1. Introduction
Adequate activity throughout life helps maintain peak health and functional ability through aging. Very recent scientific evidence suggests that public health messaging for activity could be represented as ‘My Physical Activity Plate’ [
1]. This concept provides a user-friendly tool that emphasizes the benefit of movement, allowing exercise habits to be individualized. Exercise elicits a blood pressure (BP) response, and rhythmic aerobic exercise leads to a healthy BP-lowering adaptation, but heavy resistance exercise has a differing dosage-dependent response [
2]. The American Heart Association suggests that moderate resistance training is a safe and effective approach to reducing cardiovascular disease (CVD) risk and even recommends weightlifting 2 times per week [
3]. Recently functional exercise has become more accepted as a therapeutic modality and fitness trend. Functional exercise includes movements that incorporate multiple joints, muscles, and ranges of motion and essentially improves activities of daily living [
4]. Interventions that are designed to model activities of daily living are considered functional exercise. Functional exercise programs are reported to be beneficial to well-being, to improve work capacity, and to improve functional ability. For example, a 9-month supervised program which included aerobic and circuit-style resistance training was shown to improve functional capacity, reduce BP, and increase strength in older women [
5]. Separately, Chien et al. reported that 12 weeks of sandbag carry training improved glucose control and increased strength [
6].
Load carriage is quickly becoming a strength training option that offers realistic and functional training that is relative to everyday activities. Functional training that incorporates load carriage has direct applications to certain occupations (firefighting, military, industrial, etc.), but load carriage exercise could become a valuable component to clinical exercise programs as well. Strength training programs often include machines or free weight exercises, but another option is the loaded carry (load carriage). Simply put, ‘loaded’ refers to using a weighted implement and ‘carry’ refers to the exercise of carrying that weight over a distance. Load carriage exercise works the entire body to effectively strengthen the core postural muscles. Studies have shown that load carriage can improve health, work capacity, overall strength, and grip-strength [
7]. Load carriage exercise can be accomplished in multiple ways [
8]. A farmer’s handle load carriage is where the load is carried in the hands with arms hanging down and the person walks a distance carrying the weight. The zercher load carriage is where the load is carried in front of the body and held in the arms while the person walks a distance carrying the weight. It seems that no study has compared the BP responses to these types of weighted carry; so, to encourage individualized exercise programs that include functional weighted carries, the vascular responses need to be examined.
Exercise improves blood vessel health, but each type of exercise (aerobic, resistance, or combination) has a different effect on cardiovascular health overall [
9,
10]. Furthermore, there seems to be no studies that examine sex-differences in vascular responses to load carriage. Vascular health and blood vessel stiffness can be measured by pulse pressure (PP) and augmentation index (AIx) which is an index of arterial stiffness that quantifies the reflected blood flow waveforms [
10]. Previously we reported that 24 weeks of aerobic exercise improved vascular health in hypertensive black adults [
11]. Separately we reported that 4 weeks of circuit-style resistance training had a larger effect on vascular health measures and BP more than traditional resistance training [
12]. To best of our knowledge, cardiovascular responses to the farmer’s handle load carriage (load carried with arms hanging down) or to zercher load carriage (load in front of the body held in the arms) have never been examined. Therefore, the purpose of our study was to measure and compare the vascular and BP responses to a farmer’s handle load carriage and to a zercher load carriage and to examine sex-differences in the responses.
2. Methods
We used a within-subject repeated measures study design to compare the vascular responses to load carriage in two configurations. The study consisted of two visits to the exercise physiology laboratory where the participants arrived at the same time each morning, seven days apart, and the same procedure was followed for each visit. Young adults were recruited from the Department of Kinesiology. Criteria for inclusion were no prior diagnosis of hypertension and no prior back, hip, or shoulder injury. All participants gave written informed consent and filled out a general health history form prior to the study. The study protocol was approved by the Institutional Review Board of California State University San Marcos, and all procedures were in accordance with the ethical standards of the Declaration of Helsinki.
2.1. Experimental Protocol
Upon arrival, anthropometric measurements were collected. Height (cm) and weight (kg) were measured using a stadiometer and scale. Body mass index (BMI, kg⋅m−2) was calculated. Participants were asked to remove any jewelry, shoes and socks, and any excess clothing before having body composition measured. Body fat percentage was assessed with a bioelectrical impedance machine (InBody770, Cerritos, CA, USA). After this, participants were asked to sit in a chair with feet flat on the floor. Seated peripheral BP was manually measured in the dominant arm twice during each visit, and the average of all readings over the visits is reported as clinical BP. Peripheral BP is measured at the arm level, is performed in clinical offices and is the BP that hypertension guidelines follow.
2.2. Vascular Measurements
We conducted a pre-exercise pulse wave analysis in the reclined position. Participants then completed a 30 s weighted carry followed by a post-exercise pulse wave analysis within 10 s of exercise. Vascular measurements and pulse wave analysis were collected using the SphygmoCor XCEL system (SphygmoCor XCEL, AtCor Medical, Sydney Australia) as previously reported [
13]. Data from pulse waveforms were assessed by the software’s internal quality control index (operator index > 80%). The average of three measures is reported. Pulse wave analysis is reliable and provides measurements of multiple vascular parameters: central aortic systolic and diastolic BP, augmentation index adjusted to HR of 75 beats per min (AIx@75), and subendocardial viability ratio (SEVR) [
14]. Central BP is the measured BP at the heart level and has been shown to be a better predictor of CVD risk [
15]. AIx@75 is an indirect measure of arterial stiffness, an independent predictor of CVD, and related to many chronic diseases [
16]. SEVR is an estimate of myocardial oxygenation related to cardiac workload and could be an indicator of coronary blood flow [
17]. In our laboratory, we have calculated the intraclass correlation coefficient (ICC) for pulse wave measurements at >0.962.
2.3. Load Carriage Tests
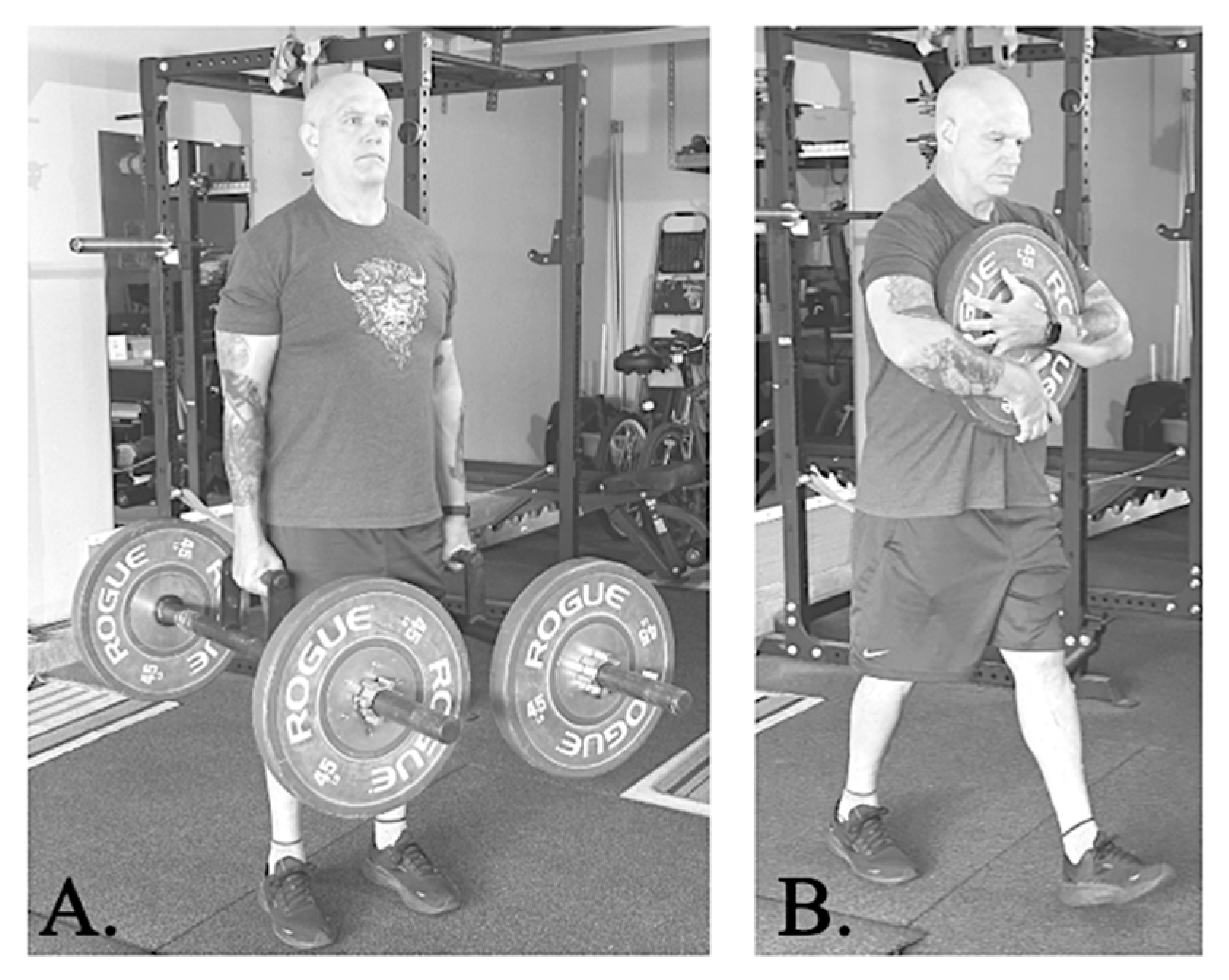
All participants completed the farmer’s handle load carriage first and the zercher load carriage one week later (
Figure 1). The study was designed this way to limit variations in the methodology for each type of loaded carry. Both load carriage maneuvers required walking for 30 s on an inside temperature-regulated flat surface while holding onto a training implement. All participants were instructed to walk with shoulders back in an upright position for the duration of each protocol. This study is the first to test a walking load carriage for 30 s. It is our hope that future research will investigate different protocols and perhaps examine time and dosage responses. For the current study, we calculated an individualized (to body weight) and relative (to participant training status) load amount for each carry. Each participant was asked how many times per week they participate in resistance training workouts.
Using strength-based guides [
18], the following relative body weight percentages were used to calculate each individualized amount of weight for the carry:
- ♦
Participant reports resistance training 0–3 times/week: weight carried was 50% body weight for the farmer’s handle (with the load split in ½ so that each hand carried the same amount) and 30% body weight for the zercher carry.
- ♦
Participant reports resistance training > 3 times/week: weight carried was 75% body weight for the farmer’s handle (with the load split in ½ so that each hand carried the same amount) and 40% body weight for the zercher carry.
Each carry weight was rounded to the nearest pound for each test, and calibrated professional Olympic weight plates (Rogue Fitness, Columbus, OH, USA) were used for both tests.
Farmer’s handle load carriage (load in both hands on the side of body) was completed in the first experimental visit. Farmer’s handles are basically barbells (Rogue Farmers Walk handles, Rogue Fitness, Columbus, OH, USA) with a handle in the middle of the bar for the participant to hold, and the load is adjusted by placing calibrated plates on the end of each farmer’s handle. When these implements are used in training, the farmer’s handles can be carried unilaterally in one hand or bilaterally in both hands with the arms hanging at the side. The participants in our study carried weight bilaterally on the farmer’s handles with equal weight (½ of the total load) in each hand. It has been reported that unilateral carriage is inherently riskier because it results in asymmetrical loading of the spine, hip, and increased bending of the lumbar region which leads to higher lateral forces and spinal compression [
8,
19]. Zercher load carriage (load in the crook of elbows in front of the body) was completed in the second experimental visit. Participants were instructed to carry the weight plate(s) in front of them as shown in
Figure 1.
2.4. Statistical Analysis
Statistical analyses were performed using SPSS 29.0.2 (SPSS Inc., Chicago, IL, USA) The corresponding author had full access to the data in the study and was responsible for the integrity of the data set and data analysis. The distribution of outcome variables was examined by the Shapiro–Wilk test of normality, and Levene test was used to determine homogeneity of variances. Differences between pre- and post-load carriage values were compared using the paired sample t-test. All pre- and post- parameters were compared with independent sample t-test and confirmed using one-way analysis of variance. The effect size for analysis was examined using Cohen’s d. Repeated measures analysis of variance were used to evaluate time (levels: pre- and post-) and carry (levels: farmer’s handle and zercher) by group (levels: female and male) interactions, and within-group Tukey’s post hoc analysis was performed. Relationships were examined with correlations (Pearson, two-tailed). The results are expressed as mean and standard deviation (mean ± SD) with p < 0.05 required for statistical significance.
3. Results
Thirty-nine young adults were enrolled in the study, and one dropped out, so we report data on 38 participants: 22 females and 16 males.
Table 1 provides basic physiological characteristics of the participants. The females reported less times exercising each week (3.1 ± 1.2 vs. 4.8 ± 1.9 times;
p < 0.05,
d = 1.08) and less frequent resistance training (1.5 ± 1.5 vs. 2.6 ± 1.7 times;
p < 0.05,
d = 0.69) compared to males). The females in our study had lower clinic systolic BP levels (121.5 ± 10.3 mmHg vs. 131.3 ± 8.3 mmHg for males;
p < 0.05,
d = 1.03). Females weighed less (64.3 ± 8.9 kg vs. 83.5 ± 12.9 kg;
p < 0.05,
d = 1.77) but had higher percent body fat (30.3 ± 6.6% vs. 19.0 ± 7.2%;
p < 0.05,
d = 1.64) compared to males. Body composition was not related to any vascular health responses to load carriage in males. Body fat percentage in females had a direct relationship with change in vascular stiffness measured by AIx@75 with both types of load carriage (
r = 0.539,
p < 0.05 for zercher carriage;
r = 0.571,
p < 0.05 for farmer’s handle carriage).
Experimental data from pre- to post-carry are reported in
Table 2 and
Table 3. Males carried more weight under both conditions. Both types of load carriage led to significant increases in central systolic BP and AIx@75 for both sexes.
Table 2 reports data from the farmer’s handle carry. Peripheral systolic BP, central systolic BP, and AIx@75 increased with carry in both females and males with this type of carry (
p < 0.05 for both). The post-carry peripheral systolic BP and central systolic BP were lower in females compared to males suggesting a smaller BP response in females with carry.
Table 3 reports data from the zercher load carry. Peripheral systolic BP only increased in females, but central systolic BP and AIx@75 increased with carry in both females and males with this type of carry (
p < 0.05 for both). The peripheral systolic BP and central systolic BP were both lower in females at both pre- and post-carry timepoints. This is a representation of BP variability over days, but we still report an increase in BP with the load carriage.
Figure 2 displays the change values (difference from pre- to post-carry) in peripheral BP, in central BP, in AIx@75, and in SEVR. We found that the zercher carry elicited a larger increase in arterial stiffness (AIx@75) than farmer’s handle carry in both females and males (
p < 0.05 for both). Farmer’s handle carriage elicited a significantly larger change in peripheral systolic BP for males but a larger change in SEVR for females.
We found larger effects in vascular stiffness with zercher carry and larger effects in systolic BP with farmer’s handle carry. For AIx@75 the main effect of carry {λ = 0.76, F(1,37) = 11.16, p < 0.001}, of test time {λ = 0.14, F(1,37) = 213.69, p < 0.001}, and interaction of carry X test time {λ = 0.44, F(1,37) = 46.58, p < 0.001} were significant, but there was no interaction of test, carry, and sex. For peripheral systolic BP the main effect of carry {Wilks’ λ = 0.89, F(1,37) = 4.39, p < 0.05}, of test time {λ = 0.54, F(1,37) = 30.95, p < 0.001}, interaction of carry X test time {λ = 0.83, F(1,37) = 7.35, p < 0.05}, and interaction of test, carry, and sex were all significant. For central systolic BP, only the main effect of test time {λ = 0.27, F(1,37) = 97.03, p < 0.001} was found to be significant. There was no interaction effect found for SEVR.
4. Discussion
We found that a 30 s load carriage exercise with the load in front of the body (zercher) elicits a larger increase in arterial stiffness, and a load carriage exercise with the load on the side of the body (farmer’s handle) elicits larger increase in peripheral systolic BP. We found no sex differences in these responses; both groups had larger increases in arterial stiffness with zercher carry and larger increases in BP with farmer’s handle carry. Our findings have clinical implications because the responses differ based on where the load is carried. The observed changes that we report suggest that both arm and heart BP increase with both types of load carriage. We report an increase in stiffness with both types of load carriage which could be risky for clinical populations who already suffer from vascular disease. Our data suggests that patients with cardiac issues may be at higher risk with weight carried in front of the body, but future studies should be conducted in clinical populations to examine this. These findings also have training implications because the physiological response differs based on the location of the resistance relative to the body. Load carriage is a known risk but has a direct application to activities of daily living and to occupational health; so, future research is needed to examine BP and vascular responses in different populations to zercher- or farmer’s handle-type load carriage.
Recent meta-analyses came to the overall conclusion that resistance training does not increase arterial stiffness in healthy adults [
20] or in adults at risk for CVD [
21], yet it is still important to understand the vascular responses to load carriage. Like our findings, a 2014 study measured arterial stiffness pre- and post-treadmill walking with and without load carriage in 14 young adult males. In their study, the load carried was 10% of the participant’s body weight, which was carried in two water carboys with handles, one in each hand. The participants in their study walked for 10 min on a treadmill with and without the load carriage. The authors reported increases in central and peripheral BP and an increase in AIx@75 with the load [
22]. Our study used a higher relative percentage for the load and a shorter walking duration. Importantly, we report that when weight is carried in front of the body there are larger increases in AIx@75 than when the weight is carried on the side of the body. This could have important clinical implications if creating training programs for patients who have cardiac issues. It is also important to note that postural change may affect the hemodynamic response to load carriage. While this is not the purpose of our study, it could be examined in a future study.
Previous studies using similar load percentages as ours have characterized the biomechanics of the carry and predicted the maximal safe load for carry. The dumbbell suitcase carry is similar to a farmer’s handle but uses dumbbell implements instead of the farmer’s handle barbell. Dumbbell load carriage studies have used as up to 63% body weight [
23]. Holmstrup et al. concluded that around 52% bodyweight for females and 63% bodyweight for males is the maximal safe highest load carriage capacity in a unilateral lift before technical error [
23]. Middleton et al. conducted an experimental study with young adults where the load was a weighted vest and their participants walked for 10 min with no load, with 20% and with 40% body weight loads. They found that increasing load led to slower walking time and altered joint kinematics and kinetics, but they also found no sex-by-load interactions [
24]. These studies did not examine vascular responses or BP levels, but these studies also report no sex differences in the responses. We report no differences in response between male and female adults but did find an interaction effect with peripheral BP. Our data adds to the literature base on BP and vascular responses but suggests that sex-differences should be examined with different protocols.
Acute resistance exercise studies have previously reported an increase in AIx@75. Kingsley et al. had adults complete 30 min of supine quiet control and 30 min of resistance exercise [
25]. The exercise bout consisted of three sets of 10 repetitions of squat, bench press, and deadlift with two minutes of rest between each set. The load was standardized at 75% 1RM per set with a 50% RM warm-up set. Vascular measurements and peripheral and central BP were measured pre- and 10 min-post condition. Kingsley et al. reported no change in peripheral or central BP after exercise but found increases in AIx@75 [
25]. Comparing this to our study, it is important to note the differences between type of exercise and time of post-exercise measurement, but it also shows the risk related to increases in arterial stiffness that occurs with resistance exercise. Our findings could have implications for the current trend to incorporate resistance training programs in clinical exercise physiology settings. Patients with cardiac issues may be at increased risk with resistance training programs that include front bearing weights. In a recent systematic review and meta-analysis, researchers found that in patients with heart failure, resistance training led to improvements in VO2
max and functional capacity, with no damage or stress on cardiac function [
26]. Yet, they did not include vascular stiffness measurements in their studies, so we offer novel findings in a healthy population.
Our study has a few limitations. First, all participants in this study were young healthy adults, so this sample may not be indicative of the general population. Second, the load carriage visits were not randomized or blinded, which could have led to participant familiarization with the carries. Third, it seems clear that the biomechanics would be different based on the positioning of the load carriage. However, the vascular responses and the BP responses to load carriage will not relate to biomechanics. This is something that a future study could address. Fourth, we did not control for menstrual cycle phases, which could have influenced the vascular responses. Finally, the post-load carriage vascular measurement was not repeated; so, one value may not reflect the true response. However, the XCEL system has a validated internal qualification check, which confirmed the quality of each assessment.
In conclusion, load carriage affects BP and vascular stiffness differently based on how the load is carried. Farmer’s handle (side of body) and zercher (front of body) load carriages both led to significant increases in peripheral systolic BP, central systolic BP, and vascular stiffness (AIx@75). Larger increases in peripheral BP were seen with the farmer’s handle load carriage, while larger increases in stiffness were seen in the zercher load carriage. These data suggest that type of load carriage is important to consider and could have implications for the resistance training in clinical exercise physiology settings. Patients with cardiac issues may be at increased risk with resistance training programs that include front bearing weights, but this needs to be examined. Future research is needed to further examine different physiological responses to other types of loaded carry, especially in clinical populations (i.e., elderly or patients with cardiac issues).