1. Introduction
To improve survival rates in out-of-hospital cardiac arrest (OHCA), which has a poor outcome to date, it is crucial to direct attention to the locations where these events transpire. A comprehensive assessment of patient characteristics at the location of the OHCA occurrences provides valuable insights. These findings can be employed to devise more effective strategies, including widespread education of laypersons.
Certain daily human activities are associated with OHCA. Bathing [
1] and visiting toilet facilities are representative activities. In particular, toilets are considered a unique place where cardiac arrest is likely to occur because people use them not only for urination/defecation purposes but also when they feel unwell prior to a cardiac arrest. In addition, the detection of OHCA is delayed because toilets are typically enclosed, restricted spaces that provide maximum privacy. Therefore, the outcome for OHCA in toilets is expected to be poor. Except in studio apartments, household toilets and bathrooms are generally separated in Japan, making them suitable for evaluating OHCA in the toilets except when patients are bathing.
The previous two small-scale retrospective studies of OHCA in toilets have reported poor outcomes [
2,
3]. However, factors associated with surviving OHCA in the toilet and other detailed patient characteristics are unknown. Therefore, although a toilet is one of the most familiar places in a person’s daily life, little is known regarding the actual status of OHCA that occurs in toilets. Elucidating such an association could help develop more effective strategies to improve survival after OHCA.
Herein, we aimed to identify factors associated with a neurologically favourable 1-month survival of OHCA occurring in the toilet using a national Japanese database, which contains information on all patients with medical emergencies, including OHCA.
2. Materials and Methods
2.1. Study Population and Setting
In this nationwide observational study, we matched transport data from 23,472,547 all-Japan emergency medical service (EMS)-transported cases, including information on detailed characteristics and location and time records of patients registered from 1 January 2016 to 31 December 2019 who were not affected by the coronavirus disease 2019 pandemic, with data from 504,561 all-Japan OHCA cases based on standardised Utstein forms [
4]. In Japan, ambulance transportation is free of charge, and emergency medical technicians (EMTs) are not allowed to terminate resuscitation and transportation in the field unless an OHCA patient shows noticeable post-mortem changes. After excluding 39,463 cases of failed case matching, 4,307,440 cases of missing location data, including toilets, 5,466,213 non-medical (trauma) cases, and 13,298,604 non-OHCA cases, 360,827 OHCA cases were included in the final analysis. Of these, 4.1% (14,975) of OHCA occurred in the toilet. In addition, 1.9% (253,942) of all 13,659,431 emergency transports pertained to patients experiencing OHCA in toilets. The results revealed a high incidence of OHCA in all emergency patients transported from toilets (crude odds ratio [cOR] [95% confidence interval [CI]]: 2.52 [2.48–2.57]). Finally, we excluded 29,978 EMS-witnessed cardiac arrest cases because their characteristics and outcomes differed [
5,
6] and analysed the outcomes of 330,849 non-EMS-witnessed OHCA cases, with 4.2% (13,881) of these occurring in toilets.
2.2. Statistical Analysis
We calculated the cORs and 95% CIs using univariate analysis for significant variables. Multivariable logistic regression analysis was also used to examine whether factors associated with neurologically favourable 1-month survival (defined as Cerebral Performance Category 1–2 [
7]) differ between OHCA in toilets and OHCA in other places. The other places were defined as places other than toilets in the home and places other than public toilets outside the home.
p-values for subgroup interactions were calculated using multivariable interaction tests. In the multivariable analysis model, variables known to be potentially associated with outcomes of OHCA [
5,
6,
8] were added: age, sex, witness status with bystander classification (unwitnessed or witnessed by family, friend/colleague, others), arrest location (home or public locations), place of occurrence (toilets or other places), aetiology (presumed cardiac or not), prehospital initial electrocardiogram (ECG) rhythm (shockable or not), provision of bystander cardiopulmonary resuscitation (CPR), provision of public-access defibrillation (PAD), and time interval from call dispatch to arrival at patients (EMS response time).
All statistical analyses were performed using JMP ver. 17.0 (SAS Institute, Cary, NC, USA). The null hypothesis was evaluated for each analysis with a two-sided significance level of p < 0.05, with 95% CIs calculated using the profile likelihood.
3. Result
The incidence of OHCA in toilet rooms was higher among older people and during night-time and lower among children and during winter. Bystander-witnessed cases (cOR [95% CI]: 1.09 [1.02–1.16]) and unwitnessed cases (cOR [95% CI]: 1.20 [1.12–1.27]) were predominantly higher than EMS-witnessed cases. The proportion of initial shock-adapted ECG rhythm was lower (2.8% in the toilets vs. 4.8% in other places); however, the aetiology (cardiac and non-cardiac) did not significantly differ. Compared with OHCA in toilets at home, OHCA in public toilets was more likely to occur during the day, with fewer older adult patients, and was more frequently unwitnessed (
Table 1).
For non-EMS-witnessed OHCA cases, the bystander CPR rates (cOR [95% CI]: 0.44 [0.43–0.46]) and PAD rates (cOR [95% CI]: 0.12 [0.08–0.17]) were lower in OHCA in toilets than in other places (
Supplemental Table S1). The witness was predominantly a family member, and the incidence was also associated with toilets (5.6%; cOR [95% CI]: 1.32 [1.27–1.37]). In addition, bystander CPR was less frequent in OHCA in public toilets than in OHCA in home toilets (0.5% vs. 4.0%).
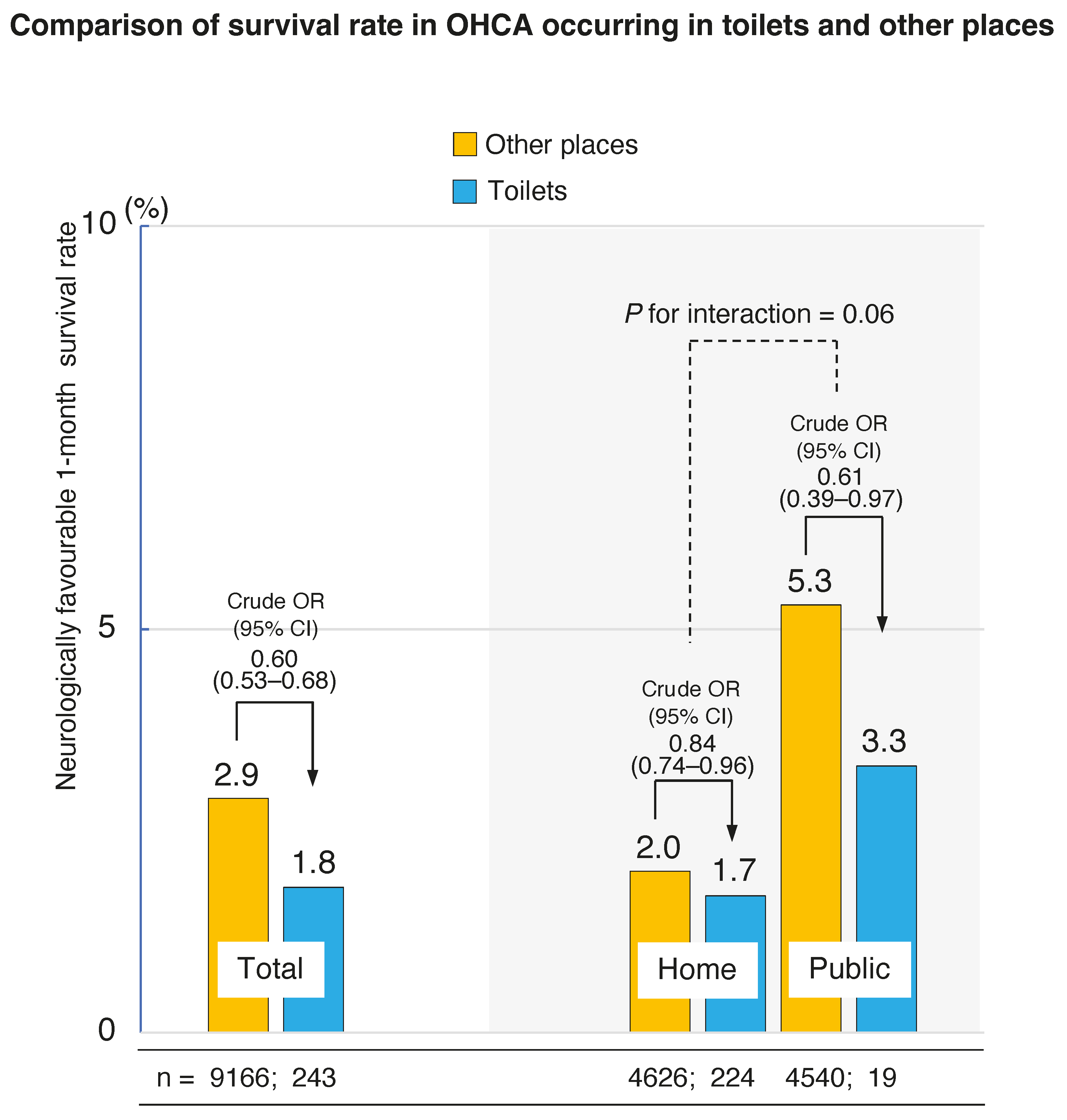
The rates of neurologically favourable 1-month survival (1.8% [243/13,881] in toilets vs. 2.9% [9166/316,968] in other places, cOR [95% CI]: 0.60 [0.53–0.68]) were significantly lower in toilets compared with those in other places. In addition, this survival rate was significantly lower at home (1.7% [224/13,310] in toilets vs. 2.0% in other places [4626/231,297], cOR [95% CI]: 0.84 [0.74–0.96]) than in public (3.3% [19/571] in toilets vs. 5.3% [4540/85,671] in other places, cOR [95% CI]: 0.61 [0.39–0.97]) (
Figure 1).
Multiple logistic regression analysis of the factors associated with neurologically favourable 1-month survival showed that age <18 years was significantly associated with improved neurologic outcomes for both OHCA in toilets and other spaces. Among patients with OHCA at home, those with OHCA in toilets had worse neurological outcomes than those with OHCA in other places. For patients with OHCA in toilets, those who had family-witnessed OHCA had better neurological outcomes than those with non-witnessed OHCA (adjusted odds ratio [aOR] [95% CI]: 3.41 [2.54–4.58]). However, OHCA witnessed by friends/colleagues had no association with outcomes (aOR [95% CI]: 1.52 [0.43–5.31]). For toilet room OHCA, PAD provision was significantly associated with better neurological survival, while presumed cardiac aetiology was associated with poorer survival. Notably, the provision of bystander CPR and PAD for OHCA in other places was associated with better neurological survival (aOR [95% CI]: 1.61 [1.53–1.70] and 1.63 [1.50–1.77], respectively) but not for OHCA in toilets (aOR [95% CI]: 1.19 [0.91–1.57] and 2.05 [0.65–6.41], respectively) (
Figure 2).
4. Discussion
The current study observed that the incidence of OHCAs in the toilet is higher than in patients with other minor illnesses, with 4.1% of cardiac arrest cases occurring in toilets. In addition, cardiac arrests were more likely to occur in toilets than in other places, considering the amount of time spent in these rooms (approximately 20 min per day [1.4%/day]) [
9]. The likelihood of experiencing cardiac arrest was 7.7 times higher in home toilets than in public toilets.
Family member-witnessed OHCA, but not friend/colleague-witnessed OHCA, had a higher likelihood of favourable neurological survival. Previous studies have demonstrated that OHCA cases witnessed by friends/colleagues have better outcomes than cases witnessed by family members in the context of psychological effects and other factors [
10]. Since toilets are private spaces, friends/colleagues are more likely to hesitate to call out or knock on the door than family members, and this may contribute to the lack of improvement in friend/colleague-witnessed OHCA outcomes. Notably, our study also found that providing bystander CPR and PAD, significant prognostic factors for cardiac arrest patients [
5,
6], were not associated with improved outcomes for OHCA in toilets. One of the causes was that provision rates of both bystander CPR and PAD were very low in toilets. We speculate that toilets are very confined spaces, which limit the space for resuscitation efforts, and that it may be difficult to reposition patients into the supine position, since they are sometimes found seated on a toilet seat. In addition, this particular situation may prolong the time of EMS field activities, resulting in a poor outcome [
11]. Therefore, we consider that resuscitation education methods for OHCA in toilets should incorporate strategies for specific situations in which cardiac arrest occurs in the toilets, including how to rescue patients from the toilets.
Another possible contributing factor could be that although there was no difference in the EMS response time between emergencies in toilets and other places, the time from patient collapse to call (finding) might be longer for OHCAs occurring in toilets. Thus, the crucial time when bystander CPR and PAD are effective immediately after collapse may be missed. Therefore, to improve the outcome of OHCA in toilets, it is essential to recognise a patient in distress as soon as possible. It is necessary to educate the public that (1) if a person with a history of syncope or who is not feeling well uses the toilet, they should inform those around them before using it, and (2) it is vital to make an early emergency call before entering the toilet, especially when realising that someone in poor health is unwell or has a sudden onset of symptoms such as chest pain.
Preventive approaches are also critical when there is no one around. It is essential to install an intelligent home emergency notification system that automatically detects collapses, especially in home toilets, and the emergency dispatcher or security company is automatically notified. It would also be critical to install automated external defibrillators (AEDs) at the entrance to public toilets, in addition to requiring the installation of emergency buzzers. Smartwatches that automatically detect and report falls would also be effective, especially for older adults.
Our study has some limitations. First, this was an observational study, and unmeasured confounding factors or trends may explain outcome differences. Second, the combining/reconciling process of the two databases failed to include 0.17% of case failures, and 0.76% of cases had missing location information. The exclusion of these patients may have affected the outcomes. Nonetheless, this study included a notably large retrospective cohort, and the results will help develop new strategies to manage OHCAs occurring in toilets.
5. Conclusions
Although the neurologically favourable survival rate of OHCA in toilets is poor, the provision of bystander CPR and PAD was not associated with that outcome. Possible causes include low provisioning rates and delayed patient detection. In addition to paying particular attention to unwell patients who use the toilets, preventive approaches, such as early emergency calls and the installation of systems that automatically detect collapses, should be promoted.
Author Contributions
Y.T. and H.I. take responsibility for the paper as a whole. Y.T. and H.I.: Conceptualisation and Validation; Y.T. and H.I.: Data curation; H.I.: Formal analysis; Y.T.: Writing—original draft preparation; Y.T., T.K., H.O. and H.I.: Supervision and Validation; Y.T. and H.I.: Project administration. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
This study was approved by the Ethical Review Committee of Kanazawa Medical University (No. 1729) and was conducted in accordance with the STROBE guidelines.
Informed Consent Statement
Patient consent was waived because of retrospective data collected without personal identifying information.
Data Availability Statement
Restrictions apply to the availability of these data. These data were obtained from the Fire and Disaster Management Agency (FDMA) in Japan.
Acknowledgments
We would like to thank all the EMS personnel and the FDMA in Japan for their cooperation in collecting and managing the patient databases.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kiyohara, K.; Nishiyama, C.; Hayashida, S.; Matsuyama, T.; Hatakeyama, T.; Shimamoto, T.; Izawa, J.; Fujii, T.; Katayama, Y.; Iwami, T.; et al. Characteristics and outcomes of bath-related out-of-hospital cardiac arrest in Japan. Circ. J. 2016, 80, 1564–1570. [Google Scholar] [CrossRef] [PubMed]
- Inamasu, J.; Miyatake, S. Cardiac arrest in the toilet: Clinical characteristics and resuscitation profiles. Environ. Health Prev. Med. 2013, 18, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Kiyohara, K.; Nishiyama, C.; Kiguchi, T.; Kobayashi, D.; Iwami, T.; Kitamura, T. Out-of-hospital cardiac arrests in the toilet in Japan: A population-based descriptive study. Acute Med. Surg. 2018, 5, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Perkins, G.D.; Jacobs, I.G.; Nadkarni, V.M.; Berg, R.A.; Bhanji, F.; Biarent, D.; Bossaert, L.L.; Brett, S.J.; Chamberlain, D.; de Caen, A.R.; et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation 2015, 132, 1286–1300. [Google Scholar] [PubMed]
- Soar, J.; Böttiger, B.W.; Carli, P.; Couper, K.; Deakin, C.D.; Djärv, T.; Lott, C.; Olasveengen, T.; Paal, P.; Pellis, T.; et al. European Resuscitation Council Guidelines 2021: Adult advanced life support. Resuscitation 2021, 161, 115–151. [Google Scholar] [CrossRef] [PubMed]
- Panchal, A.R.; Bartos, J.A.; Cabañas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2020, 142, S366–S468. [Google Scholar] [CrossRef] [PubMed]
- Safar, P. Resuscitation after Brain Ischemia. In Brain Failure and Resuscitation; Grenvik, A., Safar, P., Eds.; Churchill Livingstone: New York, NY, USA, 1981; pp. 155–184. [Google Scholar]
- Myat, A.; Song, K.J.; Rea, T. Out-of-hospital cardiac arrest: Current concepts. Lancet 2018, 391, 970–979. [Google Scholar] [CrossRef] [PubMed]
- Cabinet Secretariat in Japan. Available online: https://www.cas.go.jp/jp/seisaku/kurashinoshitsu/bunkakai1/dai3/index.html#gaiyou (accessed on 10 March 2024).
- Tanaka, Y.; Maeda, T.; Kamikura, T.; Nishi, T.; Omi, W.; Hashimoto, M.; Sakagami, S.; Inaba, H. Potential association of bystander-patient relationship with bystander response and patient survival in daytime out-of-hospital cardiac arrest. Resuscitation 2015, 86, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Coute, R.A.; Nathanson, B.H.; Kurz, M.C.; McNally, B.; Mader, T.J.; CARES Surveillance Group. The association between scene time interval and neurologic outcome following adult bystander witnessed out-of-hospital cardiac arrest. Am. J. Emerg. Med. 2021, 46, 628–633. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).