Near-Infrared Spectroscopy (NIRS) in the Assessment of Cerebral Tissue Oxygenation (rSO2): Methodological Issues and Dilemmas
Abstract
1. Introduction
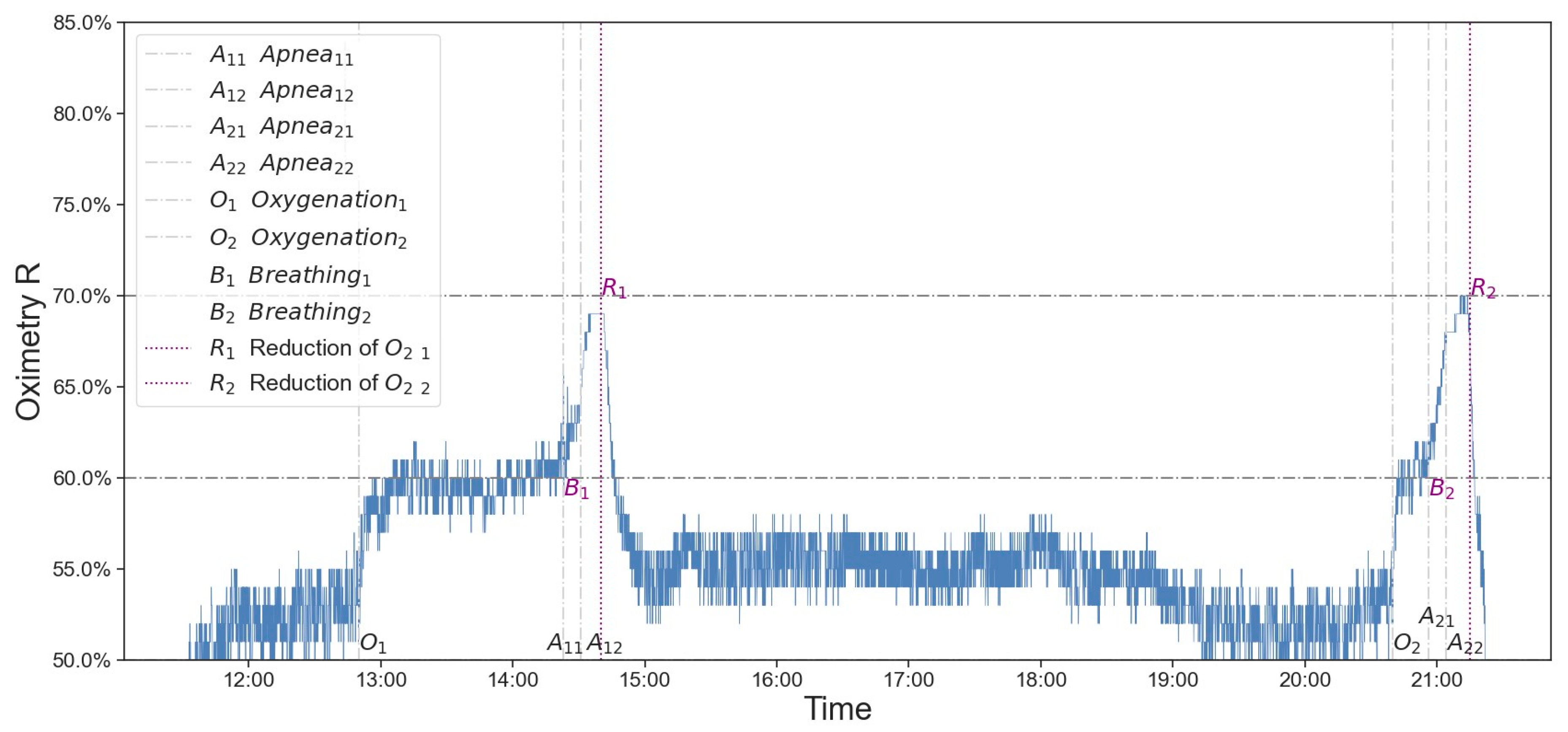
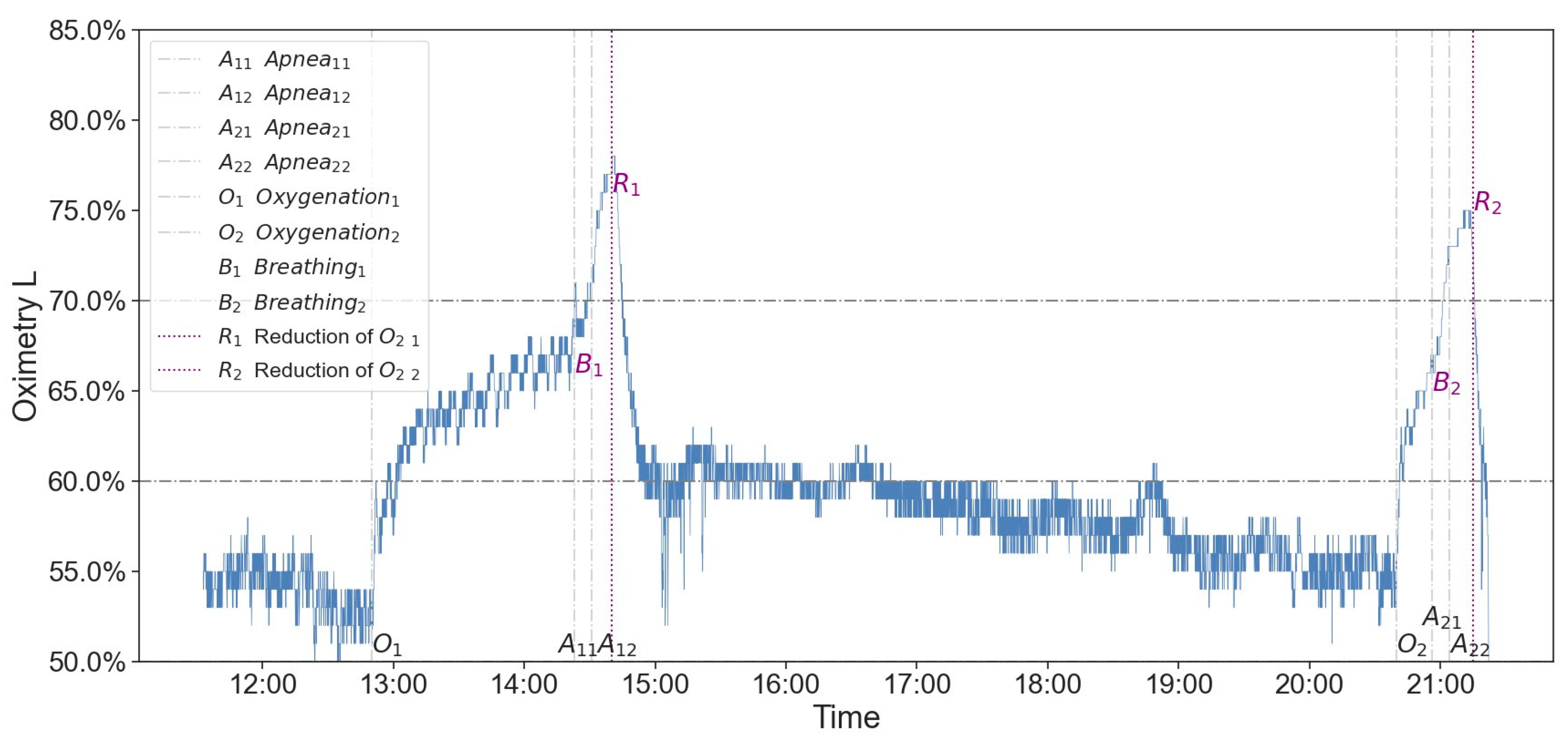
2. Case
3. Discussion
4. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vinciguerra, L.; Bösel, J. Noninvasive Neuromonitoring: Current Utility in Subarachnoid Hemorrhage, Traumatic Brain Injury, and Stroke. Neurocrit. Care 2017, 27, 122–140. [Google Scholar] [CrossRef] [PubMed]
- Roldán, M.; Kyriacou, P.A. Near-infrared spectroscopy (nirs) in traumatic brain injury (tbi). Sensors 2021, 21, 1586. [Google Scholar] [CrossRef] [PubMed]
- Sekhon, M.S.; Griesdale, D.E. Individualised perfusion targets for hypoxic ischaemic brain injury after cardiac arrest. Crit. Care 2017, 21, 259. [Google Scholar] [CrossRef] [PubMed]
- Barud, M.; Dabrowski, W.; Siwicka-Gieroba, D.; Robba, C.; Bielacz, M.; Badenes, R. Usefulness of Cerebral Oximetry in TBI by NIRS. J. Clin. Med. 2021, 10, 2938. [Google Scholar] [CrossRef] [PubMed]
- Thiele, R.H.; Shaw, A.D.; Bartels, K.; Brown, C.H., IV; Grocott, H.; Heringlake, M.; Gan, T.J.; Miller, T.E.; McEvoy, M.D.; Perioperative Quality Initiative (POQI) 6 Workgroup. American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on the Role of Neuromonitoring in Perioperative Outcomes: Cerebral Near-Infrared Spectroscopy. Anesth. Analg. 2020, 131, 1444–1455. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Yoshitani, K.; Kubota, Y.; Inatomi, Y.; Ohnishi, Y. Effect of posture and extracranial contamination on results of cerebral oximetry by near-infrared spectroscopy. J. Anesth. 2017, 31, 103. [Google Scholar] [CrossRef] [PubMed]
- Tatli, O.; Bekar, O.; Imamoglu, M.; Gonenc Cekic, O.; Aygun, A.; Eryigit, U.; Karaca, Y.; Sahin, A.; Turkmen, S.; Turedi, S. Cerebral Oximetry as an Auxiliary Diagnostic Tool in the Diagnosis of Brain Death. Transplant. Proc. 2017, 49, 1702–1707. [Google Scholar] [CrossRef]
- Kyttä, J.; Ohman, J.; Tanskanen, P.; Randell, T. Extracranial contribution to cerebral oximetry in brain dead patients: A report of six cases. J. Neurosurg. Anesthesiol. 1999, 11, 252–254. [Google Scholar] [CrossRef]
- Eleveld, N.; Esquivel-Franco, D.C.; Drost, G.; Absalom, A.R.; Zeebregts, C.J.; de Vries, J.P.M.; Elting, J.W.J.; Maurits, N.M. The Influence of Extracerebral Tissue on Continuous Wave Near-Infrared Spectroscopy in Adults: A Systematic Review of In Vivo Studies. J. Clin. Med. 2023, 12, 2776. [Google Scholar] [CrossRef]
- Moerman, A.T.; Vandenheuvel, M.; Tuybens, P.J.; Van Gompel, C.; De Hert, S.G. Incongruous effect of phenylephrine on changes in cerebral blood volume measured by near-infrared spectroscopy (NIRS) indicating extracranial contamination. J. Clin. Monit. Comput. 2022, 36, 745–750. [Google Scholar] [CrossRef]
- Canova, D.; Roatta, S.; Bosone, D.; Micieli, G. Inconsistent detection of changes in cerebral blood volume by near infrared spectroscopyin standard clinical tests. J. Appl. Physiol. 2011, 110, 1646–1655. [Google Scholar] [CrossRef] [PubMed]
- Davie, S.N.; Grocott, H.P. Impact of extracranial contamination on regional cerebral oxygen saturation: A comparison of three cerebral oximetry technologies. Anesthesiology 2012, 116, 834–840. [Google Scholar] [CrossRef]
- Spears, W.; Mian, A.; Greer, D. Brain death: A clinical overview. J. Intensive Care 2022, 10, 16. [Google Scholar] [CrossRef] [PubMed]
- Greer, D.M.; Shemie, S.D.; Lewis, A.; Torrance, S.; Varelas, P.; Goldenberg, F.D.; Bernat, J.L.; Souter, M.; Topcuoglu, M.A.; Alexandrov, A.W.; et al. Determination of Brain Death/Death by Neurologic Criteria: The World Brain Death Project. JAMA 2020, 324, 1078–1097. [Google Scholar] [CrossRef] [PubMed]
- Lewis, A.; Kirschen, M.P.; Greer, D. The 2023 AAN/AAP/CNS/SCCM Pediatric and Adult Brain Death/Death by Neurologic Criteria Consensus Practice Guideline: A Comparison With the 2010 and 2011 Guidelines. Neurol. Clin. Pract. 2023, 13, e200189. [Google Scholar] [CrossRef]
- Gisolf, J.; van Lieshout, J.J.; van Heusden, K.; Pott, F.; Stok, W.J.; Karemaker, J.M. Human cerebral venous outflow pathway depends on posture and central venous pressure. J. Physiol. 2004, 560, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Lanning, K.M.; Ylikauma, L.A.; Erkinaro, T.M.; Ohtonen, P.P.; Vakkala, M.A.; Kaakinen, T.I. Changes in transcranial near-infrared spectroscopy values reflect changes in cardiac index during cardiac surgery. Acta Anaesthesiol. Scand. 2023, 67, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Schraag, S. Combined Monitoring—Brain Function Monitoring and Cerebral Oximetry. J. Cardiothorac. Vasc. Anesth. 2019, 33, S53–S57. [Google Scholar] [CrossRef] [PubMed]
- Robba, C.; Cardim, D.; Ball, L.; Battaglini, D.; Dabrowski, W.; Bassetti, M.; Giacobbe, D.R.; Czosnyka, M.; Badenes, R.; Pelosi, P.; et al. The Use of Different Components of Brain Oxygenation for the Assessment of Cerebral Haemodynamics: A Prospective Observational Study on COVID-19 Patients. Front. Neurol. 2021, 12, 735469. [Google Scholar] [CrossRef]
- Rivera-Lara, L.; Geocadin, R.; Zorrilla-Vaca, A.B.; Healy, R.J.B.; Radzik, B.R.C.; Palmisano, C.C.; Mirski, M.; White, M.A.; Suarez, J.; Brown, C.; et al. Optimizing Mean Arterial Pressure in Acutely Comatose Patients Using Cerebral Autoregulation Multimodal Monitoring with Near-Infrared Spectroscopy. Crit. Care Med. 2019, 47, 1409–1415. [Google Scholar] [CrossRef]
- Takegawa, R.; Hayashida, K.; Rolston, D.M.; Li, T.; Miyara, S.J.; Ohnishi, M.; Shiozaki, T.; Becker, L.B. Near-Infrared Spectroscopy Assessments of Regional Cerebral Oxygen Saturation for the Prediction of Clinical Outcomes in Patients with Cardiac Arrest: A Review of Clinical Impact, Evolution, and Future Directions. Front. Med. 2020, 7, 587930. [Google Scholar] [CrossRef]
- Hansen, M.L.; Hyttel-Sørensen, S.; Jakobsen, J.C.; Gluud, C.; Kooi, E.M.W.; Mintzer, J.; de Boode, W.P.; Fumagalli, M.; Alarcon, A.; Alderliesten, T. Cerebral near-infrared spectroscopy monitoring (NIRS) in children and adults: A systematic review with meta-analysis. Pediatr. Res. 2022; ahead of print. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lukaszewski, M.; Nelke, K. Near-Infrared Spectroscopy (NIRS) in the Assessment of Cerebral Tissue Oxygenation (rSO2): Methodological Issues and Dilemmas. Anesth. Res. 2024, 1, 24-33. https://doi.org/10.3390/anesthres1010004
Lukaszewski M, Nelke K. Near-Infrared Spectroscopy (NIRS) in the Assessment of Cerebral Tissue Oxygenation (rSO2): Methodological Issues and Dilemmas. Anesthesia Research. 2024; 1(1):24-33. https://doi.org/10.3390/anesthres1010004
Chicago/Turabian StyleLukaszewski, Marceli, and Kamil Nelke. 2024. "Near-Infrared Spectroscopy (NIRS) in the Assessment of Cerebral Tissue Oxygenation (rSO2): Methodological Issues and Dilemmas" Anesthesia Research 1, no. 1: 24-33. https://doi.org/10.3390/anesthres1010004
APA StyleLukaszewski, M., & Nelke, K. (2024). Near-Infrared Spectroscopy (NIRS) in the Assessment of Cerebral Tissue Oxygenation (rSO2): Methodological Issues and Dilemmas. Anesthesia Research, 1(1), 24-33. https://doi.org/10.3390/anesthres1010004






