorder, schizoaffective disorder or schizophrenia who were capable of consenting and willing to change their diets. | A randomized clinical trial. Duration = 14 weeks. Κetogenic diet compared to a diet following the Australian Guide to Healthy Eating. | Ketogenic metabolic therapy was well tolerated and resulted in improved psychiatric and metabolic outcomes as well as global measures of social and community functioning. | (Longhitano et al., 2024) |
| Brinkworth et al. | 2016 | N = 150 obese adults with type 2 diabetes. | A randomized controlled diet. Duration = 1 year. Effects of very low-carbohydrate and high-carbohydrate weight-loss diets on psychological health. | Both diets achieved substantial weight loss and comparable improvements in QoL, mood state and affect. | (Brinkworth et al., 2016) |
| Agarwal et al. | 2015 | N = 292 adults with body mass index ≥ 25 kg/m2 and/or previous diagnosis of type 2 diabetes. | A randomized clinical trial. Duration = 18 weeks. Weekly instruction in following a vegan diet or no instruction was given. | A dietary intervention improves depression, anxiety and productivity. | (Agarwal et al., 2015) |
| Kahleov et al. | 2020 | N = 168 overweight adults aged 25 to 75 years. | A randomized clinical trial. Duration = 16 weeks. Low-fat vegan diet. | A low-fat vegan diet induced significant changes in gut microbiota, which were related to changes in weight, body composition and insulin sensitivity in overweight adults. | (Kahleova et al., 2020) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dimopoulou, M.; Dimopoulou, A.; Gortzi, O. Dietary Patterns and Mental Health Across the Lifespan: A Systematic Review of Randomized Clinical Trials. Psychol. Int. 2025, 7, 87. https://doi.org/10.3390/psycholint7040087
Dimopoulou M, Dimopoulou A, Gortzi O. Dietary Patterns and Mental Health Across the Lifespan: A Systematic Review of Randomized Clinical Trials. Psychology International. 2025; 7(4):87. https://doi.org/10.3390/psycholint7040087
Chicago/Turabian StyleDimopoulou, Maria, Aliki Dimopoulou, and Olga Gortzi. 2025. "Dietary Patterns and Mental Health Across the Lifespan: A Systematic Review of Randomized Clinical Trials" Psychology International 7, no. 4: 87. https://doi.org/10.3390/psycholint7040087
APA StyleDimopoulou, M., Dimopoulou, A., & Gortzi, O. (2025). Dietary Patterns and Mental Health Across the Lifespan: A Systematic Review of Randomized Clinical Trials. Psychology International, 7(4), 87. https://doi.org/10.3390/psycholint7040087








