A Review of Smart Healthcare: Concept, Drivers, Characteristics, and Challenges
Abstract
1. Introduction
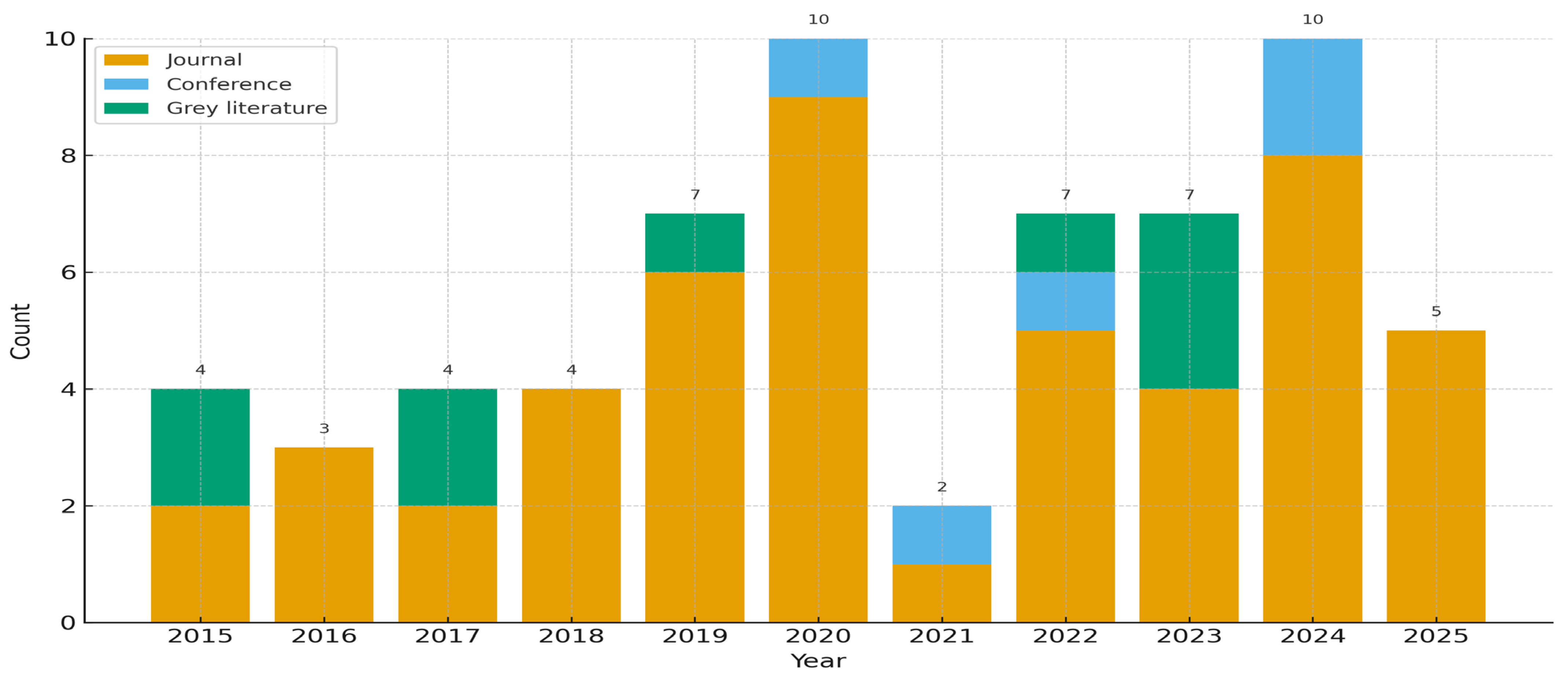
2. Materials and Methods
- What is the concept of SHC?
- What are the main drivers and characteristics of SHC?
- What challenges are associated with its implementation?
3. Results
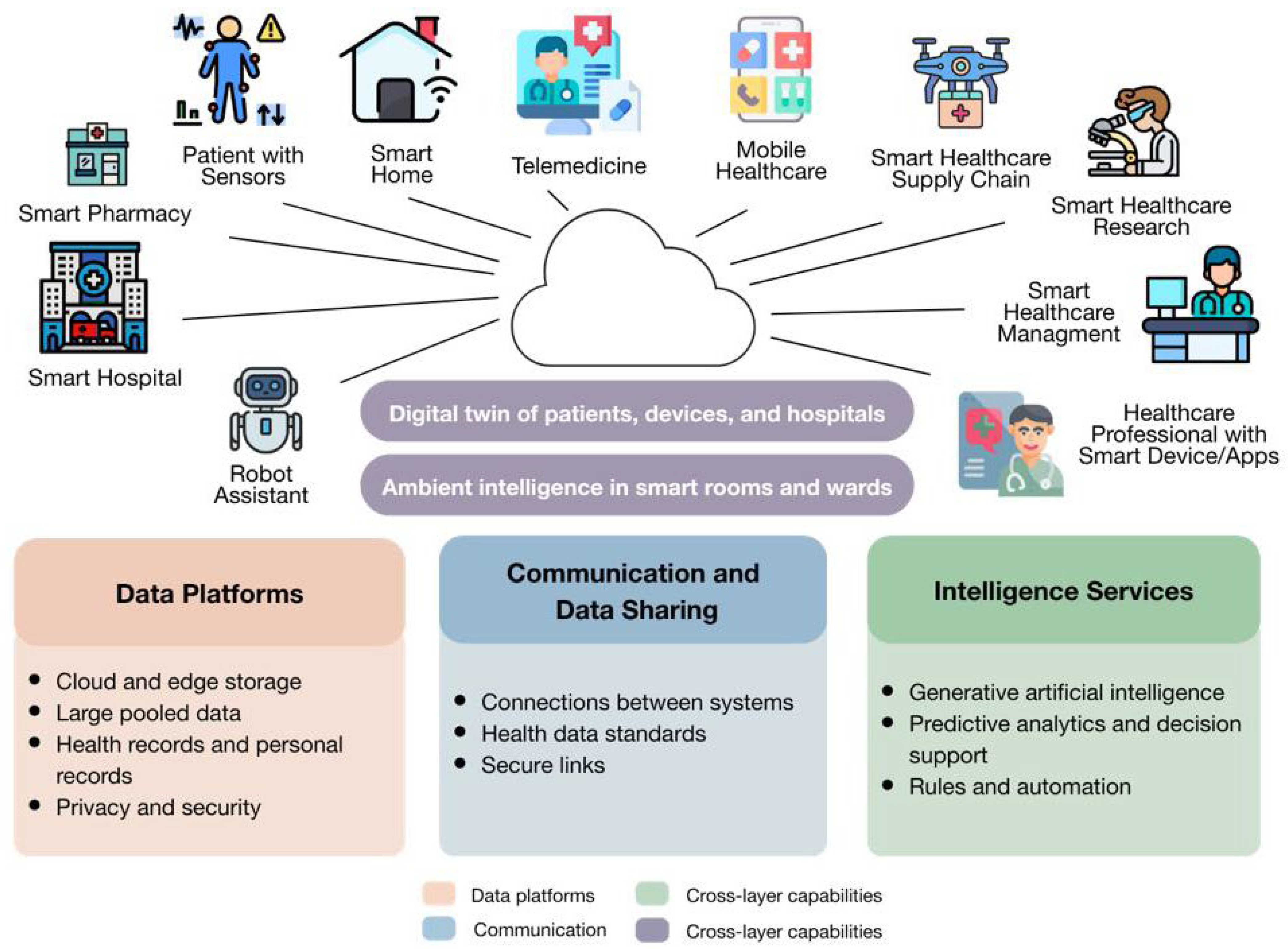
3.1. SHC Conceptualization
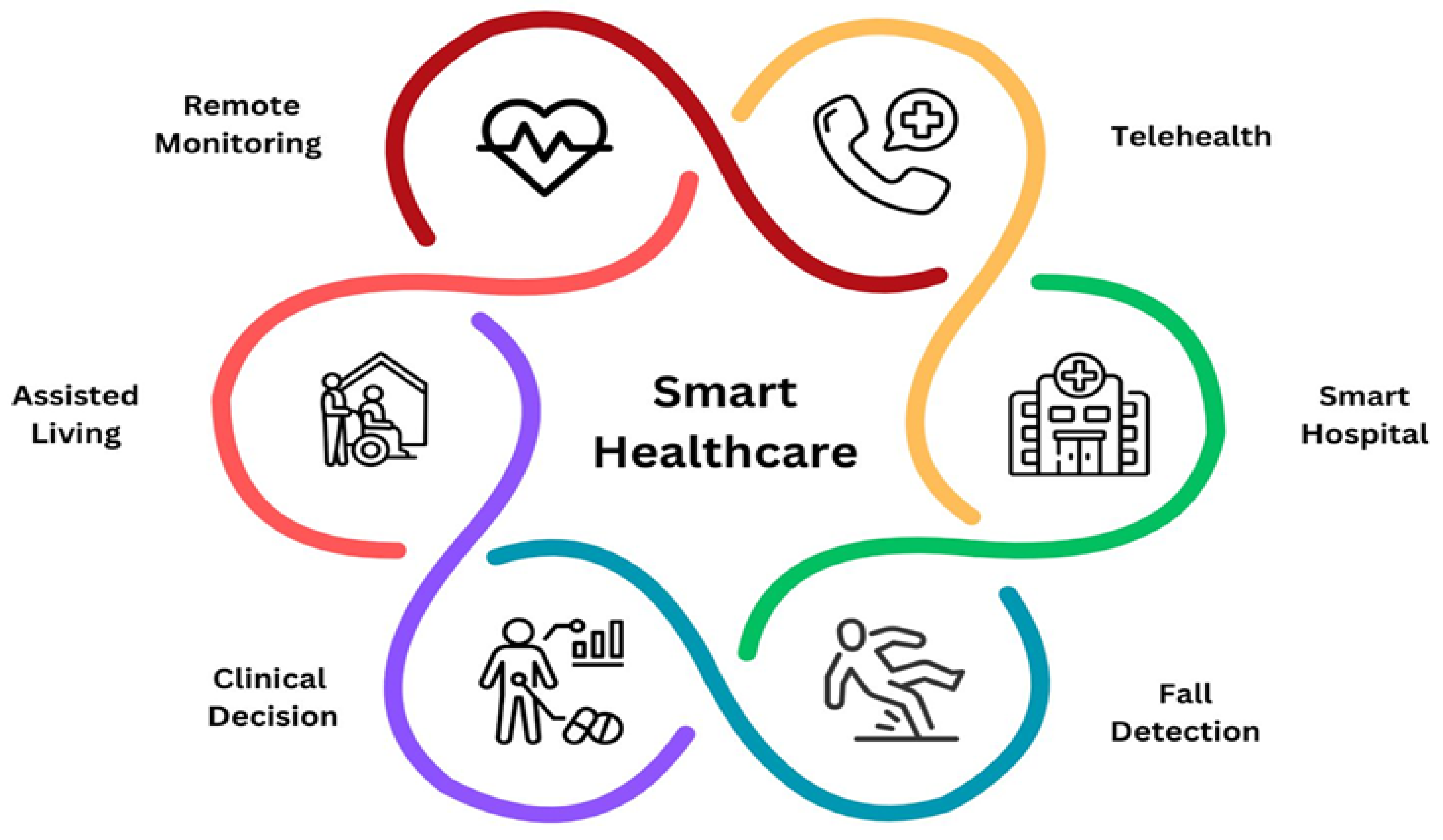
3.2. SHC Characteristics
3.2.1. Overview
3.2.2. Bridging Drivers and Characteristics
3.2.3. Mini Cases: From Generic Challenges to Actionable Lessons
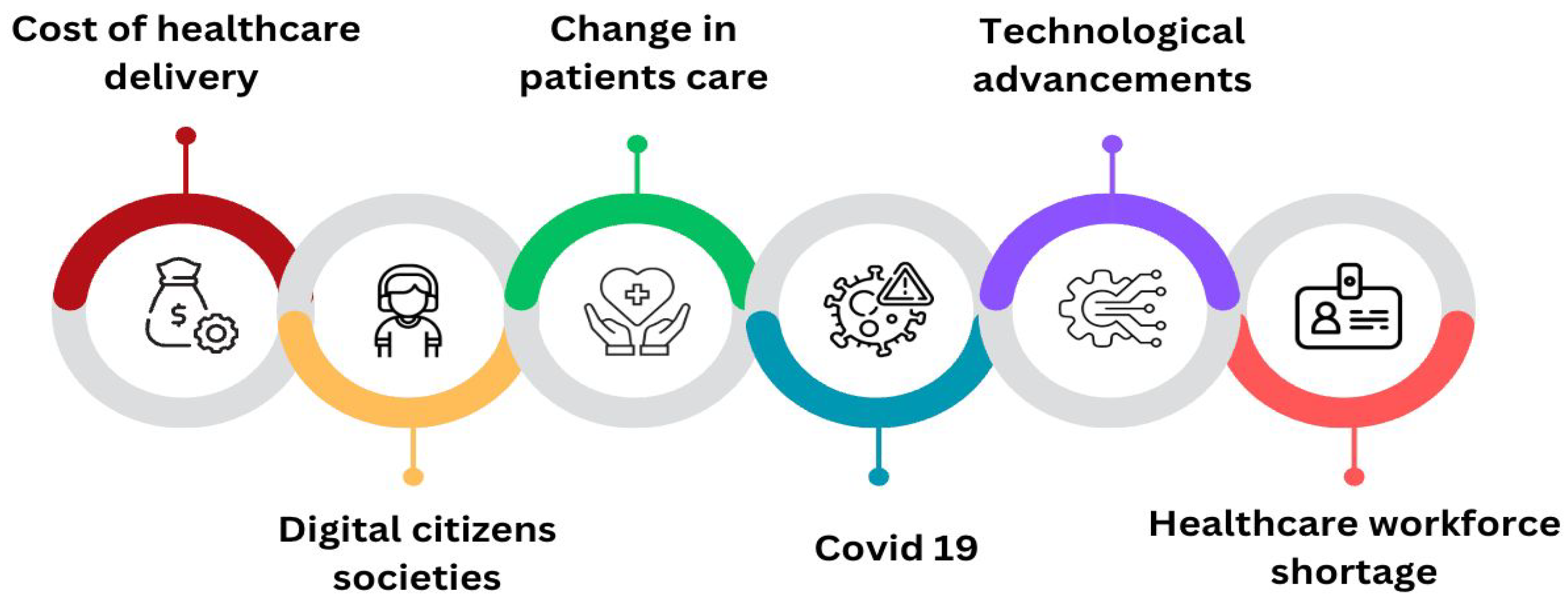
3.3. SHC Drivers
3.3.1. Technological Advancements
3.3.2. Digital Citizen Societies
3.3.3. Shifting Models of Patient Care
3.3.4. Healthcare Workforce Shortages
3.3.5. Rising Costs of Healthcare Delivery
3.3.6. Impact of COVID-19
3.4. SHC Deployment Challenges
3.4.1. Reduced Human Interaction and Patient Monitoring
3.4.2. Data Accuracy and Reliability
3.4.3. Data Security and Privacy
3.4.4. Interoperability and System Performance
3.4.5. Ethical Concerns and Trust in AI
3.4.6. High Financial Costs
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| AMI | Ambient Intelligence |
| CDSS | Clinical Decision Support System |
| EHealth | Electronic health |
| HCPs | Healthcare professionals |
| ICTs | Information and communication technologies |
| IoMT | Internet of Medical Things |
| IoT | Internet of Things |
| MHealth | Mobile health |
| RFID | Radio Frequency Identification |
| SHC | Smart healthcare |
References
- Gopal, G.; Suter-Crazzolara, C.; Toldo, L.; Eberhardt, W. Digital transformation in healthcare–architectures of present and future information technologies. Clin. Chem. Lab. Med. 2019, 57, 328–335. [Google Scholar] [CrossRef]
- Thacharodi, A.; Singh, P.; Meenatchi, R.; Tawfeeq Ahmed, Z.H.; Kumar, R.R.; V, N.; Kavish, S.; Maqbool, M.; Hassan, S. Revolutionizing healthcare and medicine: The impact of modern technologies for a healthier future—A comprehensive review. Health Care Sci. 2024, 3, 329–349. [Google Scholar] [CrossRef]
- Ahmad, K.A.B.; Khujamatov, H.; Akhmedov, N.; Bajuri, M.Y.; Ahmad, M.N.; Ahmadian, A. Emerging trends and evolutions for smart city healthcare systems. Sustain. Cities Soc. 2022, 80, 103695. [Google Scholar] [CrossRef]
- Yin, H.; Akmandor, A.O.; Mosenia, A.; Jha, N.K. Smart healthcare. Found. Trends Electron. Des. Autom. 2018, 12, 401–466. [Google Scholar] [CrossRef]
- Du-Harpur, X.; Watt, F.M.; Luscombe, N.M.; Lynch, M.D. What is AI? Applications of artificial intelligence to dermatology. Brit. J. Dermatol. 2020, 183, 423–430. [Google Scholar] [CrossRef]
- Wan, J.; Al-awlaqi, M.A.A.H.; Li, M.; O’Grady, M.; Gu, X.; Wang, J.; Cao, N. Wearable IoT enabled real-time health monitoring system. J. Wirel. Commun. Netw. 2018, 298. [Google Scholar] [CrossRef]
- Guo, C.; Chen, J. Big data analytics in healthcare. In Knowledge Technology and Systems: Toward Establishing Knowledge Systems Science; Nakamori, Y., Ed.; Springer: Cham, Switzerland, 2023; pp. 27–70. ISBN 978-981-99-1075-5. [Google Scholar] [CrossRef]
- Faridi, F.; Sarwar, H.; Ahtisham, M.; Jamal, K. Cloud computing approaches in health care. Mater. Today Proc. 2022, 51, 1217–1223. [Google Scholar] [CrossRef]
- Sood, S.; Mbarika, V.; Jugoo, S.; Dookhy, R.; Doarn, C.R.; Prakash, N.; Merrell, R.C. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed. e-Health 2007, 13, 573–590. [Google Scholar] [CrossRef] [PubMed]
- Dias, D.; Paulo Silva Cunha, J. Wearable health devices—Vital sign monitoring, systems and technologies. Sensors 2018, 18, 2414. [Google Scholar] [CrossRef] [PubMed]
- Pagliari, C.; Sloan, D.; Gregor, P.; Sullivan, F.; Detmer, D.; Kahan, J.P.; Oortwijn, W.; MacGillivray, S. What is eHealth (4): A scoping exercise to map the field. J. Med. Internet Res. 2005, 7, e391. [Google Scholar] [CrossRef] [PubMed]
- Cortez, N. The mobile health revolution. UCDL Rev. 2013, 47, 1173. [Google Scholar]
- Beeler, P.E.; Bates, D.W.; Hug, B.L. Clinical decision support systems. Swiss Med. Wkly. 2014, 144, w14073. [Google Scholar] [CrossRef] [PubMed]
- Mechanic, O.J.; Persaud, Y.; Kimball, A.B. TeleHealth Systems; StatPearls Publishing: Treasure Island, FL, USA, 2017. Available online: https://www.ncbi.nlm.nih.gov/books/NBK459384/ (accessed on 3 February 2025).
- Koçak, B.; Durmaz, E.Ş.; Ateş, E.; Kılıçkesmez, Ö. Radiomics with artificial intelligence: A practical guide for beginners. Diagn. Interv. Radiol. 2019, 25, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Krukowski, A.; Barca, C.C.; Rodríguez, J.M.; Vogiatzaki, E. Personal health record. In Cyberphysical Systems for Epilepsy and Related Brain Disorders: Multi-Parametric Monitoring and Analysis for Diagnosis and Optimal Disease Management; Voros, N., Antonopoulos, C., Eds.; Springer: Cham, Switzerland, 2015; pp. 205–238. ISBN 978-3-319-20049-1. [Google Scholar] [CrossRef]
- Kamel, M.; George, L. Remote patient tracking and monitoring system. Int. J. Comput. Sci. Mob. Comput. 2013, 2, 88–94. [Google Scholar]
- Jarrahi, M.H.; Eshraghi, A. Digital natives vs digital immigrants: A multidimensional view on interaction with social technologies in organizations. J. Enterp. Inf. Manag. 2019, 32, 1051–1070. [Google Scholar] [CrossRef]
- Chua, J.A. Cybersecurity in the healthcare industry. Physician Leadersh. J. 2021, 8, 69–72. Available online: https://www.physicianleaders.org/articles/cybersecurity-healthcare-industry-collaborative-approach (accessed on 3 February 2025).
- Kuziemsky, C.E.; Peyton, L. A framework for understanding process interoperability and health information technology. Health Policy Technol. 2016, 5, 196–203. [Google Scholar] [CrossRef]
- Ajami, S.; Rajabzadeh, A. Radio frequency identification (RFID) technology and patient safety. J. Res. Med. Sci. 2013, 18, 809–813. [Google Scholar]
- Cook, D.J.; Augusto, J.C.; Jakkula, V.R. Review: Ambient intelligence: Technologies, applications, and opportunities. Pervasive Mob. Comput. 2009, 5, 277–298. [Google Scholar] [CrossRef]
- Vishnu, S.; Ramson, S.J.; Jegan, R. Internet of medical things (IoMT)—An overview. In Proceedings of the 2020 5th International. Conference on Devices, Circuits and Systems (ICDCS), Coimbatore, India, 5–6 March 2020; IEEE: New York, NY, USA, 2020; pp. 101–104. [Google Scholar] [CrossRef]
- Zhao, W.; Luo, X.; Qiu, T. Smart healthcare. Appl. Sci. 2017, 7, 1176. [Google Scholar] [CrossRef]
- Dukhanin, V.; Topazian, R.; DeCamp, M. Metrics and evaluation tools for patient engagement in healthcare organization and system-level decision-making: A systematic review. Int. J. Health Policy. Manag. 2018, 7, 889. [Google Scholar] [CrossRef]
- Holzinger, A.; Röcker, C.; Ziefle, M. From smart health to smart hospitals. In Smart Health: Open Problems and Future Challenges; Holzinger, A., Röcker, C., Ziefle, M., Eds.; Springer: Cham, Switzerland, 2015; pp. 1–20. ISBN 978-3-319-16226-3. [Google Scholar] [CrossRef]
- Quaranta-Finsiel, A.A. “Smart hospitals” in the environment and in the territory. J. Clin. Comput. 1988, 17, 23–27. [Google Scholar]
- Kaldoudi, E. Smart hospital: The future of healthcare. Comput. Struct. Biotechnol. J. 2024, 24, 87–88. [Google Scholar] [CrossRef] [PubMed]
- Tian, S.; Yang, W.; Le Grange, J.M.; Wang, P.; Huang, W.; Ye, Z. Smart healthcare: Making medical care more intelligent. Glob. Health J. 2019, 3, 62–65. [Google Scholar] [CrossRef]
- Dhar, J.; Ranganathan, A. Machine learning capabilities in medical diagnosis applications: Computational results for hepatitis disease. Int. J. Biomed. Eng. Technol. 2015, 17, 330–340. [Google Scholar] [CrossRef]
- Sulaiman, H.; Wickramasinghe, N. Assimilating healthcare information systems in a Malaysian hospital. Commun. Assoc. Inf. Syst. 2014, 34, 77. [Google Scholar] [CrossRef]
- Zaw, T.O.K.; Muthaiyah, S.; Jasbi, A. Contextualization of smart healthcare: A systematic review. In Proceedings of the 2021 7th International Conference on Research and Innovation in Information Systems (ICRIIS), Johor Bahru, Malaysia, 25–26 October 2021; IEEE: New York, NY, USA, 2021; pp. 1–6. [Google Scholar] [CrossRef]
- Vidyasekar, A.D. Strategic Opportunity Analysis of the Global Smart City Market: Smart City Market Is Likely to Be Worth A Cumulative 1.565 Trillion by 2020. 2013. Available online: http://www.digitaljournal.com/pr/1601758 (accessed on 3 February 2025).
- Sundaravadivel, P.; Kougianos, E.; Mohanty, S.P.; Ganapathiraju, M.K. Everything you wanted to know about smart health care: Evaluating the different technologies and components of the internet of things for better health. IEEE Consum. Electron. Mag. 2017, 7, 18–28. [Google Scholar] [CrossRef]
- Zeadally, S.; Siddiqui, F.; Baig, Z.; Ibrahim, A. Smart healthcare: Challenges and potential solutions using internet of things (IoT) and big data analytics. PSU Res. Rev. 2020, 4, 149–168. [Google Scholar] [CrossRef]
- Harwood, T.G.; Garry, T. An overview of content analysis. Mark. Rev. 2003, 3, 479–498. [Google Scholar] [CrossRef]
- Sligo, J.; Gauld, R.; Roberts, V.; Villa, L. A literature review for large-scale health information system project planning, implementation and evaluation. Int. J. Med. Inf. 2017, 97, 86–97. [Google Scholar] [CrossRef]
- Sarkar, M.; Lee, T.H.; Sahoo, P.K. Smart healthcare: Exploring the internet of medical things with ambient intelligence. Electronics 2024, 13, 2309. [Google Scholar] [CrossRef]
- Kwon, H.; An, S.; Lee, H.-Y.; Cha, W.C.; Kim, S.; Cho, M.; Kong, H.-J. Review of smart hospital services in real healthcare environments. Healthc. Inform. Res. 2022, 28, 3–15. [Google Scholar] [CrossRef]
- Kathirvel, S.; Chakraborty, S. Rural Community Health Workers’ Readiness for Mobile-Phone-Based Telemedicine Uptake in India. J. Rural Med. 2022, 17, 166–170. [Google Scholar]
- Tan, H.Y.; Tan, J.K.; Lam, L.T.; Tan, D.H.; Chua, Y.X. Insights into Singapore’s national strategy for primary care reform: Physician attitudes, facilitators and barriers to healthier SG. BMC Health Serv. Res. 2025, 25, 1021. [Google Scholar] [CrossRef]
- Woon, B. [Singapore] Health Database in an IT society. Jpn. Med. Assoc. J. 2014, 57, 212–215. [Google Scholar]
- Yang, Y.; Venkatachalam, I.; Low, C.T.; Foo, M.Z.Q.; Aung, M.K.; See, S.W.J.; Aung, M.O.; Chan, D.Y.W.; Arora, S.; Sim, J.X.Y.; et al. Transforming healthcare system: Outcomes of Healthier-SG from a large tertiary-care hospital in Singapore. Health Policy Technol. 2025, 14, 100968. [Google Scholar] [CrossRef]
- Man, R.E.K.; Ho, A.X.Y.; Lee, E.P.X.; Fenwick, E.K.D.; Aravindhan, A.; Ho, K.C.; Tan, G.S.W.; Ting, D.S.W.; Wong, T.Y.; Yeo, K.K.; et al. Awareness and attitudes of elderly Southeast Asian adults towards telehealth during the COVID-19 pandemic: A qualitative study. Singap. Med. J. 2025, 66, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Dastidar, B.G.; Jani, A.R.; Suri, S.; Nagaraja, V.H. Reimagining India’s National Telemedicine Service to improve access to care. Lancet Reg. Health Southeast Asia 2024, 30, 100480. [Google Scholar] [CrossRef] [PubMed]
- Verma, N.; Buch, B.; Taralekar, R.; Acharya, S. Diagnostic concordance of telemedicine as compared with face-to-face care in primary health care clinics in rural India: Randomized crossover trial. JMIR Form. Res. 2023, 7, e42775. [Google Scholar] [CrossRef]
- Joshi, K.; Modi, B.; Katoch, C.D.S. Utilization of telemedicine services of institute of national importance in the western region of India: A mixed-method study. J. Fam. Med. Prim. Care 2024, 13, 3782–3787. [Google Scholar] [CrossRef]
- Nagaraja, V.H.; Dastidar, B.G.; Suri, S.; Jani, A.R. Perspectives and use of telemedicine by doctors in India: A cross-sectional study. Health Policy Technol. 2024, 13, 100845. [Google Scholar] [CrossRef]
- Narwadiya, S.C.; Rao, D.R. Telemedicine in India: An impact analysis. Intell. Hosp. 2025, 1, 100004. [Google Scholar] [CrossRef]
- NHS. About the NHS App. 2023. Available online: https://www.nhs.uk/nhs-app/about-the-nhs-app/ (accessed on 3 February 2025).
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J.; et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 2020, 27, 957–962. [Google Scholar] [CrossRef]
- Kumar, S.; Merchant, S.; Reynolds, R. Tele-ICU: Efficacy and cost-effectiveness approach of remotely managing the critical care. Open Med. Inform. J. 2013, 7, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, B.A.; Dorman, T.; Breslow, M.J.; Pronovost, P.; Jenckes, M.; Zhang, N.; Anderson, G.; Rubin, H. Intensive care unit telemedicine: Alternate paradigm for providing continuous intensivist care. Crit. Care Med. 2000, 28, 3925–3931. [Google Scholar] [CrossRef]
- Almarri, A.; Hunaiti, Z.; Daoud, M.S.; Manivannan, N. Shaping the future of healthcare: The key characteristics and drivers of smart hospitals. In Proceedings of the 2024 Global Digital Health Knowledge Exchange & Empowerment Conference (gDigiHealthKEE), Abu Dhabi, United Arab Emirates, 24–26 September 2024; IEEE: New York, NY, USA, 2024; pp. 1–7. [Google Scholar] [CrossRef]
- Cheng, T.O. How Laënnec invented the stethoscope. Int. J. Cardiol. 2007, 118, 281–285. [Google Scholar] [CrossRef] [PubMed]
- Avram, R.; Olgin, J.E.; Kuhar, P.; Hughes, J.W.; Marcus, G.M.; Pletcher, M.J.; Aschbacher, K.; Tison, G.H. A digital biomarker of diabetes from smartphone-based vascular signals. Nat. Med. 2020, 26, 1576–1582. [Google Scholar] [CrossRef] [PubMed]
- Lamberti, M.J.; Wilkinson, M.; Donzanti, B.A.; Wohlhieter, G.E.; Parikh, S.; Wilkins, R.G.; Getz, K. A study on the application and use of artificial intelligence to support drug development. Clin. Ther. 2019, 41, 1414–1426. [Google Scholar] [CrossRef]
- Barisoni, L.; Lafata, K.J.; Hewitt, S.M.; Madabhushi, A.; Balis, U.G. Digital pathology and computational image analysis in nephropathology. Nat. Rev. Nephrol. 2020, 16, 669–685. [Google Scholar] [CrossRef]
- Foo, C.; Woon, T.H.; Chia, H.X.; Yap, J.C.H.; Lee, W.S.; Lee, C.E.; Valderas, J.M.; Tan, C.; Teo, K.W. Healthier SG: A gateway for evolving public-private-population partnerships in population health. Lancet Reg. Health West. Pac. 2025, 60, 101606. [Google Scholar] [CrossRef]
- Wang, S.-K.; Hsu, H.-Y.; Campbell, T.; Coster, D.C.; Longhurst, M. An investigation of middle school science teachers and students use of technology inside and outside of classrooms: Considering whether digital natives are more technology savvy than their teachers. Educ. Technol. Res. Dev. 2014, 62, 637–662. [Google Scholar] [CrossRef]
- Lu, J.; Hao, Q.; Jing, M. Consuming, sharing, and creating content: How young students use new social media in and outside school. Comput. Hum. Behav. Rep. 2016, 64, 55–64. [Google Scholar] [CrossRef]
- Chan, M.; Campo, E.; Estève, D.; Fourniols, J.Y. Smart homes—Current features and future perspectives. Maturitas 2009, 64, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Tamura, T.; Ogawa, M.; Yoda, M.; Togawa, T. Fully automated health monitoring system in the home. Med. Eng. Phys. 1998, 20, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Vrančić, A.; Zadravec, H.; Orehovački, T. The role of smart homes in providing care for older adults: A systematic literature review from 2010 to 2023. Smart Cities 2024, 7, 1502–1550. [Google Scholar] [CrossRef]
- Patil, S.; Shankar, H. Transforming healthcare: Harnessing the power of AI in the modern era. Int. J. Multidiscip. Sci. Arts 2023, 2, 60–70. [Google Scholar] [CrossRef]
- Jakobs, R. How Tech Can Tackle Healthcare Workloads and Staff Shortages. Available online: https://www.weforum.org/agenda/2023/01/healthcare-workloads-and-staff-shortages-davos23/ (accessed on 3 February 2025).
- Drouin, J.P.; Hediger, V.; Henke, N. Health Care Costs: A Market-Based View. Available online: https://www.mckinsey.com/~/media/mckinsey/dotcom/client_service/healthcare%20systems%20and%20services/pdfs/healthcare-costs-a-market-based-view.pdf (accessed on 3 February 2025).
- Sakr, S.; Elgammal, A. Towards a comprehensive data analytics framework for smart healthcare services. Big Data Res. 2016, 4, 44–58. [Google Scholar] [CrossRef]
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital transformation in healthcare: Technology acceptance and its applications. Int. J. Environ. Res. Public Health 2023, 20, 3407. [Google Scholar] [CrossRef]
- Richardson, E.; Aissat, D.; Williams, G.A.; Fahy, N. Keeping what works: Remote consultations during the COVID-19 pandemic. Eurohealth 2020, 26, 73–76. [Google Scholar]
- Pronk, N.P.; McEvoy, C. Equitable well-being, social trust, and the economy: An integrated health system’s perspectives on the long-term implications of COVID-19. Prog. Cardiovasc. Dis. 2023, 76, 57–60. [Google Scholar] [CrossRef]
- Donaghy, E.; Atherton, H.; Hammersley, V.; McNeilly, H.; Bikker, A.; Robbins, L.; Campbell, J.; McKinstry, B. Acceptability, benefits, and challenges of video consulting: A qualitative study in primary care. Br. J. Gen. Pract. 2019, 69, e586–e594. [Google Scholar] [CrossRef]
- NHS Digital. Appointments in General Practice Data. 2022. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/mi-appointments-in-general-practice/current (accessed on 3 February 2025).
- Nwobodo-Anyadiegwu, E.N.; Ditend, M.N.; Lumbwe, A.K. The benefits and challenges of implementing smart hospital projects: A systematic review. In Proceedings of the 2022 IEEE 28th International Conference on Engineering, Technology and Innovation (ICE/ITMC) & 31st International Association for Management of Technology (IAMOT) Joint Conference, Nancy, France, 19–23 June 2022; pp. 1–7. [Google Scholar] [CrossRef]
- Uslu, B.Ç.; Okay, E.; Dursun, E. Analysis of factors affecting IoT-based smart hospital design. J. Cloud Comput. 2020, 9, 67. [Google Scholar] [CrossRef]
- Sebastian, M.P. Smart Hospitals: Challenges and Opportunities. Available online: https://forms.iimk.ac.in/websiteadmin/FacultyPublications/Working%20Papers/3052smartHospitals_MPS2019.pdf (accessed on 3 February 2025).
- Ameri, A.; Salmanizadeh, F.; Keshvardoost, S.; Bahaadinbeigy, K. Investigating pharmacists’ views on telepharmacy: Prioritizing key relationships, barriers, and benefits. J. Pharm. Technol. 2020, 36, 171–178. [Google Scholar] [CrossRef]
- Rizk, D.K.A.A.; Hosny, H.M.; ElHorbety, S.; Salem, A.B. SMART hospital management systems based on internet of things: Challenges, intelligent solutions and functional requirements. Int. J. Intell. Comput. Inf. Sci. 2022, 22, 32–43. [Google Scholar] [CrossRef]
- de Paiva Marques Carvalho, T.; de Paiva, J.C.; de Medeiros Valentim, R.A.; Silva, C.B.P.; de Lima, D.F.; Silva, E.C. Sabiá: An authentication, authorization, and user data delivery architecture based on user consent for health information systems in Brazil. Res. Biomed. Eng. 2020, 36, 197–202. [Google Scholar] [CrossRef]
- Dawson, J.; Fisher, E.; Wiese, J. Hospital employee experiences caring for patients in smart patient rooms. In Proceedings of the 2024 CHI Conference on Human Factors in Computing Systems (CHI’24), Honolulu, HI, USA, 11–16 May 2024; ACM: New York, NY, USA, 2024; pp. 1–16. [Google Scholar] [CrossRef]
- Renukappa, S.; Mudiyi, P.; Suresh, S.; Abdalla, W.; Subbarao, C. Evaluation of challenges for adoption of smart healthcare strategies. Smart Health 2022, 26, 100330. [Google Scholar] [CrossRef]
- Kruse, C.S.; Mileski, M.; Alaytsev, V.; Carol, E.; Williams, A. Adoption factors associated with electronic health record among long-term care facilities: A systematic review. BMJ Open 2015, 5, e006615. [Google Scholar] [CrossRef]
- Seckman, C.; Bauer, A.; Moser, T.; Paaske, S. The Benefits and Barriers to RFID Technology in Healthcare. Available online: https://www.himss.org/resources/benefits-and-barriers-rfid-technology-healthcare (accessed on 3 February 2025).

| Term | Simplified Explanation |
|---|---|
| Smart Healthcare (SHC) | A modern healthcare system that uses digital tools like sensors and apps to improve care [4]. |
| Artificial Intelligence (AI) | AI solutions offer simulacrums of human-like intelligence, generating active predictive outputs based on training data, to help users make more informed decisions [5]. |
| Internet of Things (IoT) | Everyday devices (like watches or sensors) connected to the internet that collect health data [6]. |
| Big Data Analytics | Using large sets of health information to find patterns and improve medical decisions [7]. |
| Cloud Computing | Storing health data on the internet so it can be accessed anytime, anywhere [8]. |
| Telemedicine | Talking to HCPs through telephone calls or (more commonly nowadays) video conferencing, instead of going to a clinical office [9]. |
| Wearable Devices | Gadgets like smartwatches, tracking indicators like heart rate and steps [10]. |
| eHealth | Using the internet and technology to manage health and access services [11]. |
| mHealth | Health services are accessed through mobile devices like smartphones [12]. |
| Clinical Decision Support Systems (CDSS) | Computer tools that help HCPs decide on the best treatment [13]. |
| Telehealth | Remote healthcare that includes video calls, online monitoring, and virtual care [14]. |
| Smart Radiomics | Using AI to analyze medical images for more precise cancer treatment [15]. |
| Personal Health Records | A person’s health history that they can manage using apps or online tools [16]. |
| Remote Patient Monitoring | Keeping track of a patient’s health from a distance using technology [17]. |
| Digital Citizens | People familiar with using advanced digital technologies (i.e., digital “natives,” rather than “immigrants”), especially younger generations [18]. |
| Cybersecurity | Protecting personal health data from being stolen or misused online [19]. |
| Interoperability | Making sure different health technologies and systems can work well together [20]. |
| Radio Frequency Identification (RFID) | A system using wireless tags to track items or people, such as patients in hospitals [21]. |
| Ambient Intelligence (AMI) | Smart environments that automatically adjust and respond to people’s needs—like lights, temperature, or alerts—using sensors and intelligent systems to improve comfort and safety in healthcare settings [22]. |
| Internet of Medical Things (IoMT) | A network of connected medical devices (like smart monitors, wearable sensors, and health apps) that collect and share patient data in real time to support better diagnosis and care [23]. |
| Study | Definition |
|---|---|
| Vidyasekar (2013) [33] | “Smart healthcare encompasses the use of eHealth and mHealth systems, integrated with connected and intelligent medical devices, alongside policies that promote the health and well-being of citizens.” |
| Sundaravadivel et al. (2017) [34] | “The context of smart healthcare requires that smart solutions operate in a fully autonomous environment.” |
| Tian et al. (2019) [29] | “Smart healthcare employs technologies like wearable devices, IoT, and mobile internet to dynamically access and share information, linking individuals, materials, and healthcare institutions. Additionally, it actively manages and responds to the medical ecosystem in an intelligent manner.” |
| Zeadally et al. (2020) [35] | “Smart healthcare involves using mobile devices along with wearable medical gadgets like blood pressure monitors and glucometers, as well as IoT devices such as implantable sensors, to facilitate continuous patient monitoring and remote treatment.” |
| Zaw et al. (2021) [32] | “Smart healthcare refers to healthcare services that utilize IoT and AI at their core. It involves gathering information via machine learning and acting autonomously based on that data. Intelligent sensors and advanced data acquisition platforms support this process by accurately indexing and analyzing data, thereby enabling value creation.” |
| Topic | Singapore (HIC) | India (LMIC) |
|---|---|---|
| Main goal | Joined-up care and prevention | Access for everyone, everywhere |
| What works best | Shared records, clear rules, stable funding | Huge reach, low cost, faster access |
| Key gaps | Universal provider onboarding; senior inclusion | Connectivity, skills, consistent quality, record integration |
| Characteristic | Description |
|---|---|
| Integration of Advanced Technologies | Utilize AI, surgical robots, and mixed reality to enhance diagnosis, treatment, and efficiency in healthcare processes. |
| Mobile Health Services | Use mobile devices such as smartphones and wearables for patient self-monitoring and remote health management, including access to personal health records. |
| Telehealth | Remote delivery of healthcare services via teleconsultations, tele-ICUs, and virtual agents, ensuring continuous patient care anytime, anywhere. |
| Prevention and Monitoring | Implementation of data collection and monitoring through wearable technology, enabling early illness detection and easy access to patient information for HCPs. |
| Support for Healthcare Research | Foster the use of digital tools in healthcare research to streamline drug discovery, clinical trials, and data collection, improving accuracy, safety, and patient care. |
| Dimension | Drivers (Why Adoption Happens) | Characteristics (How SHC Looks in Practice) |
|---|---|---|
| Core idea | External pressures and socio-technical enablers | Visible features and qualities of SHC systems |
| Typical items | Tech progress (AI/IoT/analytics), aging and chronic disease, workforce/cost pressures, policy and standards, pandemic shocks [5,6,7,20,51] | Telemedicine, mHealth, wearables/RPM, CDSS, radiomics, cloud/shared records [9,10,11,12,13,15,17] |
| Level | System/market context | Service/workflow/interface |
| Example metric | Adoption readiness; compliance with standards; broadband/device availability | Safety, effectiveness, usability, equity of access/outcomes |
| Primary risk if overlooked | Low uptake despite investment | Poor quality/safety despite uptake |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almarri, A.; Hunaiti, Z.; Manivannan, N. A Review of Smart Healthcare: Concept, Drivers, Characteristics, and Challenges. Hospitals 2025, 2, 26. https://doi.org/10.3390/hospitals2040026
Almarri A, Hunaiti Z, Manivannan N. A Review of Smart Healthcare: Concept, Drivers, Characteristics, and Challenges. Hospitals. 2025; 2(4):26. https://doi.org/10.3390/hospitals2040026
Chicago/Turabian StyleAlmarri, Alanoud, Ziad Hunaiti, and Nadarajah Manivannan. 2025. "A Review of Smart Healthcare: Concept, Drivers, Characteristics, and Challenges" Hospitals 2, no. 4: 26. https://doi.org/10.3390/hospitals2040026
APA StyleAlmarri, A., Hunaiti, Z., & Manivannan, N. (2025). A Review of Smart Healthcare: Concept, Drivers, Characteristics, and Challenges. Hospitals, 2(4), 26. https://doi.org/10.3390/hospitals2040026







