Firearm Injuries: A Review of Wound Ballistics and Related Emergency Management Considerations
Abstract
1. Introduction
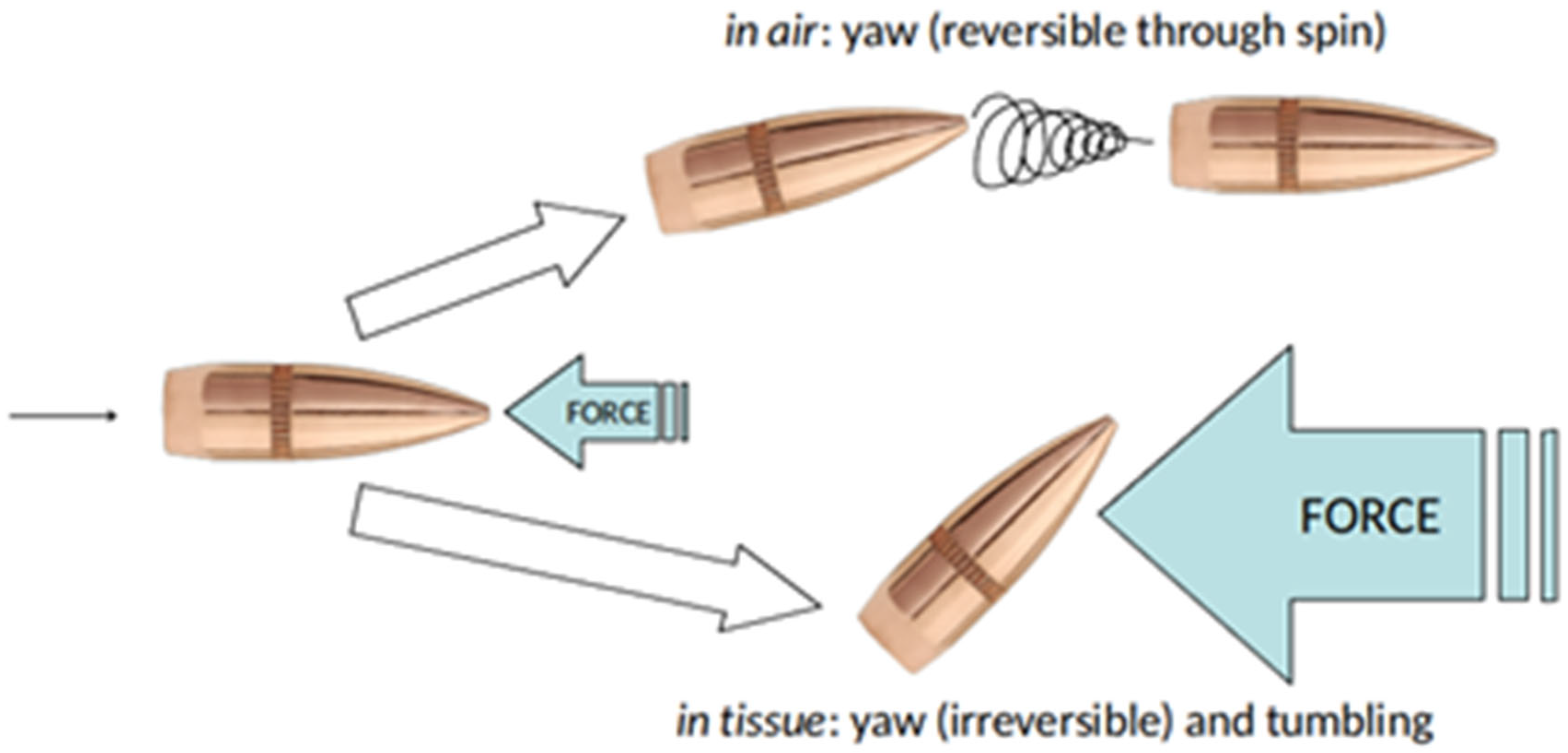
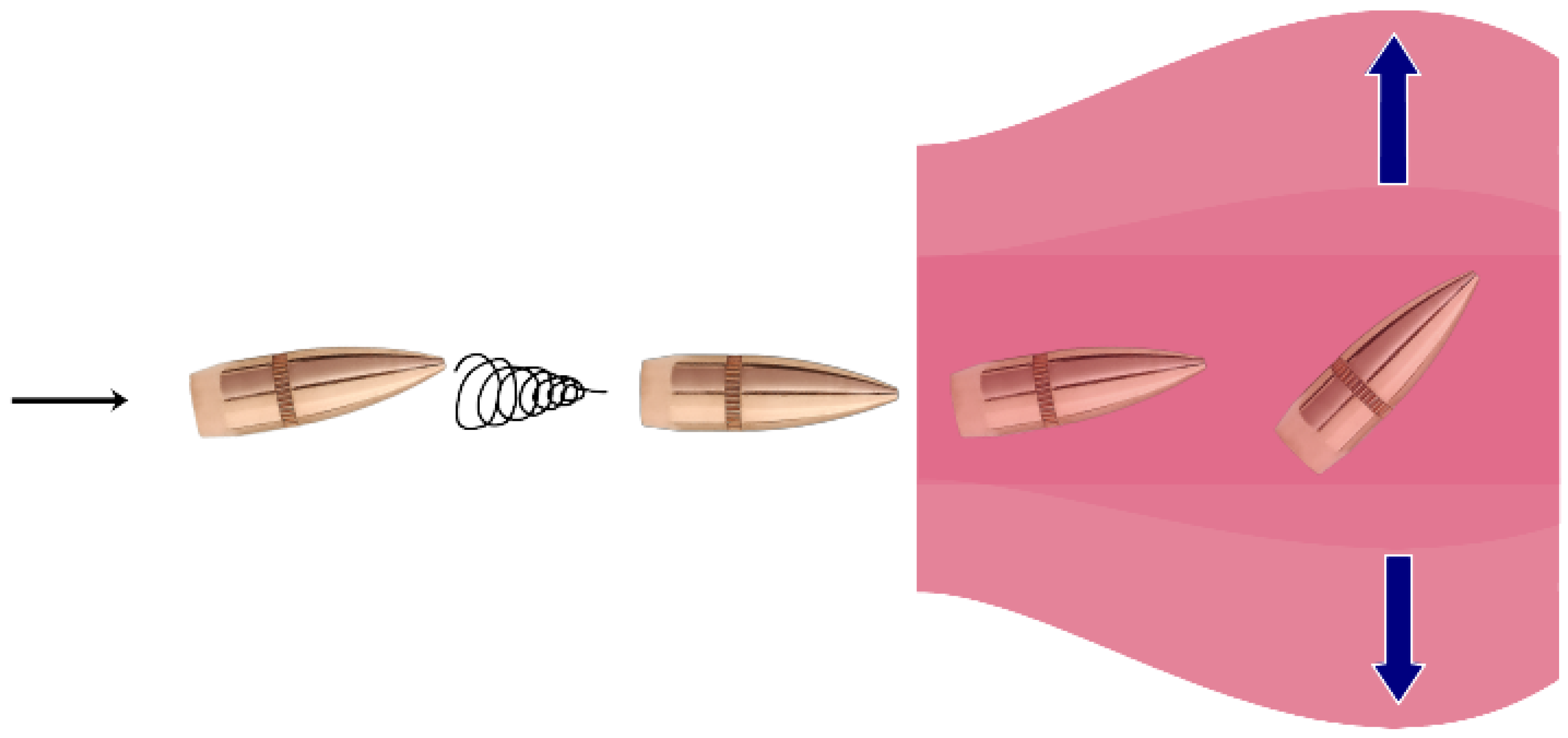
2. Wound Ballistics: The Dynamics and Interaction of Projectiles Penetrating Tissue
2.1. Pathophysiology of Bullet Wounds and Cavitation Injuries
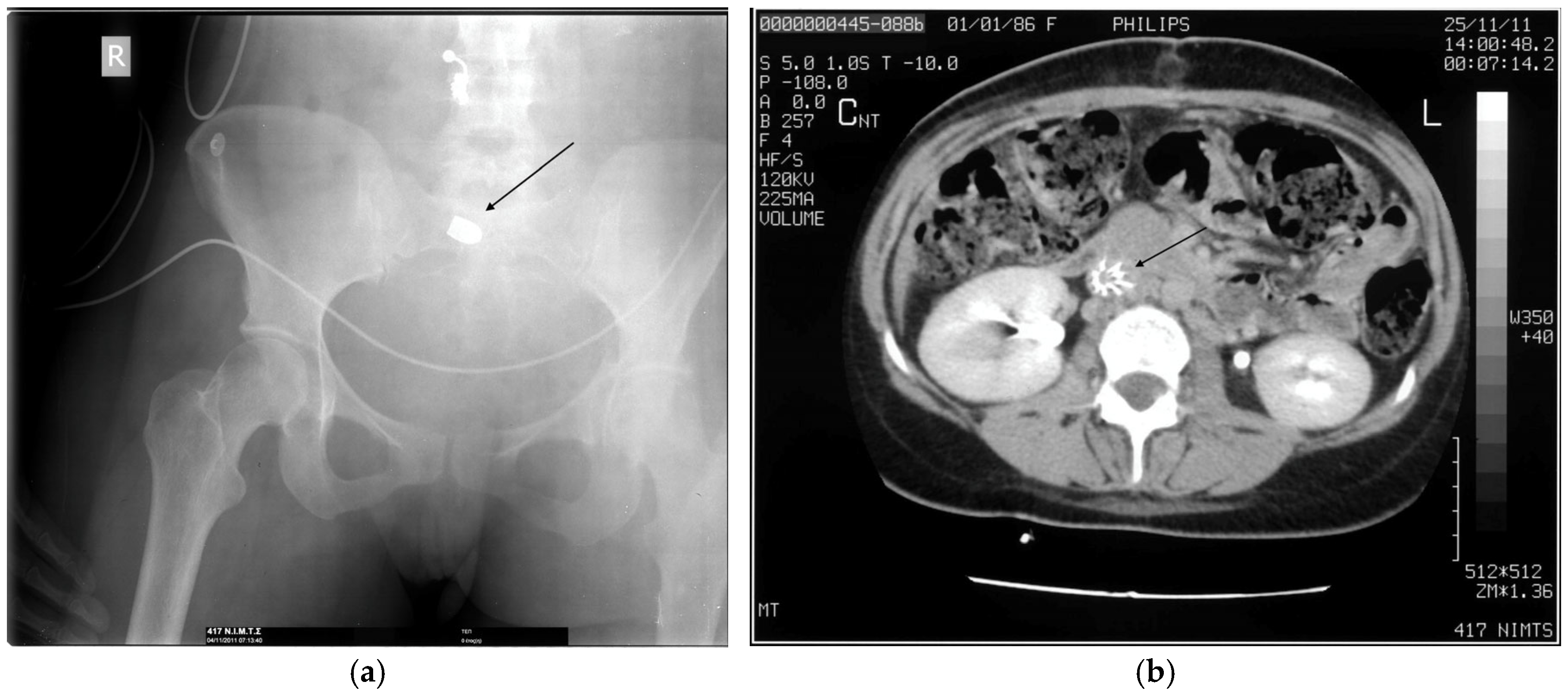
2.2. High Energy Injuries
2.3. Shotgun Injuries
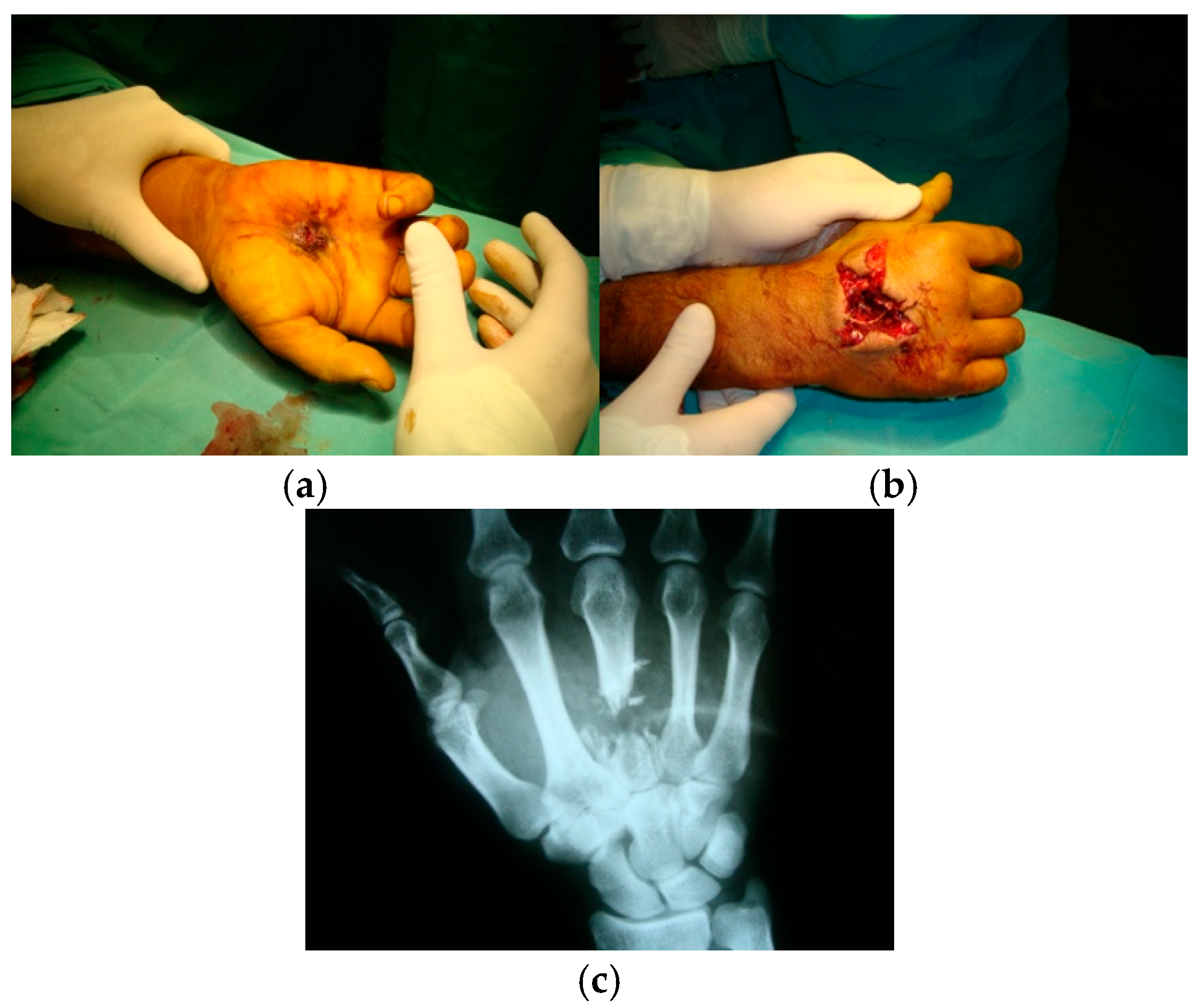
2.4. Bone Injuries
2.5. Infectious Potential of Gunshot Wounds
3. Initial Assessment and Resuscitation
3.1. General Principles
3.2. Hemorrhage Control
3.3. Trajectory Analysis and Imaging
3.4. Management Considerations
3.5. Soft Tissue Wounds
3.6. Removal of Retained Projectiles
3.7. Management of Gunshot Wounds in Regions with Limited Resources
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Johns Hopkins Bloomberg School of Public Health. Firearm Violence in the United States. Available online: https://publichealth.jhu.edu/center-for-gun-violence-solutions/research-reports/gun-violence-in-the-united-states#:~:text=Evidence%20consistently%20shows%20that%20access%20to%20firearms%20increases%20the%20risk%20of%20suicide.&text=Access%20to%20a%20firearm%20in,suicide%20more%20than%20three%2Dfold.&text=Firearms%20are%20dangerous%20when%20someone,most%20lethal%20suicide%20attempt%20method (accessed on 1 July 2025).
- Centers for Disease Control and Prevention. Fast Facts: Firearm Injury and Death. 5 July 2024. Available online: https://www.cdc.gov/firearm-violence/data-research/facts-stats/index.html (accessed on 1 July 2025).
- Rozenfeld, M.; Givon, A.; Rivkind, A.; Bala, M.; Peleg, K.; Alfici, R.; Bahouth, H.; Becker, A.; Jeroukhimov, I.; Karawani, M.; et al. New trends in terrorism-related injury mechanisms: Is there a difference in injury severity? Ann. Emerg. Med. 2019, 74, 697–705. [Google Scholar] [CrossRef]
- Binkley, J.M.; Kemp, K.M. Mobilization of resources and emergency response on the national scale. Surg. Clin. N. Am. 2022, 102, 169–180. [Google Scholar] [CrossRef]
- Ditkofsky, N.; Nair, J.R.; Frank, Y.; Mathur, S.; Nanda, B.; Moreland, R.; Rotman, J.A. Understanding ballistic injuries. Radiol. Clin. N. Am. 2023, 61, 119–128. [Google Scholar] [CrossRef]
- Ferreira, C.; Correia, M. Surgical frontiers in war zones: Perspectives and challenges of a humanitarian surgeon in conflict environments. Trauma Surg. Acute Care Open 2024, 9, e001234. [Google Scholar] [CrossRef]
- Baum, G.R.; Baum, J.T.; Hayward, D.; MacKay, B.J. Gunshot wounds: Ballistics, pathology, and treatment recommendations, with a focus on retained bullets. Orthop. Res. Rev. 2022, 14, 293–317. [Google Scholar] [CrossRef] [PubMed]
- Rhee, P.M.; Moore, E.E.; Joseph, B.; Tang, A.; Pandit, V.; Vercruysse, G. Gunshot wounds: A review of ballistics, bullets, weapons, and myths. J. Trauma Acute Care Surg. 2016, 80, 853–867. [Google Scholar] [CrossRef] [PubMed]
- DiMaio, V.J.M. Gunshot Wounds: Practical Aspects of Firearms, Ballistics, and Forensic Techniques, 3rd ed.; CRC Press: Boca Raton, FL, USA, 2016; ISBN 978-1-4987-2569-9. [Google Scholar]
- Stewart, R.M. ATLS® Advanced Trauma Life Support® Student Course Manual, 10th ed.; American College of Surgeons: Chicago, IL, USA, 2018; ISBN 78-0-9968262-3-5. [Google Scholar]
- Strong, B.L.; Lauerman, M.H.; Scalea, T.M. Sequelae and care after firearm injury. JAMA 2025, 334, 726–727. [Google Scholar] [CrossRef]
- Cestero, R.; Plurad, D.; Demetriades, D. Ballistics. In Color Atlas of Emergency Trauma, 3rd ed.; Demetriades, D., Chudnofsky, C.R., Benjamin, E.R., Eds.; Cambridge University Press: Cambridge, UK, 2021; pp. 247–262. [Google Scholar] [CrossRef]
- Bledsoe, B.E. Mechanism of injury. In Bledsoe’s Paramedic Care: Principles & Practice, 6th ed.; Bledsoe, B.E., Porter, R.S., Cherry, R.A., Eds.; Pearson: Upper Saddle River, NJ, USA, 2023; Volume 2, pp. 1757–1793. ISBN 978-013-691459-4. [Google Scholar]
- Walker, J. Halliday & Resnick Fundamentals of Physics, 12th ed.; Wiley: Hoboken, NJ, USA, 2022; Volume 1, Chapter 7: Kinetic energy and work; pp. 156–185. ISBN 978-1-119-80115-3. [Google Scholar]
- McAninch, J.W.; Santucci, R.A. Renal and ureteral trauma. In Campbell-Walsh Urology, 9th ed.; Kavoussi, L.R., Novick, A.C., Partin, A.W., Peters, C.A., Eds.; Saunders: Philadelphia, PA, USA, 2007; Volume 2, pp. 1274–1292. ISBN 978-0-7216-0798-5. [Google Scholar]
- Karger, B. Forensic ballistics: Injuries from gunshots, explosives and arrows. In Handbook of Forensic Medicine, 2nd ed.; Madea, B., Ed.; Wiley: Chichester, UK, 2022; Volume 2, pp. 459–503. [Google Scholar] [CrossRef]
- Burkhalter, W.E. Orthopedic Surgery in Vietnam; Office of the Surgeon General: Washington, DC, USA, 1994. [Google Scholar]
- Fackler, M.L. Wound ballistics. A review of common misconceptions. JAMA 1988, 259, 2730–2736. [Google Scholar] [CrossRef] [PubMed]
- Hollerman, J.J.; Fackler, M.L. Wound ballistics. In Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7th ed.; Tintinalli, J.E., Ed.; McGraw-Hill: New York, NY, USA, 2011; pp. e38–e43. ISBN 978-0-07-148480-0. [Google Scholar]
- DeMuth, W.E., Jr. Bullet velocity and design as determinants of wounding capability: An experimental study. J. Trauma 1966, 6, 222–232. [Google Scholar] [CrossRef]
- Bruner, D.; Gustafson, C.G.; Visintainer, C. Ballistic injuries in the emergency department. Emerg. Med. Pract. 2011, 13, 1–32. [Google Scholar]
- Ommundsen, H.; Robinson, E.H. Rifles and Ammunition; Cassell: London, UK, 1915; Chapter 10: Sporting Rifle Ammunition; pp. 179–185. [Google Scholar]
- Kneubuehl, B.P. General wound ballistics. In Wound Ballistics: Basics and Applications, 2nd ed.; Kneubuehl, B.P., Ed.; Springer: Berlin, Germany, 2022; pp. 87–163. [Google Scholar] [CrossRef]
- Kneubuehl, B.P. Wound ballistics and international agreements. In Wound Ballistics: Basics and Applications, 2nd ed.; Kneubuehl, B.P., Ed.; Springer: Berlin, Germany, 2022; pp. 337–358. [Google Scholar] [CrossRef]
- Anatoliyovych, I.L.; Yuriyovych, O.U.; Valentynovych, O.H. Surgical treatment features of liver gunshot wound with a dumdum bullet (expanding bullet). Int. J. Emerg. Med. 2022, 15, 57. [Google Scholar] [CrossRef]
- Gumeniuk, K.; Lurin, I.A.; Tsema, I.; Malynovska, L.; Gorobeiko, M.; Dinets, A. Gunshot injury to the colon by expanding bullets in combat patients wounded in hybrid period of the Russian-Ukrainian war during 2014–2020. BMC Surg. 2023, 23, 23. [Google Scholar] [CrossRef] [PubMed]
- Mendelson, J.A. The relationship between mechanisms of wounding and principles of treatment of missile wounds. J. Trauma 1991, 31, 1181–1202. [Google Scholar] [CrossRef] [PubMed]
- Owen-Smith, M.S. High-velocity and military gunshot wounds. In Management of Gunshot Wounds; Ordog, G.J., Ed.; Elsevier: New York, NY, USA, 1988; pp. 61–94. ISBN 0-444-01246-X. [Google Scholar]
- Kneubuehl, B.P. Ballistics: Theory and Practice; Rawcliffe, S., Translator; Springer: Berlin, Germany, 2024; Chapter 2: Physical basics; p. 34. [Google Scholar] [CrossRef]
- Haag, L.C. Base deformation of full metal-jacketed rifle bullets as a measure of impact velocity and range of fire. Am. J. Forensic Med. Pathol. 2015, 36, 16–22. [Google Scholar] [CrossRef]
- Janzon, B. Projectile-material interactions: Simulants. In Scientific Foundations of Trauma; Cooper, G.J., Dudley, H.A.F., Gann, D.S., Little, R.A., Maynard, R.L., Eds.; Butterworth Heinemann: Oxford, UK, 1997; pp. 26–36. ISBN 0 7506 1585 0. [Google Scholar]
- Fackler, M.L.; Surinchak, J.S.; Malinowski, J.A.; Bowen, R.E. Bullet fragmentation: A major cause of tissue disruption. J. Trauma 1984, 24, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Berlin, R.H.; Janzon, B.; Lidén, E.; Nordström, G.; Schantz, B.; Seeman, T.; Westling, F. Terminal behaviour of deforming bullets. J. Trauma 1988, 28, S58–S62. [Google Scholar] [CrossRef]
- MacPherson, D. Bullet Penetration: Modelling the Dynamics and the Incapacitation Resulting from Wound Trauma; Ballistic Publications: El Segundo, CA, USA, 2005; Chapter 4: Incapacitation of bullet wounds; p. 52. ISBN 0-9643577-1-2. [Google Scholar]
- Reginelli, A.; Russo, A.; Maresca, D.; Martiniello, C.; Cappabianca, S.; Brunese, L. Imaging assessment of gunshot wounds. Semin. Ultrasound CT MR 2015, 36, 57–67. [Google Scholar] [CrossRef]
- Altheimer, I.; Schaible, L.M.; Klofas, J.; Comeau, M. Victim characteristics, situational factors, and the lethality of urban gun violence. J. Interpers. Violence 2019, 34, 1633–1656. [Google Scholar] [CrossRef]
- Moritz, A.R. The Pathology of Trauma, 2nd ed.; Lea & Febiger: Philadelphia, PA, USA, 1954; p. 64. [Google Scholar]
- Riddez, L. Wounds of war in the civilian sector: Principles of treatment and pitfalls to avoid. Eur. J. Trauma Emerg. Surg. 2014, 40, 461–468. [Google Scholar] [CrossRef]
- Braga, A.A.; Cook, P.J. The association of firearm caliber with likelihood of death from gunshot injury in criminal assaults. JAMA Netw. Open 2018, 1, e180833. [Google Scholar] [CrossRef]
- Tracqui, A.; Deguette, C.; Delabarde, T.; Delannoy, Y.; Plu, I.; Sec, I.; Hamza, L.; Taccoen, M.; Ludes, B. An overview of forensic operations performed following the terrorist attacks on November 13, 2015, in Paris. Forensic Sci. Res. 2020, 5, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Spitz, W.U.; Diaz, F.J. Spitz and Fisher’s Medicolegal Investigation of Death: Guidelines for the Application of Pathology to Crime Investigation, 5th ed.; Charles C Thomas: Springfield, IL, USA, 2020; Chapter 8: Injury by gunfire; pp. 313–403. ISBN 9780398093129. [Google Scholar]
- DeMuth, W.E., Jr.; Smith, J.M. High-velocity bullet wounds of muscle and bone: The basis of rational early treatment. J. Trauma 1966, 6, 744–755. [Google Scholar] [CrossRef]
- Amato, J.L.; Billy, L.J.; Lawson, N.S.; Rich, N.M. High velocity missile injury. An experimental study of the retentive forces of tissue. Am. J. Surg. 1974, 127, 454–459. [Google Scholar] [CrossRef]
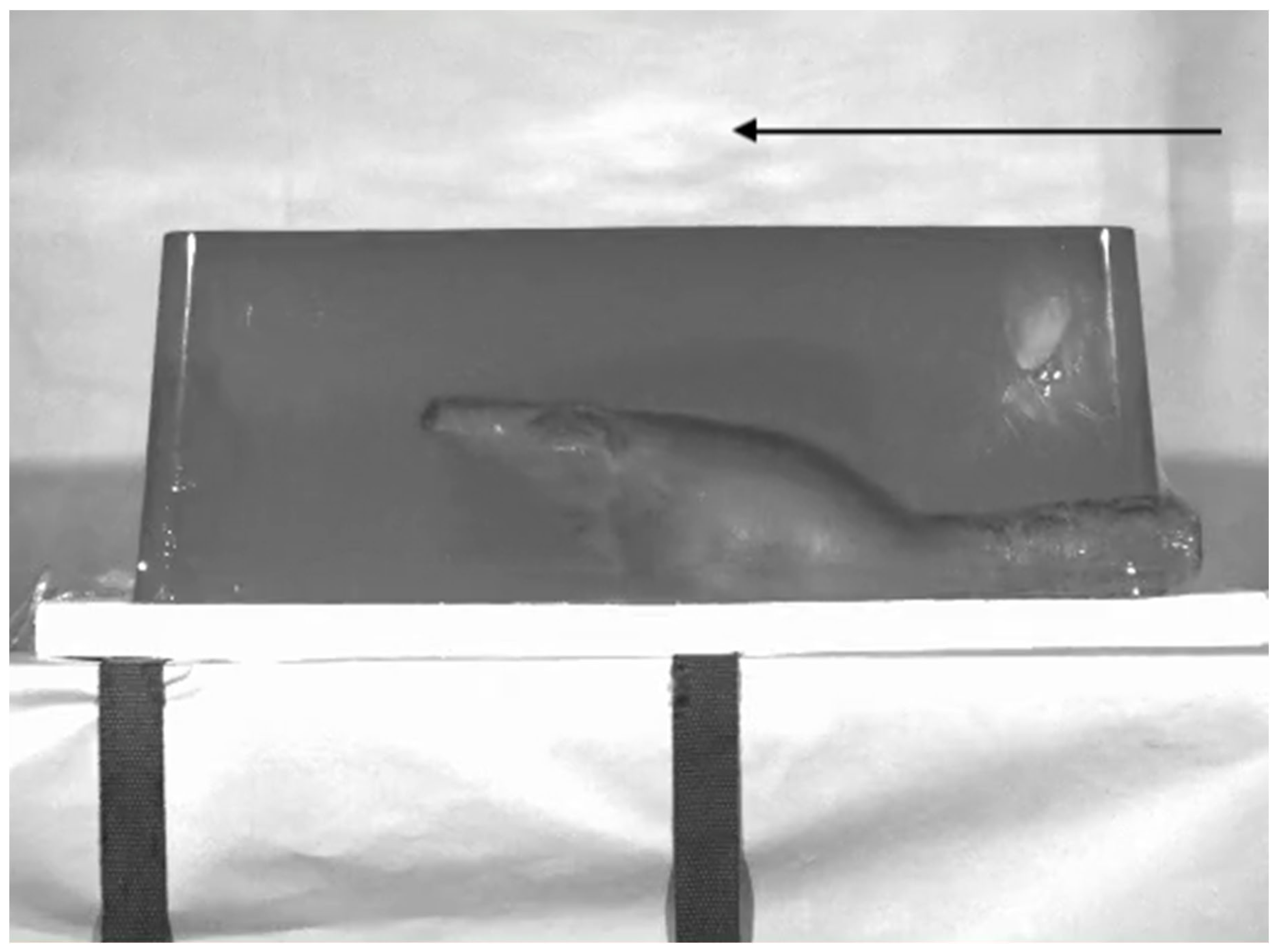
- Wen, Y.; Xu, C.; Jin, Y.; Batra, R.C. Rifle bullet penetration into ballistic gelatin. J. Mech. Behav. Biomed. Mater. 2017, 67, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Stefanopoulos, P.K.; Mikros, G.; Pinialidis, D.E.; Oikonomakis, I.N.; Tsiatis, N.E.; Janzon, B. Wound ballistics of military rifle bullets: An update on controversial issues and associated misconceptions. J. Trauma Acute Care Surg. 2019, 87, 690–698. [Google Scholar] [CrossRef]
- Fackler, M.L.; Surinchak, J.S.; Malinowski, J.A.; Bowen, R.E. Wounding potential of the Russian AK-74 assault rifle. J. Trauma 1984, 24, 263–266. [Google Scholar] [CrossRef]
- Karademir, K.; Gunhan, M.; Can, C. Effects of blast injury on kidneys in abdominal gunshot wounds. Urology 2006, 68, 1160–1163. [Google Scholar] [CrossRef]
- Owers, C.; Garner, J. Intra-abdominal injury from extra-peritoneal ballistic trauma. Injury 2014, 45, 655–658. [Google Scholar] [CrossRef]
- Chai, L.F.; Nahass, M.M.; Iacono, S.A.; Grover, K.; Shan, Y.; Ferraro, J.; Ikegami, H.; Hanna, J.S. Delayed cardiac tamponade secondary to blast injury from gunshot wound. Trauma Case Rep. 2023, 47, 100914. [Google Scholar] [CrossRef] [PubMed]
- Serafetinides, E.S. Renal and ureteric trauma. In Primer on Urology; Chapple, C.R., Wein, A.J., Eds.; Springer: Cham, Switzerland, 2025; pp. 1013–1024. [Google Scholar] [CrossRef]
- Khandar, S.J.; Johnson, S.B.; Calhoon, J.H. Overview of thoracic trauma in the United States. Thorac. Surg. Clin. 2007, 17, 1–9. [Google Scholar] [CrossRef]
- Fischer, R.P.; Geiger, J.P.; Guernsey, J.M. Pulmonary resections for severe pulmonary contusions secondary to high-velocity missile wounds. J. Trauma 1974, 14, 293–302. [Google Scholar] [CrossRef]
- Nicolaou, N.; Conlan, A.A. High-velocity missile injuries of the thorax. S. Afr. Med. J. 1982, 28, 324–328. [Google Scholar]
- Spencer Netto, F.; Pannell, D.; Tien, H.C. Hollow-point ammunition and handguns: The potential for large temporary cavities. Inj. Extra 2008, 39, 50–52. [Google Scholar] [CrossRef]
- Jorgensen, J.J.; Naess, P.A.; Gaarder, C. Injuries caused by fragmenting rifle ammunition. Injury 2016, 47, 1951–1954. [Google Scholar] [CrossRef]
- Zhang, J.; Yoganandan, N.; Pintar, F.A.; Gennarelli, T.A. Temporal cavity and pressure distribution in a brain simulant following ballistic penetration. J. Neurotrauma 2005, 22, 1335–1347. [Google Scholar] [CrossRef]
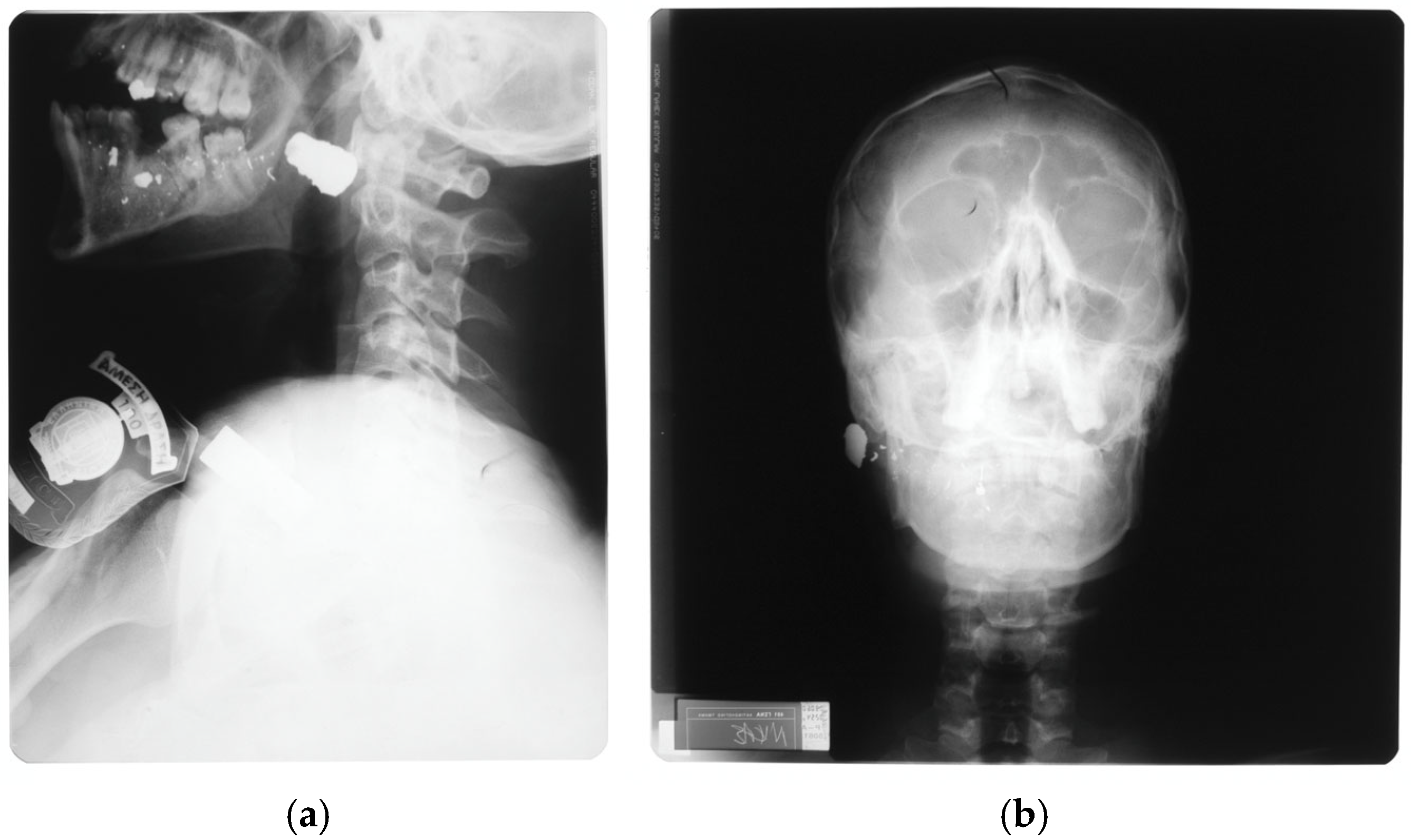
- Oehmichen, M.; Meissner, C.; König, H.G.; Gehl, H.B. Gunshot injuries to the head and brain caused by low-velocity handguns and rifles: A review. Forensic Sci. Int. 2004, 146, 111–120. [Google Scholar] [CrossRef]
- Janzon, B.; Hull, J.B.; Ryan, J.M. Projectile-material interactions: Soft tissue and bone. In Scientific Foundations of Trauma; Cooper, G.J., Dudley, H.A.F., Gann, D.S., Little, R.A., Maynard, R.L., Eds.; Butterworth Heinemann: Oxford, UK, 1997; pp. 37–52. ISBN 0 7506 1585 0. [Google Scholar]
- Myerson, M.S.; Sammarco, V.J. Penetrating and lacerating injuries of the foot. Foot Ankle Clin. 1999, 4, 647–672. [Google Scholar]
- Shin, E.H.; Sabino, J.M.; Nanos, G.P., III; Valerio, I.L. Ballistic trauma: Lessons learned from Iraq and Afghanistan. Semin. Plast. Surg. 2015, 29, 10–19. [Google Scholar] [CrossRef]
- Adams, M.H.; Gaviria, M.; Sabbag, C.M. Military ballistic injuries of the upper extremity. Hand Clin. 2025, 41, 269–280. [Google Scholar] [CrossRef] [PubMed]
- Dahlgren, B.; Berlin, R.; Janzon, B.; Nordström, G.; Nylöf, U.; Rybeck, B.; Schantz, B.; Seeman, T. The extent of muscle tissue damage following missile trauma one six and twelve hours after the infliction of trauma, studied by the current method of debridement. Acta Chir. Scand. Suppl. 1979, 489, 137–144. [Google Scholar] [PubMed]
- Wang, Z.G.; Feng, J.X.; Liu, Y.Q. Pathomorphological observations of gunshot wounds. Acta Chir. Scand. Suppl. 1982, 508, 185–195. [Google Scholar]
- Fackler, M.L.; Breteau, J.P.; Courbil, L.J.; Taxit, R.; Glas, J.; Fievet, J.P. Open wound drainage versus wound excision in treating the modern assault rifle wound. Surgery 1989, 105, 576–584. [Google Scholar] [PubMed]
- Popov, V.A.; Vorob’ev, V.V.; Pitenin, I.Y. Microcirculatory changes in tissues surrounding a gunshot wounds. Bull. Exp. Biol. Med. 1990, 109, 437–441. [Google Scholar] [CrossRef]
- Vuong, P.N.; Berry, C. The Pathology of Vessels; Springer: Berlin, Germany, 2002; Chapter 6: Vascular trauma; pp. 119–137. [Google Scholar] [CrossRef]
- Le Gros Clark, W.E.; Blomfield, L.B. The efficiency of intramuscular anastomoses, with observations on the regeneration of devascularized muscle. J. Anat. 1945, 79, 15–32. [Google Scholar]
- Watson, J.D.B.; Tai, N.R.M.; Martin, M.J. Military vascular injuries; considerations and techniques. In Vascular Injury: Endovascular and Open Surgical Management; DuBose, J.J., Teixeira, P.G., Rajani, R.R., Eds.; McGraw-Hill: New York, NY, USA, 2023; pp. 273–284. ISBN 978-1-26-426983-9. [Google Scholar]
- Ragsdale, B.D.; Josselson, A. Experimental gunshot fractures. J. Trauma 1988, 28, S109–S115. [Google Scholar] [CrossRef]
- Wang, Z.G.; Qian, C.W.; Zhan, D.C.; Shi, T.Z.; Tang, C.G. Pathological changes of gunshot wounds at various intervals after wounding. Acta Chir. Scand. Suppl. 1982, 508, 197–210. [Google Scholar]
- Fackler, M.L. Wounding patterns of military rifle bullets. Int. Defense Rev. 1989, 22, 159–165. [Google Scholar]
- Penn-Barwell, J.G.; Sargeant, I.D.; Bennett, P.; Fries, C.; Kendrew, J.; Midwinter, M.; Bishop, J.; Rickard, R.; Porter, K.; Rowlands, T.; et al. Gun-shot injuries in UK military casualties—Features associated with wound severity. Injury 2016, 47, 1067–1071. [Google Scholar] [CrossRef] [PubMed]
- Manta, A.M.; Petrasso, P.E.Y.; Tomassini, L.; Piras, G.N.; De Maio, A.; Cappelletti, S.; Straccamore, M.; Siodambro, C.; De Simone, S.; Peonim, V.; et al. The wounding potential of assault rifles: Analysis of the dimensions of entrance and exit wounds and comparison with conventional handguns. A multicentric study. Forensic Sci. Med. Pathol. 2024, 20, 896–909. [Google Scholar] [CrossRef]
- Sanders, M.J.; McKenna, K.D. Sander’s Paramedic Textbook, 6th ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2025; ISBN 9781284264791. [Google Scholar]
- Ng, E.; Choong, A.M.T.L. External iliac artery injury secondary to indirect pressure wave effect from gunshot wound. Chin. J. Traumatol. 2016, 19, 134–135. [Google Scholar] [CrossRef]
- Sanchez, L.D.; Ketterer, A.R. Gunshot attacks: Mass casualties. In Ciottone’s Disaster Medicine, 3rd ed.; Ciottone, G.R., Ed.; Elsevier: Philadelphia, PA, USA, 2024; pp. 904–906. [Google Scholar] [CrossRef]
- Rasmussen, T.E.; Stannard, A. Injury to extremities. In Fischer’s Mastery of Surgery, 6th ed.; Fischer, J.E., Ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2012; pp. 2495–2504. ISBN 978-1-60831-740-0. [Google Scholar]
- White, J.M.; Stannard, A.; Burkhardt, G.E.; Eastridge, B.J.; Blackbourne, L.H.; Rasmussen, T.E. The epidemiology of vascular injury in the wars in Iraq and Afghanistan. Ann. Surg. 2011, 25, 1184–1189. [Google Scholar] [CrossRef] [PubMed]
- Tarkunde, Y.R.; Clohisy, C.J.; Calfee, R.P.; Halverson, S.J.; Wall, L.B. Firearm injuries to the wrist and hand in children and adults: An epidemiologic study. Hand 2023, 18, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Rich, N.M.; Spencer, F.C. Vascular Trauma; Saunders: Philadelphia, PA, USA, 1978; Chapter 3: Experimental arterial trauma; pp. 44–60. ISBN 0-7216-7580-8. [Google Scholar]
- Straszewski, A.J.; Schultz, K.; Dickherber, J.L.; Dahm, J.S.; Wolf, J.M.; Strelzow, J.A. Gunshot-related upper extremity nerve injuries at a level 1 trauma center. J. Hand Surg. Am. 2022, 47, 88.e1–88.e6. [Google Scholar] [CrossRef]
- McQuillan, T.J., III; Zelenski, N.A. Ballistic injuries of the brachial plexus. Hand Clin. 2025, 41, 351–359. [Google Scholar] [CrossRef]
- Otten, E.J. Hunting and fishing injuries. In Auerbach’s Wilderness Medicine, 7th ed.; Auerbach, P.S., Cushing, T.A., Harris, N.S., Eds.; Elsevier: Philadelphia, PA, USA, 2017; Volume 1, pp. 549–563. ISBN 978-0-323-35942-9. [Google Scholar]
- Schmidt, A.; Wise, K.; Kelly, B. The physics of trauma. In PHTLS Prehospital Trauma Life Support, 10th ed.; Pollak, A.N., Ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2023; pp. 103–147. ISBN 9781284264746. [Google Scholar]
- Glezer, J.A.; Minard, G.; Croce, M.A.; Fabian, T.C.; Kudsk, K.A. Shotgun wounds to the abdomen. Am. Surg. 1993, 59, 129–132. [Google Scholar] [PubMed]
- Breitenecker, R. Shotgun wound patterns. Am. J. Clin. Pathol. 1969, 52, 258–269. [Google Scholar] [CrossRef]
- Gestring, M.L.; Geller, E.R.; Akkad, N.; Bongiovanni, P.J. Shotgun slug injuries: Case report and literature review. J. Trauma 1996, 40, 650–653. [Google Scholar] [CrossRef]
- Stefanopoulos, P.K.; Tsiatis, N.E.; Herbstein, J.A. Gunshot wounds. In Encyclopedia of Forensic Sciences, 3rd ed.; Houck, M.M., Ed.; Elsevier: Oxford, UK, 2023; Volume 3, pp. 75–98. [Google Scholar] [CrossRef]
- Smith, H.W.; Wheatley, K.K. Biomechanics of femur fractures secondary to gunshot wounds. J. Trauma 1984, 24, 970–977. [Google Scholar] [CrossRef]
- Rose, S.C.; Fujisaki, K.; Moore, E.E. Incomplete fractures associated with penetrating trauma: Etiology, appearance, and natural history. J. Trauma 1988, 28, 106–109. [Google Scholar] [CrossRef]
- Christensen, A.M.; Rickman, J.M. Cone cracking in human bone: A CT case review series. Forensic Imaging 2022, 30, 200510. [Google Scholar] [CrossRef]
- Caister, A.J.; Carr, D.J.; Campbell, P.D.; Brock, F.; Breeze, J. The ballistic performance of bone when impacted by fragments. Int. J. Leg. Med. 2020, 134, 1387–1393. [Google Scholar] [CrossRef]
- Pandey, P.K.; Joshi, Y.K.; Ganpule, S.G. Review of interaction of bullets and fragments with skin-bone-muscle parenchyma. J. Eng. Sci. Med. Diagn. Ther. 2025, 8, 040801. [Google Scholar] [CrossRef]
- Schwab, N.; Jordana, X.; Monreal, J.; Garrido, X.; Soler, J.; Vega, M.; Brillas, P.; Galtés, I. Ballistic long bone fracture pattern: An experimental study. Int. J. Leg. Med. 2024, 138, 1685–1700. [Google Scholar] [CrossRef] [PubMed]
- Rickman, J.M.; Painter, J.; Hazael, R. A scanning electron microscopy study of projectile entry fractures in cortical bone; genesis and microarchitectural features. Int. J. Leg. Med. 2022, 136, 629–648. [Google Scholar] [CrossRef] [PubMed]
- Kieser, D.C.; Carr, D.J.; Leclair, S.C.J.; Horsfall, I.; Theis, J.C.; Swain, M.V.; Kieser, J.A. Gunshot induced indirect femoral fracture: Mechanism of injury and fracture morphology. J. R. Army Med Corps 2013, 159, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Tian, H.M.; Huang, M.J.; Liu, Y.Q.; Wang, Z.G. Primary bacterial contamination of wound track. Acta Chir. Scand. Suppl. 1982, 508, 265–269. [Google Scholar]
- Hinz, B.J.; Muci-Küchler, K.H.; Smith, P.M. Distribution of bacterial in simplified surrogate extremities shot with small caliber projectiles. In Proceedings of the ASME 2013 International Mechanical Engineering Congress and Exposition (IMECE2013). Volume 3A: Biomedical and Biotechnology Engineering, San Diego, CA, USA, 15–21 November 2013; pp. 1–11. [Google Scholar] [CrossRef]
- Lazovic, R.; Radojevic, N.; Curovic, I. Performance of primary repair on colon injuries sustained from low- versus high-energy projectiles. J. Forensic Leg. Med. 2016, 39, 125–129. [Google Scholar] [CrossRef]
- Jones, R.C. Surgical infections in trauma. In Infectious Diseases, 2nd ed.; Gorbach, S.L., Bartlett, J.G., Blacklow, N.R., Eds.; Saunders: Philadelphia, PA, USA, 1998; pp. 927–932. ISBN 0-7216-6119-X. [Google Scholar]
- Pilbery, R.; Lethbridge, K. Ambulance Care Practice, 2nd ed.; Class Professional Publishing: Bridgwater, UK, 2019; Chapter 17: Trauma; pp. 311–371. ISBN 9-781859-598542. [Google Scholar]
- Mosesso, V.; Holtz, M.; Greenhill, M. Patient assessment and management. In PHTLS Prehospital Trauma Life Support, 10th ed.; UK edition; Pollak, A.N., Smith, C., Eds.; Jones & Bartlett Learning: Burlington, MA, USA, 2026; pp. 169–200. ISBN 978-1-284-29914-4. [Google Scholar]
- Smith, B.P.; Schwab, C.W. Initial assessment and resuscitation. In The Trauma Manual: Trauma and Acute Care Surgery, 5th ed.; Peitzman, A.B., Yealy, D.M., Fabian, T.C., Schwab, C.W., Eds.; Wolters Kluwer: Philadelphia, PA, USA, 2020; pp. 34–47. ISBN 978-1-975113-04-9. [Google Scholar]
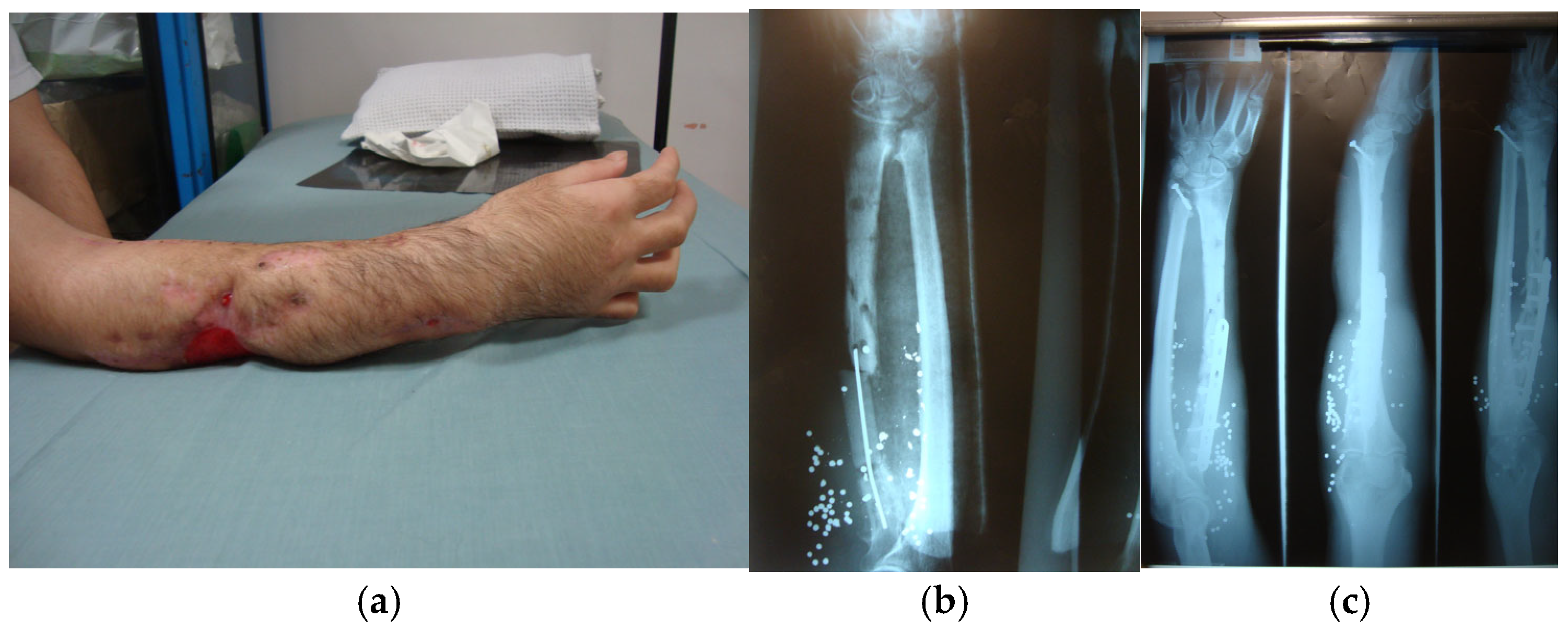
- Lin, J.S.; Rhee, P.C. Wrist and forearm fractures from ballistic injuries. Hand Clin. 2025, 41, 313–322. [Google Scholar] [CrossRef]
- Nasser, A.A.H.; Nederpelt, C.; El Hechi, M.; Mendoza, A.; Saillant, N.; Fagenholz, P.; Velmahos, G.; Kaafarani, H.M.A. Every minute counts: The impact of pre-hospital response time and scene time on mortality of penetrating trauma patients. Am. J. Surg. 2020, 220, 240–244. [Google Scholar] [CrossRef]
- Mosesso, V.; Holtz, M. Patient assessment and management. In PHTLS Prehospital Trauma Life Support, 10th ed.; Pollak, A.N., Ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2023; pp. 173–205. ISBN 978-1-284-27227-7. [Google Scholar]
- Lennquist, S. Medical Response to Major Incidents and Disasters: A Practical Guide for All Medical Staff; Springer: Heidelberg, Germany, 2012; ISBN 978-3-642-21894-1. [Google Scholar]
- Giannou, C.; Baldan, M. War Surgery: Working with Limited Resources in Armed Conflict and Other Situations of Violence, 2nd ed.; International Committee of the Red Cross: Geneva, Switzerland, 2019; Volume 1. [Google Scholar]
- Burlew, C.C.; Moore, E.E.; Moore, F.A.; Coimbra, R.; McIntyre, R.C., Jr.; Davis, J.W.; Sperry, J.; Biffl, W.L. Western Trauma Association critical decisions in trauma: Resuscitative thoracotomy. J. Trauma Acute Care Surg. 2012, 73, 1359–1363. [Google Scholar] [CrossRef]
- Liu, A.; Nguyen, J.; Ehrlich, H.; Bisbee, C.; Santiesteban, L.; Santos, R.; McKenney, M.; Elkbuli, A. Emergency resuscitative thoracotomy for civilian thoracic trauma in the field and emergency department settings: A systematic review and meta-analysis. J. Surg. Res. 2022, 273, 22–55. [Google Scholar] [CrossRef] [PubMed]
- Dave, S.B.; Shriki, J. The big five—Lifesaving procedures in the trauma bay. Emerg. Med. Clin. N. Am. 2023, 41, 161–182. [Google Scholar] [CrossRef] [PubMed]
- Neuhaus, V.; Navsaria, P.H.; Nicol, A.J. Management of trauma for the general surgeon. In Core Topics in General and Emergency Surgery, 7th ed.; Paterson, H.M., Deans, C., Eds.; Elsevier: Oxford, UK, 2024; pp. 205–223. ISBN 978-0-7020-8474-4. [Google Scholar]
- Wessels, L.E.; Krzyzaniak, M.J.; Martin, M.J. Penetrating abdominal trauma. In Surgical Decision Making in Acute Care Surgery; Davis, K.A., Coimbra, R., Eds.; Thieme: Stuttgart, Germany, 2020; pp. 62–76. ISBN 978-1-68420-058-0. [Google Scholar]
- Wisner, D.H. Initial assessment. In Cervicothoracic Trauma, 2nd ed.; Blaisdell, F.W., Trunkey, D.D., Eds.; Thieme: New York, NY, USA, 1994; pp. 1–13. ISBN 0-86577-492-7. [Google Scholar]
- Clare, D.; Baxley, S. An evidence-based approach to managing gunshot wounds in the emergency department. Emerg. Med. Pract. 2023, 25, 1–28. [Google Scholar]
- Turner, C.D.A.; Lockey, D.J.; Rehn, M. Pre-hospital management of mass casualty civilian shootings: A systematic literature review. Crit. Care 2016, 20, 362, Erratum in Crit. Care. 2017, 21, 94. [Google Scholar] [CrossRef] [PubMed]
- Kuckelman, J.; Derickson, M.; Long, W.B.; Martin, M.J. MASCAL management from Baghdad to Boston: Top ten lessons learned from modern military and civilian MASCAL events. Curr. Trauma Rep. 2018, 4, 138–148. [Google Scholar] [CrossRef]
- Brito, A.M.P.; Schreiber, M. x-ABC versus ABC: Shifting paradigms in early trauma resuscitation. Trauma Surg. Acute Care Open 2025, 10 (Suppl. S1), e001773. [Google Scholar] [CrossRef]
- Ferrada, P.; Dissanaike, S. Circulation first for the rapidly bleeding trauma patient—It is time to reconsider the ABCs of trauma care. JAMA Surg. 2023, 158, 884–885. [Google Scholar] [CrossRef]
- Hirsch, M.; Carli, P.; Nizard, R.; Riou, B.; Baroudjian, B.; Baubet, T.; Chhor, V.; Chollet-Xemard, C.; Dantchev, N.; Fleury, N.; et al. The medical response to multisite terrorist attacks in Paris. Lancet 2015, 386, 2535–2538. [Google Scholar] [CrossRef]
- Galvagno, S.; Shirki, J. Shock: Pathophysiology of life and death. In PHTLS Prehospital Trauma Life Support, 10th ed.; Pollak, A.N., Ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2023; pp. 49–102. ISBN 978-1-284-27227-7. [Google Scholar]
- Manifold, C.; Abraham, H.; Latham, S.; Weekes, T. Shock: Pathophysiology of life and death. In PHTLS Prehospital Trauma Life Support, 10th ed.; UK edition; Pollak, A.N., Smith, C., Eds.; Jones & Bartlett Learning: Burlington, MA, USA, 2026; pp. 49–97. ISBN 978-1-284-29914-4. [Google Scholar]
- Fedor, P.J.; Burns, B.; Lauria, M.; Richmond, C. Major trauma outside a trauma center: Prehospital, emergency department, and retrieval considerations. Emerg. Med. Clin. N. Am. 2018, 36, 203–218. [Google Scholar] [CrossRef]
- Ferrada, P.; Duschesne, J.; Piehl, M. Prioritizing circulation over airway in trauma patients with exsanguinating injuries: What you need to know. J. Trauma Acute Care Surg. 2025, 99, 679–683. [Google Scholar] [CrossRef]
- Gangidine, M.M.; Sorensen, D.M. Penetrating extremity trauma: Part I. Trauma. Reports 2019, 20, 1–11. [Google Scholar]
- Evans, C.; Chaplin, T.; Zelt, D. Management of major vascular injuries: Neck, extremities, and other things that bleed. Emerg. Med. Clin. N. Am. 2018, 36, 181–202. [Google Scholar] [CrossRef]
- Berry, C.; Gallagher, J.M.; Goodloe, J.M.; Dorlac, W.C.; Dodd, J.; Fischer, P.E. Prehospital hemorrhage control and treatment by clinicians: A joint position statement. Prehosp Emerg. Care 2023, 27, 544–551. [Google Scholar] [CrossRef] [PubMed]
- Callaway, D.W.; Phillips, J.P. Active-shooter response. In Ciottone’s Disaster Medicine, 3rd ed.; Ciottone, G.R., Ed.; Elsevier: Philadelphia, PA, USA, 2024; pp. 459–464. [Google Scholar] [CrossRef]
- Roberts, B.; James, D.; Haft, J.; Balakrishnan, N.; Prince, J.; Sathya, C. Wounding patterns in pediatric firearm fatalities. Injury 2023, 54, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Slama, R.; Villaume, F. Penetrating vascular injury: Diagnosis and management updates. Emerg. Med. Clin. N. Am. 2017, 35, 789–801. [Google Scholar] [CrossRef]
- Qasim, Z. Resuscitative endovascular balloon occlusion of the aorta: A practical review. Emerg. Med. Clin. N. Am. 2023, 41, 71–88. [Google Scholar] [CrossRef]
- Naeem, M.; Hoegger, M.J.; Petraglia, F.W.; Ballard, D.H.; Zulfigar, M.; Patlas, M.N.; Raptis, C.; Mellnick, V.M. CT of penetrating abdominopelvic trauma. Radiographics 2021, 41, 1064–1081. [Google Scholar] [CrossRef]
- Hynes, A.M. Finding the missing bullet: A case report of an unusual trajectory from the left scapula into the left orbit. Trauma Case Rep. 2021, 35, 100530, Erratum in Trauma Case Rep. 2023, 45, 100820. [Google Scholar] [CrossRef]
- Martin, M.J.; Davis, J.W. To operate or image? (Pulling the trigger). In Front Line Surgery: A Practical Approach, 2nd ed.; Martin, M.J., Beekley, A.C., Eckert, M.J., Eds.; Springer: Cham, Switzerland, 2017; pp. 77–87. ISBN 978-3-319-56780-8. [Google Scholar]
- Failla, A.V.M.; Licciardello, G.; Cocimano, G.; Di Mauro, L.; Chisari, M.; Sessa, F.; Salerno, M.; Esposito, M. Diagnostic challenges in uncommon firearm injury cases: A multidisciplinary approach. Diagnostics 2025, 15, 31. [Google Scholar] [CrossRef]
- Ledgerwood, A.M. The wandering bullet. Surg. Clin. N. Am. 1977, 57, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Rammo, R.A.; DeFazio, M.V.; Bullock, M.R. Management of migrating intracranial bullets: Lessons learnt from surviving an AK-47 bullet through the lateral brainstem. World Neurosurg. 2012, 77, 591.e19–591.e24. [Google Scholar] [CrossRef]
- Cooper, P.R. Gunshot wounds to the brain. In Head Injury, 3rd ed.; Cooper, P.R., Ed.; Williams & Wilkins: Baltimore, MD, USA, 1993; pp. 355–371. ISBN 0-683-02108-7. [Google Scholar]
- Aarabi, B.; Eisenberg, H. Surgical management and prognosis of penetrating brain injury. In Youmans & Winn Neurological Surgery, 8th ed.; Winn, H.R., Ed.; Elsevier: Philadelphia, PA, USA, 2023; pp. 3092–3104. ISBN 978-0-323-66192-8. [Google Scholar]
- Part2: Prognosis in penetrating brain injury (no authors listed). J. Trauma 2001, 51 (Suppl. S2), S44–S86.
- Rosenfeld, J.V.; Bell, R.S.; Armonda, R. Current concepts in penetrating and blast injury to the central nervous system. World J. Surg. 2015, 39, 1352–1362. [Google Scholar] [CrossRef]
- Zakrison, T.L.; Essig, R.; Polcari, A.; McKinley, W.; Arnold, D.; Beyene, R.; Wilson, K.; Rogers, S., Jr.; Matthews, J.B.; Millis, J.M.; et al. Review paper on penetrating brain injury: Ethical quandaries in the trauma bay and beyond. Ann. Surg. 2023, 277, 66–72. [Google Scholar] [CrossRef]
- Asensio, J.A.; Valenziano, C.P.; Falcone, R.E.; Grosh, J.D. Management of penetrating neck injuries: The controversy surrounding zone II injuries. Surg. Clin. N. Am. 1991, 71, 267–296. [Google Scholar] [CrossRef]
- Majors, J.S.; Brennan, J.; Holt, G.R. Management of high-velocity injuries of the head and neck. Facial Plast. Surg. Clin. North. Am. 2017, 25, 493–502. [Google Scholar] [CrossRef]
- Scott, B.G. Approach to penetrating injuries of the neck. In Head, Face, and Neck Trauma: Comprehensive Management; Stewart, M.G., Ed.; Thieme: New York, NY, USA, 2005; pp. 202–206. ISBN 1-58890-308-7. [Google Scholar]
- Bean, A.S. Trauma to the neck. In Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9th ed.; Tintinalli, J.E., Ed.; McGraw-Hill: New York, NY, USA, 2020; pp. 1722–1729. ISBN 978-1-260-01993-3. [Google Scholar]
- Loss, L.; Henry, R.; White, A.; Matsushima, K.; Barrett, C.; Lammers, D.; Schreiber, M.; Inaba, K. Penetrating neck trauma: A comprehensive review. Trauma Surg. Acute Care Open 2025, 24, e001619. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, J.M.; Chan, T.G.; Moore, C.E. Penetrating head and neck trauma: A narrative review of evidence-based evaluation and treatment protocols. Otolaryngol. Clin. N. Am. 2023, 53, 1013–1025. [Google Scholar] [CrossRef]
- Zhao, F.Z.; Biffl, W.L. Thoracic trauma. In Textbook of Critical Care, 8th ed.; Vincent, J.-L., Moore, F.A., Bellomo, R., Marini, J.J., Eds.; Elsevier: Oxford, UK, 2024; pp. 1255–1263. ISBN 978-0-323-75929-8. [Google Scholar]
- Raja, A.S. Peripheral vascular trauma. In Rosen’s Emergency Medicine: Concepts and Clinical Practice, 10th ed.; Walls, R.M., Ed.; Elsevier: Philadelphia, PA, USA, 2023; Volume 1, pp. 429–437. ISBN 978-0-323-75847-5. [Google Scholar]
- Kirkpatrick, J.B.; Di Maio, V. Civilian gunshot wounds of the brain. J. Neurosurg. 1978, 49, 185–198. [Google Scholar] [CrossRef] [PubMed]
- Dawoud, F.M.; Feldman, M.J.; Yengo-Kahn, A.M.; Roth, S.G.; Wolfson, D.I.; Ahluwalia, R.; Kelly, P.D.; Chitale, R.V. Traumatic cerebrovascular injuries associated with gunshot wounds to the head: A single-institution ten-year experience. World Neurosurg. 2021, 146, e1031–e1044. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, F.; Gonzalez, P.; Dang, C.; Fleming, A.; Sterling-Scott, R. The Glasgow Coma Scale and prognosis in gunshot wounds to the brain. J. Trauma 1993, 35, 75–77. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, M.S. Greenberg’s Handbook of Neurosurgery, 10th ed.; Thieme: New York, NY, USA, 2023; Chapter 65: Gunshot wounds and non-missile penetrating brain injuries; pp. 1093–1097. ISBN 978-1-68420-504-2. [Google Scholar]
- Benjamin, E.R.; Demetriades, D.; Owattanapanich, N.; Shackelford, S.A.; Roedel, E.; Polk, T.M.; Biswas, S.; Rasmussen, T. Therapeutic interventions and outcomes in civilian and military isolated gunshot wounds to the head: A Department of Defense Trauma Registry and ACS TQIP-matched study. Ann. Surg. 2023, 278, e131–e136. [Google Scholar] [CrossRef] [PubMed]
- Piaseczny, M.; La, J.; Chaplin, T.; Evans, C. Protect that neck! Management of blunt and penetrating neck trauma. Emerg. Med. Clin. N. Am. 2023, 41, 35–49. [Google Scholar] [CrossRef]
- Tisherman, S.A.; Bokhari, F.; Collier, B.; Cumming, J.; Ebert, J.; Holevar, M.; Kurek, S.; Leon, S.; Rhee, P. Clinical practice guideline: Penetrating zone II neck trauma. J. Trauma 2008, 64, 1392–1405. [Google Scholar] [CrossRef]
- Nganzeu, C.; Esce, A.; Abu-Ghanem, S.; Meiklejohn, D.A.; Sims, H.S. Laryngeal trauma. Otolaryngol. Clin. N. Am. 2023, 56, 1039–1053. [Google Scholar] [CrossRef]
- Schellenberg, M.; Inaba, K. Critical decisions in the management of thoracic trauma. Emerg. Med. Clin. N. Am. 2018, 36, 135–147. [Google Scholar] [CrossRef]
- Boffard, K.D.; White, J.O. Manual of Definitive Surgical Trauma Care: Incorporating Definitive Anaesthetic Trauma Care, 6th ed.; CRC Press: Boca Raton, FL, USA, 2024; ISBN 9781032157818. [Google Scholar]
- Smith, E.R.; Sarani, B.; Shapiro, G.; Gondek, S.; Rivas, L.; Ju, T.; Robinson, B.R.; Estroff, J.M.; Fudenberg, J.; Amdur, R.; et al. Incidence and cause of potentially preventable death after civilian public mass shooting in the US. J. Am. Coll. Surg. 2019, 229, 244–251. [Google Scholar] [CrossRef]
- Brenner, M.; Hicks, C. Major abdominal trauma: Critical decisions and new frontiers in management. Emerg. Med. Clin. N. Am. 2018, 36, 149–160. [Google Scholar] [CrossRef]
- Aylwin, C.; Jenkins, M. Abdominal aortic trauma, iliac and visceral vessel injuries. In Rich’s Vascular Trauma, 4th ed.; Rasmussen, T.E., Tai, N.R.M., Eds.; Elsevier: Philadelphia, PA, USA, 2022; pp. 212–225. [Google Scholar] [CrossRef]
- Pryor, J.P.; Reilly, P.M.; Dabrowski, G.P.; Grossman, M.D.; Schwab, C.W. Nonoperative management of abdominal gunshot wounds. Ann. Emerg. Med. 2004, 43, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Wilkes, G. Abdominal trauma. In Textbook of Adult Emergency Medicine, 5th ed.; Cameron, P., Little, M., Mitra, B., Deasy, C., Eds.; Elsevier: Oxford, UK, 2020; pp. 92–95. ISBN 978-0-7020-7624-4. [Google Scholar]
- Velmahos, G.C.; Demetriades, D.; Toutouzas, K.G.; Sarkisyan, G.; Chan, L.S.; Ishak, R.; Alo, K.; Vassiliu, P.; Murray, J.A.; Salim, A.; et al. Selective nonoperative management in 1856 patients with abdominal gunshot wounds: Should routine laparotomy still be the standard of care? Ann. Surg. 2001, 234, 395–403. [Google Scholar] [CrossRef]
- Sander, A.; Spence, R.; Ellsmere, J.; Hoogerboord, M.; Edu, S.; Nicol, A.; Navsaria, P. Penetrating abdominal trauma in the era of selective conservatism: A prospective cohort study in a level 1 trauma center. Eur. J. Trauma Emerg. Surg. 2022, 48, 881–889. [Google Scholar] [CrossRef]
- Hughes, R.K. Thoracic trauma. Ann. Thorac. Surg. 1965, 1, 778–804. [Google Scholar] [CrossRef]
- Martin, M.J.; Brown, C.V.R.; Shatz, D.V.; Alam, H.; Brasel, K.; Hauser, C.J.; de Moya, M.; Moore, E.E.; Vercruysse, G.; Inaba, K. Evaluation and management of abdominal gunshot wounds: A Western Trauma Association critical decisions algorithm. J. Trauma Acute Care Surg. 2019, 87, 1220–1227. [Google Scholar] [CrossRef]
- Khomenko, I.; Tsema, I.; Humeniuk, K.; Makarov, H.; Rahushyn, D.; Yarynych, Y.; Sotnikov, A.; Slobodianyk, V.; Shypilov, S.; Dubenko, D.; et al. Application of damage control tactics and transpapillary biliary decompression for organ-preserving surgical management of liver injury in combat patient. Mil. Med. 2022, 187, e781–e786. [Google Scholar] [CrossRef]
- Persad, I.J.; Reddy, R.S.; Saunders, M.A.; Patel, J. Gunshot injuries to the extremities: Experience of a U.K. trauma centre. Injury 2005, 36, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Laubscher, M.; Ferreira, N.; Birkholtz, F.F.; Graham, S.M.; Maqungo, S.; Held, M. Civilian gunshot injuries in orthopedics: A narrative review of ballistics, current concepts, and the South African experience. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Papasoulis, E.; Patzakis, M.J.; Zalavras, C.G. Antibiotics in the treatment of low-velocity gunshot -induced fractures: A systematic literature review. Clin. Orthop. Relat. Res. 2013, 471, 3937–3944. [Google Scholar] [CrossRef] [PubMed]
- Sathiyakumar, V.; Thakore, R.V.; Stinner, D.J.; Obremskey, W.T.; Ficke, J.R.; Sethi, M.K. Gunshot-induced fractures of the extremities: A review of antibiotic and debridement practices. Curr. Rev. Musculoskelet. Med. 2015, 8, 276–289. [Google Scholar] [CrossRef]
- Omid, R.; Stone, M.A.; Zalavras, C.G.; Marecek, G.S. Gunshot wounds to the upper extremity. J. Am. Acad. Orthop. Surg. 2019, 27, e301–e310. [Google Scholar] [CrossRef]
- Maqungo, S.; Kauta, N.; Held, M.; Mazibuko, T.; Keel, M.J.B.; Laubscher, M.; Ahmad, S.S. Gunshot injuries to the lower extremities: Issues, controversies and algorithm of management. Injury 2020, 51, 1426–1431. [Google Scholar] [CrossRef]
- Kauvar, D.S.; Sarfati, M.R.; Kraiss, L.W. National trauma databank analysis of mortality and limb loss in isolated lower extremity vascular trauma. J. Vasc. Surg. 2011, 53, 1598–1603. [Google Scholar] [CrossRef]
- Hynes, A.M. Traumatic proximal brachial artery injury selectively managed non-operatively: A case report and review of the literature. Trauma Case Rep. 2022, 38, 100612. [Google Scholar] [CrossRef] [PubMed]
- de Sauza, I.S.; Benabbas, R.; McKee, S.; Zangbar, B.; Jain, A.; Paladino, L.; Boudourakis, L.; Sinert, R. Accuracy of physical examination, ankle-brachial index, and ultrasonography in the diagnosis of arterial injury in patients with penetrating extremity trauma: A systematic review and meta-analysis. Acad. Emerg. Med. 2017, 24, 994–1017. [Google Scholar] [CrossRef]
- Kobayashi, L.; Coimbra, R.; Goes, A.M.O., Jr.; Reva, V.; Santorelli, J.; Moore, E.; Galante, J.; Abu-Zidan, F.; Peitzman, A.B.; Ordonez, C.; et al. American Association for the Surgery of Trauma—World Society of Emergency Surgery guidelines on diagnosis and management of peripheral vascular injuries. J. Trauma Acute Care Surg. 2020, 89, 1183–1196. [Google Scholar] [CrossRef]
- Carpenter, C.R.; Raja, A.S. Penetrating trauma to the extremities and vascular injuries. In Evidence-Based Emergency Care: Diagnostic Testing and Clinical Decision Rules, 3rd ed.; Pines, J.M., Bellolio, F., Carpenter, C.R., Raja, A.S., Eds.; Wiley Blackwell: Chichester, UK, 2023; pp. 214–224. [Google Scholar] [CrossRef]
- Wahlgren, C.M.; Riddez, L. Penetrating arterial injuries below elbow/knee. In Penetrating Trauma: A Practical Guide on Operative Technique and Peri-Operative Management, 3rd ed.; Degiannis, E., Doll, D., Velmahos, G.C., Eds.; Springer: Cham, Switzerland, 2023; pp. 635–640. [Google Scholar] [CrossRef]
- Colip, C.G.; Gorantla, V.; LeBedis, C.A.; Soto, J.A.; Anderson, S.W. Extremity CTA for penetrating trauma: 10-year experience using a 64-detector row CT scanner. Emerg. Radiol. 2017, 24, 223–232. [Google Scholar] [CrossRef]
- Feliciano, D.V. Pittalls in the management of peripheral vascular injuries. Trauma Surg. Acute Care Open 2017, 2, e000110. [Google Scholar] [CrossRef]
- Warwick, H.; Cherches, M.; Shaw, C.; Toogood, P. Comparison of computed tomography angiography and physical exam in the evaluation of arterial injury in extremity trauma. Injury 2021, 52, 1727–1731. [Google Scholar] [CrossRef]
- Romagnoli, A.N.; DuBose, J.; Dua, A.; Betzold, R.; Bee, T.; Fabian, T.; Morrison, J.; Skarupa, D.; Podbielski, J.; Inaba, K.; et al. Hard signs gone soft: A croitical evaluation of presenting signs of extremity vascular injury. J. Trauma Acute Care Surg. 2021, 90, 1–10. [Google Scholar] [CrossRef]
- Kauvar, D.S.; Propper, B.W. Lower extremity vascular trauma. In Rich’s Vascular Trauma, 4th ed.; Rasmussen, T.E., Tai, N.R.M., Eds.; Elsevier: Philadelphia, PA, USA, 2022; pp. 273–287. [Google Scholar] [CrossRef]
- Guthrie, H.C.; Clasper, J.C.; Kay, A.R.; Parker, P.J. Initial extremity war wound debridement: A multidisciplinary consensus. BMJ Mil. Health 2011, 157, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, T.M.; Russo, C.J. Management of specific soft tissue injuries. In Reichman’s Emergency Medicine Procedures, 3rd ed.; Reichman, E.F., Ed.; McGraw-Hill: New York, NY, USA, 2019; pp. 1034–1049. ISBN 978-1-259-86192-5. [Google Scholar]
- Muetterties, C.; Miller, A.J.; Strohl, A. Soft tissue reconstruction of the upper extremity after ballistic injury. Hand Clin. 2025, 41, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Kay, A. Wound management in a field hospital environment. In Field Hospitals: A Comprehensive Guide to Preparation and Operation; Bar-On, E., Peleg, K., Kreiss, Y., Eds.; Cambridge University Press: Cambridge, UK, 2020; pp. 160–179. [Google Scholar] [CrossRef]
- Bowyer, M.W.; Rhee, P.; DuBose, J.J. Soft tissue wounds and fasciotomies. In Front Line Surgery: A Practical Approach, 2nd ed.; Martin, M.J., Beekley, A.C., Eckert, M.J., Eds.; Springer: Cham, Switzerland, 2017; pp. 329–352. ISBN 978-3-319-56780-8. [Google Scholar]
- Stefanopoulos, P.K.; Aloizos, S.; Mikros, G.; Nikita, A.S.; Tsiatis, N.E.; Bissias, C.; Breglia, G.A.; Janzon, B. Assault rifle injuries in civilians: Ballistics of wound patterns, assessment and initial management. Eur. J. Trauma Emerg. Surg. 2024, 50, 2741–2751. [Google Scholar] [CrossRef]
- Sassoon, A.; Riehl, J.; Rich, A.; Langford, J.; Haidukewych, G.; Pearl, G.; Koval, K.J. Muscle viability revisited: Are we removing normal muscle? A critical evaluation of dogmatic debridement. J. Orthop. Trauma 2016, 30, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Schmalbruch, H. Skeletal Muscle; Springer: Berlin, Germany, 1985; p. 282. [Google Scholar] [CrossRef]
- Hadlock, T.A.; Cheney, M.L. Soft tissue injuries of the face. In Facial Surgery: Plastic and Reconstructive; Cheney, M.L., Hadlock, T.A., Eds.; CRC Press: Boca Raton, FL, USA, 2015; Volume 2, pp. 671–682. ISBN 978-1-62623-665-3. [Google Scholar]
- Grillo, R.; Quinta Reis, B.A.; Brozoski, M.A.; Zindel Deboni, M.C.; Melhem-Elias, F. A historical perspective on ballistic evolution and its implications for maxillofacial surgery. J. Craniomaxilllofac Surg. 2025, 53, 1052–1060. [Google Scholar] [CrossRef] [PubMed]
- Dienstknecht, T.; Horst, K.; Sellei, R.M.; Berner, A.; Nerlich, M.; Hardcastle, T.C. Indications for bullet removal: Overview of the literature, and clinical practice guidelines for European trauma surgeons. Eur. J. Trauma Emerg. Surg. 2012, 38, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Giannou, C.; Baldan, M.; Molde, Å. War Surgery: Working with Limited Resources in Armed Conflict and Other Situations of Violence, 2nd ed.; International Committee of the Red Cross: Geneva, Switzerland, 2021; Volume 2. [Google Scholar]
- ICRC Antibiotic Protocol for Weapon Wounded. 2022. Available online: https://www.icrc.org/en/publication/4593-icrc-antibiotic-protocol-weapon-wounded (accessed on 8 October 2025).



| Bullet Type | Profile of Injury * | Energy Transfer | Description |
|---|---|---|---|
| FMJ |  | Low energy—small exit wound | The bullet fails to yaw due to short wound channel |
| FMJ | 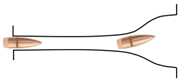 | High energy—large exit wound | The bullet tumbles close to the point of exit with cavitation |
| FMJ |  | High energy—relatively small exit wound | A long wound channel allows bullet tumbling deep within the tissues with the bullet moving base-forward near the exit |
| JSP |  | High energy +/− exit wound(s) | Expanding bullet demonstrating fragmentation with early large temporary cavity (the fragments may create multiple exit wounds) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stefanopoulos, P.K.; Breglia, G.A.; Bissias, C.; Nikita, A.S.; Papageorgiou, C.; Tsiatis, N.E.; Serafetinides, E.; Gyftokostas, D.A.; Aloizos, S.; Mikros, G. Firearm Injuries: A Review of Wound Ballistics and Related Emergency Management Considerations. Emerg. Care Med. 2025, 2, 52. https://doi.org/10.3390/ecm2040052
Stefanopoulos PK, Breglia GA, Bissias C, Nikita AS, Papageorgiou C, Tsiatis NE, Serafetinides E, Gyftokostas DA, Aloizos S, Mikros G. Firearm Injuries: A Review of Wound Ballistics and Related Emergency Management Considerations. Emergency Care and Medicine. 2025; 2(4):52. https://doi.org/10.3390/ecm2040052
Chicago/Turabian StyleStefanopoulos, Panagiotis K., Gustavo A. Breglia, Christos Bissias, Alexandra S. Nikita, Chrysovalantis Papageorgiou, Nikolaos E. Tsiatis, Efrem Serafetinides, Dimitrios A. Gyftokostas, Stavros Aloizos, and Georgios Mikros. 2025. "Firearm Injuries: A Review of Wound Ballistics and Related Emergency Management Considerations" Emergency Care and Medicine 2, no. 4: 52. https://doi.org/10.3390/ecm2040052
APA StyleStefanopoulos, P. K., Breglia, G. A., Bissias, C., Nikita, A. S., Papageorgiou, C., Tsiatis, N. E., Serafetinides, E., Gyftokostas, D. A., Aloizos, S., & Mikros, G. (2025). Firearm Injuries: A Review of Wound Ballistics and Related Emergency Management Considerations. Emergency Care and Medicine, 2(4), 52. https://doi.org/10.3390/ecm2040052






