Abstract
Compression is the cornerstone of treatment for lymphoedema; however, in patients with Stage III lymphoedema that causes a significant alteration of limb shape and size, additional creative problem solving is required in order to find a solution that fits the person, their limb and their personal circumstances. Medical adaptive compression (MAC) systems provide solutions to complex situations. We present two cases of individuals who completed an inpatient rehabilitation stay for intensive treatment of their lymphoedema and were fitted with MAC devices to ensure long-term success.
1. Introduction
The lymphatic system is a one-way system working together with the circulatory system [1,2]. It is composed of a network of initial lymphatic vessels that absorb the protein-rich fluid from the subcutaneous tissues and direct it into collecting vessels that transport lymph [3,4]. There are three primary functions of the lymphatic system.
- To maintain fluid balance through collection and transport of fluid from tissue spaces back to the systemic circulation [3,5], thus preventing fluid accumulation (oedema) in the tissues.
- The intestinal lymph vessels absorb protein, fat and fat-soluble vitamins from the small intestine.
- To promote immunity through the circulation of lymph fluid to help fight potentially harmful bacteria and viruses [6].
Lymphoedema results from a failure of the lymphatic system and occurs when the demand for lymphatic drainage exceeds the capacity of the lymphatic transportation [7,8]. It is a chronic, debilitating condition, which if not treated early can progress and cause significant problems [9].
The primary form of lymphoedema management is through complex decongestive therapy (CDT) [10]. This involves two stages of treatment: decongestion and maintenance. CDT utilises compression therapy, skin care, exercise and manual lymphatic drainage, all being adapted to each patient’s needs, depending on which approach is being used, with further treatment modalities added where necessary [10,11,12]. Of these modalities, compression is considered the single most important element of treatment [13,14].
Compression can be applied in various ways including compression garments, intermittent pneumatic compression and multi-layer bandaging. Compression garments are found in multiple forms including circular knit, flat knit, off-the-shelf, custom made and medical adaptive compression (MAC) wraps [15]. The effectiveness of compression therapy is dependent on the pressure exerted, the materials used and the right fit for the person [14].
Lymphoedema can cause multiple difficulties including skin changes and changes to the normal form of the leg. In these cases, additional problem solving is required in order to apply appropriate compression to manage or improve their lymphoedema and prevent further deterioration. This article will highlight two cases where the standard compression stocking was not appropriate and additional options in the form of adaptive compression wraps were required.
2. Case Study 1
Mr B is a 68-year-old gentleman who was admitted to the Földi clinic in October 2023 for the treatment of his lower limb lymphoedema. Whilst he reports that he normally receives manual lymphatic drainage three times per week and wears flat knit compression stockings bilaterally on a daily basis, he indicated that during the COVID-19 pandemic, he and his wife isolated themselves at home and therefore did not receive any regular treatment for his lymphoedema. He experienced increased swelling, including a significant increase in the oedema in his left thigh (see Figure 1).

Figure 1.
Mr B on arrival at the Földiklinik—rear view.
He is retired and lives with his wife in their own home. Mr B mobilises with a wheeled walking frame. He is independent with personal cares and receives help for cleaning and gardening.
2.1. Clinical Findings/Physical Examination
On examination all vital signs were within normal range. His abdomen was non-tender; however, there was pronounced connective tissue induration in the lower abdomen with lymphoedema of the abdominal wall. Despite undergoing a gastric balloon implantation and an initial weight reduction of 60 kg, he presented with a Grade III obesity (BMI 52 kg/m2).
Mr B suffered most recently with erysipelas in 2020. He has hyperuricemia with gout attacks and arterial hypertension controlled with medication. Furthermore he reported that hesmokes 40 packs of cigarettes per year. COPD was ruled out by a pulmonologist in 2022. Orthopaedic diseases included knee joint arthrosis on both sides. The relevant surgical history includes an inguinal hernia operation and dermal lipectomy of both lower limbs in 2007. Mr B has arthropathy which reduces his mobility.
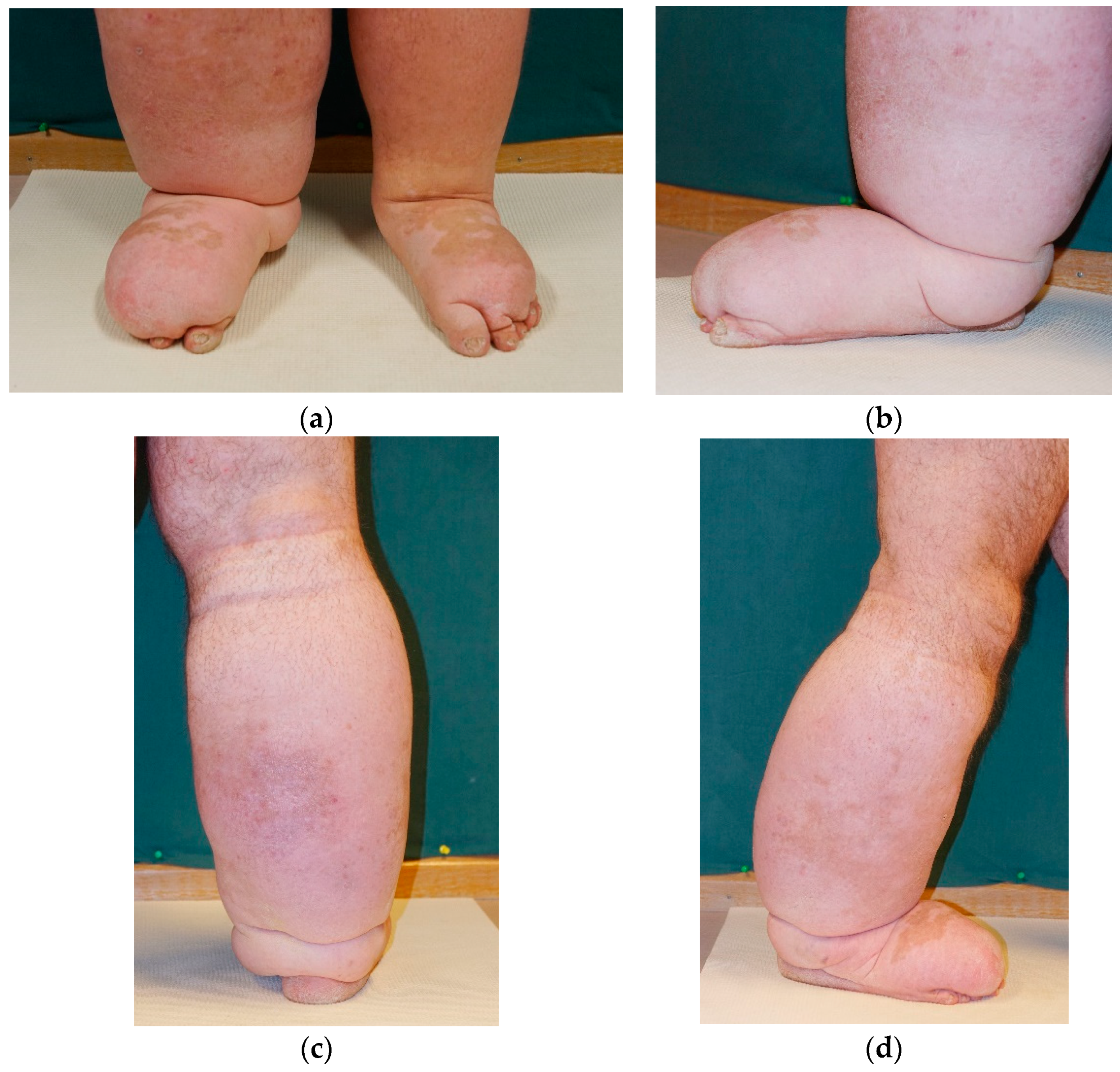
He has Stage III lymphoedema in both lower limbs with the joint contours of the knees, as shown in Figure 2, which are completely abolished, as the tissue is lobularly altered with clear fibrotic hyperkeratotic changes in the area of the lower legs. There was pronounced oedema of the dorsum of the foot with a clearly positive Stemmer’s skin fold sign.

Figure 2.
Mr B on arrival at the Földiklinik—front view.
2.2. Treatment
During his 6-week lymphoedema rehabilitation stay, he received manual lymphatic drainage twice daily and multi-layer compression bandaging 5 days per week. Bandaging was applied from his toes to his knees on both legs. An adapted flat knit compression device with Velcro was applied to his left thigh (Figure 3). This option was chosen because of the great irregularity of the patient’s lymphoedema in this area and it enabled him to maintain his mobility during the reduction phase. He also participated in movement therapy, received skin care and advice on the adaptation of his clothes and shoes, care of the skin fold areas, nutrition and psychological support.

Figure 3.
A flat knit garment was adapted to be able to wrap Mr B’s upper leg to provide sufficient compression during therapy.
2.3. Outcomes
Mr B had a volume reduction of 3.2 L from his left leg and over 2 L from his right leg (see Table 1). He had a significant reduction in fibrosis in both legs with a major reduction in skin folds. Although not formally measured, he indicated an improved quality of life as his mobility improved as did his independence with personal cares. He was fitted with below knee flat knit class 2 compression garments with a toe cap that he was able to don and doff with assistance from his wife. He was also supported by his wife at home regarding the management of his compression garments.

Table 1.
Mr B left and right leg volume measures.
The major challenge for Mr B was finding an appropriate solution for his left thigh. Given his weight and reduced mobility, he was not able to independently manage waist-high or thigh-high garment options.
Two thigh piece adjustable compression wraps were sourced from Juzo (Figure 4 and Figure 5). A major advantage of the wraps was that they could be applied with upward pressure on the straps of the garment, to support the shape of his leg and provide compression from the knee up towards the hip. The Velcro ends mean they can be adjusted throughout the day as ongoing volume reduction occurs to ensure continual pressure and therefore continue to progress the positive results of his inpatient stay. The flexibility from the long arms made it possible to fit the wraps on his complex limb shape.

Figure 4.
Wearing the adjustable compression wraps on his left thigh—front view.

Figure 5.
Rear view of the adjustable compression wrap thigh pieces.
As Mr B is also supported at home by his wife, the thigh compression needed to be easy to manage both by Mr B and by his wife. Given the unusual form of his leg, the wraps made it easier for someone else to help don and doff, as well as enabling easy wear and care.
For this complex presentation, a combination of lower limb compression garments and upper limb compression wraps enabled the perfect solution that both maximised the lymphoedema management as well as enabled increased quality of life.
3. Case Study 2
Mr M is a 40-year-old gentleman who was admitted for treatment of his lymphoedema in September 2022. Mr M has a disability and lives with his parents who are the primary carers. Due to the patient’s brain damage in early childhood, with limited intelligence and clear behavioural abnormalities, therapy is only possible in the company of his mother. She therefore assists in all aspects of his lymphoedema management.
At home, he receives two hours of manual lymph drainage per week and wears knee-high compression stockings bilaterally. He has significant localised oedema on his right foot which was very limiting for Mr M because he could not wear shoes properly. He has a history of recurrent cellulitis, with the foot oedema previously causing him to have friction sores and therefore more erysipelas.
3.1. Clinical Findings
Mr M presented with a BMI of 55 (height 170 cm and weight 159.1 kg). He had Stage III lymphoedema in both lower limbs with his right leg ballooned, distended, and firmly interspersed with tissue, lymphatic cysts and hyperkeratoses distally increasing firm connective tissue areas (see Figure 6). The ankle contour was no longer definable and the rearfoot was massively cushion-like, overhanging over the toes with deep-pitting oedema under strong pressure. There was also deep-pitting oedema over his lower leg. The lymphoedema spread slightly over the knee region to the thigh, especially medially where there was still some pitting oedema.
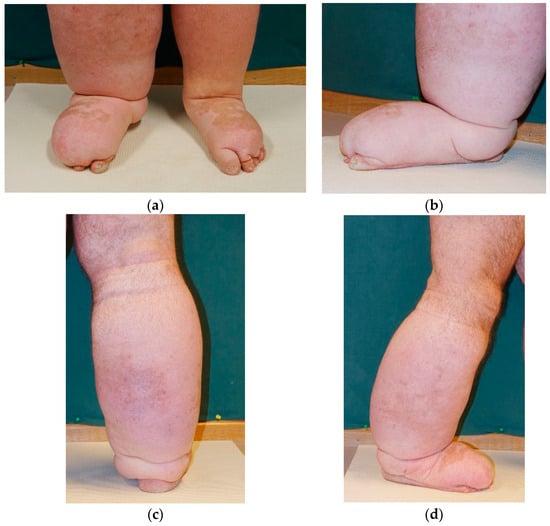
Figure 6.
Photos of Mr M’s right leg and foot on arrival at the Földi clinic: (a) front view feet; (b) right foot medial view; (c) right leg view from the back; (d) right leg lateral view.
The left lower leg was columnar, massively increased in volume and interspersed with tissue with deep-pitting oedema. His ankle contour was not evident, with the back of the foot on the left also cambered. His toes were more clearly affected. Stemmer’s skin fold sign was strongly positive bilaterally.
Mr M had reduced mobility of his lower limbs with a hip flexion of 90 degrees. He was able to lift his legs; however, due to the severity of his lymphoedema, this was very laborious, especially on his right leg.
3.2. Treatment
As per Mr B, Mr M received manual lymphatic drainage twice daily and multi-layer compression bandaging 5 days per week. He was strongly encouraged to move and participated in sport groups and movement therapy. He received skin care advice and, together with his mother, was encouraged to be actively involved in his inpatient care.
3.3. Outcomes
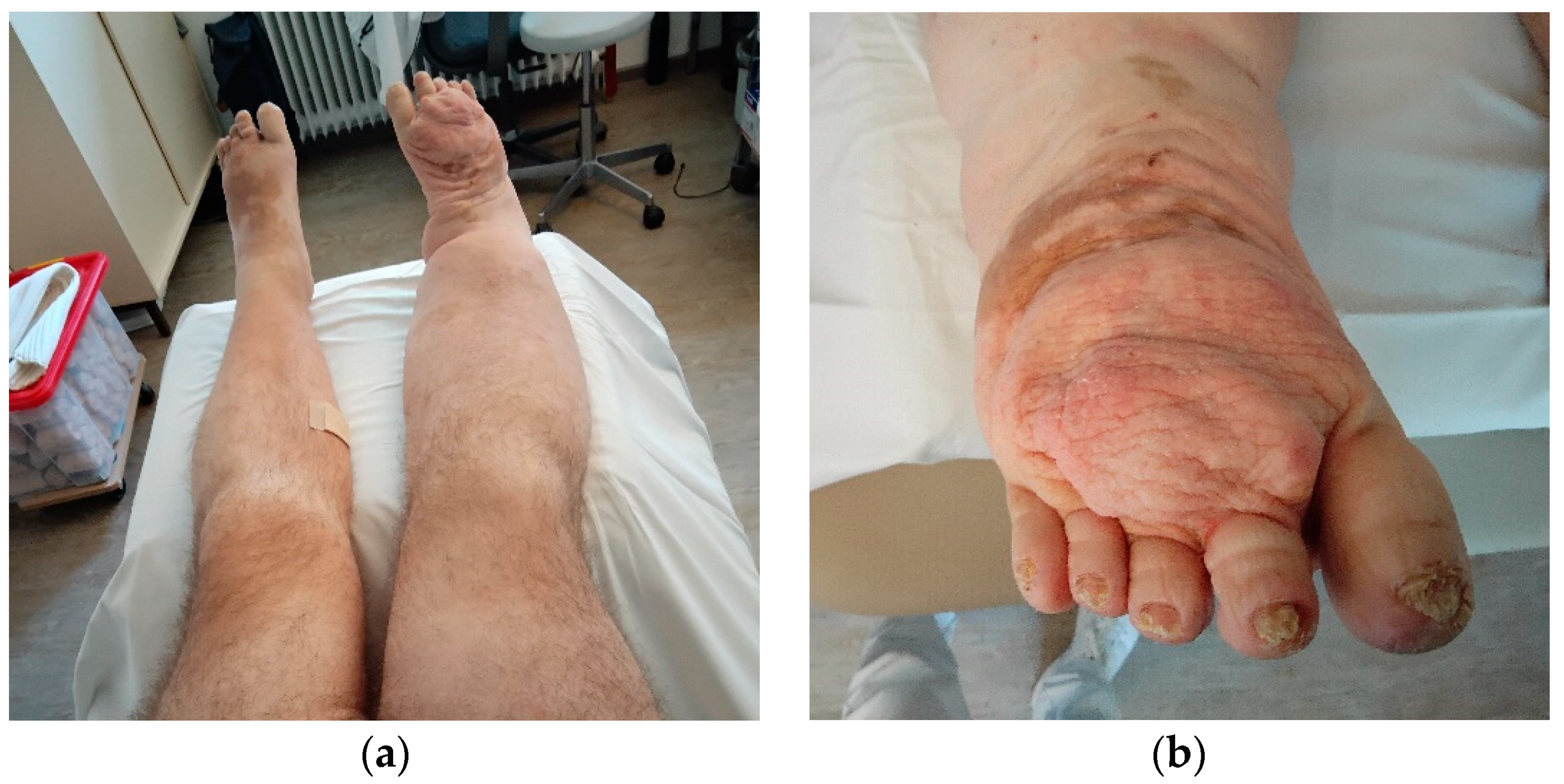
Mr M responded really well to the decongestive therapy, and over the course of his 4 ½ week inpatient stay, had a volume reduction of 3 L in the left leg and almost 7 L in the right leg (see Table 2 and Figure 7). The localised oedema on the dorsum of his feet reduced significantly. Unfortunately, his rehabilitation ended earlier than planned due to a family emergency.

Table 2.
Mr M lower limb volume measures.
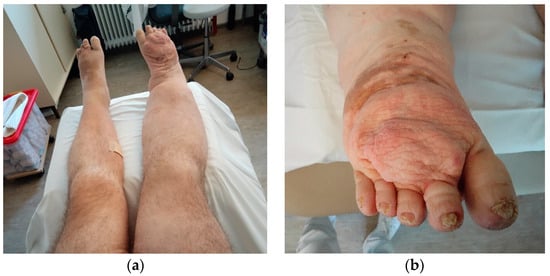
Figure 7.
Mr M after decongestive therapy: (a) front view legs; (b) right foot top view.
The major challenge for Mr M was finding a long-term solution to maintain the improved status of his lymphoedema. He had previously been issued with standard knee-high stockings; however, his mother indicated that with her increasing age, and Mr M’s increased weight, she was finding it extremely difficult to comply with the daily use of the stockings. A solution was required that provided appropriate, ongoing compression and fitted with the needs of the family in terms of donning and doffing.
A combination of an adapted Jobst class 2 foot piece and adjustable compression wraps from Juzo was successfully trialled and prescribed for him. The foot piece (Figure 8) was used to provide appropriate compression for his distal forefoot, with the adjustable compression wrap (Figure 9) providing compression for the rest of his right foot and leg. This system, with the multiple separate components (foot piece (Jobst), foot piece, leg piece, knee piece, thigh piece (Juzo)) meant Mr M’s mother could effectively assist him to don the compression therapy daily and thereby prevent the deterioration of his lymphoedema. Additional inserts in the form of wavey foam were also able to be layered underneath the wraps to provide additional, ongoing decongestive therapy as required.

Figure 8.
Jobst class 2 foot piece.

Figure 9.
Mr M was fitted with an adjustable compression wrap from Juzo.
4. Discussion
Compression is an essential cornerstone of lymphoedema management. However, in order to be effective, it needs to fit with the person, be easily donned and doffed, be tolerated throughout the day and offer maximised function/mobility. Whilst compression garments have traditionally been either flat knit or circular knit stockings, in recent years medial adaptive compression (MAC) devices, also known as adjustable compression wraps (ACW), or adjustable Velcro compression devices (AVCD) have become available. MAC devices are low-stretch compression wraps which apply firm, even pressure on affected areas. They can be easier to put on and off in comparison to flat knit stockings, especially when needing assistance from a care giver. MAC devices can be applied at different pressure levels and can be easily readjusted during the course of the day by the care giver or the patient [16], making them responsive to ongoing decongestive therapy.
Studies have shown that MAC devices are effective in both the decongestive stage and the maintenance stage of CDT [17,18,19]. Mosti and Cavezzi [17] found that MAC devices were more effective for volume reduction than bandages when used during the initial decongestive treatment phase. Ochalek and Kurpiewska [18] also report clinically significant volume reductions in patients using MAC devices for decongestive treatment; however, in their study, there was an equal or better volume reduction for the patients using bandages. Reißhauser and Kornappel [19] suggest that MAC devices are also effective during the maintenance phase of lymphoedema, particularly for patients who require assistance donning and doffing garments.
Complex presentations of lymphoedema often require creative compression solutions and considering a combination of compression options is warranted. From Stage II lymphoedema onwards, the swelling is chronic (i.e., irreversible) [20]. In addition to the pure increase in circumference or volume of the affected limb, there is also a chronic inflammatory change in the interstitium and fibrosis (a hardening of the skin and subcutaneous tissue) develops [4]. The test for pitting oedema is more difficult to perform and requires more pressure. The overall severity of the lymphoedema is much more pronounced and can lead to disability and severely limited functioning of the limb [4]. Our case studies have shown that MAC devices can be a particularly great option for unusual limb shape and for the situation when assistance is required from a care giver.
Ongoing effective management of lymphoedema depends on the ongoing, daily use of compression garments to maintain the reduction achieved during an intensive phase of treatment. These two patients both needed help from their caregivers to don and doff their compression garments, thereby making the MAC the ideal solution for them.
5. Conclusions
Complex physical therapy (manual lymphatic drainage and multilayer compression bandaging) decreases the size of lymphoedema. Tailored compression garments are necessary to maintain the volume of lymphoedema. In Stage III lymphoedema, the irregular lymphoedema volume and altered limb shape may make it difficult to use a compression garment. Therefore, the use of compression wraps with adjustable Velcro segments to this irregular surface could be the solution to ensure ongoing compression in these patients.
The longer the patient maintains the reduced volume of lymphoedema achieved during therapy, the greater their functionality, quality of life and independence.
Author Contributions
Conceptualisation, investigation, writing—original draft preparation, S.W. and J.-B.G.-R.; writing—review and editing, S.W., J.-B.G.-R. and T.D.; supervision, R.M.-V., M.J.V.-G. and T.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. Juzo provided the wraps that were used for these two patients to enable testing and trial during their inpatient stay, prior to discharge.
Institutional Review Board Statement
Both participants provided informed, written consent for their data to be used in this case study. The study was conducted in accordance with the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
No new data were created or analysed in this study. All relevant data are contained within the article.
Acknowledgments
We sincerely thank M. and his family, and B. for sharing their stories with us and enabling the publication of their information. We also acknowledge and thank Juzo for supporting these patients with provision of wraps.
Conflicts of Interest
The authors declare no conflicts of interest. Susan Witt, Jesus-Baltasar Gonzalez-Rubino and Thomas Dieterle are employees of the Földiklinik GmbH & Co. KG. The Földiklinik GmbH & Co. KG had no role in the design, collection, analyses, or interpretation of the data, the writing of the manuscript, or the decision to publish the results. Juzo provided the compression wraps at no cost. Juzo had no role in the design of these case studies; in the collection, analyses or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Breslin, J.W.; Yang, Y.; Scallan, J.P.; Sweat, R.S.; Adderley, S.P.; Murfee, W.L. Lymphatic Vessel Network Structure and Physiology. Compr. Physiol. 2018, 9, 207–299. [Google Scholar] [PubMed]
- Brix, B.; Sery, O.; Onorato, A.; Ure, C.; Roessler, A.; Goswami, N. Biology of Lymphedema. Biology 2021, 10, 261. [Google Scholar] [CrossRef] [PubMed]
- Suami, H.; Scaglioni, M.F. Anatomy of the Lymphatic System and the Lymphosome Concept with Reference to Lymphedema. Semin. Plast. Surg. 2018, 32, 5–11. [Google Scholar] [PubMed]
- Witt, S.; Oberlin, M. Lymphödem—Warum treten Schwellungen auf und was kann ich dagegen tun? Prim. Hosp. Care 2024, 24, 61–66. [Google Scholar] [CrossRef]
- Yun, J.W.; Alexander, J.S. The lymphatic system in health and disease. In Integrated Systems Physiology: From Molecule to Function to Disease; Granger, D.N., Granger, J., Eds.; Morgan & Claypool Publishers: San Rafael, CA, USA, 2018. [Google Scholar]
- Houck, P.D.; Dandapantula, H.K.; Massey, J.M. Lymphatics: Future Perspectives Unrealized Potential. Lymphatics 2023, 1, 87–96. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Towards an Estimate of the Prevalence of Lymphoedema in Australia: A Data Source Scoping Report 2023; AIHW, Ed.; Australian Government: Canberra, Australia, 2023.
- British Lymphology Society. What is Lymphoedema. In Lymph Facts; British Lymphoedema Society: Birmingham, UK, 2020. [Google Scholar]
- Franks, P.J.; Quéré, I.; Keeley, V.; Tilley, A.; Liebl, M.; Murray, S.; Burian, E.A.; Moffatt, C.J.; on behalf of the Lymphedema Observational Study Group International Lymphedema Framework. Quality of Life and Costs Within Decongestive Lymphatic Therapy in Patients with Leg Lymphedema: A Multicountry, Open-Label, Prospective Study. Lymphat. Res. Biol. 2021, 19, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, A.; Baiocchi, J.M.T.; de Andrade, M.F.C. Conservative treatment of lymphedema: The state of the art. J. Vasc. Bras. 2021, 20, e20200091. [Google Scholar] [CrossRef] [PubMed]
- Michopoulos, E.; Papathanasiou, G.; Vasilopoulos, G.; Polikandrioti, M.; Dimakakos, E. Effectiveness and Safety of Complete Decongestive Therapy of Phase I: A Lymphedema Treatment Study in the Greek Population. Cureus 2020, 12, e9264. [Google Scholar] [CrossRef] [PubMed]
- Wigg, J.; Lee, N. Redefining essential care in lymphoedema. Br. J. Community Nurs. 2014, 19 (Suppl. 4), S20–S27. [Google Scholar] [CrossRef] [PubMed]
- International Lymphoedema Framework. Compression Therapy: A position document on compression bandaging. In Best Practice for the Management of Lymphoedema, 2nd ed.; International Lymphoedema Framework: London, UK, 2020. [Google Scholar]
- Rabe, E.; Földi, E.; Gerlach, H.; Jünger, M.; Lulay, G.; Miller, A.; Protz, K.; Reich-Schupke, S.; Schwarz, T.; Stücker, M.; et al. Medical compression therapy of the extremities with medical compression stockings (MCS), phlebological compression bandages (PCB), and medical adaptive compression systems (MAC): S2k guideline of the German Phlebology Society (DGP) in cooperation with the following professional associations: DDG, DGA, DGG, GDL, DGL, BVP. Der Hautarzt 2021, 72 (Suppl. 2), 37–50. [Google Scholar] [PubMed]
- Lymphoedema Framework. Compression Hosiery in Lymphoedema. In Template for Practice; Lymphoedema Framework: London, UK, 2006. [Google Scholar]
- Benigni, J.P.; Uhl, J.-F.; Filori, P.; Balet, F.; Penoel, L. Adjustable compression wraps: Stretch, interface pressures and static stiffness indices. Int. Angiol. 2023, 42, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Mosti, G.; Cavezzi, A.; Partsch, H.; Urso, S.; Campana, F. Adjustable Velcro Compression Devices are More Effective than Inelastic Bandages in Reducing Venous Edema in the Initial Treatment Phase: A Randomized Controlled Trial. Eur. J. Vasc. Endovasc. Surg. 2015, 50, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Ochalek, K.; Kurpiewska, J.; Gradalski, T. Adjustable Compression Wraps (ACW) vs. Compression Bandaging (CB) in the Acute Phase of Breast Cancer-Related Arm Lymphedema Management—A Prospective Randomized Study. Biology 2023, 12, 534. [Google Scholar] [CrossRef] [PubMed]
- Reißhauser, A.; Kornappel, S.; Tsatrafilis, E.; Stroux, A.; Liebl, M.E. Medizinische Adaptive Kompressionssysteme sind Flachstrick-Kompressionsstrümpfen in der KPE Phase II nicht unterlegen. Phys. Med. Rehab. Kur. 2020, 30, 214–221. [Google Scholar]
- Földi, M. Das Lymphödem: Grundlagen, Diagnostik und Therapie. Vasomed 2015, 27, 255–261. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).