1. Introduction
Esophageal plasmacytoma is not commonly reported in dogs, with only isolated case reports published, and no specific breed, sex, or age predisposition established [
1]. In general, esophageal tumors occur in older animals without clear breed or sex predilection. Primary esophageal tumors are uncommon overall, representing only about 0.08% of all tumors in dogs [
1,
2,
3,
4]. The majority of reported cases include squamous cell carcinoma, leiomyosarcoma, fibrosarcoma, and osteosarcoma, while other tumors such as leiomyoma and plasmacytoma are even less frequently diagnosed [
3,
4,
5,
6]. Plasmacytomas account for approximately 2.4% of all canine neoplasms, and esophageal plasmacytomas represent only around 1% of total plasmacytoma cases [
1]. Reported risk factors for esophageal tumors include chronic irritation and inflammation, vascular ring anomalies causing stricture, esophageal diverticula, parasitic infections such as
Spirocerca lupi, and chronic foreign bodies or reflux injury [
1]. By contrast, extramedullary plasmacytomas are more common in cutaneous and oral forms. These tumors typically affect middle-aged to older dogs, and while certain breeds such as Cocker Spaniels, Scottish Terriers, West Highland White Terriers, and Airedale Terriers appear overrepresented, no consistent sex predilection has been identified. Contributing factors are largely unknown, though immunologic and genetic influences have been suggested [
2].
In dogs, the biological behavior of plasmacytomas varies according to their anatomical location. Cutaneous and oral extramedullary plasmacytomas (EMPs) are generally benign, slow-growing tumors that are well controlled with surgical excision, whereas plasmacytomas of the gastrointestinal tract, spleen or bone may exhibit more aggressive behavior and a greater tendency to progress to multiple myeloma. The risk of metastasis is typically very low for cutaneous and oral tumors, with local recurrence reported in approximately 5% of cases and distant spread in about 2%. However, gastrointestinal and solitary osseous plasmacytomas carry a higher metastatic potential and are more likely to evolve into systemic disease. Treatment options are determined by tumor location and extent, with complete surgical excision being curative in most cutaneous and oral cases, radiotherapy reserved for nonresectable or incompletely excised lesions, and chemotherapy considered primarily in cases of systemic involvement or transformation to multiple myeloma [
1].
EMPs in dogs are generally associated with an excellent prognosis when treated with appropriate local therapy. Complete surgical excision is curative in the majority of cutaneous, oral, and conjunctival cases, with recurrence rates reported at approximately 5% and metastasis occurring in fewer than 2% of patients. In retrospective studies, overall treatment success rates for cutaneous and oral EMPs exceeded 90%, with a large series of 45 oral EMPs showing a median survival of 973 days, although about one-third of cases experienced disease progression, including rare transformation into myeloma [
7]. Incomplete excision without adjuvant therapy is associated with markedly shorter survival (median ~ 138 days) [
7]. Gastrointestinal EMPs demonstrate more variable outcomes with reported median survival around 15 months but good long-term control if complete resection is achieved [
8]. Similarly, conjunctival EMPs have been reported to carry an excellent prognosis, with no recurrence or systemic spread following surgical excision [
9]. Overall, EMPs are considered one of the more treatable plasma cell neoplasms in dogs, with surgery providing long-term disease control in the vast majority of cases, and adjunctive radiation or chemotherapy reserved for nonresectable, recurrent, or atypically aggressive presentations [
10,
11,
12].
Clinical signs are related to esophageal obstruction and most commonly include regurgitation and/or vomiting, but salivation, dysphagia, lethargy, anorexia, and weight loss might also be present. If the mass is ulcerative, melena and secondary anemia may develop. Some dogs may present with respiratory distress due to aspiration pneumonia as a result of regurgitation, and less commonly, due to metastasis [
2,
13]. Indeed, in the previous reported cases, the clinical presentation included regurgitation, ptyalism, hyporexia/anorexia, weight loss, vomiting, cough and retching, and lethargy [
4,
14,
15,
16].
This case report describes the diagnosis, management, and long-term outcome of an esophageal extramedullary plasmacytoma in a dog. This is a quite rare condition, as only four cases have been described in the veterinary literature [
4,
14,
15,
16].
2. Case Description
A nine-year-old, spayed female Poodle-mix dog, weighing 10.5 kg, was presented for evaluation of a five-day history of vomiting and regurgitation of food once per day, occasionally mixed with blood little after feeding time, and hyporexia. Other clinical signs reported by the owner over the past 2 weeks included salivation and possible discomfort during and shortly after feeding.
On physical examination, the dog demonstrated discomfort during the abdominal palpation. Otherwise, the dog was bright and alert, in a good condition, and had a body condition score (BCS) of 5 of 9 scale. The body temperature was 38.6 °C, the capillary refill time was <2 s, no cardiac or respiratory abnormalities were noticed during the auscultation, and no clinical dehydration was noticed. Complete blood count and biochemistry profile did not reveal any significant findings except for a slight increase in hematocrit, creatinine, and blood urea nitrogen. These findings indicate hemoconcentration, probably due to mild non-clinical dehydration (
Table 1). Thoracic radiographs indicated an increased opacity in the esophagus and mild hepatomegaly (
Figure 1).
The dog was scheduled for esophagoscopy under general anesthesia. The dog was premedicated with dexmedetomidine (Dexdomitor, Orion Corporation, Espoo, Finland) in combination with butorphanol (Butomidor, VetViva Richter GmbH, Wels, Austria) intramuscularly (IM). Twenty minutes later, anesthesia was induced with propofol (Propofol-Lipuro 1%, B. Braun Melsungen AG, Kronberg im Taunus, Hesse, Germany) intravenously (IV) followed by incremental doses IV to facilitate tracheal intubation. During endoscopy, anesthesia was maintained with isophlurane (Isoflurin, Vetpharma Animal Health S.L., Barcelona, Spain) in 100% O2 through a circled breathing system.
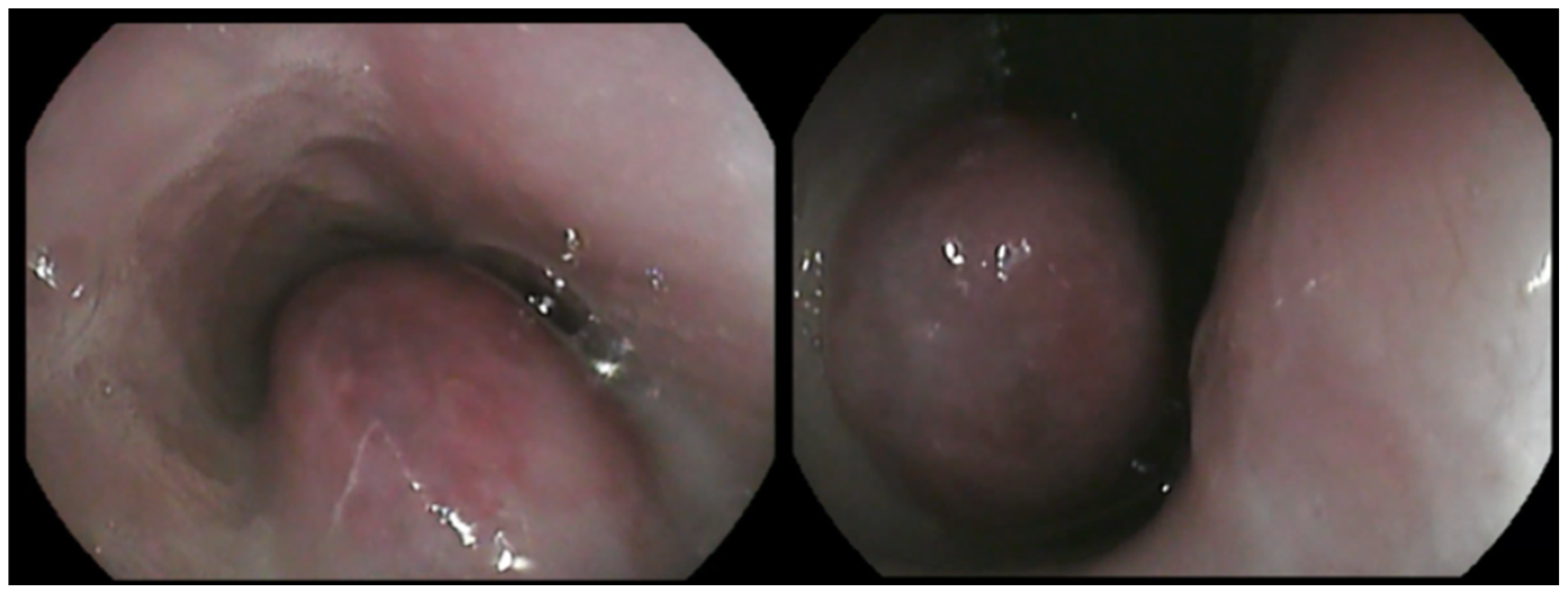
A large, highly vascular, obstructive, solitary mass with a smooth surface was detected (
Figure 2). Endoscopic biopsies of the mass were collected for histopathologic examination. Specifically, seven biopsy samples from stomach, eight from duodenum, and eight from the esophageal mass were obtained using a 2.2 mm biopsy forceps. Biopsy samples were placed in 10% neutral buffered formalin and embedded in paraffin until histopathologic examination. The owner was instructed to feed the dog a high-energy, moist, home-made diet fed from an upright position to facilitate esophageal transit until histopathologic results were available.
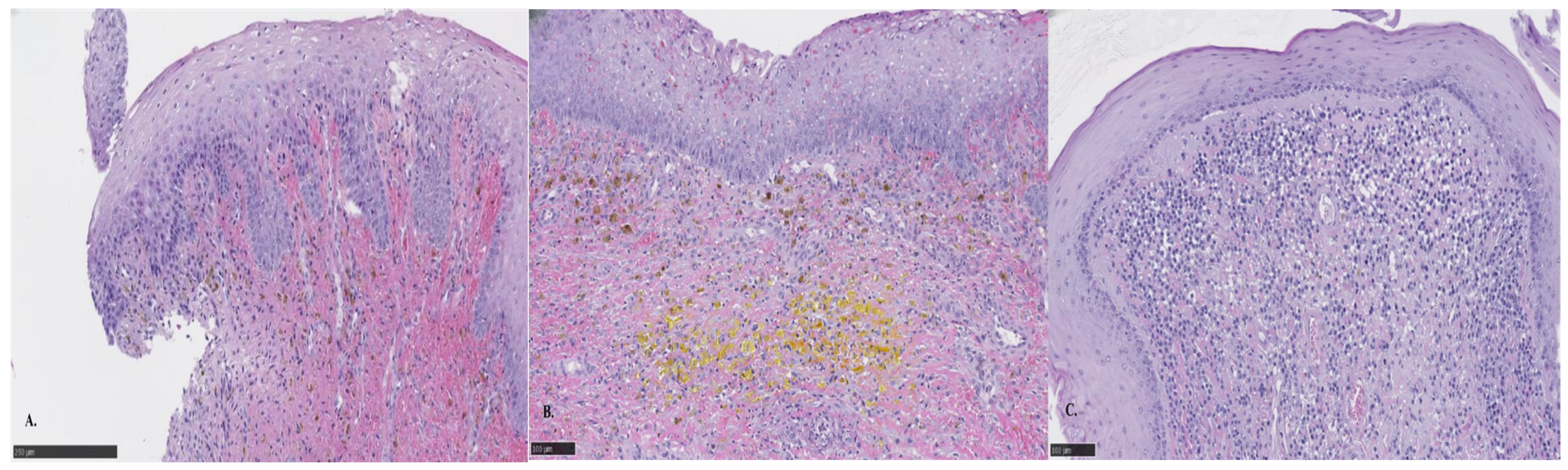
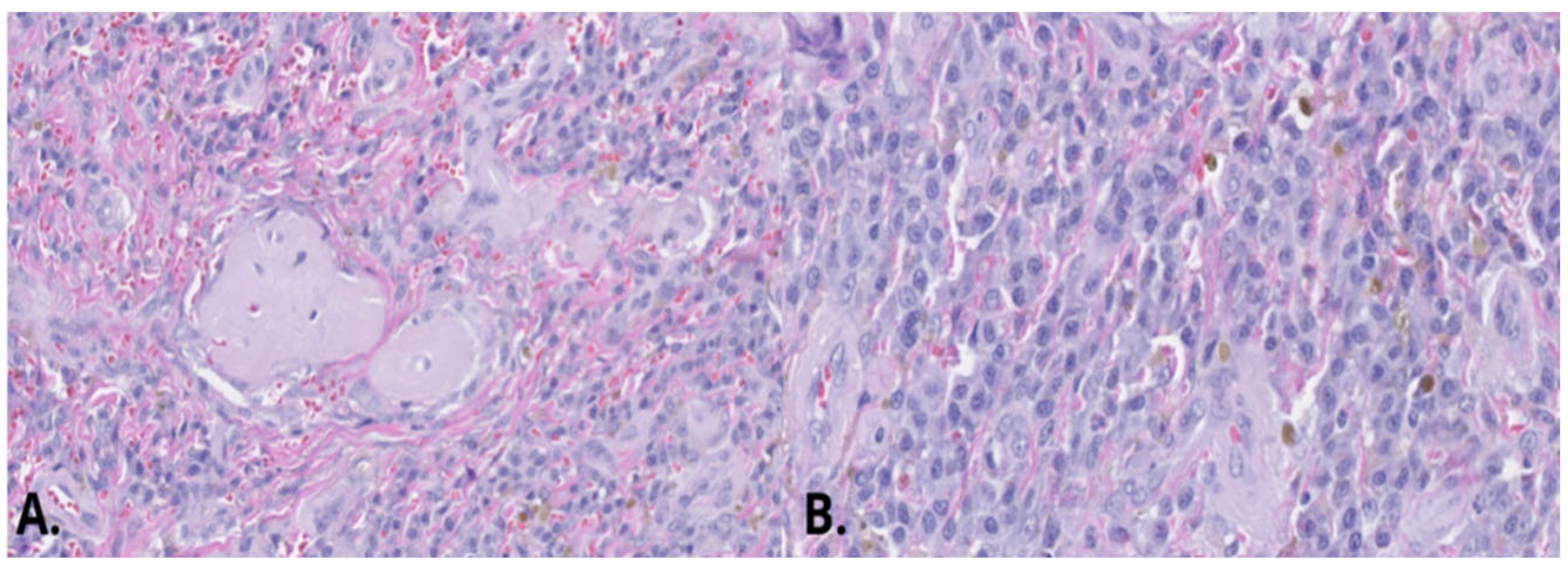
Histopathologic results indicated both proliferative and inflammatory changes suggestive of an inflammatory polyp. These included moderate diffuse chronic lymphocytic, histiocytic, and neutrophilic inflammation, with epithelial hyperplasia, fibroplasia, hemorrhage, and hemosiderin. A dense population of round cells was also noted but interpreted to be part of an inflammatory reaction (
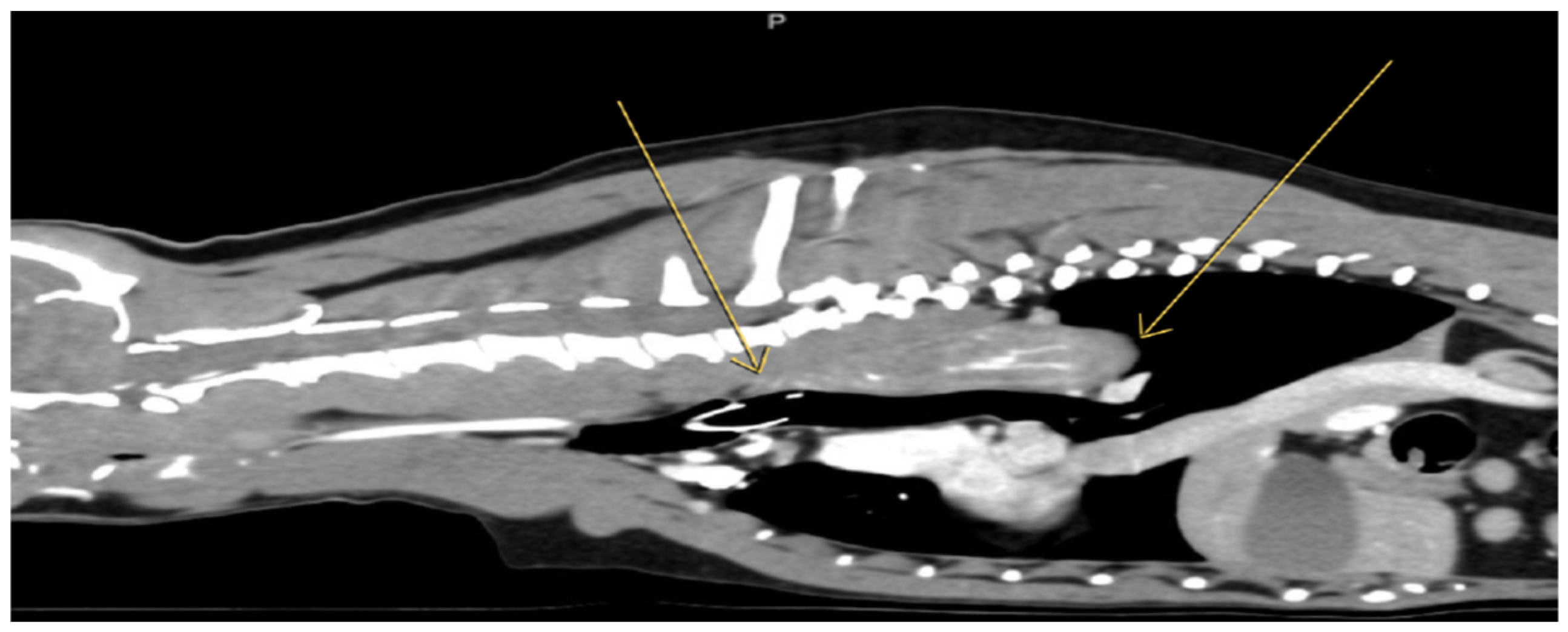
Figure 3). A contrast computed tomography (CT) was performed (
Figure 4) and surgery was recommended for mass removal.
For surgery, the dog was premedicated with acepromazine (Acepromazine maleate, Agroseed Candilidis, Atalanti, Greece) in combination with methadone (Synthadon, Le Vet. Beheer B.V., Oudewater, Utrecht, The Netherlands) IM. Twenty minutes later, anesthesia was induced with propofol (Propofol-Lipuro 1%, B. Braun Melsungen AG, Kronberg im Taunus, Hesse, Germany) IV followed by three incremental doses IV to facilitate tracheal intubation. During surgery, anesthesia was maintained with isoflurane (Isoflurin, Vetpharma Animal Health S.L., Barcelona, Spain) in 100% O2 through a circled breathing system with the ETiso at 1.1–1.3%. A constant rate infusion (CRI) of fentanyl (Fentanyl, DEMO, Athens, Greece) and lidocaine (Xylozan, DEMO, Athens, Greece) was instituted after intubation after a loading dose, and crystalloids (Lactated Ringer’s) were administered throughout the procedure.
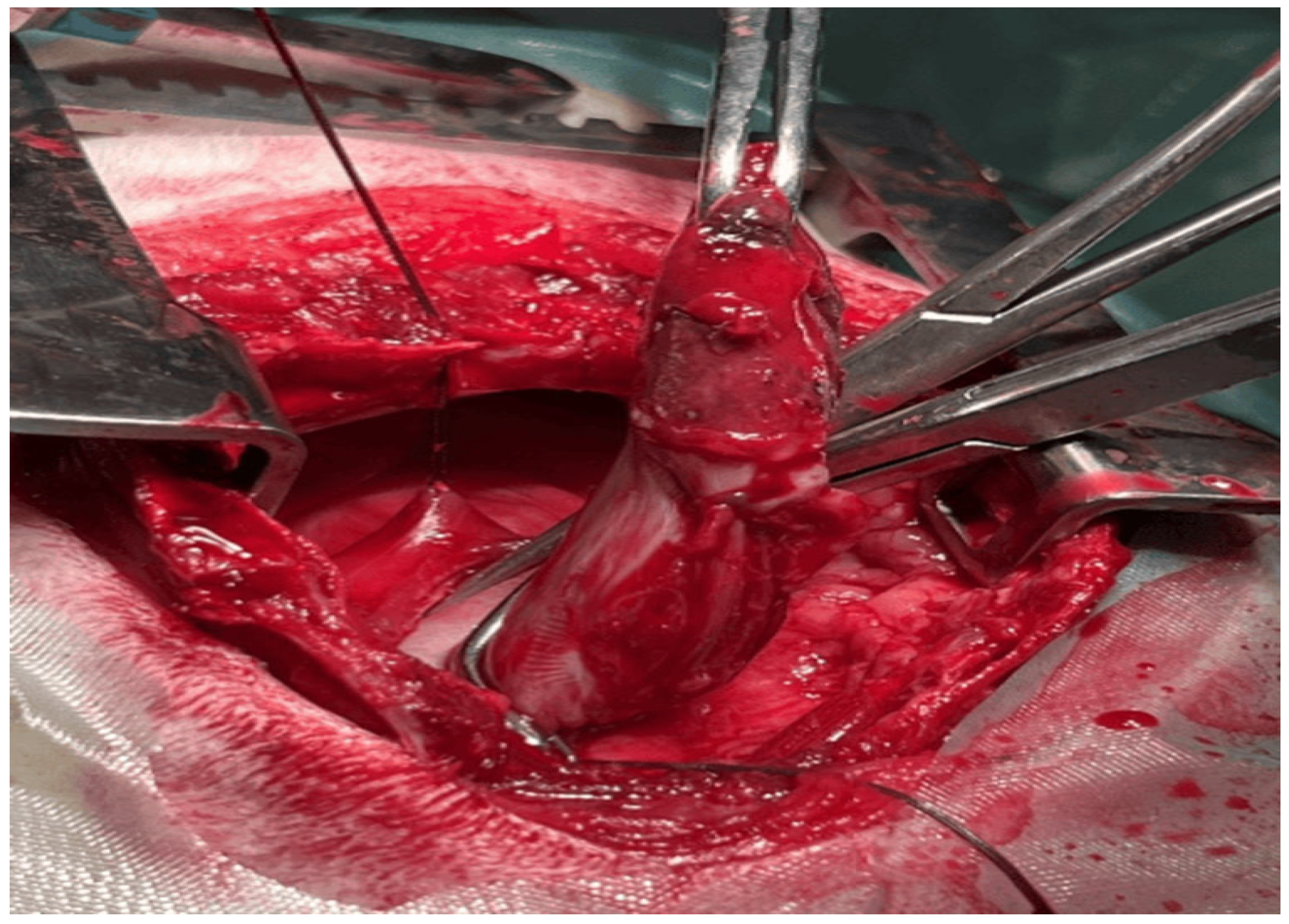
A cranial median sternotomy from the manubrium to the seventh thoracic vertebra was performed to gain access to the mass, which was located between the first and seventh thoracic vertebra (
Figure 5).
The mass was visible from the serosal surface, and a full thickness incision was performed around its base with a 0.5 cm margin. The mass was removed, and closure of the esophagus was performed with a double layer simple continuous pattern with monofilament suture (4-0 polydioxanone). The thoracic cavity was lavaged thoroughly with saline solution at body temperature and a chest tube inserted before closure, which was removed after 24 h as fluid or air were not aspired. A gastrostomy tube was also placed. Levo-bupivacaine (Chirocaine, AbbVie, Athens, Greece) was irrigated in site before closure of the incision.
The analgesic plan consisted of meloxicam (Meloxidyl, CEVA, Lenexa, KS, USA) subcutaneously (SC) once daily for 6 days, methadone (Synthadon, Le Vet. Beheer B.V., Oudewater, Utrecht, The Netherlands) IM three times a day for 2 days, paracetamol (Apotel plus, uniPharma, Athens, Greece) IM twice daily for 5 days. Drug doses used in the protocols above are found in
Appendix A.
The patient was fed via the gastrotomy tube for 10 days and postoperative complications did not occur. Seven days postoperatively and while the dog was still being fed using the gastrotomy tube, the dog was offered small amounts of wet food per os, and at 10 days postoperatively, the gastrostomy tube was removed, while the dog started eating voluntarily.
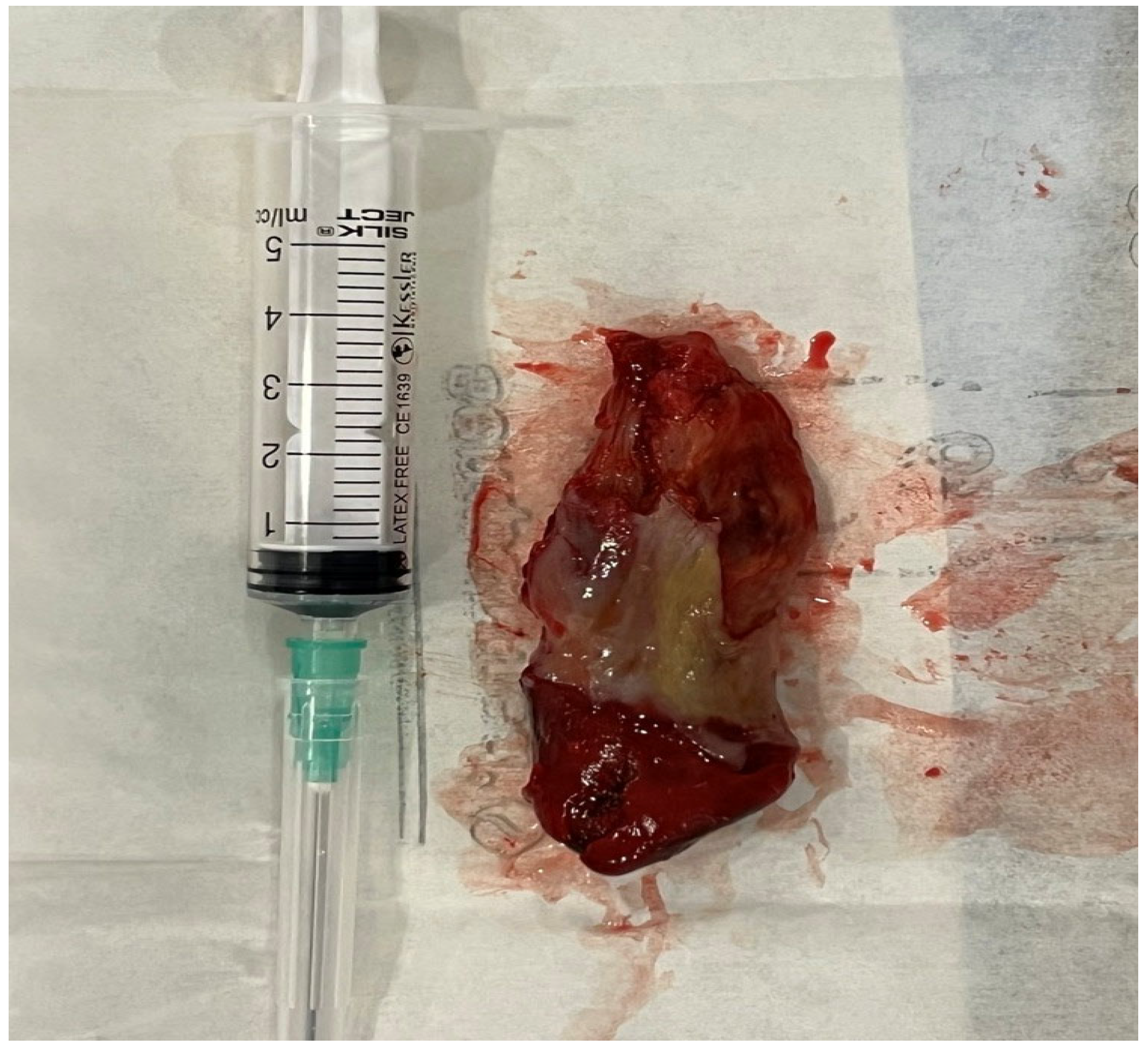
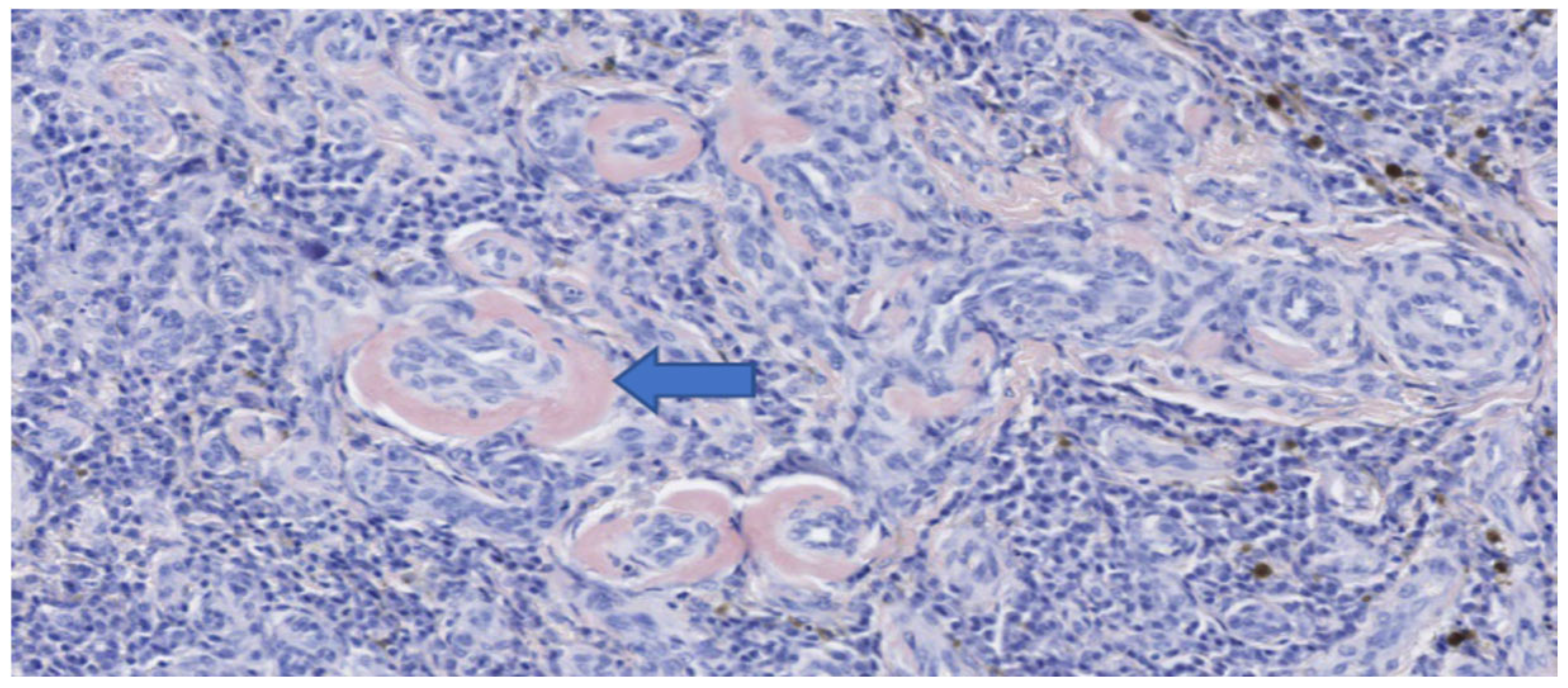
The mass measured approximately 7 cm in length (
Figure 6). Histopathological and immunohistochemical examination of the mass revealed that despite the abundant necrosis and hemorrhage, there was a neoplastic proliferation of plasma cells with extracellular amorphous eosinophilic material interpreted as amyloid based on Congo red staining (
Figure 7 and
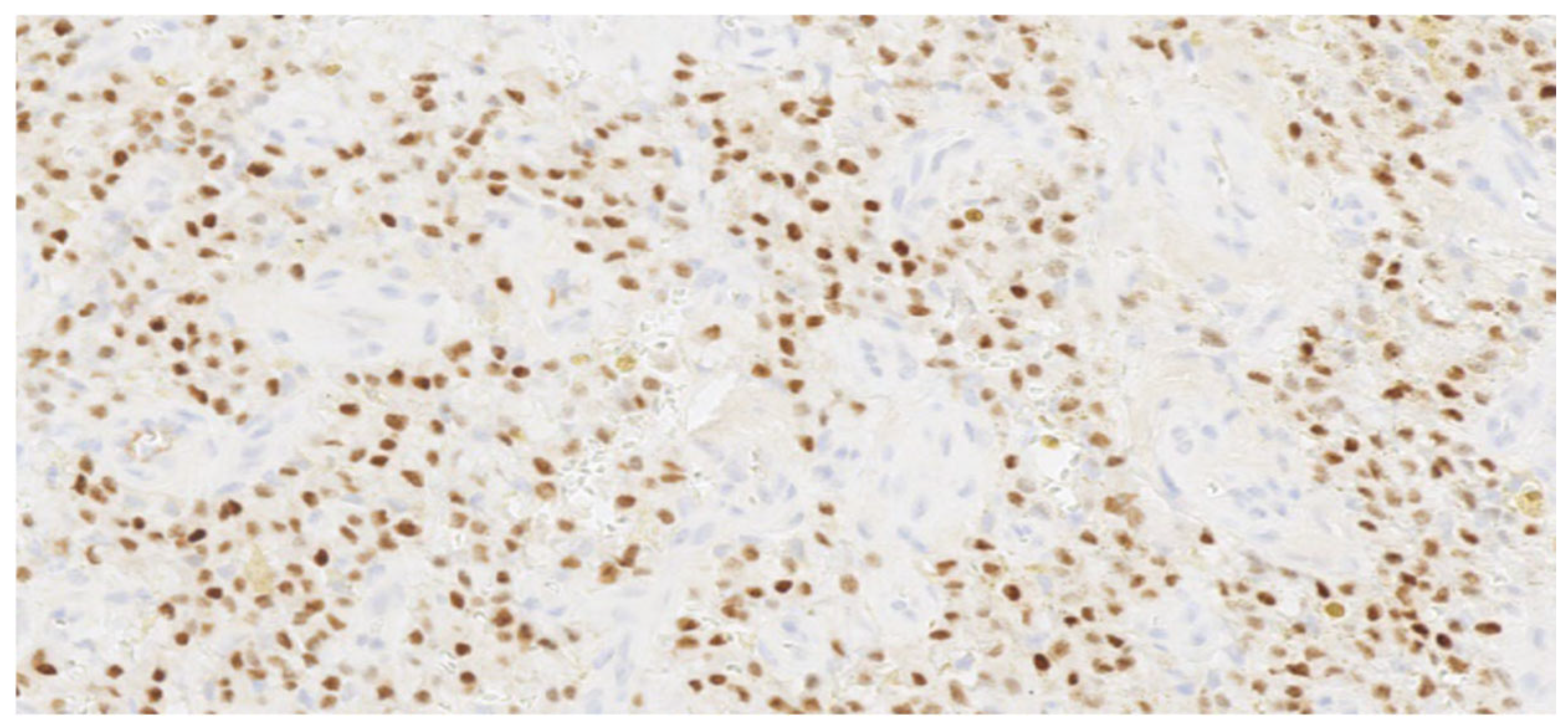
Figure 8). Therefore, a diagnosis of a plasma cell tumor with perivascular amyloid deposition was made. This diagnosis was confirmed by immunohistochemistry (IHC) with a monoclonal anti-multiple myeloma oncogene 1 (MUM-1) antibody (clone MUM1p, Catalog #GA64461-2, Dako Omnis, Agilent, Richmond, VI, USA) (
Figure 9).
Follow-up esophagoscopies were performed every 3–6 months after surgical excision and did not show evidence of tumor regrowth in the esophagus until 18 months after surgery, when recurrence of the mass was identified (
Figure 10). The dog still remains asymptomatic, with the exception of one episode of vomiting and regurgitation, which was resolved after symptomatic treatment.
3. Discussion
This is a case of esophageal plasma cell tumor in a dog. Plasma cell tumors located in the esophagus of dogs are uncommonly reported, with only four cases reported in the literature [
4,
14,
15,
16].
Clinical signs in the dog in our report included regurgitation, vomiting, and occasional hematemesis. These clinical signs are likely driven by partial or complete obstruction of the esophageal lumen, which can lead to weight loss. These signs were similar with the previous reported cases [
4,
14,
16]. The dog reported by Kwon [
15] presented with weight loss and anorexia, which were attributed to the recurrence of oral acanthomatous ameloblastoma, and the esophageal masses were incidental findings. Thus, the more severe signs in this case may be a result of the ameloblastoma and the presence of two esophageal masses.
In our case, surgical removal of the mass was recommended to the owner in order to increase the chances of complete removal of the mass despite its large size. The decision, regarding the surgical approach to the esophagus [
17], was based on the endoscopic and CT information as to the location and extent of the mass attachment to the esophageal wall. The surgeon judged that resection of the part of esophagus invaded by the mass and anastomosis was not possible. Surgical removal of a solitary plasmacytoma, as in our case, is considered the best treatment option when feasible, because it has the potential of complete excision of the tumor, achieving immediate local control and minimizing the risk of recurrence [
1]. Chemotherapy is not indicated as initial treatment since the disease is localized rather than systemic [
1]. Radiotherapy is mainly used when surgery is not possible, providing good local control but with potential late side effects [
2].
Similarly, the dog described in the case by Hamilton [
15] underwent surgical excision of the esophageal mass. In the case of Wood [
16], partial esophagectomy was considered as the best option in order to minimize the possibility of the regrowth of the mass. Moreover, in the case reported by Suarez [
4], the option of complete surgical excision was not acceptable to the dog’s owner. Therefore, laser ablation was performed during endoscopic examination by means of a 10 W diode laser combined with high-frequency monopolar snare for extraction of larger mass fragments. In another report by Kwon [
15], the two masses were endoscopically resected but owners declined chemotherapy with melphalan and prednisolone.
The dog was performing clinically well and follow-up endoscopies did not reveal any evidence of mass regrowth for the first 18 months. However, the follow-up endoscopy at 18 months revealed a minimal regrowth of the mass (
Figure 10). Among the four reported cases of canine esophageal plasmacytoma, recurrence after initial treatment appears uncommon but is variably addressed. In the earliest report [
4], surgical excision was performed, and no recurrence was described in the short-term follow-up (18 months), although no diagnostics were performed to confirm the absence of the regrowth of the mass. However, in one of the reported cases [
4], a recurrence of the mass was documented following the initial therapeutic intervention, highlighting that relapse can occur despite treatment. In another case [
15], they described the endoscopic removal and adjunctive management, with no recurrence noted during 12-month follow-up. However, they did not mention if any diagnostics were performed to confirm the absence of recurrence. In the last case reported [
16], they documented the surgical excision guided by CT and endoscopy, and follow-up confirmed the absence of tumor regrowth after 7 months. Taken together, these reports suggest that when complete excision or effective minimally invasive removal is achieved, esophageal plasmacytomas in dogs may have a favorable prognosis with low risk of recurrence, although the limited number of cases and generally short follow-up periods prevent firm conclusions.
This relapse of the mass will likely affect the long-term prognosis of the dog. Depending on the degree of the obstruction of the esophagus, the clinical signs could return and affect the quality of life of the dog or even lead to death (i.e., in case of aspiration pneumonia). All these could have an impact on the survival time. The owner is considering additional surgery to remove the mass if that is deemed necessary. However, the dog is currently asymptomatic.
It looks like, even with incomplete removal, esophageal plasmacytomas require time to recure. Therefore, absence of mass regrowth cannot be considered definitive until at least 18 months have passed after surgery. Interestingly, the dog in our report remains asymptomatic despite mass regrowth for at least 6 months.
Unfortunately, no further investigation for distant metastases was performed in this case (e.g., abdominal CT, bone marrow aspiration) due to economic reasons. The long-term outcome of this case, however, makes the occurrence of metastases less likely.