No Learner Left Behind: How Medical Students’ Background Characteristics and Psychomotor/Visual–Spatial Abilities Correspond to Aptitude in Learning How to Perform Clinical Ultrasounds †
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Selection of Participants
2.3. Data Collection and Processing
2.4. Data Analysis
3. Results
| N | % (of Total 97) | |
|---|---|---|
| Total Students | 97 | |
| Medical School | ||
| Ross University | 27 | 28% |
| Saint George’s University | 70 | 72% |
| Hand Dominance | ||
| Left | 11 | 11% |
| Right | 86 | 89% |
| Number Students (Out N = 97) | Percentage Chance | p-Value (Chi-Squared) | |
|---|---|---|---|
| Medical School | |||
| Ross University | 27 | 55.0% | 1.0 |
| Saint George’s University | 70 | 56.6% | 1.0 |
| Hand Dominance | |||
| Left | 11 | 79.8% | 0.14 |
| Right | 86 | 55.6% | 0.14 |
| Frequency of Video Game Playing | |||
| Never | 7 | 46.3% | 0.86 |
| Occasionally (monthly) | 38 | 55.8% | 0.86 |
| Often (weekly) | 37 | 58.9% | 0.86 |
| Daily | 15 | 59.2% | 0.86 |
| Length of Time/Day on Computer | |||
| Less than 2 h/day | 10 | 59.8% | 0.95 |
| 2 to 5 h/day | 36 | 56.5% | 0.95 |
| 5 h and more/day | 31 | 56.3% | 0.95 |
| Median | Mean | Standard Deviation | p-Value (t-Test) | 95%CI [±95%CI] | |
|---|---|---|---|---|---|
| Rating on Anatomical Knowledge | 3.0 | 3.0 | 0.779 | 0.194 | 0.15 [3.05–3.35] |
| Study Resources Usefulness to Learn Anatomy | |||||
| Anatomy books | 4.0 | 3.69 | 0.979 | 0.755 | 0.19 [3.50–3.88] |
| Cadavers | 5.0 | 4.35 | 0.844 | 0.0237 | 0.17 [4.18–4.52] |
| Computer 2D images | 3.0 | 3.05 | 1.04 | 0.692 | 0.21 [2.84–3.26] |
| 3D models | 4.0 | 4.07 | 0.979 | 0.995 | 0.19 [3.88–4.26] |
| Pre-dissected organ models | 4.0 | 3.75 | 1.02 | 0.518 | 0.20 [3.55–2.95] |
| Skill at Map Interpretation and Finding Directions | 4.0 | 4.05 | 0.911 | 0.674 | 0.18 [3.87–4.26] |
| Interest Level in Learning and Training on Ultrasound | 5 | 4.49 | 0.635 | 0.111 | 0.13 [4.36–4.62] |
| Median | Mean | Standard Deviation | p-Value (t-Test) | 95%CI [±95%CI] | |
|---|---|---|---|---|---|
| Psychomotor Task Score | |||||
| Score 1 | 44 | 43.6 | 4.13 | 0.19 | 0.82 [42.78–44.42] |
| Score 2 | 40 | 39.5 | 5.92 | 0.00636 | 1.17 [38.33–40.67] |
| Visual–spatial Task Score (max 30) | 25 | 24 | 5.17 | 0.00777 | 1.02 [22.98–25.02] |
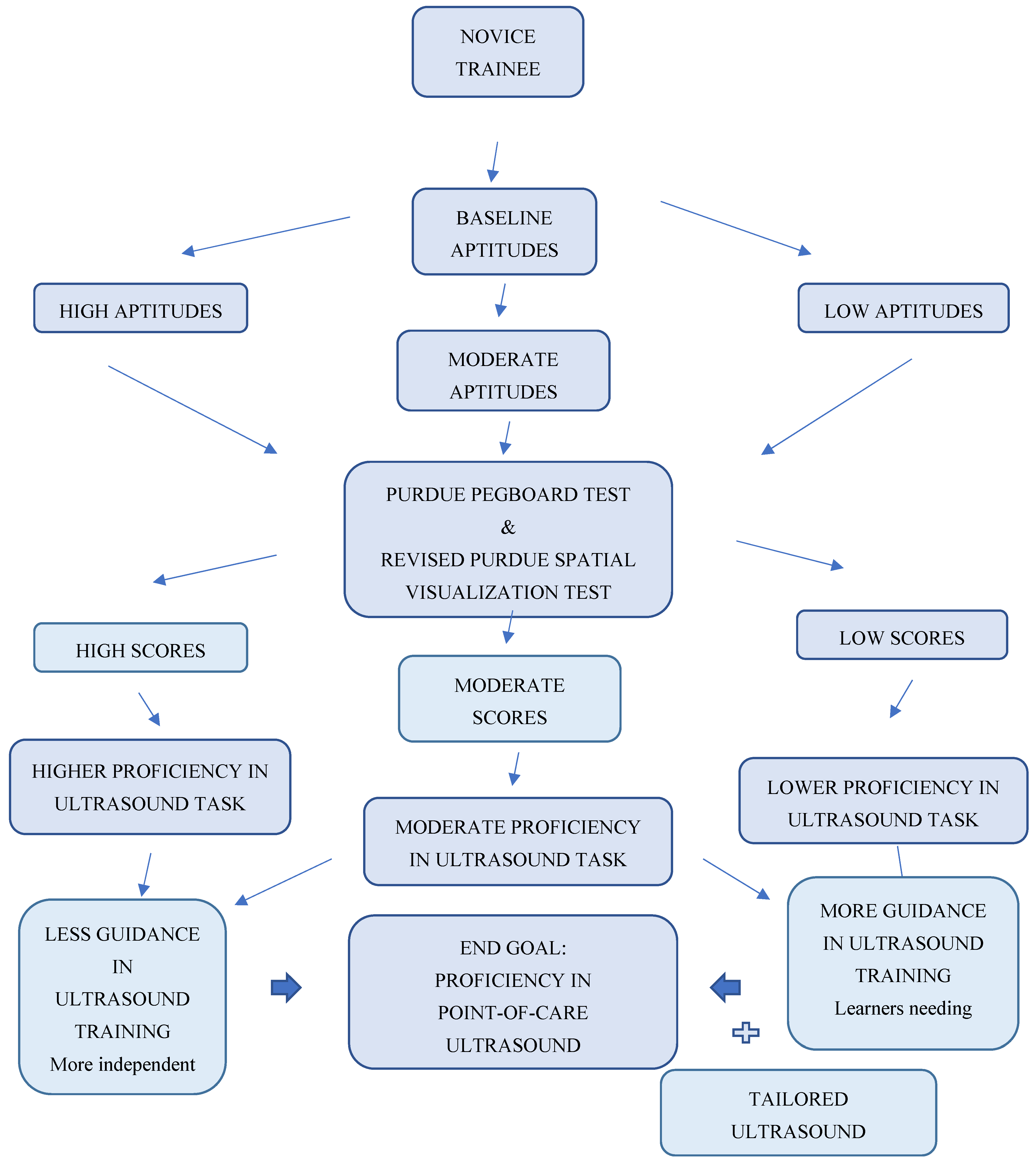
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- Which medical school do you attend?
- Age?
- Dominant hand, left or right?
- How would you rate your current knowledge and memory of human anatomy?
- Rate on a scale from 1–5 the usefulness of the following study resources for learning human anatomy.
- Anatomy books?
- Cadavers?
- Computer 2D images?
- 3D models?
- Pre-dissected organ models?
- How skilled are you at interpreting a geographical map and finding directions?
- How often do you play video games (of any type)?
- Never
- Occasionally (monthly basis)
- Often (weekly basis)
- Daily
- How much time per day do you work on a computer?
- Less than 2 h/day
- 2 to 5 h/day
- 5 h and more/day
- Rate your interest level in learning and training on an ultrasound machine.
Appendix B

- Using the right hand only: First, an individual uses only their right hand to place small pins into a series of holes in a column. They have 30 s for this task. The examiner counts the number of pins placed in the holes and records this score. The board is then reset.
- Using the left hand only: Next, the individual uses only their left hand to place small pins into the column holes. Again, they have 30 s for this task. The examiner counts the number of pins placed in the holes and records this score. The board is then reset.
- Using both hands: Next, the individual has 30 s to place pins in two adjacent columns of holes using both hands at the same time. The examiner counts the number of pins placed in the holes on each side and records this score. The board is then reset.
- Assembly apparatus: Lastly, using both hands, individuals assemble a four-part unit consisting of a pin, washer, collar, and washer (in that order). They have 60 s for this task. The score equals the number of each part successfully placed.
- Two final scores are obtained. Score number 1 is the summation of steps 1, 2, and 3. Score number 2 is the final score of Step 4 only.
Appendix C

Appendix D
| SCORE | 1 | 2 | 3 |
| Holds probe in correct orientation | 2 corrections | 1 correction | No correction |
| SCORE | 1 | 2 | 3 |
| Places probe on correct spot on the model | 2 corrections | 1 correction | No correction |
| SCORE | 1 | 2 | 3 |
| Holds probe at correct angle | 2 corrections | 1 correction | No correction |
| SCORE | 1 | 2 | 3 |
| Properly identifies the chambers of the heart viewed | 3 guesses | 2 guesses | 1 guess |
| SCORE | 1 | 2 | 3 |
| Captures image at best gain quality | Sub-optimal | Acceptable | Optimal |
| SCORE | 1 | 2 | 3 |
| Places image at best depth | Sub-optimal | Acceptable | Optimal |
| SCORE | 1 | 2 | 3 |
| Stores image | 2 reminders | 1 reminder | No reminder |
| SCORE | 1 | 2 | 3 |
| Total time to obtain image | >5 Minutes | 1-5 Minutes | 1 Minute |
| SCORE | 1 | 2 | 3 |
| Overall image quality | Poor | Good | Excellent |
Appendix E
References
- Cross, S.S. Aptitude testing and assessment of training progress in histopathology. Curr. Diagn. Pathol. 2005, 11, 299–307. [Google Scholar] [CrossRef]
- Smith, H.M.; Kopp, S.L.; Johnson, R.L.; Long, T.R.; Cerhan, J.H.; Hebl, J.R. Looking into learning: Visuospatial and psychomotor predictors of ultrasound-guided procedural performance. Reg. Anesth. Pain Med. 2012, 37, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Enochsson, L.; Isaksson, B.; Tour, R.; Kjellin, A.; Hedman, L.; Wredmark, T.; Tsai-Felländer, L. Visuospatial skills and computer game experience influence the performance of virtual endoscopy. J. Gastrointest. Surg. 2004, 8, 874–880. [Google Scholar] [CrossRef] [PubMed]
- Early, D.S.; Hall, M.; Aslanian, H.R.; Casey, B.; Burbridge, R.; Chak, A.; Wani, S. A prospective, multicenter study researching the aptitude of trainees in endoscopic ultrasonography (rate US study) using cumulative sum analysis. (Abstract) Gastrointestinal Endoscopy. In Proceedings of the Conference: Digestive Disease Week, DDW 2014 ASGE, Chicago, IL, USA, 3–6 May 2014. [Google Scholar]
- Ritter, E.M.; McClusky, D.A.; Gallagher, A.G.; Enochsson, L.; Smith, C.D. Perceptual, visuospatial, and psychomotor abilities correlate with duration of training required on a virtual-reality flexible endoscopy simulator. Am. J. Surg. 2006, 192, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, D.; Sweet, L.; Hyett, J. Psychomotor Skills in Medical Ultrasound Imaging. J. Ultrasound Med. 2014, 33, 1349–1352. [Google Scholar] [CrossRef] [PubMed]
- Clem, D.W.; Donaldson, J.; Curs, B.; Anderson, S.; Hdeib, M. Role of Spatial Ability as a Probable Ability Determinant in Skill Acquisition for Sonographic Scanning. J. Ultrasound Med. 2013, 32, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Mulder, T.A.; van de Velde, T.; Dokter, E.; Boekestijn, B.; Olgers, T.J.; Bauer, M.P.; Hierck, B.P. Unravelling the skillset of point-of-care ultrasound: A systematic review. Ultrasound J. 2023, 15, 19. [Google Scholar] [CrossRef] [PubMed]
- Jian, Y.; Bakar, J. Comparing cognitive load in learning spatial ability: Immersive learning environment vs. digital learning media. Discov. Sustain. 2024, 5, 111. [Google Scholar] [CrossRef]
- Mackie, R. Multiple Intelligences and Graphic Design Ability in Five North Carolina Community Colleges; Adult and Community College Education; North Carolina State University: Raleigh, NC, USA, 2005. [Google Scholar]
- Castro-Alonso, J.C.; Ayres, P.; Sweller, J. Instructional visualizations, cognitive load theory, and visuospatial processing. Visuospatial Process. Educ. Health Nat. Sci. 2019, 5, 111–143. [Google Scholar]
- Changiz, T.; Amouzeshi, Z.; Najimi, A.; Adibi, P. A narrative review of psychomotor abilities in medical sciences: Definition, categorization, tests, and training. J. Res. Med. Sci. 2021, 26, 69. [Google Scholar] [CrossRef] [PubMed]
- Purdue Pegboard Test Manual PDF. Model 32020A User’s Manual. Available online: www.lafayetteinstrument.com (accessed on 3 May 2015).
- Yoon, S.Y. Psychometric Properties of the Revised Purdue Spatial Visualization Tests: Visualization of Rotations (The Revised PSVT:R). Ph.D. Thesis, Purdue University, West Lafayette, IN, USA, 2011. Order Number: 3480934. [Google Scholar]
- Maurice-Ventouris, M.; Moran, H.R.M.; Alharbi, M.; Ahn, B.T.; Harley, J.M.; Lachapelle, K.J. The study of visuospatial abilities in trainees: A scoping review and proposed model. Surg. Open Sci. 2021, 5, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Leppink, J.; Heuvel, A.V.D. The evolution of cognitive load theory and its application to medical education. Perspect. Med. Educ. 2015, 4, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Akhigbe, T. Cognitivism and Ultrasound Skills in Emergency Medicine Training: From Theory to Practice. Int. J. Med. Rev. 2018, 5, 47–49. [Google Scholar] [CrossRef]
- Wani, S.; Hall, M.; Keswani, R.N.; Aslanian, H.R.; Casey, B.; Burbridge, R.; Early, D. Variation of aptitude of trainees in endoscopic ultrasonography, based on cumulative sum analysis. Clin. Gastroenterol. Hepatol. 2015, 13, 1318–1325. [Google Scholar] [CrossRef] [PubMed]
- Ayala, S.; Abrams, E.; Chiricolo, G. Assessing medical student background characteristics, psychomotor and visual-spatial abilities and how they correlate to aptitude in learning medical ultrasound. Academic Emergency Medicine. In Proceedings of the Conference: 2014 World Congress of Ultrasound in Medical Education (WCUME), Portland, OR, USA, 10–12 October 2014. [Google Scholar]
- Ayala, S.; Abrams, E.; Chiricolo, G. Assessing medical student background characteristics, psychomotor and visual-spatial abilities and how they correlate to aptitude in learning medical ultrasound. Academic Emergency Medicine. In Proceedings of the Conference: 2015 Annual Meeting of the Society for Academic Emergency Medicine, SAEM 2015, San Diego, CA, USA, 12–15 May 2015. [Google Scholar]
- Chapman, E. Is there a relationship between ultrasound scanning ability and visuospatial perception or psychomotor ability? Should this type of assessment be employed as a pre-selection tool for ultrasound training? Br. Med. Ultrasound Soc. 2016, 24, 214–221. [Google Scholar]
- Kondrashova, T.; Kondrashov, P. Integration of Ultrasonography into the Undergraduate Medical Curriculum: Seven Years of Experience. Mo. Med. 2018, 115, 38–43. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ayala, S.; Abrams, E.R.; Melniker, L.A.; Melville, L.D.; Chiricolo, G.C. No Learner Left Behind: How Medical Students’ Background Characteristics and Psychomotor/Visual–Spatial Abilities Correspond to Aptitude in Learning How to Perform Clinical Ultrasounds. Emerg. Care Med. 2025, 2, 31. https://doi.org/10.3390/ecm2030031
Ayala S, Abrams ER, Melniker LA, Melville LD, Chiricolo GC. No Learner Left Behind: How Medical Students’ Background Characteristics and Psychomotor/Visual–Spatial Abilities Correspond to Aptitude in Learning How to Perform Clinical Ultrasounds. Emergency Care and Medicine. 2025; 2(3):31. https://doi.org/10.3390/ecm2030031
Chicago/Turabian StyleAyala, Samuel, Eric R. Abrams, Lawrence A. Melniker, Laura D. Melville, and Gerardo C. Chiricolo. 2025. "No Learner Left Behind: How Medical Students’ Background Characteristics and Psychomotor/Visual–Spatial Abilities Correspond to Aptitude in Learning How to Perform Clinical Ultrasounds" Emergency Care and Medicine 2, no. 3: 31. https://doi.org/10.3390/ecm2030031
APA StyleAyala, S., Abrams, E. R., Melniker, L. A., Melville, L. D., & Chiricolo, G. C. (2025). No Learner Left Behind: How Medical Students’ Background Characteristics and Psychomotor/Visual–Spatial Abilities Correspond to Aptitude in Learning How to Perform Clinical Ultrasounds. Emergency Care and Medicine, 2(3), 31. https://doi.org/10.3390/ecm2030031






