Paediatric Emergency Injury Presentations During the COVID-19 Pandemic in Regional Victoria, Australia: A Silver Lining?
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Demographics
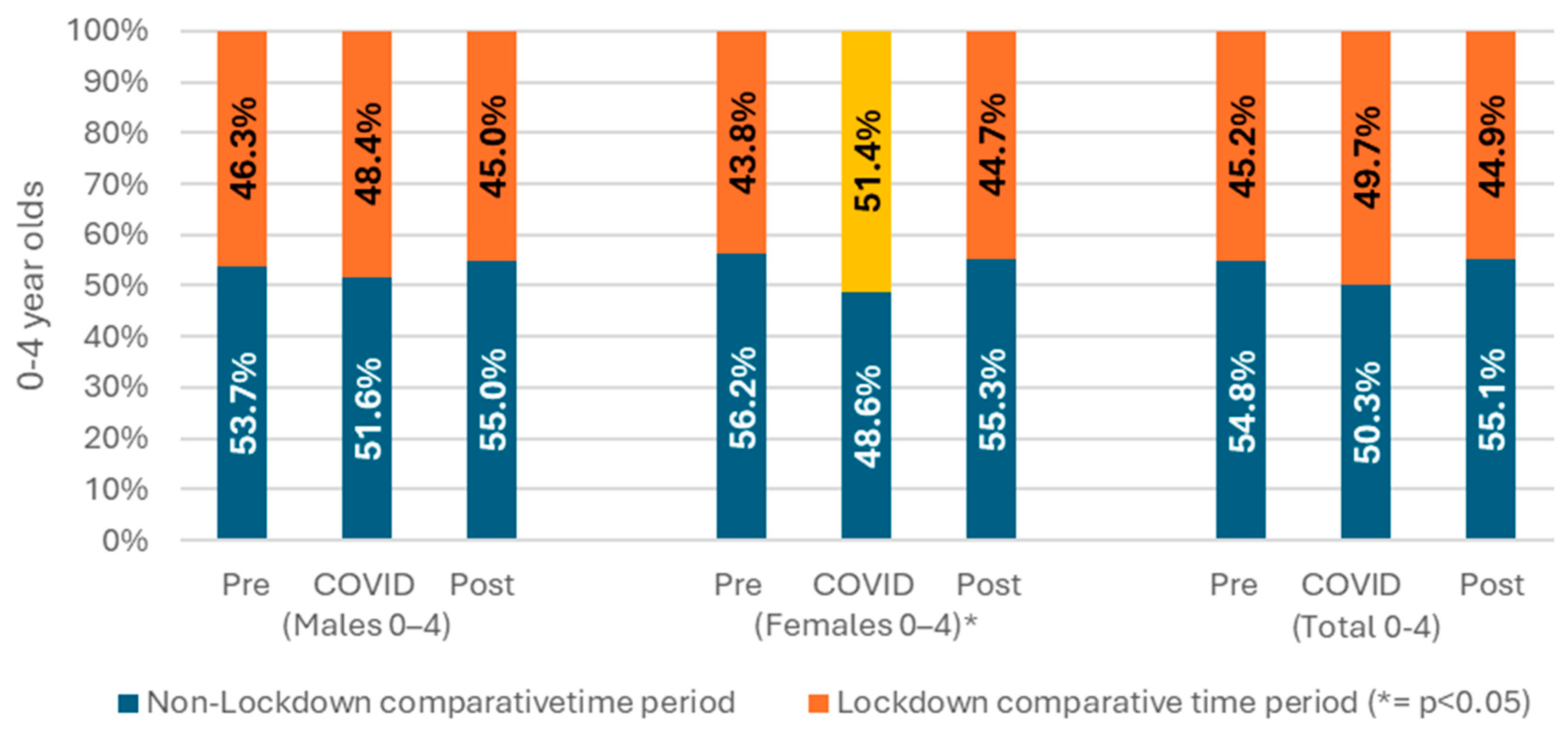
3.2. Lockdown Comparison
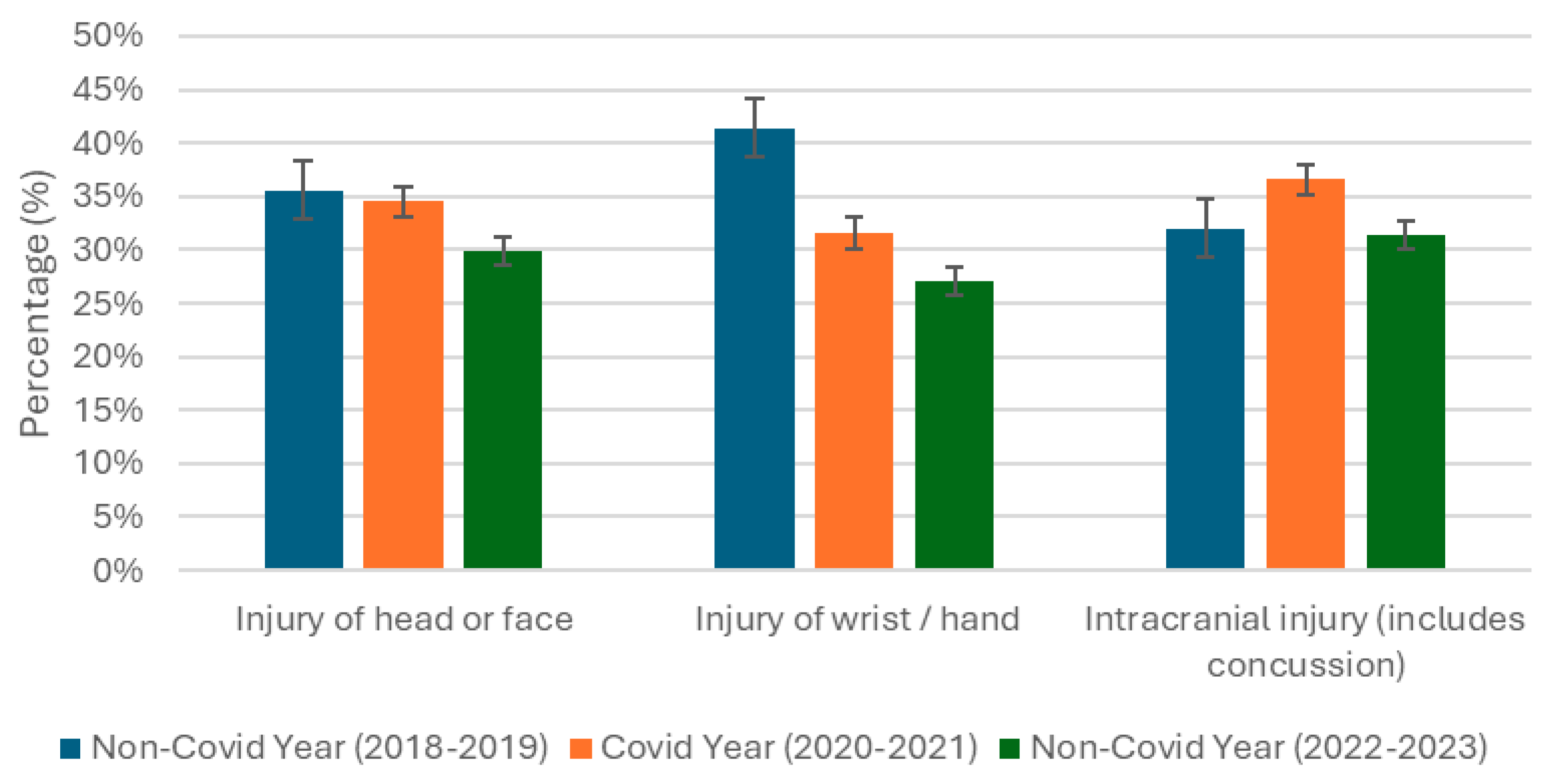
3.3. Comparative Time Period by Most Common Injury Type
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McPhail, R.; Wen, C.X.; Robyn, M.; Wilkinson, A. Post-COVID remote working and its impact on people, productivity, and the planet: An exploratory scoping review. Int. J. Hum. Resour. Manag. 2024, 35, 154–182. [Google Scholar] [CrossRef]
- Barlow, P.; van Schalkwyk, M.C.; McKee, M.; Labonté, R.; Stuckler, D. COVID-19 and the collapse of global trade: Building an effective public health response. Lancet Planet. Health 2021, 5, e102–e107. [Google Scholar] [CrossRef] [PubMed]
- Verity, R.; Okell, L.C.; Dorigatti, I.; Winskill, P.; Whittaker, C.; Imai, N.; Cuomo-Dannenburg, G.; Thompson, H.; Walker, P.G.T.; Fu, H.; et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect. Dis. 2020, 20, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Trauer, J.M.; Lydeamore, M.J.; Dalton, G.W.; Pilcher, D.; Meehan, M.T.; McBryde, E.S.; Cheng, A.C.; Sutton, B.; Ragonnet, R. Understanding how Victoria, Australia gained control of its second COVID-19 wave. Nat. Commun. 2021, 12, 6266. [Google Scholar] [CrossRef] [PubMed]
- Palmer, C.S.; Teague, W.J. Childhood injury and injury prevention during COVID-19 lockdown–stay home, stay safe? Injury 2021, 52, 1105–1107. [Google Scholar] [CrossRef]
- Griffiths, D.; Sheehan, L.; Petrie, D.; van Vreden, C.; Whiteford, P.; Collie, A. The health impacts of a 4-month long community-wide COVID-19 lockdown: Findings from a prospective longitudinal study in the state of Victoria, Australia. PLoS ONE 2022, 17, e0266650. [Google Scholar] [CrossRef]
- Haug, N.; Geyrhofer, L.; Londei, A.; Dervic, E.; Desvars-Larrive, A.; Loreto, V.; Pinior, B.; Thurner, S.; Klimek, P. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat. Hum. Behav. 2020, 4, 1303–1312. [Google Scholar] [CrossRef]
- Goldfeld, S.; O’Connor, E.; Sung, V.; Roberts, G.; Wake, M.; West, S.; Hiscock, H. Potential indirect impacts of the COVID-19 pandemic on children: A narrative review using a community child health lens. Med. J. Aust. 2022, 216, 364–372. [Google Scholar] [CrossRef]
- AIHW. Australia’s Children; AIHW: Canberra, ACT, Australia, 2020. [Google Scholar]
- Mitchell, R.J.; Curtis, K.; Foster, K. A 10-year review of child injury hospitalisations, health outcomes and treatment costs in Australia. Inj. Prev. 2018, 24, 344–350. [Google Scholar] [CrossRef]
- Van Gelder, N.; Peterman, A.; Potts, A.; O’Donnell, M.; Thompson, K.; Shah, N.; Oertelt-Prigione, S. COVID-19: Reducing the risk of infection might increase the risk of intimate partner violence. EClinicalMedicine 2020, 21, 100348. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.M.; Rodean, J.; Cook, L.; Sills, M.R.; Neuman, M.I.; Kornblith, A.E.; Jain, S.; Hirsch, A.W.; Goyal, M.K.; Fleegler, E.W.; et al. Injury-related pediatric emergency department visits in the first year of COVID-19. Pediatrics 2022, 150, e2021054545. [Google Scholar] [CrossRef] [PubMed]
- Sanford, E.L.; Zagory, J.; Blackwell, J.-M.; Szmuk, P.; Ryan, M.; Ambardekar, A. Changes in pediatric trauma during COVID-19 stay-at-home epoch at a tertiary pediatric hospital. J. Pediatr. Surg. 2021, 56, 918–922. [Google Scholar] [CrossRef]
- Sherman, W.F.; Khadra, H.S.; Kale, N.N.; Wu, V.J.; Gladden, P.B.; Lee, O.C. How did the number and type of injuries in patients presenting to a regional level I trauma center change during the COVID-19 pandemic with a stay-at-home order? Clin. Orthop. Relat. Res. 2021, 479, 266–275. [Google Scholar] [CrossRef]
- Chaiyachati, B.H.; Agawu, A.; Zorc, J.J.; Balamuth, F. Trends in Pediatric Emergency Department Utilization after Institution of Coronavirus Disease-19 Mandatory Social Distancing. J. Pediatr. 2020, 226, 274–277.e1. [Google Scholar] [CrossRef] [PubMed]
- Collings, A.T.; Farazi, M.; Van Arendonk, K.J.; Fallat, M.E.; Minneci, P.C.; Sato, T.T.; Speck, K.E.; Gadepalli, S.; Deans, K.J.; Falcone, R.A., Jr.; et al. Evaluating the Regional Differences in Pediatric Injury Patterns During the COVID-19 Pandemic. J. Surg. Res. 2023, 289, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Papachristou, E.; Deftereos, S.; Oikonomou, P.; Bekiaridou, K.; Foutzitzi, S.; Gogoulis, I.; Sinopidis, X.; Romanidis, K.; Tsaroucha, A.; Kambouri, K. Is it safe to stay at home? Parents’ perceptions of child home injuries during the COVID-19 lockdown. Healthcare 2022, 10, 2056. [Google Scholar] [CrossRef]
- Peck, B.; Terry, D.; Kloot, K. The socioeconomic characteristics of childhood injuries in regional victoria, australia: What the missing data tells us. Int. J. Environ. Res. Public Health 2021, 18, 7005. [Google Scholar] [CrossRef]
- Peck, B.; Terry, D.; Kloot, K. Predictive Characteristics of Childhood Emergency Injury Presentations in a Non-Urban Area of Victoria, Australia. Emerg. Care Med. 2024, 1, 165–175. [Google Scholar] [CrossRef]
- Peck, B.; Terry, D.R.; Kloot, K. Understanding childhood injuries in rural areas: Using Rural Acute Hospital Data Register to address previous data deficiencies. Emerg. Med. Australas. 2020, 32, 646–649. [Google Scholar] [CrossRef]
- Terry, D.R.; Peck, B.; Kloot, K. The data deficit for asthma emergency presentations might surprise you: How RAHDaR addresses the data chasm. Rural Remote Health 2020, 20, 5776. [Google Scholar] [CrossRef]
- Kloot, K.; Baker, T. Building a research-ready database of rural emergency presentations: The RAHDaR pilot study. Emerg. Med. Australas. 2019, 31, 126–128. [Google Scholar]
- ABS. Population: Census Canberra Australian Bureau of Statistics; ABS: Canberra, ACT, Australia, 2021. [Google Scholar]
- VicHealth. Victorian Emergency Minimum Dataset (VEMD), 25th ed.; v3.0.0 2020-21; Victorian Government: Melbourne, VIC, Australia, 2021. Available online: https://www.health.vic.gov.au/data-reporting/victorian-emergency-minimum-dataset-vemd (accessed on 1 July 2021).
- Independent Hospital Pricing Authority [IHPA]. The International Classification of Diseases, 10th revision, 11th ed.; Australian modification (ICD-10-AM); Independent Hospital Pricing Authority IHPA: Darlinghurst, NSW, Australia, 2019. [Google Scholar]
- Macreadie, I. Reflections from Melbourne, the world’s most locked-down city, through the COVID-19 pandemic and beyond. Microbiol. Aust. 2022, 43, 3–4. [Google Scholar]
- Pallant, J. SPSS Survival Manual: A Step by Step Guide to Data Analysis Using IBM SPSS; Routledge: Melbourne, VIC, Australia, 2020. [Google Scholar]
- Isba, R.; Edge, R.; Jenner, R.; Broughton, E.; Francis, N.; Butler, J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch. Dis. Child. 2020, 105, 704. [Google Scholar] [CrossRef] [PubMed]
- Dopfer, C.; Wetzke, M.; Zychlinsky Scharff, A.; Mueller, F.; Dressler, F.; Baumann, U.; Sasse, M.; Hansen, G.; Jablonka, A.; Happle, C. COVID-19 related reduction in pediatric emergency healthcare utilization–a concerning trend. BMC Pediatr. 2020, 20, 427. [Google Scholar]
- Hu, N.; Nassar, N.; Shrapnel, J.; Perkes, I.; Hodgins, M.; O’Leary, F.; Trudgett, C.; Eapen, V.; Woolfenden, S.; Knight, K.; et al. The impact of the COVID-19 pandemic on paediatric health service use within one year after the first pandemic outbreak in New South Wales Australia–a time series analysis. Lancet Reg. Health–West. Pac. 2022, 19, 100311. [Google Scholar] [PubMed]
- Tan, C.D.; Bressan, S.; Carter, R.; Hylén, M.; Kristensson, I.; Lakhanpaul, M.; Mintegi, S.; Moll, H.A.; Neill, S. Parental help-seeking behaviour for, and care of, a sick or injured child during the COVID-19 pandemic: A European online survey. BMC Health Serv. Res. 2023, 23, 397. [Google Scholar]
- Nicholson, E.; McDonnell, T.; De Brún, A.; Barrett, M.; Bury, G.; Collins, C.; Hensey, C.; McAuliffe, E. Factors that influence family and parental preferences and decision making for unscheduled paediatric healthcare–systematic review. BMC Health Serv. Res. 2020, 20, 663. [Google Scholar] [CrossRef]
- Watson, G.; Pickard, L.; Williams, B.; Hargreaves, D.; Blair, M. ‘Do I, don’t I?’A qualitative study addressing parental perceptions about seeking healthcare during the COVID-19 pandemic. Arch. Dis. Child. 2021, 106, 1118–1124. [Google Scholar]
- Kadambari, S.; Abo, Y.-N.; Phuong, L.K.; Osowicki, J.; Bryant, P.A. Decrease in infection-related hospital admissions during COVID-19: Why are parents avoiding the doctor? Pediatr. Infect. Dis. J. 2020, 39, e385–e386. [Google Scholar] [CrossRef]
- Jansen, D.E.; Illy, K.E. Delayed presentation to regular Dutch paediatric care in COVID-19 times: A national survey. BMJ Paediatr. Open 2020, 4, e000834. [Google Scholar] [CrossRef]
- Duncanson, M.; Wheeler, B.J.; Jelleyman, T.; Dalziel, S.R.; McIntyre, P. Delayed access to care and late presentations in children during the COVID-19 pandemic New Zealand-wide lockdown: A New Zealand Paediatric Surveillance Unit study. J. Paediatr. Child Health 2021, 57, 1600–1604. [Google Scholar] [CrossRef] [PubMed]
- Wong Shee, A.; Donaldson, A.; Clapham, R.P.; Aitken, J.C.; Ananthapavan, J.; Ugalde, A.; Versace, V.L.; Mc Namara, K. Identifying health and healthcare priorities in rural areas: A concept mapping study informed by consumers, health professionals and researchers. Health Res. Policy Syst. 2024, 22, 105. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.T.; Lewis, R.W.; Kataoka, S.; Schenke, K.; Vandell, D.L. Out-of-school time and behaviors during adolescence. J. Res. Adolesc. 2018, 28, 284–293. [Google Scholar] [CrossRef]
- Sheridan, G.A.; Nagle, M.; Russell, S.; Varghese, S.; O’Loughlin, P.F.; Boran, S.; Taylor, C.; Harty, J.A. Pediatric trauma and the COVID-19 pandemic: A 12-year comparison in a level-1 trauma center. HSS J. 2020, 16 (Suppl. S1), 92–96. [Google Scholar] [CrossRef]
- Arundell, L.; Salmon, J.; Timperio, A.; Sahlqvist, S.; Uddin, R.; Veitch, J.; Ridgers, N.D.; Brown, H.; Parker, K. Physical activity and active recreation before and during COVID-19: The Our Life at Home study. J. Sci. Med. Sport 2022, 25, 235–241. [Google Scholar] [CrossRef]
- Ramgopal, S.; Dunnick, J.; Siripong, N.; Conti, K.A.; Gaines, B.A.; Zuckerbraun, N.S. Seasonal, weather, and temporal factors in the prediction of admission to a pediatric trauma center. World J. Surg. 2019, 43, 2211–2217. [Google Scholar] [CrossRef]
- Rossi, L.; Behme, N.; Breuer, C. Physical activity of children and adolescents during the COVID-19 pandemic—A scoping review. Int. J. Environ. Res. Public Health 2021, 18, 11440. [Google Scholar] [CrossRef] [PubMed]




| Factor | Pre-COVID | COVID | Post-COVID | Total | p-Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| (2018–2019) | (2020–2021) | (2022–2023) | |||||||
| n = 21,076 | n | % | n | % | n | % | n | % | |
| Gender | |||||||||
| Female | 3189 | 35.7% | 2992 | 33.5% | 2745 | 30.8% | 8926 | 100.0% | <0.001 |
| Male | 4310 | 35.5% | 4066 | 33.5% | 3770 | 31.0% | 12,146 | 100.0% | <0.001 |
| Age group | |||||||||
| 0–4 years | 2186 | 35.0% | 2149 | 34.5% | 1900 | 30.5% | 6235 | 100.0% | <0.001 |
| 5–9 years | 2341 | 36.3% | 2200 | 34.2% | 1903 | 29.5% | 6444 | 100.0% | <0.001 |
| 10–14 years | 2972 | 35.4% | 2709 | 32.3% | 2712 | 32.3% | 8393 | 100.0% | <0.001 |
| Where presented | |||||||||
| non-VEMD | 2952 | 34.3% | 2710 | 31.5% | 2947 | 34.2% | 8611 | 100.0% | 0.001 |
| VEMD | 4547 | 36.5% | 4348 | 34.9% | 3568 | 28.6% | 12,461 | 100.0% | <0.001 |
| Year | Pre-COVID (2018–2019) | COVID (2020–2021) | Post-COVID (2022–2023) | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| 0–4 years | Female | 963 | 30.2% | 958 | 32.0% | 852 | 31.0% | 0.014 |
| 5–9 years | 1009 | 31.6% | 965 | 32.3% | 857 | 31.2% | 0.002 | |
| 10–14 years | 1217 | 38.2% | 1069 | 35.7% | 1036 | 37.8% | <0.001 | |
| 0–4 years | Male | 1223 | 28.4% | 1191 | 29.3% | 1048 | 27.8% | <0.001 |
| 5–9 years | 1332 | 30.9% | 1235 | 30.4% | 1046 | 27.7% | <0.001 | |
| 10–14 years | 1755 | 40.7% | 1640 | 40.3% | 1676 | 44.5% | 0.129 | |
| Total | 7499 | 7058 | 6515 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kloot, K.; Peck, B.; Terry, D. Paediatric Emergency Injury Presentations During the COVID-19 Pandemic in Regional Victoria, Australia: A Silver Lining? Emerg. Care Med. 2025, 2, 47. https://doi.org/10.3390/ecm2040047
Kloot K, Peck B, Terry D. Paediatric Emergency Injury Presentations During the COVID-19 Pandemic in Regional Victoria, Australia: A Silver Lining? Emergency Care and Medicine. 2025; 2(4):47. https://doi.org/10.3390/ecm2040047
Chicago/Turabian StyleKloot, Kate, Blake Peck, and Daniel Terry. 2025. "Paediatric Emergency Injury Presentations During the COVID-19 Pandemic in Regional Victoria, Australia: A Silver Lining?" Emergency Care and Medicine 2, no. 4: 47. https://doi.org/10.3390/ecm2040047
APA StyleKloot, K., Peck, B., & Terry, D. (2025). Paediatric Emergency Injury Presentations During the COVID-19 Pandemic in Regional Victoria, Australia: A Silver Lining? Emergency Care and Medicine, 2(4), 47. https://doi.org/10.3390/ecm2040047








