Neurocognitive Sequelae and Rehabilitation after Subarachnoid Hemorrhage: Optimizing Outcomes
Abstract
1. Introduction
2. Neuropsychiatric and Neurocognitive Sequelae Following SAH
2.1. Depression
2.2. Anxiety
2.3. PTSD
2.4. Sexual Dysfunction
2.5. Cognitive Dysfunction
3. Rehabilitation after Subarachnoid Hemorrhage in the Acute Setting
3.1. Fluid and Electrolyte Management
3.2. Nutritional Rehabilitation
3.3. Early Mobilization and Cognitive Rehabilitation
3.4. Multidisciplinary Care
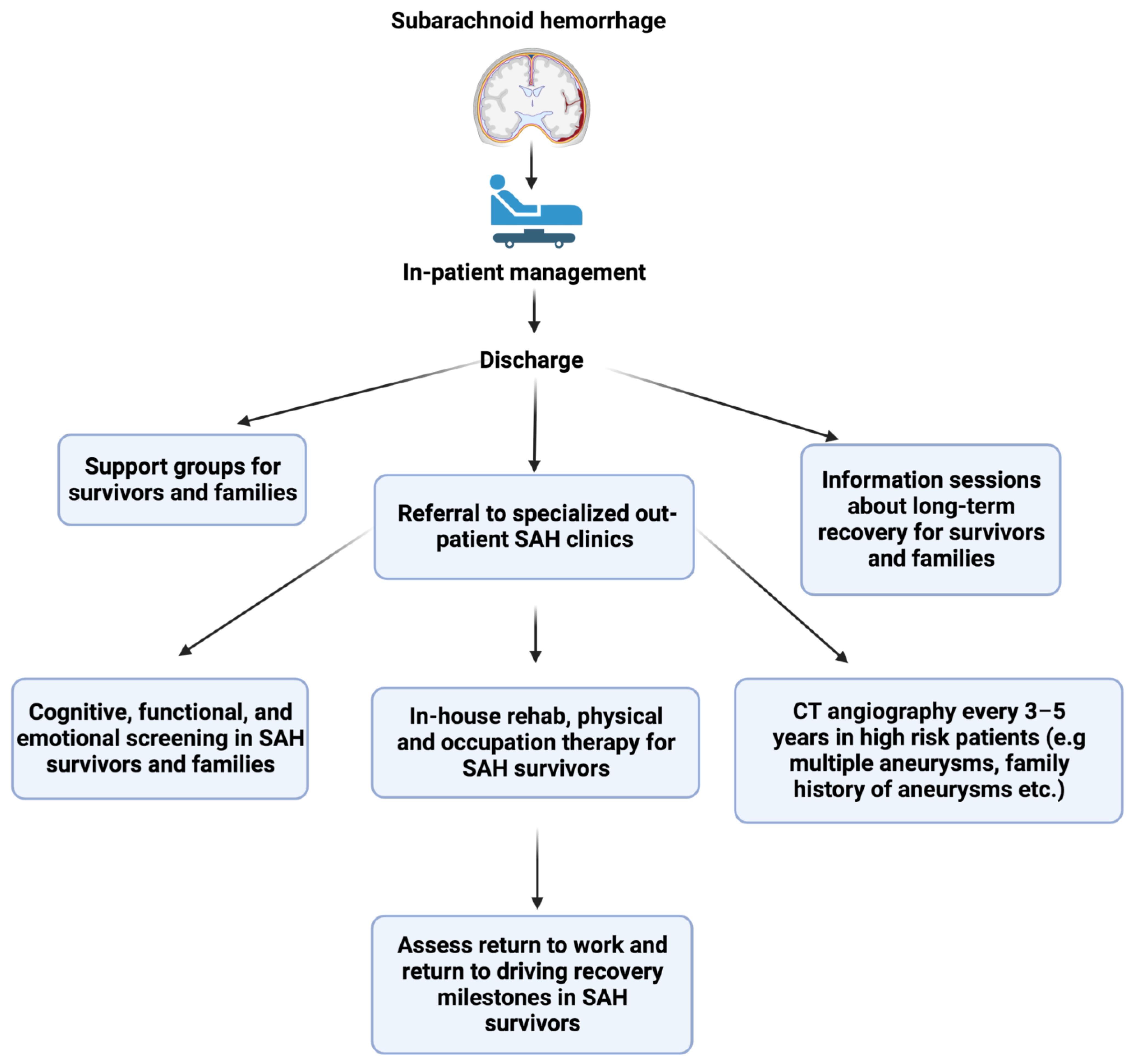
4. Long-Term Rehabilitation Following Subarachnoid Hemorrhage
4.1. Long-Term Outcomes Following SAH
4.2. Determinants of Health Post-SAH
4.3. Novel Rehabilitative Strategies and Future Directions
5. Subarachnoid Hemorrhage Prognostic Biomarkers and Imaging Modalities
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bartlett, M.; Bulters, D.; Hou, R. Psychological distress after subarachnoid haemorrhage: A systematic review and meta-analysis. J. Psychosom. Res. 2021, 148, 110559. [Google Scholar] [CrossRef] [PubMed]
- Benke, T.; Koylu, B.; Delazer, M.; Trinka, E.; Kemmler, G. Cholinergic treatment of amnesia following basal forebrain lesion due to aneurysm rupture--an open-label pilot study. Eur. J. Neurol. 2005, 12, 791–796. [Google Scholar] [CrossRef] [PubMed]
- Powell, J.; Kitchen, N.; Heslin, J.; Greenwood, R. Psychosocial outcomes at three and nine months after good neurological recovery from aneurysmal subarachnoid haemorrhage: Predictors and prognosis. J. Neurol. Neurosurg. Psychiatry 2002, 72, 772–781. [Google Scholar] [CrossRef] [PubMed]
- Epprecht, L.; Messerli, M.; Samuel, R.; Seule, M.; Weber, J.; Fournier, J.Y.; Surbeck, W. Sexual Dysfunction After Good-Grade Aneurysmal Subarachnoid Hemorrhage. World Neurosurg. 2018, 111, e449–e453. [Google Scholar] [CrossRef]
- Al-Khindi, T.; Macdonald, R.L.; Schweizer, T.A. Cognitive and functional outcome after aneurysmal subarachnoid hemorrhage. Stroke 2010, 41, e519–e536. [Google Scholar] [CrossRef]
- Morris, P.G.; Wilson, J.T.; Dunn, L. Anxiety and depression after spontaneous subarachnoid hemorrhage. Neurosurgery 2004, 54, 47–54. [Google Scholar] [CrossRef]
- Catapano, J.S.; Rumalla, K.; Koester, S.W.; Winkler, E.A.; Rudy, R.F.; Cole, T.S.; Baranoski, J.F.; Graffeo, C.S.; Srinivasan, V.M.; Jha, R.P.; et al. Incidence and prediction of chronic depression following aneurysmal subarachnoid hemorrhage: A single-center 17-year experience. World Neurosurg. 2022, 171, e206–e212. [Google Scholar] [CrossRef]
- Tang, W.K.; Wang, L.; Kwok Chu Wong, G.; Ungvari, G.S.; Yasuno, F.; Tsoi, K.K.F.; Kim, J.S. Depression after Subarachnoid Hemorrhage: A Systematic Review. J. Stroke 2020, 22, 11–28. [Google Scholar] [CrossRef]
- Kreiter, K.T.; Rosengart, A.J.; Claassen, J.; Fitzsimmons, B.F.; Peery, S.; Du, Y.E.; Connolly, E.S.; Mayer, S.A. Depressed mood and quality of life after subarachnoid hemorrhage. J. Neurol. Sci. 2013, 335, 64–71. [Google Scholar] [CrossRef]
- von Vogelsang, A.C.; Svensson, M.; Wengstrom, Y.; Forsberg, C. Cognitive, physical, and psychological status after intracranial aneurysm rupture: A cross-sectional study of a Stockholm case series 1996 to 1999. World Neurosurg. 2013, 79, 130–135. [Google Scholar] [CrossRef]
- Al Yassin, A.; Ouyang, B.; Temes, R. Depression and Anxiety Following Aneurysmal Subarachnoid Hemorrhage Are Associated With Higher Six-Month Unemployment Rates. J. Neuropsychiatry Clin. Neurosci. 2017, 29, 67–69. [Google Scholar] [CrossRef] [PubMed]
- Colledge, F.; Brand, S.; Zimmerer, S.; Puhse, U.; Holsboer-Trachsler, E.; Gerber, M. In Individuals Following Aneurysmal Subarachnoid Haemorrhage, Hair Cortisol Concentrations Are Higher and More Strongly Associated with Psychological Functioning and Sleep Complaints than in Healthy Controls. Neuropsychobiology 2017, 75, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Kreitschmann-Andermahr, I.; Poll, E.; Hutter, B.O.; Reineke, A.; Kristes, S.; Gilsbach, J.M.; Saller, B. Quality of life and psychiatric sequelae following aneurysmal subarachnoid haemorrhage: Does neuroendocrine dysfunction play a role? Clin. Endocrinol. 2007, 66, 833–837. [Google Scholar] [CrossRef] [PubMed]
- Vaswani, M.; Linda, F.K.; Ramesh, S. Role of selective serotonin reuptake inhibitors in psychiatric disorders: A comprehensive review. Prog. Neuropsychopharmacol. Biol. Psychiatry 2003, 27, 85–102. [Google Scholar] [CrossRef]
- Renoux, C.; Vahey, S.; Dell’Aniello, S.; Boivin, J.F. Association of Selective Serotonin Reuptake Inhibitors With the Risk for Spontaneous Intracranial Hemorrhage. JAMA Neurol. 2017, 74, 173–180. [Google Scholar] [CrossRef]
- Ackermark, P.Y.; Schepers, V.P.; Post, M.W.; Rinkel, G.J.; Passier, P.E.; Visser-Meily, J.M. Longitudinal course of depressive symptoms and anxiety after aneurysmal subarachnoid hemorrhage. Eur. J. Phys. Rehabil. Med. 2017, 53, 98–104. [Google Scholar] [CrossRef]
- Hedlund, M.; Zetterling, M.; Ronne-Engstrom, E.; Carlsson, M.; Ekselius, L. Depression and post-traumatic stress disorder after aneurysmal subarachnoid haemorrhage in relation to lifetime psychiatric morbidity. Br. J. Neurosurg. 2011, 25, 693–700. [Google Scholar] [CrossRef]
- Visser-Meily, J.M.; Rinkel, G.J.; Vergouwen, M.D.; Passier, P.E.; van Zandvoort, M.J.; Post, M.W. Post-traumatic stress disorder in patients 3 years after aneurysmal subarachnoid haemorrhage. Cerebrovasc. Dis. 2013, 36, 126–130. [Google Scholar] [CrossRef]
- Noble, A.J.; Baisch, S.; Mendelow, A.D.; Allen, L.; Kane, P.; Schenk, T. Posttraumatic stress disorder explains reduced quality of life in subarachnoid hemorrhage patients in both the short and long term. Neurosurgery 2008, 63, 1095–1105. [Google Scholar] [CrossRef]
- Noble, A.J.; Schenk, T. Posttraumatic stress disorder in the family and friends of patients who have suffered spontaneous subarachnoid hemorrhage. J. Neurosurg. 2008, 109, 1027–1033. [Google Scholar] [CrossRef]
- Rueckriegel, S.M.; Baron, M.; Domschke, K.; Neuderth, S.; Kunze, E.; Kessler, A.F.; Nickl, R.; Westermaier, T.; Ernestus, R.I. Trauma- and distress-associated mental illness symptoms in close relatives of patients with severe traumatic brain injury and high-grade subarachnoid hemorrhage. Acta Neurochir. 2015, 157, 1329–1336. [Google Scholar] [CrossRef] [PubMed]
- Baisch, S.B.; Schenk, T.; Noble, A.J. What is the cause of post-traumatic stress disorder following subarachnoid haemorrhage? Post-ictal events are key. Acta Neurochir. 2011, 153, 913–922. [Google Scholar] [CrossRef] [PubMed]
- Noble, A.J.; Baisch, S.; Covey, J.; Mukerji, N.; Nath, F.; Schenk, T. Subarachnoid hemorrhage patients’ fears of recurrence are related to the presence of posttraumatic stress disorder. Neurosurgery 2011, 69, 323–333. [Google Scholar] [CrossRef]
- Rees, P.M.; Fowler, C.J.; Maas, C.P. Sexual function in men and women with neurological disorders. Lancet 2007, 369, 512–525. [Google Scholar] [CrossRef] [PubMed]
- Korpelainen, J.T.; Nieminen, P.; Myllyla, V.V. Sexual functioning among stroke patients and their spouses. Stroke 1999, 30, 715–719. [Google Scholar] [CrossRef]
- Song, H.; Oh, H.; Kim, H.; Seo, W. Effects of a sexual rehabilitation intervention program on stroke patients and their spouses. NeuroRehabilitation 2011, 28, 143–150. [Google Scholar] [CrossRef]
- Monga, T.N.; Lawson, J.S.; Inglis, J. Sexual dysfunction in stroke patients. Arch Phys. Med. Rehabil. 1986, 67, 19–22. [Google Scholar]
- Martin, C.O.; Rymer, M.M. Hemorrhagic stroke: Aneurysmal subarachnoid hemorrhage. Mo Med. 2011, 108, 124–127. [Google Scholar]
- Aimaretti, G.; Ambrosio, M.R.; Di Somma, C.; Fusco, A.; Cannavo, S.; Gasperi, M.; Scaroni, C.; De Marinis, L.; Benvenga, S.; degli Uberti, E.C.; et al. Traumatic brain injury and subarachnoid haemorrhage are conditions at high risk for hypopituitarism: Screening study at 3 months after the brain injury. Clin. Endocrinol. 2004, 61, 320–326. [Google Scholar] [CrossRef]
- Schneider, H.J.; Kreitschmann-Andermahr, I.; Ghigo, E.; Stalla, G.K.; Agha, A. Hypothalamopituitary dysfunction following traumatic brain injury and aneurysmal subarachnoid hemorrhage: A systematic review. JAMA 2007, 298, 1429–1438. [Google Scholar] [CrossRef]
- Nussbaum, E.S.; Mikoff, N.; Paranjape, G.S. Cognitive deficits among patients surviving aneurysmal subarachnoid hemorrhage. A contemporary systematic review. Br. J. Neurosurg. 2021, 35, 384–401. [Google Scholar] [CrossRef] [PubMed]
- Rowland, M.J.; Garry, P.; Ezra, M.; Corkill, R.; Baker, I.; Jezzard, P.; Westbrook, J.; Douaud, G.; Pattinson, K.T.S. Early brain injury and cognitive impairment after aneurysmal subarachnoid haemorrhage. Sci. Rep. 2021, 11, 23245. [Google Scholar] [CrossRef]
- Alfonso, M.; Aftab, S.; Hamadneh, T.; Sherali, N.; Tsouklidis, N. Understanding Cognitive Deficit After Subarachnoid Hemorrhage: A Memory Focused Approach. Cureus 2020, 12, e11513. [Google Scholar] [CrossRef] [PubMed]
- Buunk, A.M.; Spikman, J.M.; Metzemaekers, J.D.M.; van Dijk, J.M.C.; Groen, R.J.M. Return to work after subarachnoid hemorrhage: The influence of cognitive deficits. PLoS ONE 2019, 14, e0220972. [Google Scholar] [CrossRef] [PubMed]
- Passier, P.E.; Visser-Meily, J.M.; van Zandvoort, M.J.; Post, M.W.; Rinkel, G.J.; van Heugten, C. Prevalence and determinants of cognitive complaints after aneurysmal subarachnoid hemorrhage. Cerebrovasc. Dis. 2010, 29, 557–563. [Google Scholar] [CrossRef]
- Shukla, D.P. Outcome and rehabilitation of patients following aneurysmal subarachnoid haemorrhage. J. Neuroanaesth. Crit. Care 2017, 4, S65–S75. [Google Scholar] [CrossRef]
- Dubosh, N.M.; Edlow, J.A. Diagnosis and Initial Emergency Department Management of Subarachnoid Hemorrhage. Emerg. Med. Clin. N. Am. 2021, 39, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Oddo, M.; Poole, D.; Helbok, R.; Meyfroidt, G.; Stocchetti, N.; Bouzat, P.; Cecconi, M.; Geeraerts, T.; Martin-Loeches, I.; Quintard, H.; et al. Fluid therapy in neurointensive care patients: ESICM consensus and clinical practice recommendations. Intensive Care Med. 2018, 44, 449–463. [Google Scholar] [CrossRef]
- van der Jagt, M. Fluid management of the neurological patient: A concise review. Crit. Care 2016, 20, 126. [Google Scholar] [CrossRef]
- Rinkel, G.J.E. Hypervolemia in Aneurysmal Subarachnoid Hemorrhage. Stroke 2005, 36, 1104–1105. [Google Scholar] [CrossRef]
- Ayling, O.G.S.; Ibrahim, G.M.; Alotaibi, N.M.; Gooderham, P.A.; Macdonald, R.L. Anemia After Aneurysmal Subarachnoid Hemorrhage Is Associated With Poor Outcome and Death. Stroke 2018, 49, 1859–1865. [Google Scholar] [CrossRef] [PubMed]
- Marupudi, N.I.; Mittal, S. Diagnosis and Management of Hyponatremia in Patients with Aneurysmal Subarachnoid Hemorrhage. J. Clin. Med. 2015, 4, 756–767. [Google Scholar] [CrossRef] [PubMed]
- Schmutzhard, E.; Rabinstein, A.A. Participants in the International Multi-Disciplinary Consensus Conference on the Critical care Management of Subarachnoid, H. Spontaneous subarachnoid hemorrhage and glucose management. Neurocrit. Care 2011, 15, 281–286. [Google Scholar] [CrossRef]
- Gharaibeh, K.A.; Brewer, J.M.; Agarwal, M.; Fulop, T. Risk factors, complication and measures to prevent or reverse catastrophic sodium overcorrection in chronic hyponatremia. Am. J. Med. Sci. 2015, 349, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Murphy, T.; Dhar, R.; Diringer, M. Conivaptan bolus dosing for the correction of hyponatremia in the neurointensive care unit. Neurocrit. Care 2009, 11, 14–19. [Google Scholar] [CrossRef]
- Singer, P.; Blaser, A.R.; Berger, M.M.; Alhazzani, W.; Calder, P.C.; Casaer, M.P.; Hiesmayr, M.; Mayer, K.; Montejo, J.C.; Pichard, C.; et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin. Nutr. 2019, 38, 48–79. [Google Scholar] [CrossRef]
- Kofler, M.; Beer, R.; Marinoni, S.; Schiefecker, A.J.; Gaasch, M.; Rass, V.; Lindner, A.; Lanosi, B.A.; Rhomberg, P.; Pfausler, B.; et al. Early supplemental parenteral nutrition for the achievement of nutritional goals in subarachnoid hemorrhage patients: An observational cohort study. PLoS ONE 2022, 17, e0265729. [Google Scholar] [CrossRef]
- Badjatia, N.; Fernandez, L.; Schlossberg, M.J.; Schmidt, J.M.; Claassen, J.; Lee, K.; Connolly, E.S.; Mayer, S.A.; Rosenbaum, M. Relationship between energy balance and complications after subarachnoid hemorrhage. J. Parenter. Enter. Nutr. 2010, 34, 64–69. [Google Scholar] [CrossRef]
- Cinotti, R.; Dordonnat-Moynard, A.; Feuillet, F.; Roquilly, A.; Rondeau, N.; Lepelletier, D.; Caillon, J.; Asseray, N.; Blanloeil, Y.; Rozec, B.; et al. Risk factors and pathogens involved in early ventilator-acquired pneumonia in patients with severe subarachnoid hemorrhage. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 823–830. [Google Scholar] [CrossRef]
- Alsharif, D.J.; Alsharif, F.J.; Aljuraiban, G.S.; Abulmeaty, M.M.A. Effect of Supplemental Parenteral Nutrition Versus Enteral Nutrition Alone on Clinical Outcomes in Critically Ill Adult Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2020, 12, 2968. [Google Scholar] [CrossRef]
- Nicolo, M.; Heyland, D.K.; Chittams, J.; Sammarco, T.; Compher, C. Clinical Outcomes Related to Protein Delivery in a Critically Ill Population: A Multicenter, Multinational Observation Study. JPEN J. Parenter Enteral. Nutr. 2016, 40, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Karic, T.; Roe, C.; Nordenmark, T.H.; Becker, F.; Sorteberg, W.; Sorteberg, A. Effect of early mobilization and rehabilitation on complications in aneurysmal subarachnoid hemorrhage. J. Neurosurg. 2017, 126, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Okamura, M.; Konishi, M.; Sagara, A.; Shimizu, Y.; Nakamura, T. Impact of early mobilization on discharge disposition and functional status in patients with subarachnoid hemorrhage: A retrospective cohort study. Medicine 2021, 100, e28171. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, J.; Langhorne, P.; Lindley, R.I.; Thrift, A.G.; Ellery, F.; Collier, J.; Moodie, M.; Dewey, H.; Donnan, G. Efficacy and safety of very early mobilisation within 24 h of stroke onset (AVERT): A randomised controlled trial. Lancet 2015, 386, 46–55. [Google Scholar] [CrossRef]
- Haug Nordenmark, T.; Karic, T.; Sorteberg, W.; Sorteberg, A. Predictors of cognitive function in the acute phase after aneurysmal subarachnoid hemorrhage. Acta Neurochir. 2019, 161, 177–184. [Google Scholar] [CrossRef]
- Milovanovic, A.; Grujicic, D.; Bogosavljevic, V.; Jokovic, M.; Mujovic, N.; Markovic, I.P. Efficacy of Early Rehabilitation After Surgical Repair of Acute Aneurysmal Subarachnoid Hemorrhage: Outcomes After Verticalization on Days 2-5 Versus Day 12 Post-Bleeding. Turk Neurosurg. 2017, 27, 867–873. [Google Scholar] [CrossRef]
- Chen, B.Y. Early tablet-assisted cognitive rehabilitation for aneurysmal subarachnoid hemorrhage: Feasibility of a single-center randomized controlled trial. Neurology 2018, 90, P3.227. [Google Scholar]
- Burrows, A.M.; Korumilli, R.; Lanzino, G. How we do it: Acute management of subarachnoid hemorrhage. Neurol. Res. 2013, 35, 111–116. [Google Scholar] [CrossRef]
- Norberg, E.; Odenstedt-Herges, H.; Rydenhag, B.; Oras, J. Impact of Acute Cardiac Complications After Subarachnoid Hemorrhage on Long-Term Mortality and Cardiovascular Events. Neurocrit. Care 2018, 29, 404–412. [Google Scholar] [CrossRef]
- Mesotten, D.; Preiser, J.C.; Kosiborod, M. Glucose management in critically ill adults and children. Lancet Diabetes Endocrinol. 2015, 3, 723–733. [Google Scholar] [CrossRef]
- Rawal, G.; Kumar, R.; Yadav, S.; Singh, A. Anemia in Intensive Care: A Review of Current Concepts. J. Crit. Care Med. 2016, 2, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Askenazi, D.J.; Heung, M.; Connor, M.J., Jr.; Basu, R.K.; Cerda, J.; Doi, K.; Koyner, J.L.; Bihorac, A.; Golestaneh, L.; Vijayan, A.; et al. Optimal Role of the Nephrologist in the Intensive Care Unit. Blood Purif. 2017, 43, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Terblanche, E. The role of dietitians in critical care. J. Intensive Care Soc. 2019, 20, 255–257. [Google Scholar] [CrossRef] [PubMed]
- Moheet, A.M.; Livesay, S.L.; Abdelhak, T.; Bleck, T.P.; Human, T.; Karanjia, N.; Lamer-Rosen, A.; Medow, J.; Nyquist, P.A.; Rosengart, A.; et al. Standards for Neurologic Critical Care Units: A Statement for Healthcare Professionals from The Neurocritical Care Society. Neurocrit. Care 2018, 29, 145–160. [Google Scholar] [CrossRef]
- Dodd, J.N.; Hall, T.A.; Guilliams, K.; Guerriero, R.M.; Wagner, A.; Malone, S.; Williams, C.N.; Hartman, M.E.; Piantino, J. Optimizing Neurocritical Care Follow-Up Through the Integration of Neuropsychology. Pediatr. Neurol. 2018, 89, 58–62. [Google Scholar] [CrossRef]
- Olkowski, B. Early Mobilization in Aneurysmal Subarachnoid Hemorrhage Accelerates Recovery and Reduces Length of Stay. J. Acute Care Phys. Ther. 2015, 6, 47–55. [Google Scholar] [CrossRef]
- Diringer, M.N.; Bleck, T.P.; Claude Hemphill, J., 3rd; Menon, D.; Shutter, L.; Vespa, P.; Bruder, N.; Connolly, E.S., Jr.; Citerio, G.; Gress, D.; et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: Recommendations from the Neurocritical Care Society’s Multidisciplinary Consensus Conference. Neurocrit. Care 2011, 15, 211–240. [Google Scholar] [CrossRef] [PubMed]
- Rabinstein, A.A.; Lanzino, G.; Wijdicks, E.F. Multidisciplinary management and emerging therapeutic strategies in aneurysmal subarachnoid haemorrhage. Lancet Neurol. 2010, 9, 504–519. [Google Scholar] [CrossRef]
- Samuels, O.; Webb, A.; Culler, S.; Martin, K.; Barrow, D. Impact of a dedicated neurocritical care team in treating patients with aneurysmal subarachnoid hemorrhage. Neurocrit. Care 2011, 14, 334–340. [Google Scholar] [CrossRef]
- Lovelock, C.E.; Rinkel, G.J.; Rothwell, P.M. Time trends in outcome of subarachnoid hemorrhage: Population-based study and systematic review. Neurology 2010, 74, 1494–1501. [Google Scholar] [CrossRef]
- Taufique, Z.; May, T.; Meyers, E.; Falo, C.; Mayer, S.A.; Agarwal, S.; Park, S.; Connolly, E.S.; Claassen, J.; Schmidt, J.M. Predictors of Poor Quality of Life 1 Year After Subarachnoid Hemorrhage. Neurosurgery 2016, 78, 256–264. [Google Scholar] [CrossRef]
- Nieuwkamp, D.J.; Setz, L.E.; Algra, A.; Linn, F.H.; de Rooij, N.K.; Rinkel, G.J. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: A meta-analysis. Lancet Neurol. 2009, 8, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Sonesson, B.; Kronvall, E.; Saveland, H.; Brandt, L.; Nilsson, O.G. Long-term reintegration and quality of life in patients with subarachnoid hemorrhage and a good neurological outcome: Findings after more than 20 years. J. Neurosurg. 2018, 128, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Persson, H.C.; Tornbom, K.; Sunnerhagen, K.S.; Tornbom, M. Consequences and coping strategies six years after a subarachnoid hemorrhage - A qualitative study. PLoS ONE 2017, 12, e0181006. [Google Scholar] [CrossRef] [PubMed]
- Passier, P.E.; Visser-Meily, J.M.; Rinkel, G.J.; Lindeman, E.; Post, M.W. Determinants of health-related quality of life after aneurysmal subarachnoid hemorrhage: A systematic review. Qual. Life Res. 2013, 22, 1027–1043. [Google Scholar] [CrossRef]
- Visser-Meily, J.M.; Rhebergen, M.L.; Rinkel, G.J.; van Zandvoort, M.J.; Post, M.W. Long-term health-related quality of life after aneurysmal subarachnoid hemorrhage: Relationship with psychological symptoms and personality characteristics. Stroke 2009, 40, 1526–1529. [Google Scholar] [CrossRef]
- von Vogelsang, A.C.; Forsberg, C.; Svensson, M.; Wengstrom, Y. Patients Experience High Levels of Anxiety 2 Years Following Aneurysmal Subarachnoid Hemorrhage. World Neurosurg. 2015, 83, 1090–1097. [Google Scholar] [CrossRef]
- Lai, P.M.R.; Du, R. Return to Driving Is a Better Predictor of Patient Outcome Than Return to Work After Aneurysmal Subarachnoid Hemorrhage. World Neurosurg. 2020, 144, e285–e295. [Google Scholar] [CrossRef]
- Passier, P.E.; Visser-Meily, J.M.; Rinkel, G.J.; Lindeman, E.; Post, M.W. Life satisfaction and return to work after aneurysmal subarachnoid hemorrhage. J. Stroke Cerebrovasc. Dis. 2011, 20, 324–329. [Google Scholar] [CrossRef]
- Fertl, E.; Killer, M.; Eder, H.; Linzmayer, L.; Richling, B.; Auff, E. Long-term functional effects of aneurysmal subarachnoid haemorrhage with special emphasis on the patient’s view. Acta Neurochir. 1999, 141, 571–577. [Google Scholar] [CrossRef]
- Vetkas, A.; Lepik, T.; Eilat, T.; Ratsep, T.; Asser, T. Emotional health and quality of life after aneurysmal subarachnoid hemorrhage. Acta Neurochir. 2013, 155, 1107–1114. [Google Scholar] [CrossRef]
- Buunk, A.M.; Groen, R.J.; Veenstra, W.S.; Spikman, J.M. Leisure and social participation in patients 4-10 years after aneurysmal subarachnoid haemorrhage. Brain Inj. 2015, 29, 1589–1596. [Google Scholar] [CrossRef] [PubMed]
- Turi, E.R.; Conley, Y.; Crago, E.; Sherwood, P.; Poloyac, S.M.; Ren, D.; Stanfill, A.G. Psychosocial Comorbidities Related to Return to Work Rates Following Aneurysmal Subarachnoid Hemorrhage. J. Occup. Rehabil. 2019, 29, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Hop, J.W.; Rinkel, G.J.; Algra, A.; van Gijn, J. Quality of life in patients and partners after aneurysmal subarachnoid hemorrhage. Stroke 1998, 29, 798–804. [Google Scholar] [CrossRef] [PubMed]
- Covey, J.; Noble, A.J.; Schenk, T. Family and friends’ fears of recurrence: Impact on the patient’s recovery after subarachnoid hemorrhage. J. Neurosurg. 2013, 119, 948–954. [Google Scholar] [CrossRef] [PubMed]
- Noble, A.J.; Schenk, T. Psychological distress after subarachnoid hemorrhage: Patient support groups can help us better detect it. J. Neurol. Sci. 2014, 343, 125–131. [Google Scholar] [CrossRef]
- Wang, Y.; Gao, Y.; Lu, M.; Liu, Y. Long-term functional prognosis of patients with aneurysmal subarachnoid hemorrhage treated with rehabilitation combined with hyperbaric oxygen: Case-series study. Medicine 2020, 99, e18748. [Google Scholar] [CrossRef]
- Malinova, V.; Bleuel, K.; Stadelmann, C.; Iliev, B.; Tsogkas, I.; Psychogios, M.N.; Rohde, V.; Mielke, D. The impact of transcranial direct current stimulation on cerebral vasospasm in a rat model of subarachnoid hemorrhage. J. Cereb. Blood Flow Metab. 2021, 41, 2000–2009. [Google Scholar] [CrossRef]
- Shah, K.A.; White, T.G.; Powell, K.; Woo, H.H.; Narayan, R.K.; Li, C. Trigeminal Nerve Stimulation Improves Cerebral Macrocirculation and Microcirculation After Subarachnoid Hemorrhage: An Exploratory Study. Neurosurgery 2022, 90, 485–494. [Google Scholar] [CrossRef]
- ter Laan, M.; van Dijk, J.M.; Stewart, R.; Staal, M.J.; Elting, J.W. Modulation of cerebral blood flow with transcutaneous electrical neurostimulation (TENS) in patients with cerebral vasospasm after subarachnoid hemorrhage. Neuromodulation 2014, 17, 431–436. [Google Scholar] [CrossRef]
- Tonomura, T.; Satow, T.; Hyuga, Y.; Mima, T. Use of transcranial direct current stimulation in poststroke postural imbalance. BMJ Case Rep. 2021, 14. [Google Scholar] [CrossRef] [PubMed]
- Rinkel, G.J.; Algra, A. Long-term outcomes of patients with aneurysmal subarachnoid haemorrhage. Lancet Neurol. 2011, 10, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Harmsen, W.J.; Ribbers, G.M.; Heijenbrok-Kal, M.H.; Khajeh, L.; Sneekes, E.M.; van Kooten, F.; Neggers, S.; van den Berg-Emons, R.J. Fatigue After Aneurysmal Subarachnoid Hemorrhage Is Highly Prevalent in the First-Year Postonset and Related to Low Physical Fitness: A Longitudinal Study. Am. J. Phys. Med. Rehabil. 2019, 98, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Hong, C.M.; Tosun, C.; Kurland, D.B.; Gerzanich, V.; Schreibman, D.; Simard, J.M. Biomarkers as outcome predictors in subarachnoid hemorrhage--a systematic review. Biomarkers 2014, 19, 95–108. [Google Scholar] [CrossRef]
- Kedziora, J.; Burzynska, M.; Gozdzik, W.; Kubler, A.; Kobylinska, K.; Adamik, B. Biomarkers of Neurological Outcome After Aneurysmal Subarachnoid Hemorrhage as Early Predictors at Discharge from an Intensive Care Unit. Neurocrit. Care 2021, 34, 856–866. [Google Scholar] [CrossRef]
- Kedziora, J.; Burzynska, M.; Gozdzik, W.; Kubler, A.; Uryga, A.; Kasprowicz, M.; Adamik, B. Brain-Specific Biomarkers as Mortality Predictors after Aneurysmal Subarachnoid Haemorrhage. J. Clin. Med. 2020, 9, 4117. [Google Scholar] [CrossRef]
- Oertel, M.; Schumacher, U.; McArthur, D.L.; Kastner, S.; Boker, D.K. S-100B and NSE: Markers of initial impact of subarachnoid haemorrhage and their relation to vasospasm and outcome. J. Clin. Neurosci. 2006, 13, 834–840. [Google Scholar] [CrossRef]
- Tawk, R.G.; Grewal, S.S.; Heckman, M.G.; Rawal, B.; Miller, D.A.; Edmonston, D.; Ferguson, J.L.; Navarro, R.; Ng, L.; Brown, B.L.; et al. The Relationship Between Serum Neuron-Specific Enolase Levels and Severity of Bleeding and Functional Outcomes in Patients With Nontraumatic Subarachnoid Hemorrhage. Neurosurgery 2016, 78, 487–491. [Google Scholar] [CrossRef]
- Gyldenholm, T.; Hvas, C.L.; Hvas, A.M.; Hviid, C.V.B. Serum glial fibrillary acidic protein (GFAP) predicts outcome after intracerebral and subarachnoid hemorrhage. Neurol. Sci. 2022, 43, 6011–6019. [Google Scholar] [CrossRef]
- Katsanos, A.H.; Makris, K.; Stefani, D.; Koniari, K.; Gialouri, E.; Lelekis, M.; Chondrogianni, M.; Zompola, C.; Dardiotis, E.; Rizos, I.; et al. Plasma Glial Fibrillary Acidic Protein in the Differential Diagnosis of Intracerebral Hemorrhage. Stroke 2017, 48, 2586–2588. [Google Scholar] [CrossRef]
- Helbok, R.; Schiefecker, A.; Delazer, M.; Beer, R.; Bodner, T.; Pfausler, B.; Benke, T.; Lackner, P.; Fischer, M.; Sohm, F.; et al. Cerebral tau is elevated after aneurysmal subarachnoid haemorrhage and associated with brain metabolic distress and poor functional and cognitive long-term outcome. J. Neurol. Neurosurg. Psychiatry 2015, 86, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Zanier, E.R.; Refai, D.; Zipfel, G.J.; Zoerle, T.; Longhi, L.; Esparza, T.J.; Spinner, M.L.; Bateman, R.J.; Brody, D.L.; Stocchetti, N. Neurofilament light chain levels in ventricular cerebrospinal fluid after acute aneurysmal subarachnoid haemorrhage. J. Neurol. Neurosurg. Psychiatry 2011, 82, 157–159. [Google Scholar] [CrossRef] [PubMed]
- Garland, P.; Morton, M.; Zolnourian, A.; Durnford, A.; Gaastra, B.; Toombs, J.; Heslegrave, A.J.; More, J.; Zetterberg, H.; Bulters, D.O.; et al. Neurofilament light predicts neurological outcome after subarachnoid haemorrhage. Brain 2021, 144, 761–768. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S.B.; Wolper, R.; Chi, Y.Y.; Miralia, L.; Wang, Y.; Yang, C.; Shaw, G. Identification and preliminary characterization of ubiquitin C terminal hydrolase 1 (UCHL1) as a biomarker of neuronal loss in aneurysmal subarachnoid hemorrhage. J. Neurosci. Res. 2010, 88, 1475–1484. [Google Scholar] [CrossRef]
- Bsat, S.; Chanbour, H.; Bsat, A.; Alomari, S.; Moussalem, C.; Houshiemy, M.N.E.; Omeis, I. Clinical utility of degradomics as predictors of complications and clinical outcome in aneurysmal subarachnoid hemorrhage. J. Integr. Neurosci. 2021, 20, 489–497. [Google Scholar] [CrossRef]
- Joswig, H.; Korte, W.; Fruh, S.; Epprecht, L.; Hildebrandt, G.; Fournier, J.Y.; Stienen, M.N. Neurodegenerative cerebrospinal fluid biomarkers tau and amyloid beta predict functional, quality of life, and neuropsychological outcomes after aneurysmal subarachnoid hemorrhage. Neurosurg. Rev. 2018, 41, 605–614. [Google Scholar] [CrossRef]
- Kay, A.; Petzold, A.; Kerr, M.; Keir, G.; Thompson, E.; Nicoll, J. Temporal alterations in cerebrospinal fluid amyloid beta-protein and apolipoprotein E after subarachnoid hemorrhage. Stroke 2003, 34, e240–e243. [Google Scholar] [CrossRef]
- Kay, A.; Petzold, A.; Kerr, M.; Keir, G.; Thompson, E.; Nicoll, J. Decreased cerebrospinal fluid apolipoprotein E after subarachnoid hemorrhage: Correlation with injury severity and clinical outcome. Stroke 2003, 34, 637–642. [Google Scholar] [CrossRef]
- Fragata, I.; Alves, M.; Papoila, A.L.; Ferreira, P.; Nunes, A.P.; Moreira, N.C.; Canhao, P. Prediction of clinical outcome in subacute subarachnoid hemorrhage using diffusion tensor imaging. J. Neurosurg. 2018, 1–9. [Google Scholar] [CrossRef]
- Abdel-Tawab, M. Prognostic factors of delayed cerebral ischemia after subarachnoid hemorrhage including CT perfusion: A prospective cohort study. Egypt. J. Radiol. Nucl. Med. 2020, 51, 61. [Google Scholar] [CrossRef]
- Wermer, M.J.; Koffijberg, H.; van der Schaaf, I.C.; Group, A.S. Effectiveness and costs of screening for aneurysms every 5 years after subarachnoid hemorrhage. Neurology 2008, 70, 2053–2062. [Google Scholar] [CrossRef] [PubMed]
- van Heuven, A.W.; Dorhout Mees, S.M.; Algra, A.; Rinkel, G.J. Validation of a prognostic subarachnoid hemorrhage grading scale derived directly from the Glasgow Coma Scale. Stroke 2008, 39, 1347–1348. [Google Scholar] [CrossRef] [PubMed]
- Rosen, D.S.; Macdonald, R.L. Subarachnoid hemorrhage grading scales: A systematic review. Neurocrit. Care 2005, 2, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Oshiro, E.M.; Walter, K.A.; Piantadosi, S.; Witham, T.F.; Tamargo, R.J. A new subarachnoid hemorrhage grading system based on the Glasgow Coma Scale: A comparison with the Hunt and Hess and World Federation of Neurological Surgeons Scales in a clinical series. Neurosurgery 1997, 41, 140–147; discussion 147–148. [Google Scholar] [CrossRef]
- Claassen, J.; Bernardini, G.L.; Kreiter, K.; Bates, J.; Du, Y.E.; Copeland, D.; Connolly, E.S.; Mayer, S.A. Effect of cisternal and ventricular blood on risk of delayed cerebral ischemia after subarachnoid hemorrhage: The Fisher scale revisited. Stroke 2001, 32, 2012–2020. [Google Scholar] [CrossRef]
- de Oliveira Manoel, A.L.; Jaja, B.N.; Germans, M.R.; Yan, H.; Qian, W.; Kouzmina, E.; Marotta, T.R.; Turkel-Parrella, D.; Schweizer, T.A.; Macdonald, R.L.; et al. The VASOGRADE: A Simple Grading Scale for Prediction of Delayed Cerebral Ischemia After Subarachnoid Hemorrhage. Stroke 2015, 46, 1826–1831. [Google Scholar] [CrossRef]
- Ogilvy, C.S.; Carter, B.S. A proposed comprehensive grading system to predict outcome for surgical management of intracranial aneurysms. Neurosurgery 1998, 42, 959–968. [Google Scholar] [CrossRef]
- Shen, J.; Yu, J.; Huang, S.; Mungur, R.; Huang, K.; Pan, X.; Yu, G.; Xie, Z.; Zhou, L.; Liu, Z.; et al. Scoring Model to Predict Functional Outcome in Poor-Grade Aneurysmal Subarachnoid Hemorrhage. Front. Neurol. 2021, 12, 601996. [Google Scholar] [CrossRef]
- Li, R.; Lin, F.; Chen, Y.; Lu, J.; Han, H.; Ma, L.; Zhao, Y.; Yan, D.; Li, R.; Yang, J.; et al. A 90-Day Prognostic Model Based on the Early Brain Injury Indicators after Aneurysmal Subarachnoid Hemorrhage: The TAPS Score. Transl. Stroke Res. 2022. [Google Scholar] [CrossRef]
| Biomarker | Comments | Study References |
|---|---|---|
| S100B | Increased; correlated to poorer outcomes in the acute setting. | [95,96] |
| NSE | Increased; correlated to poorer outcomes such as increased mortality and vasospasm. | [97,98] |
| GFAP | Increased; correlated to higher mortality and poor functional outcomes. | [99,100] |
| MAPT | Increased; correlated to poorer outcomes in the acute setting, increased hypoxic brain injury, and poor functional outcomes at 12 months. | [95,101] |
| NF-L | Increased; correlated to early cerebral ischemia and poor neurological outcome at 6 months. | [102,103] |
| UCHL1 | Increased; sub-acute period correlated with increased neuronal loss and poorer outcomes. | [104,105] |
| Amyloid-B-protein | Decreased; correlated to poorer long-term functional outcomes. | [106,107] |
| ApoE | Decreased; correlated to increased inflammation and poorer outcomes. | [107,108] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nwafor, D.C.; Kirby, B.D.; Ralston, J.D.; Colantonio, M.A.; Ibekwe, E.; Lucke-Wold, B. Neurocognitive Sequelae and Rehabilitation after Subarachnoid Hemorrhage: Optimizing Outcomes. J. Vasc. Dis. 2023, 2, 197-211. https://doi.org/10.3390/jvd2020014
Nwafor DC, Kirby BD, Ralston JD, Colantonio MA, Ibekwe E, Lucke-Wold B. Neurocognitive Sequelae and Rehabilitation after Subarachnoid Hemorrhage: Optimizing Outcomes. Journal of Vascular Diseases. 2023; 2(2):197-211. https://doi.org/10.3390/jvd2020014
Chicago/Turabian StyleNwafor, Divine C., Brandon D. Kirby, Jacob D. Ralston, Mark A. Colantonio, Elochukwu Ibekwe, and Brandon Lucke-Wold. 2023. "Neurocognitive Sequelae and Rehabilitation after Subarachnoid Hemorrhage: Optimizing Outcomes" Journal of Vascular Diseases 2, no. 2: 197-211. https://doi.org/10.3390/jvd2020014
APA StyleNwafor, D. C., Kirby, B. D., Ralston, J. D., Colantonio, M. A., Ibekwe, E., & Lucke-Wold, B. (2023). Neurocognitive Sequelae and Rehabilitation after Subarachnoid Hemorrhage: Optimizing Outcomes. Journal of Vascular Diseases, 2(2), 197-211. https://doi.org/10.3390/jvd2020014







