Abstract
Both occlusion and pseudoaneurysm are complications of femoropopliteal bypass surgery. Open revision is the gold standard, but it is associated with high morbidity and mortality compared with endovascular treatment. Percutaneous stent-graft repair is a valid option either for recovering the patency of occluded prosthetic femoropopliteal bypass or for excluding anastomotic pseudoaneurysm. In this report, it is presented a case of occlusion concomitant to a pseudoaneurysm of the distal anastomosis in a previous prosthetic femoropopliteal bypass; a simultaneous endovascular treatment of both complications has been performed through self-expanding stent-graft (Viabahn) placement.
1. Introduction
A femoropopliteal (FP) bypass graft is one of the surgical options for the treatment of long superficial femoral artery occlusion. However, maintaining patency has always been difficult for failing FP bypass graft, especially in patients with occlusion and lack of collaterals; the mainstay of treatment is open surgical repair including redo bypass and patch angioplasty, burdened by high morbidity and mortality, with higher rates of complications such as nerve injury, wound and graft infection, and bleeding compared with endovascular treatment [1].
Pseudoaneurysm (PA) following vascular reconstruction is another possible complication of bypass surgery with a reported incidence of up to 7% [2]. Surgical management of PA consists of resection of the initial graft with reimplantation of a new bypass either into the original arteriotomy or to a more distal target. While this procedure has a high success rate, a secondary open surgical procedure still poses a higher risk than a primary operation, and re-exploration can be difficult due to anatomical distortion and postoperative scarring. For this reason, open surgical repair of anastomotic PA is related to higher perioperative morbidity and mortality rates as compared with primary surgery, and endovascular exclusion of PA has become an attractive and valuable alternative treatment [2,3,4,5].
In this report, an endovascular repair, consisting of the placement of self-expanding stent grafts, is presented to simultaneously treat the occlusion of a prosthetic FP bypass and the PA, due to dehiscence of the distal anastomosis.
2. Case Report
A 77-years-old Southern European Caucasian male smoker with vascular claudication presented to our department. He had a past medical history of obesity, dyslipidaemia, hypertension and peripheral arterial disease (PAD). Approximately 15 years before, a left-sided FP bypass with ePTFE graft was conducted to treat chronic limb-threatening ischemia. The patient underwent, as usual, a follow-up by sonography at 1, 3, 6, 12 months; the exams confirmed the patency of the bypass, without claudication.
On clinical examination, he had leg pain and swelling. There was no presence of motor or sensory deficits. Rutherford classification Grade II, Category 4, with AP < 38 mmHg. The angio-CT scan of the abdomen and lower limbs revealed that the iliac artery, common femoral artery and deep femoral artery of the left side were atheromasic but patent, whereas the FP bypass was completely occluded (Figure 1). At distal anastomosis, a PA which measured 31 × 38 × 55 mm was present (Figure 2a–c). The left popliteal artery was revascularized by collateral vessels coming from the deep femoral artery. On the right side, there was regular patency of the leg arteries.

Figure 1.
Three-dimensional reconstruction image from angio-CT scan. It shows complete occlusion of FP bypass on the left side; iliac artery, common femoral artery and deep femoral artery of left side are atheromasic but patent.
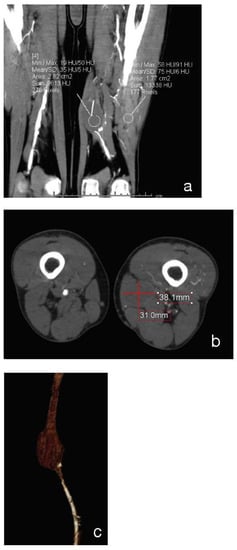
Figure 2.
Coronal (a), Axial (b) and 3D-reconstruction (c) show the occlusion of distal anastomotic PA.
Due to the patient’s comorbidities and the oral antiplatelet therapy failure, the decision was made to solve the occlusion and repair the PA via an endovascular approach. Randomized-controlled trials regarding treatment of CLTI based on occluded femoropopliteal bypass are lacking; however, studies on redo bypass surgery in CLTI patients show more postoperative complications, as well as higher rates of re-intervention and amputation when compared to patients with no history of ipsilateral arterial procedures. In order to avoid redo surgery in these patients with chronically occluded bypasses, endovascular treatment can be considered a good alternative [5,6,7].
It was decided to proceed with a US-guided approach via the right common femoral artery with 6 Fr introducer sheath after local anaesthesia (Lidocaine Hydrochloride 2%) and systemic heparinization (5000 UI). A preliminary angiogram through the introducer sheath confirmed CT findings and highlighted the widespread atheroma of the common iliac-femoral axis and medium-grade stenosis in the external iliac artery. The right-left crossover was performed with a 6 Fr 45 cm introducer sheath conveyed into the left common iliac artery. A left lower extremity arteriogram confirmed the occlusion of the FP bypass with blood supply rehabilitated in the popliteal artery (Figure 3a,b). The peroneal artery was patent and the tibial arteries were not opacified.
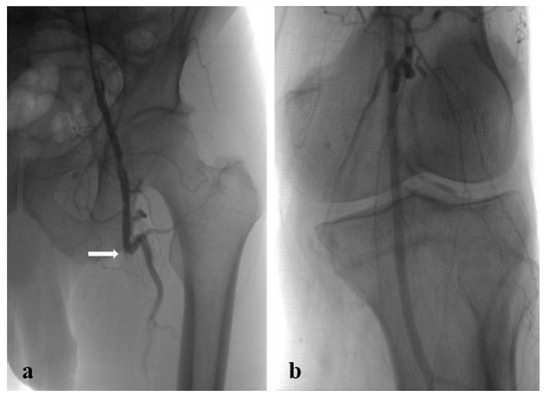
Figure 3.
Preoperative angiograms: (a) occluded prosthetic FB bypass (white arrow: proximal anastomosis); (b) popliteal artery revascularized by collateral vessels.
The bypass occlusion was crossed using a 0.018″ guidewire ASAHI Gladius (Asahi Intecc, Nagoya-Japan) and a pre-dilation was performed with a 4 mm PTA catheter Ultraverse (Becton, Dickinson and Company, Franklin Lakes, NJ, USA) at the distal portion and a 6 mm PTA catheter Dorado (Becton, Dickinson and Company, Franklin Lakes, NJ, USA) at the proximal portion of the lesion. A 6 × 250 mm self-expanding stent-graft Viabahn (W.L. Gore & Associates, Flagstaff, AZ, USA) was placed, and imbricated with another 6 × 150 mm Viabahn stent graft. A post-dilation was performed with the same approach as pre-dilation.
The completion arteriogram showed the resolution of the occlusion with the direct and increased distal flow without any complications (Figure 4a–d). Successful haemostasis with FemoSeal (Terumo Europe) was obtained. The stent graft has adapted perfectly to the morphology of the lesions to be treated. The popliteal artery was reperfused to the third proximal through the collateral vessel; the vessel did not show significant atheromatous plaques. After treatment, the patient underwent therapy with clopidogrel (75 mg) + ASA (100 mg) for 2 months; next with only ASA (100 mg). Color Doppler Ultrasound after 1-3-6-9-12 months from the procedure showed patent self-expanding stent graft inside the excluded PA (Figure 5).
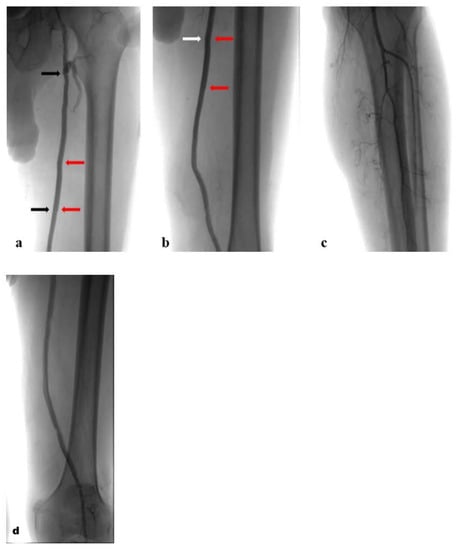
Figure 4.
Postoperative angiograms with self-expanding stent grafts inside the prosthetic FB bypass: (a). proximal stent graft (black arrows) and overlap (red arrows); (b). overlap (red arrows) and distal stent graft (white arrows); (c,d). run-off.
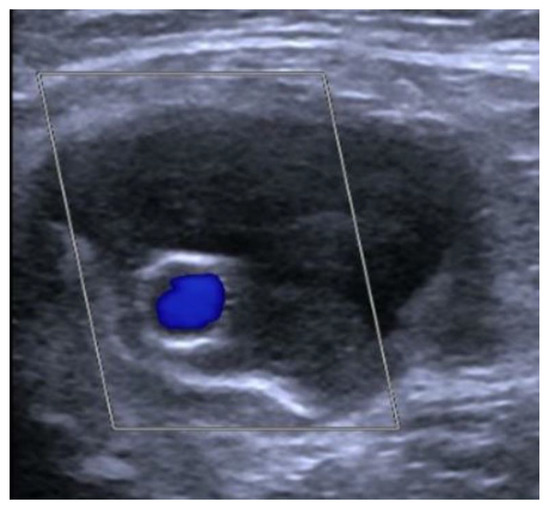
Figure 5.
Color Doppler Ultrasound: patent stent graft inside the excluded distal anastomotic PA.
3. Discussion
FP bypass represents one of the chief treatment modalities for PAD and the use of ePTFE is claimed to be as efficient as the use of autologous saphenous vein. Despite improving techniques, graft occlusion accounts for most bypass failures and a substantial incidence of reocclusion after FP bypass with ePTFE has been reported. Prosthetic graft occlusion has several related causes, including technical failure at implantation, progression of vascular disease, intimal hyperplasia at the anastomosis between the graft and vessel, and thrombosis [6,7]. There have been several strategies to manage occluded bypass grafts and, among those, surgical revision is generally considered the gold standard treatment and provides superior patency when compared to endovascular treatments. Open surgical bypass can have limitations, including postoperative morbidity/wound complications of 10%–20% and prolonged length of hospital stay and outpatient care. A study by Taha et al. concluded that the amputation rates are comparable between endovascular techniques and open techniques in bypass occlusion. In their report, overall mortality rates were significantly higher at 30 days and 1 year in the patients requiring open intervention [1]. Studies on redo bypass surgery in CLTI patients show more postoperative complications, as well as higher rates of re-intervention and amputation when compared to patients with no history of ipsilateral arterial procedures [5,6].
Some of the endovascular methods, including balloon angioplasty, cutting balloon and catheter-based thrombolysis have been reported but they appear to be associated with frequent reinterventions, suggesting these endovascular methods may not be durable. Another possible endovascular strategy that may be considered as a potential treatment option before surgical reintervention is the stent-graft placement inside the occluded FP bypass graft. About that, self-expanding stent graft has reported excellent results in treating complex long superficial femoral artery lesions, showing superiority even with in-stent restenosis, which is one of the toughest lesions for the endovascular treatment; placing self-expanding stent graft in the occluded bypass graft could minimize the effect of residual thrombus inside the bypass graft and solve the recurrent stenosis which usually occurs at the distal anastomosis [8]. A self-expanding stent graft offers optimal flexibility and conformability, that allow the stent to adapt perfectly to the morphology of the lesions to be treated. Some cases of revascularization of occluded femoro-poplliteal by-pass, with stent graft, have been published; also some cases of stent graft repair of anastomotic pseudoaneurysm of femoral-popliteal bypass. To our knowledge, a case of both occlusion and pseudoaneurysm is never been published.
Anastomotic PAs occur in association with prosthetic vascular reconstructions when there is dehiscence at the anastomosis of the graft material and the native artery. This defect may lead to a hematoma that evolves into a fibrous capsule that functions as a portion of the artery wall. Complications from PA include thrombosis with occlusion of the outflow vessels, or embolization from the thrombus within the aneurysm while rupture rarely occurs. The identification and resolution of this kind of lesion are aided by advanced imaging techniques, proper operative planning and patient-specific treatment options and the standard of care is early intervention with interposition graft placement as the treatment of choice. Although stenting of PA has been reported in the literature for over a decade, reports of endoluminal stent-graft placement to treat PA of infra-inguinal bypass grafts are few. Anyhow, with the advent of endovascular therapy, stent-graft placement is gaining popularity as a minimally invasive therapeutic alternative to open surgery, especially in patients with multiple comorbidities, deemed high risk for cardiac events during surgery, for which therefore an endovascular approach may be a safer and more viable option [4]. Nonsurgical techniques minimize operative blood loss, lower cardiac and pulmonary complications, reduce anesthetic and transfusion requirements, and allow for a rapid post-procedural recovery.
4. Conclusions
In this case report, the occlusion and PA of prosthetic FP bypass could have been addressed with surgical management but, with the use of the self-expanding stent graft, revascularization and exclusion was performed in a less invasive and time-efficient manner. This successful simultaneous treatment of both occlusion and anastomotic PA of prosthetic FP bypass led the authors to consider the placement of self-expanding stent graft as the most eligible strategy for simultaneous resolution of both complications while allowing preservation of flow in the surgical graft. However, more experience and follow-up are needed to confirm the durability of this technique.
Author Contributions
Conceptualization, A.A. and D.T.; methodology, I.M.B.; writing—original draft preparation, P.L.; writing—review and editing, C.F., S.M., G.T. and I.S.; supervision A.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Statement
Patient’s specific consent was obtained for this report, and approval by the Institutional Review Board for this retrospective study was not required.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Taha, A.G.; Byrne, R.M.; Avgerinos, E.D.; Marone, L.K.; Makaroun, M.S.; Chaer, R.A. Comparative effectiveness of endovascular versus surgical revascularization for acute lower extremity ischemia. J. Vasc. Surg. 2015, 61, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Magnetti, F.; Thalhammer, C.; Hechelhammer, L.; Husmann, M.; Pfammatter, T.; Amann-Vesti, B. Spontaneous pseudoaneurysm of a femoro-popliteal Omniflow II graft treated with a stentgraft. Vasa 2010, 39, 196–198. [Google Scholar] [CrossRef] [PubMed]
- Derom, A.; Nout, E. Treatment of femoral pseudoaneurysms with endograft in high-risk patients. Eur. J. Vasc. Endovasc. Surg. 2005, 30, 644–647.9. [Google Scholar] [CrossRef] [PubMed]
- Carollo, A.; Gagliardo, G.; DeVito, P.M.; Cicchillo, M. Stent graft repair of anastomotic pseudoaneurysm of femoral-popliteal bypass graft following patch angioplasty. J. Surg. Case Rep. 2016, 2016, rjw198. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rundback, J.; Haug, J.; Herman, K.; Manno, J.; Cerda, M. Percutaneous stent-graft repair of anastomotic pseudoaneurysms following vascular bypass procedures: A report of two cases. Case Rep. Vasc. Med. 2013, 2013, 124832. [Google Scholar] [CrossRef] [PubMed]
- Begovac, P.C.; Thomson, R.C.; Fisher, J.L.; Hughson, A.; Gällhagen, A. Improvements in GORE-TEX® Vascular Graft performance by Carmeda® BioActive Surface heparin immobilization. Eur. J. Vasc. Endovasc. Surg. 2003, 25, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.H.; Bush, R.L.; Yao, Q.; Lumsden, A.B.; Chen, C. Evaluation of platelet deposition and neointimal hyperplasia of heparin-coated small-caliber ePTFE grafts in a canine femoral artery bypass model. J. Surg. Res. 2004, 118, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Fujimura, N.; Obara, H.; Iwasa, K.; Hattori, T.; Yamamoto, H.; Watada, S.; Kobayashi, T.; Suematsu, N.; Mitsuoka, H.; Soga, Y.; et al. Preliminary Experience of Viabahn Stent Graft Inside the Occluded Prosthetic Bypass Graft for the Treatment of Above Knee Femoropopliteal Bypass Occlusion. Cardiovasc. Interv. Radiol. 2020, 43, 223–230. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).