Does the Use of Prehospital Emergency Care Units in Inter-Hospital Transfers Affect Regional Prehospital Emergency Care Readiness?—A Finnish Pilot Study
Abstract
1. Introduction
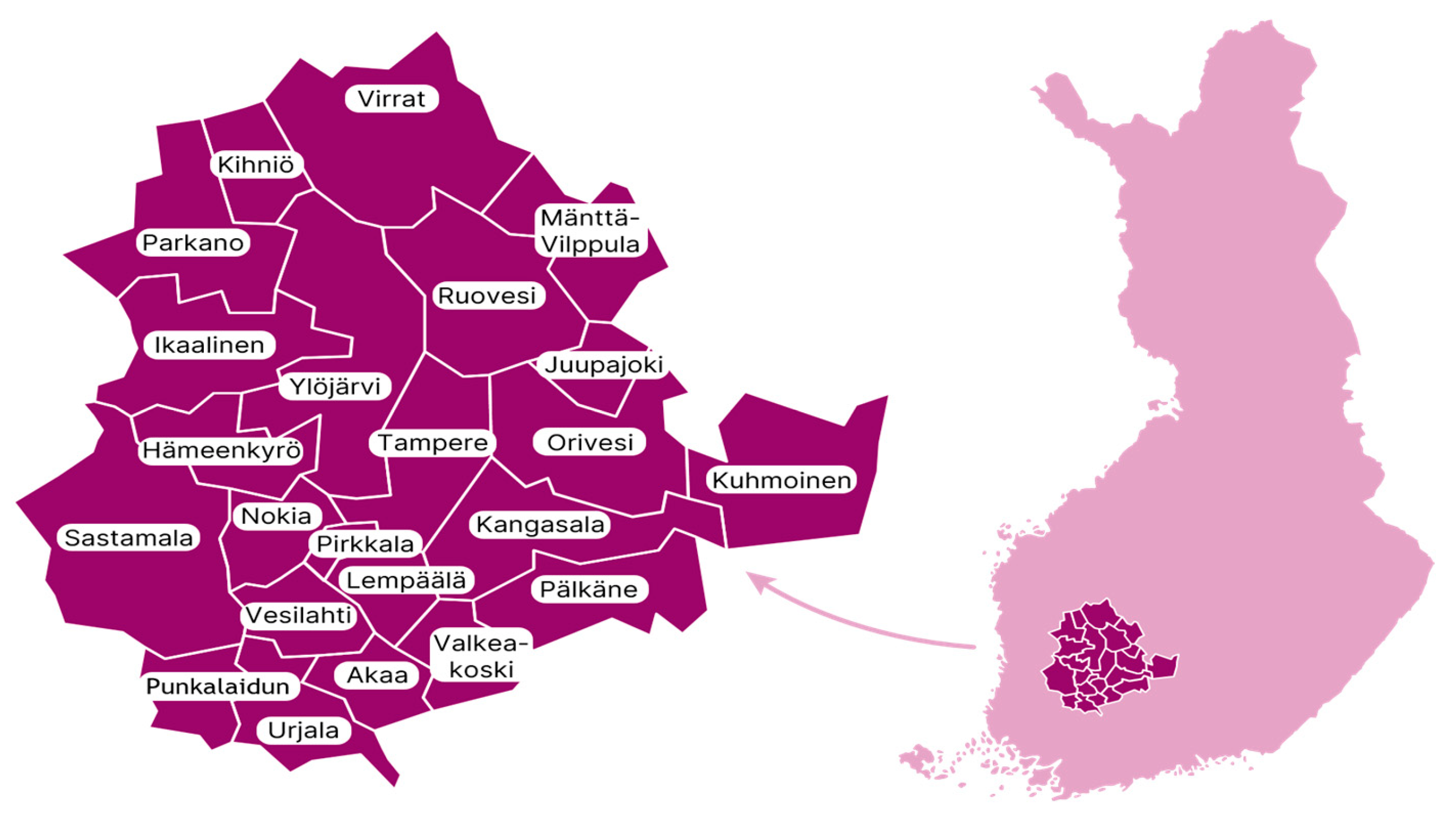
2. Materials and Methods
3. Results
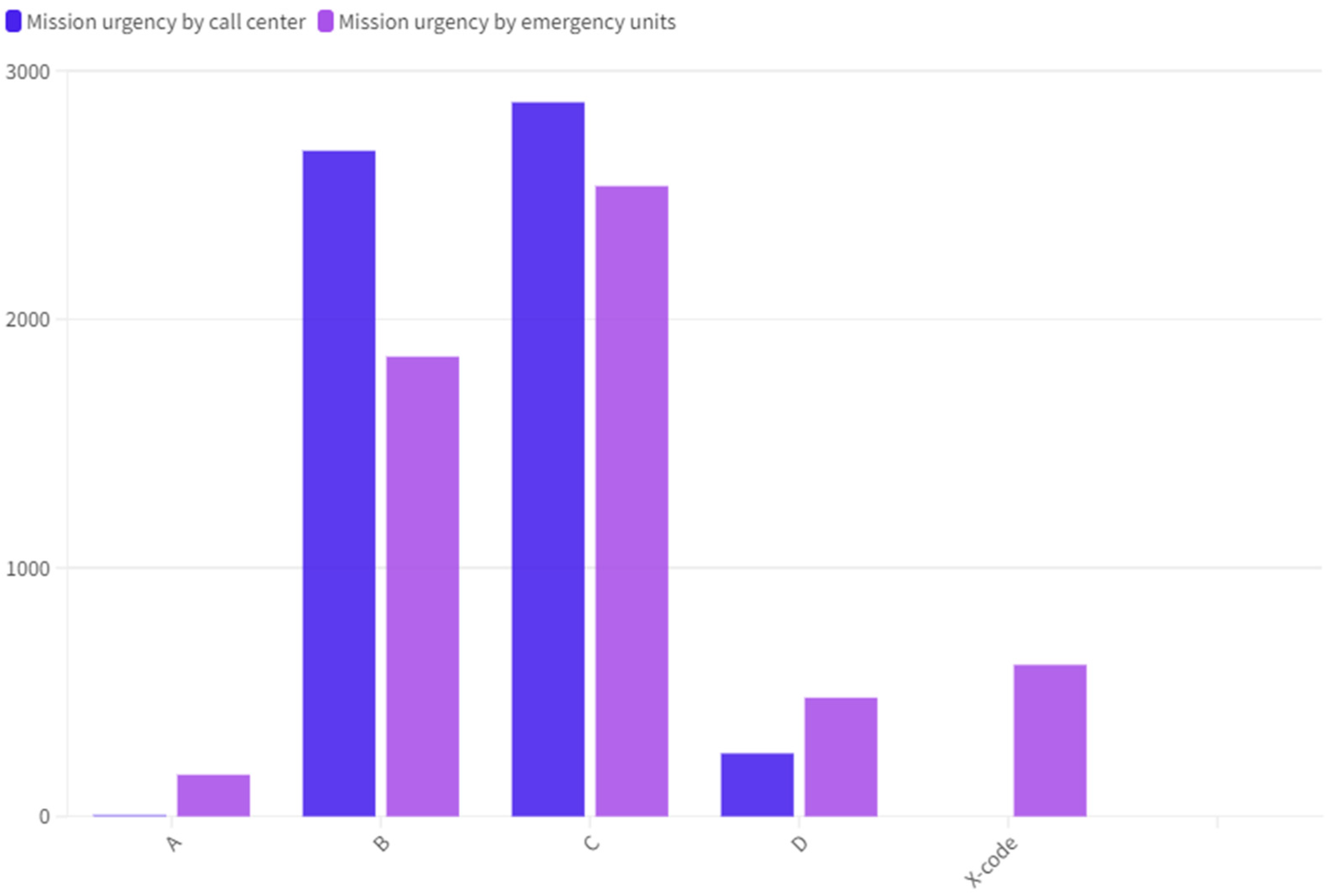
3.1. Number and Type of Prehospital Emergency Care Inter-Hospital Transfers
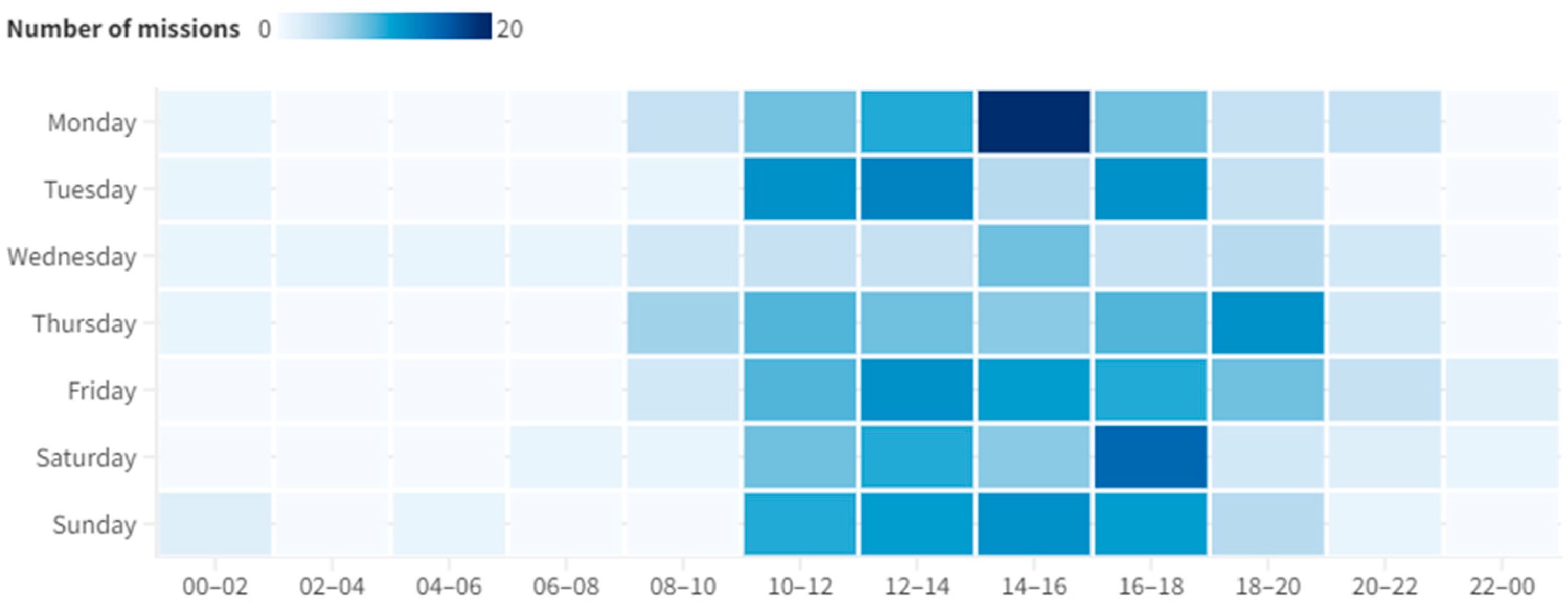
3.2. The Concentrated Strain on the Readiness of Prehospital Emergency Care Services in Certain Regions and Health Care Centers by Mission Number, Duration, and Time of Day
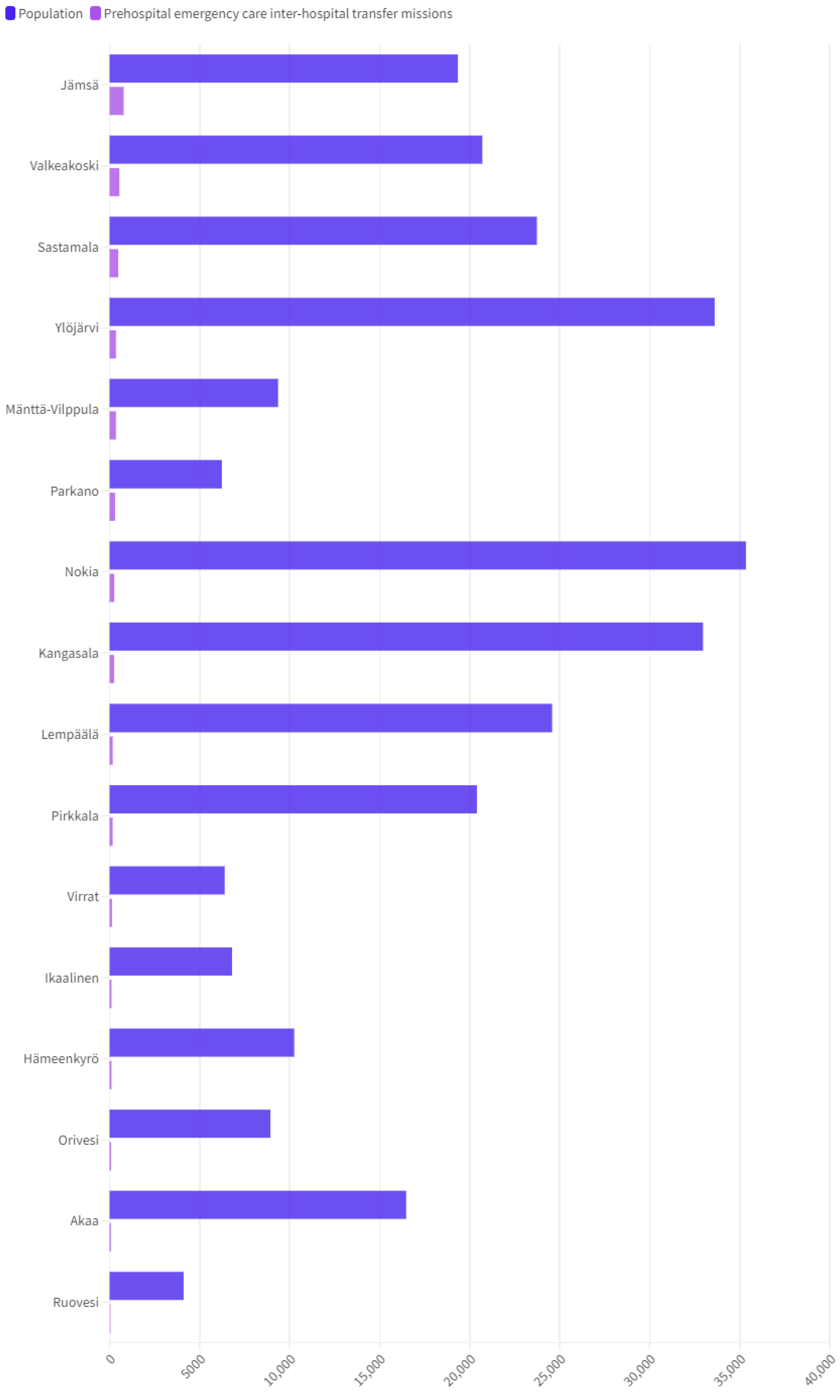
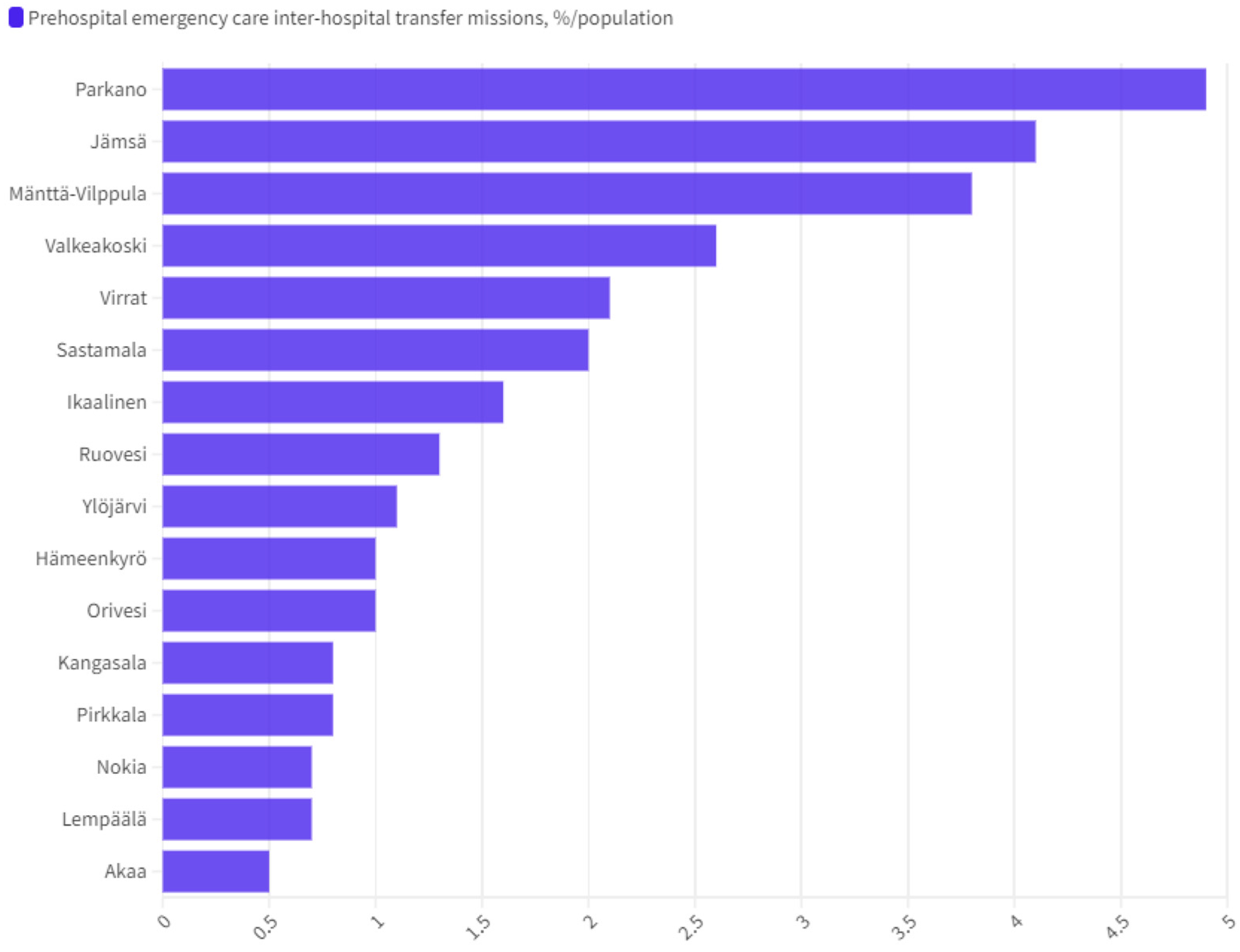
3.3. Occurrence of Prehospital Emergency Care Inter-Hospital Transfer Missions and Their Incidence with Reference to the Population of Different Municipalities in the Wellbeing Services County of Pirkanmaa
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A

Appendix B



References
- Booker, M.J.; Shaw, A.R.G.; Purdy, S. Why do patients with ‘primary care sensitive’ problems access ambulance services? A systematic mapping review of the literature. BMJ Open 2015, 5, e007726. [Google Scholar] [CrossRef] [PubMed]
- Vuilleumier, S.; Fiorentino, A.; Dénéréaz, S.; Spichiger, T. Identification of new demands regarding prehospital care based on 35,188 missions in 2018. BMC Emerg. Med. 2021, 21, 63. [Google Scholar] [CrossRef] [PubMed]
- Ilkka, L. Emergency Medical Services (EMS) in Finland: National Data Management as a Path to Better Prehospital Care. Ph.D. Thesis, University of Eastern Finland, Kuopio, Finland, 20 May 2022. Available online: https://urn.fi/URN:ISBN:978-952-61-4543-3 (accessed on 20 May 2024).
- Paulin, J.; Kurola, J.; Koivisto, M.; Iirola, T. EMS non-conveyance: A safe practice to decrease ED crowding or a threat to patient safety? BMC Emerg. Med. 2021, 21, 115. [Google Scholar] [CrossRef] [PubMed]
- Hoikka, M. Prehospital Risk Assesment and Patient Outcome—A Population Based Study in Northern Finland. Ph.D. Thesis, University of Oulu, Oulu, Finland, 7 December 2018. Available online: https://urn.fi/URN:ISBN:9789526221366 (accessed on 15 May 2024).
- Magnusson, C.; Herlitz, J.; Axelsson, C. Patient characteristics, triage utilisation, level of care, and outcomes in an unselected adult patient population seen by the emergency medical services: A prospective observational study. BMC Emerg. Med. 2020, 20, 7. [Google Scholar] [CrossRef] [PubMed]
- Kirves, H. Ennakoimattomat kiireelliset siirtokuljetukset—Hyvin suunniteltu on puoliksi tehty. Finnanest 2018, 4, 280–285. Available online: https://say.fi/files/kirves_ennakoimattomat.pdf (accessed on 15 May 2024).
- Nair, D.; Vaughan, F.; Bennett, K. A Chart Review of Acute Care Inter-Hospital Transfers from Rural WV Hospitals. Marshall J. Med. 2017, 3, 49. Available online: https://mds.marshall.edu/cgi/viewcontent.cgi?article=1100&context=mjm (accessed on 20 May 2024). [CrossRef]
- Limmer, A.M.; Edye, M.B. Interhospital transfer delays emergency abdominal surgery and prolongs stay. ANZ J. Surg. 2017, 87, 867–872. [Google Scholar] [CrossRef] [PubMed]
- Rathod, K.S.; Jain, A.K.; Firoozi, S.; Lim, P.; Boyle, R.; Nevett, J.; Dalby, M.C.; Kalra, S.; Malik, I.S.; Sirker, A.; et al. Outcome of inter-hospital transfer versus direct admission for primary percutaneous coronary intervention: An observational study of 25,315 patients with ST-elevation myocardial infarction from the London Heart Attack Group. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 948–957. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, I.E.R.; Arusoo, T.; Sigounas, D. Impact of Direct Admission Versus Interfacility Transfer on Endovascular Treatment Outcomes for Acute Ischemic Stroke: Systematic Review and Meta-Analysis. World Neurosurg. 2021, 152, e387–e397. [Google Scholar] [CrossRef] [PubMed]
- Waalwijk, J.F.; Lokerman, R.D.; van der Sluijs, R.; Fiddelers, A.A.A.; den Hartog, D.; Leenen, L.P.H.; Poeze, M.; van Heijl, M. Pre-hospital Trauma Triage Research Collaborative (PTTRC). The influence of inter-hospital transfers on mortality in severely injured patients. Eur. J. Trauma Emerg. Surg. 2023, 49, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Ebben, R.H.A.; Vloet, L.C.M.; Speijers, R.F.; Tönjes, N.W.; Loef, J.; Pelgrim, T.; Hoogeveen, M.; Berben, S.A.A. A patient-safety and professional perspective on non-conveyance in ambulance care: A systematic review. Scand J. Trauma Resusc. Emerg. Med. 2017, 17, 71. [Google Scholar] [CrossRef] [PubMed]
- Gray, J.T.; Wardrope, J. Introduction of non-transport guidelines into an ambulance service: A retrospective review. Emerg. Med. J. 2007, 24, 727–729. [Google Scholar] [CrossRef] [PubMed]
- Kindermann, D.R.; Mutter, R.L.; Houchens, R.L.; Barrett, M.L.; Pines, J.M. Emergency Department Transfers and Transfer Relationships in United States Hospitals. Acad. Emerg. Med. 2015, 22, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Social Affairs and Health. Available online: https://stm.fi/ensihoito (accessed on 15 May 2024).
- Health Care Act 1326/2010. Available online: https://www.finlex.fi/en/laki/kaannokset/2010/en20101326_20131293.pdf (accessed on 14 May 2024).
- Wellbeing Services County of Pirkanmaa. Available online: https://pirha.cloudnc.fi/fi-FI/Toimielimet/Aluehallitus/Kokous_2442023/Ensihoitopalvelun_palvelutasopaatos_vuos(6789) (accessed on 14 May 2024).
- Statistics Finland. Available online: https://www.stat.fi/tup/alue/kuntienavainluvut.html#?active1=KU702&year=2023 (accessed on 15 May 2024).
- Keiski, R.; Hämäläinen, K.; Karhunen, M.; Löfström, E.; Näreaho, S.; Varantola, K.; Spoof, S.K.; Tarkiainen, T.; Kaila, E.; Sairio, A.; et al. The Finnish Code of Conduct for Research Integrity and Procedures for Handling Alleged Violations of Research Integrity in Finland; Finnish National Board on Research Integrity TENK: Helsinki, Finland, 2023; Volume 4, Available online: https://tenk.fi/sites/default/files/2023-11/RI_Guidelines_2023.pdf (accessed on 20 May 2024).
- Kohonen, I.; Kuula-Luumi, A.; Spoof, S.K. The Ethical Principles of Research with Human Participants and Ethical Review in the Human Sciences in Finland; Finnish National Board on Research Integrity TENK: Helsinki, Finland, 2019; Volume 3, Available online: https://tenk.fi/sites/default/files/2021-01/Ethical_review_in_human_sciences_2020.pdf (accessed on 15 May 2024).
- Atmore, C.; Dovey, S.; Gauld, R.; Gray, A.R.; Stokes, T. Do people living in rural and urban locations experience differences in harm when admitted to hospital? A cross-sectional New Zealand general practice records review study. BMJ Open 2021, 6, e046207. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.; Rimmer, E.; Blattner, K.; Withington, S.; Ram, S.; Topping, M.; Kaka, H.; Bergin, A.; Pirini, J.; Smith, M.; et al. A retrospective observational study examining interhospital transfers from six New Zealand rural hospitals in 2019. Aust. J. Rural. Health 2023, 31, 921–931. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lehtimäki, S.; Lahelma, J.; Aunola, A.; Nordquist, H. Does the Use of Prehospital Emergency Care Units in Inter-Hospital Transfers Affect Regional Prehospital Emergency Care Readiness?—A Finnish Pilot Study. Emerg. Care Med. 2024, 1, 312-325. https://doi.org/10.3390/ecm1030032
Lehtimäki S, Lahelma J, Aunola A, Nordquist H. Does the Use of Prehospital Emergency Care Units in Inter-Hospital Transfers Affect Regional Prehospital Emergency Care Readiness?—A Finnish Pilot Study. Emergency Care and Medicine. 2024; 1(3):312-325. https://doi.org/10.3390/ecm1030032
Chicago/Turabian StyleLehtimäki, Simon, Joonas Lahelma, Anssi Aunola, and Hilla Nordquist. 2024. "Does the Use of Prehospital Emergency Care Units in Inter-Hospital Transfers Affect Regional Prehospital Emergency Care Readiness?—A Finnish Pilot Study" Emergency Care and Medicine 1, no. 3: 312-325. https://doi.org/10.3390/ecm1030032
APA StyleLehtimäki, S., Lahelma, J., Aunola, A., & Nordquist, H. (2024). Does the Use of Prehospital Emergency Care Units in Inter-Hospital Transfers Affect Regional Prehospital Emergency Care Readiness?—A Finnish Pilot Study. Emergency Care and Medicine, 1(3), 312-325. https://doi.org/10.3390/ecm1030032






