Abstract
Background: It remains unclear whether adherence to the 24-hour movement guidelines is beneficial for children with mental, behavioral, and developmental disorders (MBDDs). Methods: The results of the 2016–2020 National Survey of Children’s Health (NSCH) in the U.S. were used in this study. All types of MBDDs, adherence to the different movement guidelines (physical activity [PA], screen time [ST], and sleep), and various health indicators (general physical health, emotional regulation, cognitive and social functioning) were parent-reported. Weighted logistic regression models were used to assess the associations between adherence to the 24-hour movement guidelines and health indicators in children with and without MBDDs. Results: The majority of children with MBDDs had a lower weighted proportion of meeting the PA, ST, and sleep guidelines compared to those without MBDDs (all p values < 0.05). Less than half of the associations between adherence to the 24-hour movement guidelines and the different health indicators were significant among children with MBDDs, while the associations were all significant among children without MBDDs (ORs ranged 1.22–2.10, all p values < 0.05). When there were no between-group differences in the statistically significant associations between guideline adherence and health indicators (e.g., sleep guideline and general physical health), children with specific MBDDs can achieve comparable health benefits through adherence to the 24-hour movement guidelines (e.g., children with emotional disorders or developmental disorders experience better general physical health through adherence to the sleep guideline). Conclusion: We highlight the prioritization of the 24-hour guidelines for different health indicators among children with various MBDDs, and children with certain MBDDs could attain similar health benefits as those without these conditions by adhering to the 24-hour movement guidelines.
1. Introduction
According to the Global Burden of Disease Study 2019 [1], approximately 1 in 10 children worldwide suffer from mental, behavioral, and developmental disorders (MBDDs), leading to different adverse health consequences. Numerous studies have highlighted the compromised physical health of children with MBDDs [2,3,4]. Assessing general physical health offers a convenient snapshot of a patient’s overall well-being [5]. For example, children with MBDDs, such as autism spectrum disorder (ASD), often encounter challenges in regulating their emotions compared to typically developing (TD) individuals [6]. Moreover, children with MBDDs, including learning disabilities (LDs) and ASD, frequently grapple with difficulties in cognitive tasks [7] and social interactions [8]. Collectively, global efforts to improve the health outcomes of children with MBDDs are of paramount importance.
Healthy lifestyles such as engaging in moderate-to-vigorous physical activity (PA) [9], limiting screen time (ST) and sedentary behavior [10,11], and ensuring adequate sleep duration [12] have been identified as beneficial factors that can positively influence the health outcomes of children and adolescents. To encompass these three health behaviors throughout the day, the World Health Organization (WHO) and over twenty countries have introduced 24-hour movement guidelines as a practical and effective approach [13]. Our previous research [14] revealed that children with MBDDs were less likely to meet these 24-hour movement guidelines compared to their peers without MBDDs, which could partially contribute to the poorer health outcomes observed in children with MBDDs. The existing literature indicates that adhering to these guidelines has been associated with improved well-being and long-term health outcomes in TD children [15,16,17,18,19,20]. However, it remains unclear whether children with MBDDs can derive similar benefits as TD children from following these 24-hour movement guidelines. For example, some studies have suggested that adhering to the recommended sleep duration guideline did not lead to improved general physical health [21] and cognitive functioning [22] in children with ASD, while others have argued the opposite [23,24]. Moreover, different subtypes of MBDDs appear to have varying impacts on the relationship between guideline adherence and health outcomes. For example, among children with ASD [25] or attention deficit hyperactivity disorder (ADHD) [26], meeting the 24-hour movement guidelines has been linked to improved social and cognitive functioning. Nevertheless, these studies have mainly focused on individual MBDDs such as ASD and ADHD or specific health indicators including social and cognitive functioning. There is a notable absence of research that comprehensively considers the entire spectrum of MBDDs and multiple health indicators simultaneously.
Taken together, in this study, we used nationwide U.S. data to investigate the optimal 24-hour movement guideline strategies for children with and without MBDDs. We hypothesize the following: (1) higher adherence to the 24-hour movement guidelines will be associated with better health indicators (e.g., sleep guideline and general physical health) in children with MBDDs, and (2) the magnitude of these associations will differ among children with different subtypes of MBDDs.
2. Materials and Methods
2.1. Study Design and Participants
We analyzed data from the 2016–2020 National Survey of Children’s Health (NSCH), which was designed by the Centers for Disease Control and Prevention’s National Center for Health Statistics and sponsored by the Mental and Child Health Bureau of the Health Resources and Services Administration [27]. NSCH is a multistage survey conducted annually to assess the physical and emotional health of U.S. children aged 0–17 years. We have permission to obtain the information from the Child & Adolescent Health Measurement Initiative, Data Resource Center (reference numbers: 11275).
The survey design and the detailed procedure are presented publicly and are available on the following website: https://www.childhealthdata.org (accessed on 6 April 2025). The NSCH data were collected through the following two steps: (1) An initial household screener questionnaire was sent by email to identify households with children, and one child was randomly selected from each eligible household. (2) The eligible household received a detailed topical questionnaire, completed by an adult (parent or caregiver) who was familiar with the child’s health.
The dataset from the 2016–2020 NSCH contains 174,551 participants (N = 50,212 for 2016, 21,599 for 2017, N = 30,530 for 2018, N = 29,433 for 2019, N = 42,777 for 2020). Samples were weighted to account for nonresponse bias and oversampling [28]. This study only focused on children aged 6–17 years due to the NSCH’s omission of investigating physical activity behaviors in the 0–5-year age group. We also excluded samples that had missing data on key information such as adherence to the 24-hour movement guidelines and the selected health indicators. At last, we selected 120,551 participants aged 6–17 years as the samples. For each type of MBDD, specific sample sizes are presented in Supplementary Figure S1.
2.2. Measurement of MBDDs
In the NSCH, MBDDs were measured by the respondent’s answer to the question “Has a doctor or other health care provider ever told you that this child has (specified disorder)?” A child was considered to have an MBDD if their parent reported one or more of the following: “emotional disorders (EDs)”, including anxiety problems or depression; “behavioral disorders (BDs)”, including attention-deficit/hyperactivity disorder (ADHD), behavioral or conduct problems (BP), or Tourette syndrome (TS); and “developmental disorders (DDs)”, including autism spectrum disorder (ASD), learning disability (LD), intellectual disability (ID), developmental delay (DD), or speech or other language disorder (SD). A binary response was recorded as 0 = children without certain MBDDs and 1 = children with certain MBDDs.
2.3. Measurement of 24-Hour Movement Guidelines Adherence
2.3.1. Physical Activity
Physical activity was measured by the question: “During the past week, on how many days did this child exercise, play a sport, or participate in physical activity for at least 60 min?” The answers were categorized into the following four groups: “0 days”, “1–3 days”, “4–6 days”, and “every day”. Responses were dichotomized to represent whether the children met the physical activity guidelines of engaging in at least 60 min/day of physical activity (1 = every day, 0 = 6 days or less) [13].
2.3.2. Sleep Duration
Sleep duration was measured using the question: “During the past week, how many hours of sleep did this child get on an average weeknight?”. The answers were categorized into seven groups as follows: “Less than 6 h”, “6 h”, “7 h”, “8 h”, “9 h”, “10 h”, and “11 or more hours”. Children aged 6 to 12 years old who reported 9 or more hours of sleep per 24 h, as well as adolescents aged 13 to 18 years old who reported 8 or more hours of sleep per 24 h, were considered to be meeting the guideline recommendations (coded as 1); all the others were not (coded as 0) [13].
2.3.3. Screen Time
Within the 2016 to 2017 NSCH, screen time was quantified with the following two questions: (1) “on an average weekday how much time does this child usually spend in front of a TV watching TV programs, videos, or playing video games?” (2) “on an average weekday how much time does this child usually spend with computers, cell phones, handheld video games, and other electronic devices doing things other than schoolwork?”. Responses were scored on the following four-point scale: 0 = None; 0.5 = Less than 1 h; 1 = 1 h; 2 = 2 h; 3 = 3 h; and 4 = 4 or more hours. The sum of the two items represented the total screen time. Within the 2018 to 2020 NSCH, screen time was measured with the question, “On most weekdays, about how much time did this child spend in front of a TV, computer, cell phone, or other electronic device watching programs, playing games, accessing the internet, or using social media? (Do not include time spent doing schoolwork.)” Responses were scored on the following five-point rating scale: 0.5 = Less than 1 h; 1 = 1 h; 2 = 2 h; 3 = 3 h; and 4 = 4 or more hours. No more than 2 h of total screen time per day was considered to be meeting the guideline recommendations [13]. A dichotomous variable was determined to represent whether the participants met the screen time guidelines (1 = no more than 2 h per day, 0 = >2 h per day).
2.4. Measurement of Health Indicators
2.4.1. General Physical Health
General physical health was defined by answering the following question: “In general, how would you describe the child’s health?”. Response options included the following: “Excellent”; “Very good”; “Good”; “Fair”; and “Poor”. We combined the responses to create a dichotomous general physical health variable (1 = Excellent/Very good/good, 0 = Fair/Poor).
2.4.2. Emotional Regulation
Emotional regulation was defined by answering the following: “This child stays calm and in control when faced with a challenge”. Response options from the 2016 to 2017 NSCH were as follows: “Definitely true”; “Somewhat true”; and “Not true”. Response options from the 2018 to 2020 NSCH were as follows: “Always”; “Usually”; “Sometimes’; “Never”. We combined the responses to create a dichotomous emotional regulation variable (1 = Definitely true/Somewhat true, 0 = Not true, 2016–2017 NSCH; 1 = Always/Usually/Sometimes, 0 = Never, 2018–2020 NSCH).
2.4.3. Cognitive Functioning
Cognitive functioning was defined by answering the following question: “Does this child have serious difficulty concentrating, remembering, or making decisions because of a physical, mental, or emotional condition?” Response options included the following: “Yes/Serious difficulty”; “No difficulty”. This variable was binary coded (1 = No difficulty; 0 = Yes/Serious difficulty).
2.4.4. Social Functioning
Social functioning was defined by answering the following question: “Compared to other children his or her age, how much difficulty does this child have making or keeping friends?” Response options were as follows: “No difficulty”; “A little difficulty”; “A lot of difficulty”. We combined responses to create a dichotomous social functioning variable (1 = No difficulty, 0 = A little difficulty/A lot of difficulty).
2.5. Covariates
We used the following variables as covariates: age (6–11 years, 12–17 years), gender (male, female), race/ethnicity (white, non-white), highest parental education (less than high school, high school, some college or associate degree, college degree or higher), and household income level (percentage of the federal poverty level [FPL]; <100% FPL, 100–199% FPL, 200–399% FPL, ≥400% FPL). All covariates were assessed through parent-/caregiver-reported questionnaires.
2.6. Statistical Analysis
Descriptive statistics were used for all the variables. Unweighted sample sizes and weighted proportions were used to describe the categorical variables. Logistic regression models were used to assess the associations between not meeting the 24 h movement guidelines and health indicators in children with and without various MBDDs. We fitted the models with adjustments for the child’s age, gender, race/ethnicity, highest parental education, and household income level. Models were stratified by group (children with certain MBDDs vs. children without certain MBDDs). Independent adjusted logistic regressions were performed on data from each subgroup to obtain each MBDDs-specific ratio estimates. A two-sample test was used on the basis of point estimates and standard error (se) to examine the statistical differences in estimated odds ratios (OR) by groups. A former study used the same method [29]. In all analysis procedures, we used survey weights, stratification, and primary sampling units to represent noninstitutionalized population of U.S. children that were available from the NSCH data. All the data were analyzed using R Core Team Statistical Software, version 4.1.0 (2021). A p value < 0.05 (both-sided) was considered to be statistically significant.
2.7. Role of the Funding Source
The funders had no role in study design, data analysis, and interpretation, or writing of the essay. The corresponding authors had full access to all the data in the study and took final responsibility for the decision to submit this article for publication.
3. Results
Table 1 presents the participants’ characteristics. Of the 120,551 children included in this study, 51,249 children were aged 6–11years (49.69%, 95%CI: 49.04–50.35%), 51.08% of children were male, and the majority identified as White (67.09%, 95%CI: 66.43–67.74%). About one-third of the children included in this study resided in the households with low parental educational levels and family income levels. Regarding the prevalence of various MBDDs, the disorder with the highest prevalence among children with EDs was anxiety (11.47%, 95%CI: 11.10–11.85%), among children with BDs was ADHD (11.71%, 95%CI: 11.35–12.09%), and among children with DDs was LD (8.76%, 95%CI: 8.40–9.13%).

Table 1.
Participant Characteristics a.
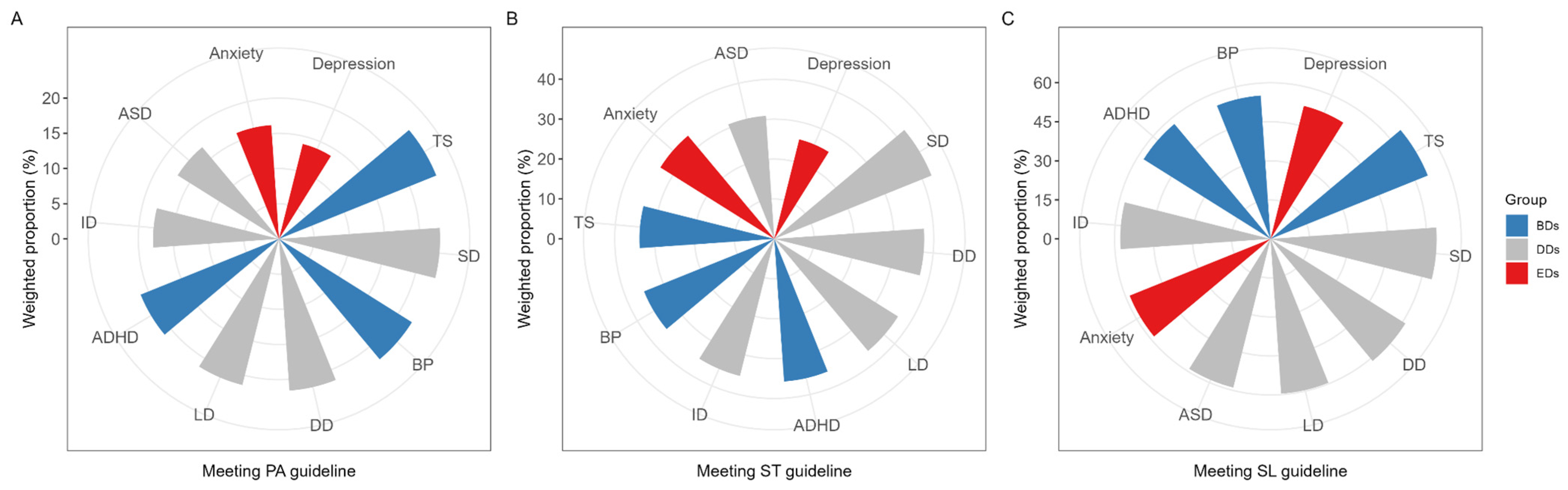
Among children with various MBDDs, those with depression had the lowest weighted proportion of meeting PA (13.91%, 95%CI: 12.02–16.03%), ST (25.74%, 95%CI: 23.46–28.17%), and sleep (52.70%, 95%CI: 50.17–55.22%) guidelines (Figure 1). As shown in Supplementary Tables S1–S10, the majority of children with MBDDs had a lower weighted proportion of meeting the PA, ST, and sleep guidelines compared to those without MBDDs, including anxiety, depression, ASD, and ID (all p values < 0.05). However, there were no significant differences in the weighted proportion of meeting the PA guideline among children with ADHD or BP in BDs, children with LD or ID in DDs, and children without corresponding disorders (all p values > 0.05).
Figure 1.
The weighted proportion of meeting 24 h movement guidelines in children with various MBDDs. (A) The weighted proportion of meeting physical activity guideline in children with various MBDDs; (B) The weighted proportion of meeting screen time guideline in children with various MBDDs; (C) The weighted proportion of meeting sleep guideline in children with various MBDDs. Abbreviation: MBDDs = Mental, Behavioral, and Developmental Disorders; EDs = Emotional Disorders; BDs = Behavioral Disorders; ADHD = Attention-Deficit/Hyperactivity Disorder; BP = Behavior/conduct Problem; TS = Tourette Syndrome; DDs = Developmental Disorders; ASD = Autism Spectrum Disorder; LD = Learning Disability; ID = Intellectual Disability; DD = Developmental Delay; SD = Speech or other language Disorder; PA = Physical Activity; ST = Screen Time; SL = sleep.
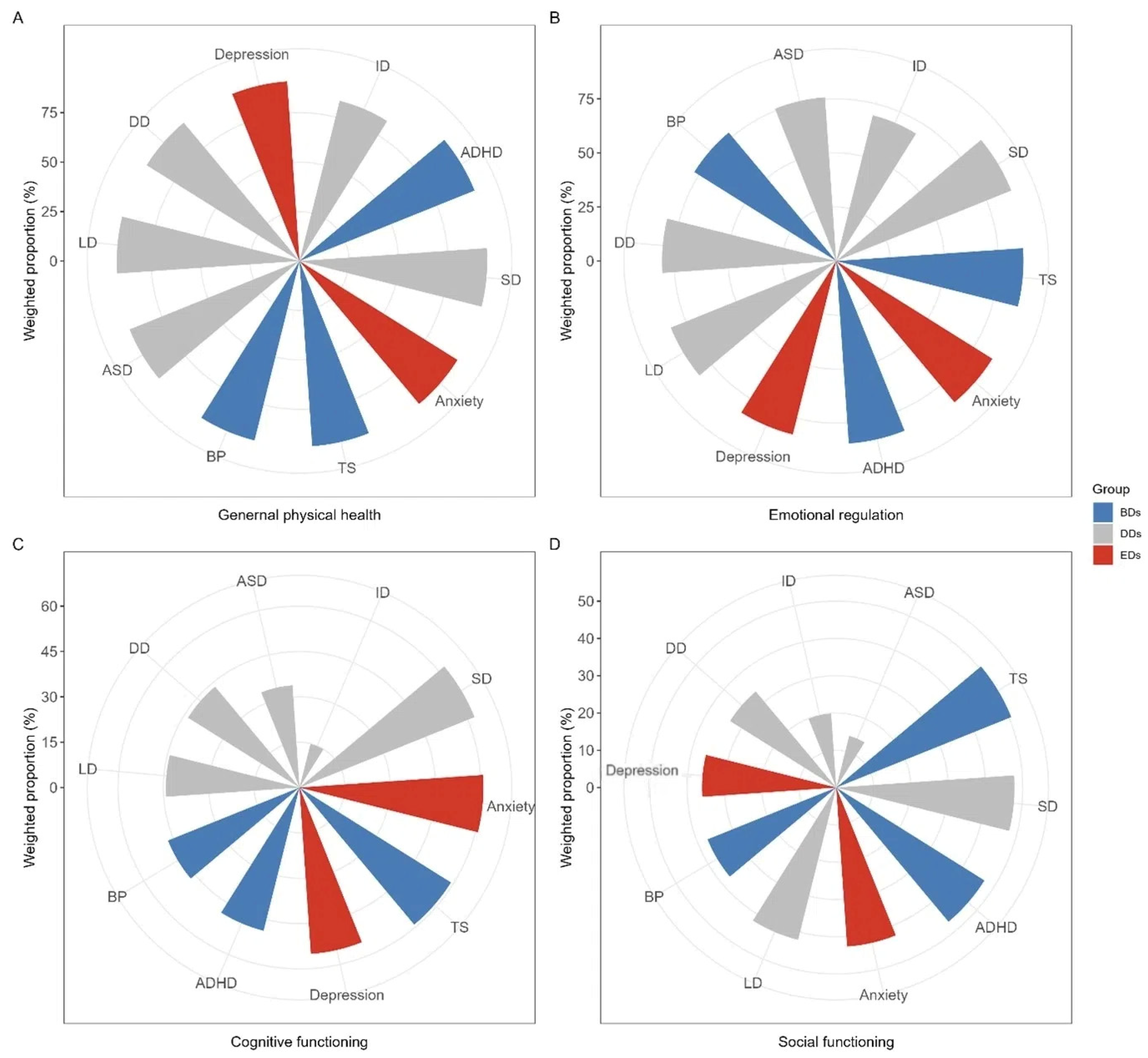
Figure 2 presents the weighted proportion of having positive health indicators among children with various MBDDs. Children with ID exhibited the lowest weighted proportions of having positive health indicators, particularly in the areas of general physical health (83.47%, 95%CI: 79.17–87.03%), emotional regulation (69.55%, 95%CI: 64.51–74.16%), and cognitive functioning (14.87%, 95%CI: 11.24–19.42%, Supplementary Table S8). Children with ASD had the lowest level of satisfactory social functioning (14.34%, 95%CI: 12.26–16.71%, Supplementary Table S6). Poor health conditions were more common among children with various MBDDs in contrast to children without corresponding disorders, including general physical health, emotional regulation, cognitive functioning and social functioning (all p values < 0.05, Supplementary Tables S1–S10).
Figure 2.
The weighted proportion of having positive health indicators in children with various MBDDs. (A) The weighted proportion of having positive general physical health in children with various MBDDs; (B) The weighted proportion of having positive emotion regulation in children with various MBDDs; (C) The weighted proportion of having positive cognitive functioning in children with various MBDDs; (D) The weighted proportion of having positive social functioning in children with various MBDDs. Abbreviation: MBDDs = Mental, Behavioral, and Developmental Disorders; EDs = Emotional Disorders; BDs = Behavioral Disorders; ADHD = Attention-Deficit/Hyperactivity Disorder; BP = Behavior/conduct Problem; TS = Tourette Syndrome; DDs = Developmental Disorders; ASD = Autism Spectrum Disorder; LD = Learning Disability; ID = Intellectual Disability; DD = Developmental Delay; SD = Speech or other language Disorder.
Among the children with MBDDs, less than half of the associations between adherence to the 24 h movement guidelines and the relevant health indicators were significant (Table 2). For example, among children with EDs and children with most of the types of DDs (i.e., ASD, LD, DD, and SD), not meeting the sleep guideline was significantly associated with higher odds for difficulties in general physical health (OR ranged 1.36–2.07, all p values < 0.05). Not meeting both the ST and sleep guidelines were significantly associated with higher odds for difficulties in emotional regulation among all types of MBDDs (OR ranged 1.45–1.75, all p values < 0.05), except for ID and TS. Positive associations of not meeting both PA and ST guidelines with difficulties in cognitive functioning were only present in children with ADHD or LD (OR ranged 1.20–1.42, all p values < 0.05). Not meeting all the PA, ST, and sleep guidelines was significantly associated with higher odds for difficulties in social functioning among children with depression, DD, and SD (OR ranged 1.26–1.84, all p values < 0.05). Among children without MBDDs, not meeting the PA, ST, and sleep guidelines was significantly associated with higher odds for difficulties in all health indicators (OR ranged 1.22–2.10, all p values < 0.05) (Table 3).

Table 2.
Significant OR of associations between meeting 24 h movement guidelines and health indicators in children with various MBDDs a.

Table 3.
Significant OR of associations between meeting 24 h movement guidelines and health indicators in children without various MBDDs a.
Table 4 shows the between-group differences regarding the estimated ORs between the children with and without various MBDDs, and the data are displayed in the Supplementary Figures S2–S11. When there were no between-group differences in the statistically significant associations between meeting the guidelines and the various health indicators, children with certain MBDDs could attain similar health benefits as those without these conditions by adhering to the 24 h movement guidelines. For example, children with all types of EDs and DDs could experience improved general physical health by following sleep guidelines (all p values > 0.05), except for ID. Similarly, children with all types of MBDDs could experience improved emotional regulation by following the ST guidelines (all p values > 0.05), except for TS and ID. More than one-third of associations between not meeting the PA, ST, or sleep guidelines and difficulties in cognitive functioning were significantly lower in children with MBDDs than in children without MBDDs (Z ranged from −1.97 to −4.10, all p values < 0.05). The associations between not meeting all the PA, ST, and sleep guidelines and difficulties in social functioning showed no significant between-group differences between the children with and without depression, DD, and SD.

Table 4.
The Z values of the comparisons of associations between meeting 24 h movement guidelines with health indicators among children with and without various MBDDs a.
4. Discussion
Overall, the principal finding of this paper was the prioritization of the 24 h guideline recommendations for different health indicators among children with various MBDDs. Among the children without MBDDs, not meeting the 24 h movement guidelines was significantly associated with higher odds for difficulties in all health indicators including general physical health, emotional regulation, cognitive functioning, and social functioning, while less than half of these associations were significant among children with MBDDs. When there were no between-group differences in the statistically significant associations between meeting the guidelines and the selected health indicators, the children with certain MBDDs could attain similar health benefits as compared to those without these conditions by adhering to 24 h movement guidelines.
For most types of children with EDs and DDs, adherence to the sleep guideline was found to be beneficial for general physical health outcomes. Since there were no between-group differences in these associations, adhering to the sleep guideline was the most efficient way to promote general physical health outcomes for both children with and without MBDDs. Recent evidence has elucidated that sleep duration is associated with circadian health thus impacting general health [30]. Consistent with our study, previous clinical trials have confirmed the significant effect of sleep intervention on children with EDs and DDs. For example, for children with ASD [31] or anxiety [32], satisfying sleep improved their behavioral functioning and quality of life or reduced the severity of anxiety. Our findings suggest that healthcare professionals could enhance the general physical health in children with EDs and DDs including ASD, anxiety, or depression by prioritizing sleep guideline adherence. Specifically for children with ASD, evidence-based strategies might include establishing structured bedtime routines, minimizing environmental distractions, and implementing visual or behavioral cues to reinforce healthy sleep patterns [33]. Similarly, for children with anxiety or depression, healthcare professionals could focus on managing nighttime worries through relaxation techniques, cognitive–behavioral therapy (CBT), or caregiver education on sleep hygiene practices [34].
In this study, adhering to both the ST and sleep guidelines had been proven to be the optimal method for facilitating emotional regulation among children with most types of MBDDs. In line with our research, a longitudinal study [35] sampling Chinese adolescents demonstrated that, at baseline, adherence to the recommended guidelines for ST and sleep was associated with a significant reduction in anxiety and depressive symptoms six months later, with an obscure effect on emotion regulation from adherence to the physical activity guideline. Another U.S. study [36] focusing on children aged 8–11 found that only adherence to the screen time guideline was significantly linked to emotion regulation. This discrepancy may be attributed to differences in the ages and geographic locations of the study groups, as the mechanisms underlying the relationship between sleep and emotional regulation may vary across developmental stages and sociocultural influences [37,38]. However, these studies were conducted on TD children, leaving a critical gap in research regarding children with MBDDs. Our study aimed to fill this gap by examining a diverse population of U.S. children aged 6 to 17 years with MBDDs. Our findings underscored the particular importance of meeting sleep and ST guidelines in promoting emotional regulation among children with MBDDs. Given the growing body of evidence highlighting the impact of sleep and ST on emotional regulation, we call for multidisciplinary efforts to help children with MBDDs achieve the goal of recommended sleep and ST duration time. For example, it is strongly recommended that clinicians provide evidence-based guidance on managing screen exposure, particularly before bedtime, while also emphasizing the role of consistent sleep routines in emotional regulation [39].
As for cognitive functioning, our study found that the majority of associations of not meeting the PA, ST, or sleep guidelines with difficulties in cognitive functioning were non-significant, while these associations were all significant among children without MBDDs. There is mounting research from Japan [40], South Africa [41], U.S. [42], and China [43] that suggest intervention through exercising, restricting screen time, or assuring sleep duration could boost executive function, working memory, and academic performance, though most studies focus on TD children, with few addressing those with MBDDs such as LD [44]. However, the evidence is still not strong enough. The results of our study revealed that adhering to the 24 h movement guidelines may not be the most efficacious way to reinforce cognitive functioning, because adverse health outcomes including cognition in children with MBDDs are usually pathological and may not be greatly affected by lifestyle improvements alone, often requiring adjunctive medication or clinical intervention [45]. For example, for children with ADHD, the most credible evidence of intervention in cognitive functioning is from a meta-analysis [46], which examined the significant effect of novel digital intervention when children have barriers to traditional interventions such as adherence to the 24 h movement guidelines. Integrating the 24 h movement guidelines with other interventions may presumably reduce the gap between the children with and without MBDDs.
For children with depression, DD, and SD, the benefit of improved social functioning through adherence to all the 24 h movement guidelines may be consistent with that of children without corresponding disorders. Some comprehensive intervention programs often encompass lifestyle factors including physical activity, screen time, and sleep duration as a package for simultaneous intervention [47]. Congruent with the preceding research [48], our results showed a favorable association between meeting all the 24 h movement guidelines and social functioning for children with depression. Nevertheless, the existing empirical evidence tailored to children with DD or SD is sparse. The present study offers a novel insight that comprehensive intervention for children with DD or SD should not be overlooked. Clinically, this highlights the need for individualized strategies that address the unique challenges faced by children with DD or SD in adhering to three movement guidelines, which involve a comprehensive assessment of each child’s specific characteristics and their personal barriers to following the recommended movement protocols [49]. For example, children with DD may find it hard to reach the recommended PA level due to motor impairments [50], or children with SD may be addicted to online communication since they find it challenging to communicate with others in the real life [51]. Based on these assessments, it is essential that intervention strategies, such as visual supports [52] or engaging activities [53], be tailored to the child’s unique interests, abilities, and developmental needs. Additionally, collaborating with caregivers, educators, and therapists to create a consistent and supportive environment can further enhance adherence to the guidelines [54]. These holistic and individualized strategies can help children with DD or SD overcome barriers to movement guideline adherence, ultimately enhancing their social skills through increased participation in group activities, peer interactions, and structured play [55].
Our findings have significant implications for public health policy and practices concerning children with MBDDs. In our previous study [14], we observed that children with MBDDs faced challenges in adhering to the guidelines, which could result in fewer benefits compared to children without MBDDs, as shown in this study. Parents or guardians of children with MBDDs were more likely to use extended screen time as a distraction [56]. Additionally, sleep disturbances were specifically prevalent in most children with MBDDs [57]. Parents perceived that the 24 h movement guidelines were not inclusive or suitable for children with disabilities [58]. These findings underscore the need for a comprehensive intervention framework that encompasses movement guidelines and additional supportive approaches, such as parental education and coaching programs, for children with MBDDs. Specific supportive strategies for parents, including the use of structured screen time schedules (e.g., limiting recreational screen use to 1–2 h per day, as recommended by the American Academy of Pediatrics [59]) or employing screen time as part of a structured reward system to encourage positive behaviors [60], combined with the access to professional support from sleep specialists and telehealth consultations [61], could address the dual challenges of screen time overuse and sleep disruptions identified in our study. It is advisable that partnerships between healthcare providers and community organizations prioritize accessible parent education platforms [62] to demonstrate guideline adaptability, such as modifying aerobic activities through aquatic therapy for children with mobility limitations [63], as a previous case series [64] reported that aquatic therapy was effective in improving outcomes in patients with physical disabilities. By equipping families with these evidence-based resources and emphasizing education on adherence to guidelines, we can empower parents and guardians to implement these recommendations more effectively, ultimately improving the long-term health outcomes for children with MBDDs.
The NSCH is a nationwide, population-based study that provides a nationally representative sample of children. The comprehensive investigation enabled us to map the associations between the 24 h movement guidelines and health indicators. However, this study had several limitations. First, all the information in the NSCH was parent-reported. Inevitably, there may be a recall bias concerning the information related to the MBDDs and adherence to the 24 h movement guidelines. Future studies are encouraged to incorporate more objective measurement tools to enhance data accuracy and reliability. For instance, wearable devices can be used to objectively assess physical activity levels and sleep duration [65], reducing potential recall bias associated with parent-reported data. Secondly, NSCH was a cross-sectional survey, which means it was limited in establishing temporal associations or causality. Future research such as longitudinal design is necessary to investigate potential causal pathways. Lastly, additional studies are needed to explore the dose–response associations between the 24 h movement guidelines and health indicators.
5. Conclusions
Among children without MBDDs, not meeting the 24 h guidelines was significantly associated with higher odds for difficulties in all health indicators including general physical health, emotional regulation, cognitive functioning, and social functioning, while less than half of these associations were significant among children with MBDDs. We highlight the prioritization of the 24 h guideline recommendations for different health indicators among children with different MBDDs, and children with certain MBDDs can attain similar health benefits as those without these conditions by adhering to the 24 h movement guidelines. Multidisciplinary support frameworks involving healthcare providers and caregivers are vital for policy recommendations such as promoting specific movement guideline adherence for different subtypes of MBDDs, thereby achieving optimal health outcomes in children with MBDDs.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/future3020006/s1, Methodology supplement, Figures S1–S11; Tables S1–S10.
Author Contributions
N.P., J.-X.Z. and X.-T.S. were all co-first authors, contributing to conceptualization, writing the original draft, reviewing, and editing. Both X.-H.L. and L.-Z.L. were co-corresponding authors, accepting full responsibility for the conduct of the study and participating in conceptualization, supervision, project administration, funding acquisition, reviewing, and editing. K.-Z.Y. helped with data curation, reviewing, and editing. L.S. assisted in data validation, reviewing, and editing. X.W. participated in data interpretation, reviewing, and editing. J.J. assisted with supervision, project administration, funding acquisition, reviewing, and editing. All authors approved the final manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
The study was supported by National Natural Science Foundation of China (82273649 and 82103794) and the Guangdong Basic and Applied Basic Research Foundation (2021A1515011757 and 2022B1515130007).
Institutional Review Board Statement
This study of an anonymous public dataset with no identifiable information on the survey participants was determined exempt by the Institutional Review Board of the Sun Yat-sen University. Ethical approval of the original NSCH for all procedures was obtained from the National Center for Health Statistics Research Ethics Review Board. The dataset from the Child and Adolescent Health Measurement Initiative, Data Resource Center, was requested for this study and with permission was granted in 1 March 2022 (reference number: 11275).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All the data we used were from the 2016–2020 National Survey of Children’s Health (NSCH). All the variables can be found online (https://www.childhealthdata.org (accessed on 6 April 2025)). We will gladly share our statistical analysis strategy and analytical code upon request to the corresponding author.
Acknowledgments
We gratefully acknowledge the financial support of the National Natural Science Foundation of China (82273649 and 82103794) and the Guangdong Basic and Applied Basic Research Foundation (2021A1515011757 and 2022B1515130007). We are also grateful to the U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau, and the Data Resource Center on Child and Adolescent Health for their assistance in gathering and providing data. Meanwhile, we like to thank the parents who took the time to participate in the 2016–2020 National Survey of Children’s Health.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- GBD Results. Institute for Health Metrics and Evaluation. Available online: https://vizhub.healthdata.org/gbd-results (accessed on 28 February 2023).
- De la Cruz, L.F.; Mataix-Cols, D. General health and mortality in Tourette syndrome and chronic tic disorder: A mini-review. Neurosci. Biobehav. Rev. 2020, 119, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Tosh, G.; Clifton, A.V.; Xia, J.; White, M.M. General physical health advice for people with serious mental illness. Cochrane Database Syst. Rev. 2014, CD008567. [Google Scholar] [CrossRef] [PubMed]
- Eisenhower, A.S.; Baker, B.L.; Blacher, J. Children’s delayed development and behavior problems: Impact on mothers’ perceived physical health across early childhood. Soc. Sci. Med. 2009, 68, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Luijten, M.A.J.; Haverman, L.; van Litsenburg, R.R.L.; Roorda, L.D.; Grootenhuis, M.A.; Terwee, C.B. Advances in measuring pediatric overall health: The PROMIS® Pediatric Global Health scale (PGH-7). Eur. J. Pediatr. 2022, 181, 2117–2125. [Google Scholar] [CrossRef]
- Reyes, N.M.; Pickard, K.; Reaven, J. Emotion regulation: A treatment target for autism spectrum disorder. Bull. Menn. Clin. 2019, 83, 205–234. [Google Scholar] [CrossRef]
- D’Mello, A.M.; Gabrieli, J.D.E. Cognitive Neuroscience of Dyslexia. Lang. Speech Hear. Serv. Sch. 2018, 49, 798–809. [Google Scholar] [CrossRef]
- Hunsche, M.C.; Cervin, M.; Storch, E.A.; Kendall, P.C.; Wood, J.J.; Kerns, C.M. Social functioning and the presentation of anxiety in children on the autism spectrum: A multimethod, multiinformant analysis. J. Psychopathol. Clin. Sci. 2022, 131, 198–208. [Google Scholar] [CrossRef]
- Poitras, V.J.; Gray, C.E.; Borghese, M.M.; Carson, V.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.T.; Pate, R.R.; Gorber, S.C.; Kho, M.E.; et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41 (Suppl. S3), S197–S239. [Google Scholar] [CrossRef]
- Paulich, K.N.; Ross, J.M.; Lessem, J.M.; Hewitt, J.K. Screen time and early adolescent mental health, academic, and social outcomes in 9- and 10- year old children: Utilizing the Adolescent Brain Cognitive Development SM (ABCD) Study. PLoS ONE 2021, 16, e0256591. [Google Scholar] [CrossRef]
- Carson, V.; Hunter, S.; Kuzik, N.; Gray, C.E.; Poitras, V.J.; Chaput, J.-P.; Saunders, T.J.; Katzmarzyk, P.T.; Okely, A.D.; Gorber, S.C.; et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: An update. Appl. Physiol. Nutr. Metab. 2016, 41 (Suppl. S3), S240–S265. [Google Scholar] [CrossRef]
- Chaput, J.-P.; Gray, C.E.; Poitras, V.J.; Carson, V.; Gruber, R.; Olds, T.; Weiss, S.K.; Gorber, S.C.; Kho, M.E.; Sampson, M.; et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41 (Suppl. S3), S266–S282. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Carson, V.; Chaput, J.-P.; Gorber, S.C.; Dinh, T.; Duggan, M.; Faulkner, G.; Gray, C.E.; Gruber, R.; Janson, K.; et al. Canadian 24-Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep. Appl. Physiol. Nutr. Metab. 2016, 41 (Suppl. S3), S311–S327. [Google Scholar] [CrossRef] [PubMed]
- Pan, N.; Lin, L.-Z.; Nassis, G.P.; Wang, X.; Ou, X.-X.; Cai, L.; Jing, J.; Feng, Q.; Dong, G.-H.; Li, X.-H. Adherence to 24-hour movement guidelines in children with mental, behavioral, and developmental disorders: Data from the 2016–2020 National Survey of Children’s Health. J. Sport Health Sci. 2023, 12, 304–311. [Google Scholar] [CrossRef]
- Lien, A.; Sampasa-Kanyinga, H.; Colman, I.; Hamilton, H.A.; Chaput, J.P. Adherence to 24-hour movement guidelines and academic performance in adolescents. Public Health 2020, 183, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Saunders, T.J.; Gray, C.E.; Poitras, V.J.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.T.; Olds, T.; Gorber, S.C.; Kho, M.E.; Sampson, M.; et al. Combinations of physical activity, sedentary behaviour and sleep: Relationships with health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41 (Suppl. S3), S283–S293. [Google Scholar] [CrossRef]
- Vaquero-Solís, M.; Tapia-Serrano, M.A.; Hortigüela-Alcalá, D.; Jacob-Sierra, M.; Sánchez-Miguel, P.A. Health Promotion through Movement Behaviors and Its Relationship with Quality of Life in Spanish High School Adolescents: A Predictive Study. Int. J. Environ. Res. Public Health 2021, 18, 7550. [Google Scholar] [CrossRef]
- Janssen, I.; Roberts, K.C.; Thompson, W. Is adherence to the Canadian 24-Hour Movement Behaviour Guidelines for Children and Youth associated with improved indicators of physical, mental, and social health? Appl. Physiol. Nutr. Metab. 2017, 42, 725–731. [Google Scholar] [CrossRef]
- Xiong, X.; Dalziel, K.; Carvalho, N.; Xu, R.; Huang, L. Association between 24-hour movement behaviors and health-related quality of life in children. Qual. Life Res. 2022, 31, 231–240. [Google Scholar] [CrossRef]
- Walsh, J.J.; Barnes, J.D.; Cameron, J.D.; Goldfield, G.S.; Chaput, J.-P.; Ledoux, A.-A.; Zemek, R.L.; Tremblay, M.S. Associations between 24 hour movement behaviours and global cognition in US children: A cross-sectional observational study. Lancet Child Adolesc. Health 2018, 2, 783–791. [Google Scholar] [CrossRef]
- Li, C.; Haegele, J.A.; Sun, F.; Alves, M.L.T.; Ang, S.H.C.; Lee, J.; Ng, K.; Alves, I.D.S.; Healy, S.; Huang, W.Y.; et al. Meeting the 24-h movement guidelines and health-related outcomes among youth with autism spectrum disorder: A seven-country observational study. Child Adolesc. Psychiatry Ment. Health 2022, 16, 50. [Google Scholar] [CrossRef]
- Liu, Z.; Herold, F.; Healy, S.; Haegele, J.; Block, M.E.; Ludyga, S.; Ng, J.L.; Gerber, M.; Hossain, M.M.; Taylor, A.; et al. Understanding 24-hour movement guideline adherence and links to school achievement, social-behavioural problems, and emotional functioning among children and adolescents with learning disabilities. Int. J. Sport Exerc. Psychol. 2025, 23, 57–81. [Google Scholar] [CrossRef]
- Brown, D.M.Y.; McPhee, P.G.; Kwan, M.Y.; Timmons, B.W. Implications of Disability Severity on 24-Hour Movement Guideline Adherence Among Children with Neurodevelopmental Disorders in the United States. J. Phys. Act. Health 2021, 18, 1325–1331. [Google Scholar] [CrossRef] [PubMed]
- Joseph, A.B. Sleep and Cognitive Functioning in Children with Disabilities. Except. Child. 2013, 79, 391–405. [Google Scholar] [CrossRef]
- Kong, C.; Chen, A.; Ludyga, S.; Herold, F.; Healy, S.; Zhao, M.; Taylor, A.; Müller, N.G.; Kramer, A.F.; Chen, S.; et al. Associations between meeting 24-hour movement guidelines and quality of life among children and adolescents with autism spectrum disorder. J. Sport Health Sci. 2023, 12, 73–86. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Haegele, J.A.; Wu, Y.; Li, C. Meeting the 24-Hour Movement Guidelines and Outcomes in Adolescents with ADHD: A Cross-Sectional Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 2132. [Google Scholar] [CrossRef]
- Ghandour, R.M.; Jones, J.R.; Lebrun-Harris, L.A.; Minnaert, J.; Blumberg, S.J.; Fields, J.; Bethell, C. The Design and Implementation of the 2016 National Survey of Children’s Health. Matern. Child Health J. 2018, 22, 1093–1102. [Google Scholar] [CrossRef]
- Cree, R.A.; Bitsko, R.H.; Robinson, L.R.; Holbrook, J.R.; Danielson, M.L.; Smith, C.; Kaminski, J.W.; Kenney, M.K.; Peacock, G. Health Care, Family, and Community Factors Associated with Mental, Behavioral, and Developmental Disorders and Poverty Among Children Aged 2–8 Years—United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 1377–1383. [Google Scholar] [CrossRef]
- Di Martino, A.; O’connor, D.; Chen, B.; Alaerts, K.; Anderson, J.S.; Assaf, M.; Balsters, J.H.; Baxter, L.; Beggiato, A.; Bernaerts, S.; et al. Enhancing studies of the connectome in autism using the autism brain imaging data exchange II. Sci. Data 2017, 4, 170010. [Google Scholar] [CrossRef]
- Roenneberg, T.; Foster, R.G.; Klerman, E.B. The circadian system, sleep, and the health/disease balance: A conceptual review. J. Sleep Res. 2022, 31, e13621. [Google Scholar] [CrossRef]
- Papadopoulos, N.; Sciberras, E.; Hiscock, H.; Williams, K.; McGillivray, J.; Mihalopoulos, C.; Engel, L.; Fuller-Tyszkiewicz, M.; Bellows, S.T.; Marks, D.; et al. Sleeping Sound Autism Spectrum Disorder (ASD): A randomised controlled trial of a brief behavioural sleep intervention in primary school-aged autistic children. J. Child Psychol. Psychiatry 2022, 63, 1423–1433. [Google Scholar] [CrossRef]
- Alfano, C.A.; Ginsburg, G.S.; Kingery, J.N. Sleep-related problems among children and adolescents with anxiety disorders. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Loring, W.; Malow, B. Sleep Hygiene and Related Interventions: Their Impact on Sleep. In Clinical Handbook of Behavioral Sleep Treatment in Children on the Autism Spectrum; McLay, L.K., France, K.G., Blampied, N.M., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2022; pp. 127–136. [Google Scholar] [CrossRef]
- Fernández-Puerta, L.; Prados, G.; Jiménez-Mejías, E. Interventions that Improve Sleep in Caregivers of Adult Care-Recipients: A Systematic Review. West. J. Nurs. Res. 2022, 44, 180–199. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Pan, Y.; Ma, Z.; Wang, D.; Zou, R.; Fan, F. Cross-sectional and longitudinal associations of adherence to the 24-hour movement guidelines with mental health problems among Chinese adolescents. J. Psychosom. Res. 2023, 170, 111352. [Google Scholar] [CrossRef] [PubMed]
- Guerrero, M.D.; Barnes, J.D.; Walsh, J.J.; Chaput, J.P.; Tremblay, M.S.; Goldfield, G.S. 24-Hour Movement Behaviors and Impulsivity. Pediatrics 2019, 144, e20190187. [Google Scholar] [CrossRef]
- Palmer, C.A.; Alfano, C.A. Sleep and emotion regulation: An organizing, integrative review. Sleep Med. Rev. 2017, 31, 6–16. [Google Scholar] [CrossRef]
- El-Sheikh, M.; Kelly, R.J.; Philbrook, L.E. Sleep and Development: Familial and Socio-cultural Considerations. In Family Contexts of Sleep and Health Across the Life Course; McHale, S.M., King, V., Buxton, O.M., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2017; pp. 25–49. [Google Scholar] [CrossRef]
- Enderlin, C.; Kuhlmann, M.E.; Harris, M.; Hadley, M.; Sullivan, A.; Rose, K.M.; Mitchell, A.; Matthews, E.E. Integrative Management of Sleep Disturbances. In Advanced Practice Psychiatric Nursing, 2nd ed.; Tusaie, K.R., Fitzpatrick, J.J., Eds.; Springer: New York, NY, USA, 2016. [Google Scholar] [CrossRef]
- Kitano, N.; Kai, Y.; Jindo, T.; Tsunoda, K.; Arao, T. Compositional data analysis of 24-hour movement behaviors and mental health in workers. Prev. Med. Rep. 2020, 20, 101213. [Google Scholar] [CrossRef]
- Sampasa-Kanyinga, H.; Standage, M.; Tremblay, M.; Katzmarzyk, P.; Hu, G.; Kuriyan, R.; Maher, C.; Maia, J.; Olds, T.; Sarmiento, O.; et al. Associations between meeting combinations of 24-h movement guidelines and health-related quality of life in children from 12 countries. Public Health 2017, 153, 16–24. [Google Scholar] [CrossRef]
- McGowan, A.L.; Gerde, H.K.; Pfeiffer, K.A.; Pontifex, M.B. Meeting 24-hour movement behavior guidelines in young children: Improved quantity estimation and self-regulation. Early Educ. Dev. 2023, 34, 762–789. [Google Scholar] [CrossRef]
- Zeng, X.; Cai, L.; Yang, W.; Tan, W.; Huang, W.; Chen, Y. Association between the 24-hour movement guidelines and executive function among Chinese children. BMC Public Health 2022, 22, 1017. [Google Scholar] [CrossRef]
- Huang, C.J.; Tu, H.Y.; Hsueh, M.C.; Chiu, Y.H.; Huang, M.Y.; Chou, C.C. Effects of Acute Aerobic Exercise on Executive Function in Children with and Without Learning Disability: A Randomized Controlled Trial. Adapt. Phys. Act. Q. 2020, 37, 404–422. [Google Scholar] [CrossRef]
- Barnhill, L.J. The diagnosis and treatment of individuals with mental illness and developmental disabilities: An overview. Psychiatr. Q. 2008, 79, 157–170. [Google Scholar] [CrossRef] [PubMed]
- Kollins, S.H.; DeLoss, D.J.; Cañadas, E.; Lutz, J.; Findling, R.L.; E Keefe, R.S.; Epstein, J.N.; Cutler, A.J.; Faraone, S.V. A novel digital intervention for actively reducing severity of paediatric ADHD (STARS-ADHD): A randomised controlled trial. Lancet Digit. Health 2020, 2, e168–e178. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.W.; Stein, M.B.; Nishimi, K.M.; Ge, T.; Coleman, J.R.I.; Chen, C.-Y.; Ratanatharathorn, A.; Zheutlin, A.B.; Dunn, E.C.; 23andMe Research Team; et al. An Exposure-Wide and Mendelian Randomization Approach to Identifying Modifiable Factors for the Prevention of Depression. Am. J. Psychiatry 2020, 177, 944–954. [Google Scholar] [CrossRef] [PubMed]
- Sampasa-Kanyinga, H.; Colman, I.; Goldfield, G.S.; Janssen, I.; Wang, J.; Podinic, I.; Tremblay, M.S.; Saunders, T.J.; Sampson, M.; Chaput, J.-P. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 72. [Google Scholar] [CrossRef]
- Shields, N.; Synnot, A.J.; Barr, M. Perceived barriers and facilitators to physical activity for children with disability: A systematic review. Br. J. Sports Med. 2012, 46, 989–997. [Google Scholar] [CrossRef]
- Gmmash, A.S.; Effgen, S.K.; Skubik-Peplaski, C.; Lane, J.D. Parental Adherence to Home Activities in Early Intervention for Young Children with Delayed Motor Development. Phys. Ther. 2021, 101, pzab023. [Google Scholar] [CrossRef]
- Nurkhamidah, N.; Mutadho, F.; Rafli, Z. Speech Delay in Early Childhood: A Case Study of a 3.5-Year-Old Child. IDEAS J. Engl. Lang. Teach. Learn. Linguist. Lit. 2024, 12, 1929–1944. [Google Scholar] [CrossRef]
- Rentschler, L.F.; Hume, K.A.; Wong, C.; Plavnic, J.; Schultz, T. Use of Visual Supports with Young Children with Autism. In Handbook of Early Intervention for Autism Spectrum Disorders: Research, Policy, and Practice; Dixon, D.R., Sturmey, P., Matson, J.L., Eds.; Springer Nature: Cham, Switzerland, 2024; pp. 317–341. [Google Scholar] [CrossRef]
- Jang, H.; Reeve, J.; Deci, E.L. Engaging students in learning activities: It is not autonomy support or structure but autonomy support and structure. J. Educ. Psychol. 2010, 102, 588–600. [Google Scholar] [CrossRef]
- Rapoff, M.A.; Duncan, C.; Karlson, C. Strategies for Improving Adherence to Pediatric Medical Regimens. In Adherence to Pediatric Medical Regimens; Rapoff, M.A., Duncan, C., Karlson, C., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2023; pp. 201–243. [Google Scholar] [CrossRef]
- Hart Barnett, J. Three Evidence-Based Strategies That Support Social Skills and Play Among Young Children with Autism Spectrum Disorders. Early Child. Educ. J. 2018, 46, 665–672. [Google Scholar] [CrossRef]
- Smith, B.J.; Grunseit, A.; Hardy, L.L.; King, L.; Wolfenden, L.; Milat, A. Parental influences on child physical activity and screen viewing time: A population based study. BMC Public Health 2010, 10, 593. [Google Scholar] [CrossRef]
- Robinson-Shelton, A.; Malow, B.A. Sleep Disturbances in Neurodevelopmental Disorders. Curr. Psychiatry Rep. 2016, 18, 6. [Google Scholar] [CrossRef] [PubMed]
- Handler, L.; Tennant, E.M.; Faulkner, G.; Latimer-Cheung, A.E. Perceptions of Inclusivity: The Canadian 24-Hour Movement Guidelines for Children and Youth. Adapt. Phys. Activ. Q. 2019, 36, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Council on Communications and Media; Hill, D.; Ameenuddin, N.; Chassiakos, Y.R.; Cross, C.; Hutchinson, J.; Levine, A.; Boyd, R.; Mendelson, R.; Moreno, M.; et al. Media and Young Minds. Pediatrics 2016, 138, e20162591. [Google Scholar] [CrossRef]
- Christakis, D.A. The Challenges of Defining and Studying “Digital Addiction” in Children. J. Am. Med. Assoc. 2019, 321, 2277–2278. [Google Scholar] [CrossRef] [PubMed]
- Malow, B.A.; Byars, K.; Johnson, K.; Weiss, S.; Bernal, P.; Goldman, S.E.; Panzer, R.; Coury, D.L.; Glaze, D.G. A Practice Pathway for the Identification, Evaluation, and Management of Insomnia in Children and Adolescents with Autism Spectrum Disorders. Pediatrics 2012, 130 (Suppl. S2), S106–S124. [Google Scholar] [CrossRef]
- DeHoff, B.A.; Staten, L.K.; Rodgers, R.C.; Denne, S.C. The Role of Online Social Support in Supporting and Educating Parents of Young Children with Special Health Care Needs in the United States: A Scoping Review. J. Med. Internet Res. 2016, 18, e6722. [Google Scholar] [CrossRef]
- Rohn, S.; Pavlic, M.N.; Rosenbaum, P. Exploring the use of Halliwick aquatic therapy in the rehabilitation of children with disabilities: A scoping review. Child Care Health Dev. 2021, 47, 733–743. [Google Scholar] [CrossRef]
- Fragala-Pinkham, M.A.; Dumas, H.M.; Barlow, C.A.; Pasternak, A. An Aquatic Physical Therapy Program at a Pediatric Rehabilitation Hospital: A Case Series. Pediatr. Phys. Ther. 2009, 21, 68. [Google Scholar] [CrossRef]
- Rosenberger, M.E.; Buman, M.P.; Haskell, W.L.; McConnell, M.V.; Carstensen, L.L. 24 Hours of Sleep, Sedentary Behavior, and Physical Activity with Nine Wearable Devices. Med. Sci. Sports Exerc. 2016, 48, 457–465. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).