Abstract
Empathy is a crucial human quality that enables healthcare professionals to connect with patients, providing physical and emotional support to enhance patient-centered care. Empathy in healthcare is critical for establishing patient-provider (healthcare) trust, increasing patient satisfaction, and, eventually, delivering high-quality healthcare. However, there is growing concern about the declining levels of empathy among healthcare providers, partly related to increased workload, burnout, and empathic distress fatigue. Moreover, the recent emphasis of medical education on the technical aspects of healthcare over empathetic care also contributed to the decline of empathy among healthcare providers with compromised patient care. This brief article summarizes the potential causes and consequences of declining empathy in medical practice with future implications on the quality of humanized healthcare.
1. Introduction
People have historically displayed specific characteristics like empathy to survive and thrive. Reiss states that “empathy plays a critical interpersonal and societal role, enabling sharing of experiences, needs, and desires between individuals and providing an emotional bridge that promotes prosocial behavior” [1]. Empathy also plays a critical role in healthcare, although its precise explanation and exact role have been heavily disputed among modern scholars. What is relatively less disputed is the decline of empathy among medical students [2]. Whether a decline in empathy among students eventually impacts patient care needs further evaluation. There is a lack of longitudinal (and cross-sectional) studies on the decline of empathy over the years of clinical practice. Also, many studies rely on self-reported empathy (often using the Jefferson Scale) rather than patients’ evaluations to objectively authenticate incidence [3]. Several pieces of literature describe clinician empathy’s positive impact on patients [4]; existing evidence suggests that empathy plays a vital role in medical practice and has a positive impact on both the patients and their physicians [5]. A systematic review of the effectiveness of empathy in general practice found that physician’s empathy improves patients’ physical and psychosocial health outcomes [3].
With heavy workloads and time constraints, healthcare professionals often have little time to build connections to provide empathetic care to patients. Persistent exposure to high-stress and decision-making environments can also lead to empathic distress fatigue among healthcare professionals, reducing their ability to empathize with patients [6]. This decline in empathy reduces the positive impact created by its presence during and after patient interactions; when compassion is impeded, distress may arise. Attempts to counter the declining clinical empathy have benefited patients, medical students, and healthcare practitioners [4]. In healthcare, Guidi and Traversa state that the current approach to dealing with a patient has primarily focused on a commitment to eliminate disease rather than a genuine interest in delivering holistic care [7], causing a widespread attitude to overlook ‘clinical empathy’; here, it is defined as “the ability to observe emotions in others, the ability to feel those emotions, and finally the ability to respond to those emotions”. It involves not only recognizing and understanding the emotions and needs of patients but also conveying this understanding to them in a compassionate and supportive manner. Therefore, clinical empathy encompasses active listening, nonverbal communication, and recognizing and validating patients’ emotions. Clinical empathy also contributes to a more potent therapeutic alliance between healthcare providers and patients, where patients feel understood and supported in their journey toward better health. Healthcare institutions must prioritize cultivating and maintaining empathy in healthcare providers to ensure the best possible patient care and a healthier, more fulfilling work environment for healthcare professionals. Mere scientific rigor within the medical field has overlooked the humanistic aspects of the multidimensionality of an illness.
This article aims to provide further insight into the vital components of empathy as defined by contemporary scholars and discusses the decline of empathy in healthcare, how its decline has impacted the healthcare landscape, and future steps that can be taken to resist and reverse its decline.
2. Empathy
As identified by the Institute of Medicine, one of the primary aims of a contemporary healthcare system is patient-centeredness. This encompasses empathy, compassion, and sensitivity to patients’ values, needs, and preferences. The importance of these qualities is further elaborated in a publication, and by using empathetic listening skills, healthcare professionals enhance the creation of trusting relationships with patients and provide quality healthcare [8].
Empathy has been defined in numerous ways to unpack its range of meanings. Reiss states that empathic capacity comprises three tentative components: perceptive components, processing components, and responsive components. Perceptive components can be influenced by the healthcare provider’s distinct outlook, trait sensitivity to others, and the surrounding environment. Similarly, Mercer and Reynolds describe physician empathy as the ability of healthcare providers to understand and feel compassion for their patients’ experiences, emotions, and perspectives. They stress the importance of empathy in fostering trust and patient satisfaction to improve patient outcomes. They advocate promoting empathy in medical education and practice by incorporating training into the medical curriculum, enhancing self-reflection, and building a supportive and empathetic work network [9].
From a non-medical perspective, Carl Rogers, the founder of the humanistic psychology movement, believed that empathy was a central concept in understanding human behavior and facilitating personal growth and change. According to Rogers, empathy involves understanding and accepting a person’s subjective experience from their point of view, without judgment or evaluation. He believed that empathy creates a helpful and non-judgmental situation that permits individuals to explore their opinions, feelings, and experiences more openly and honestly. Rogers emphasized the importance of an empathetic and non-directive approach in therapeutic relationships, where the therapist provides unconditional positive regard and empathy to the client to allow the client to develop their self-understanding and facilitate personal growth and self-actualization. Reiss also describes a mostly overlooked variable and precursor of feeling empathy: valuing a person in need and not appreciating the life and well-being of the person makes displaying empathy unrealistic and complex [1]. Developing a perspective can enhance empathy, where a person always considers another person’s thinking and feelings. Reiss defines it as the ability to see a person’s situation from their point of view [1]. To comment on its importance, Blatt and colleagues state that researchers have found that perspective-taking can elevate communication skills while lowering unprovoked aggression [10]. It can also help develop altruism, optimize agreements in business negotiations, and reduce stereotyping and prejudice.
The clinician’s ability to utilize cognitive empathy and perspective-taking better aids in compassionate behavior to appreciate the emotional states of others, which is enabled by the complex capability of empathy. Reiss says compassion and empathy go hand in hand [1]; compassion is the desire to help lessen the suffering of others, while empathy is the ability to comprehend and feel the emotions of others. Compassion is a conscious act to help others, whereas empathy is an instinctual feeling that occurs inevitably. Therefore, compassion is related to acting, while empathy is rooted in emotion.
3. Decline of Empathy
The successful modulation of empathy can lead to compassionate care, whereas failure can lead to emotional distress. Neumann and colleagues conducted studies on distress (e.g., burnout, low sense of well-being, reduced quality of life, and depression) among students and resident physicians. They found two notable findings [11]: (1) High levels of distress among both students and resident physicians, including symptoms of depression, anxiety, and burnout. The demanding nature of medical education and training, long working hours, and high-pressure environments contribute to this distress. (2) Distress negatively affects the well-being and performance of students and resident physicians. Such distress can lead to decreased empathy, decreased quality of patient care, increased medical errors, and higher rates of attrition from the medical profession. Neumann and colleagues reference Bauer’s hypothesis to add that extreme experiences of insensitivity or thoughtlessness can impair one’s existing empathic ability [11]. Furthermore, anxiety, tension, and stress can markedly impair mirror neurons’ signal rate, adversely impacting empathy. This explanation corresponds with a recent study of physicians’ brain functions, which found that medical expertise lessens the sensory processing, provoked by the perception of pain in others [12].
Neumann and colleagues outline other factors that lead to the downregulation of empathy during clinical practice. It includes trainees’ unrealistic expectations that medicine can always cure any condition that stems from increased responsibility for the patient. They also provide insight into a medical student’s career, sharing studies that showed a higher level of empathy during early student years [11]. However, it significantly declines as patient contact increases upon entering the clinical practice phase. Conversely, the study’s “managing emotions” subscale of the emotional intelligence score displayed markedly enhanced scores in final-year students compared with those of students in their first two years of study. It suggests that unrestrained empathy can lead to the mismanagement of emotions during student years. Furthermore, a correlation between specialty choice and self-perceived empathy is also noted. Higher empathy scores with patient-oriented specialties than less direct patient interaction, such as surgery or radiology, are described.
Additional factors that lead to a decline in empathy among medical students and residents in healthcare include the following (Figure 1):
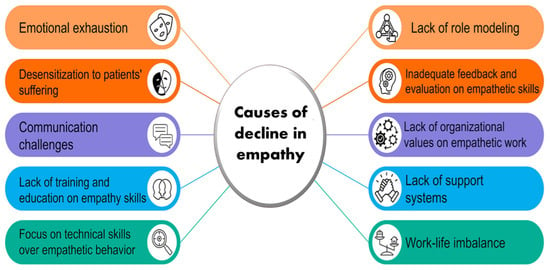
Figure 1.
List of potential causes of decline in empathy among healthcare providers.
- Medical student mistreatment ranges from humiliation to gender-specific discrimination and (sexual) harassment.
- Medical students and residents are vulnerable in facing the reality of life, including witnessing incurable illness and death of patients, to shift their attention to technology and objectivity.
- Lack of social support for the students and residents reduces contact with the families and peer groups.
- The high workload of the students and residents reduces sleeping time and inadequate recreation time.
Another study explored the influence of elitist thinking among medical students and residents as a possible factor contributing to decreased empathy [13]. It revealed that the potential sense of belonging to an elite and privileged group could lead to a rational detachment from the patient. Other studies examined the “formal/informal curriculum” elements that could contribute to empathy decline [11]. These factors include brief patient encounters, which may lead to a fragmented patient–physician relationship and a lack of opportunity for comprehensive learning from and with the patient. Additionally, an unsupportive learning environment characterized by unstructured studying, limited bedside interactions, and disrespectful treatment of medical students, combined with unrealistic expectations regarding physicians’ behavior among students, can be an additional stressful burden. A recent systematic review and thematic analysis of qualitative studies by Howick et al. has emphasized the role of the hidden curriculum in empathy decline [14]. The authors elaborated on developing an ‘empathic hidden curriculum’ that alleviates the decline in medical student empathy to eventually benefit from providing empathic care for patients and practitioners [14].
4. Positive Impact of Empathy
Relating the decline of empathy to its ramifications, Guidi and Traversa state that a patient’s illness becomes a more important focus than the person [7]. Studies have documented that about 50% of treatments are not taken as prescribed; however, empathetic patient care yields better clinical outcomes, which include patients’ compliance with the medical care plan with greater patient satisfaction and improved outcomes [15]. According to Neumann and colleagues, patient–physician communication has a beneficial impact on psychosocial outcomes such as quality of life, anxiety, and depression, as well as on objectively measurable factors like symptom reduction and improved blood pressure and blood glucose levels [11]. This is supported by studies showing a connection between empathy and positive therapeutic outcomes in patients with diabetes, as highlighted by Moudatsou and colleagues [16]. The authors also note that empathetic nursing care can reduce stress, depression, and aggression in patients with cancer. Similarly, the empathetic relationship between a midwife and an expectant mother enhances the mother’s satisfaction while reducing stress, anguish, and pain during labor, creating feelings of security, trust, and encouragement [17].
The studies have identified several potential protective factors against distress, including social support from peers and mentors, resilience, self-care practices, and access to mental health resources [11]. Addressing distress among students and resident physicians is crucial for empathetic care. Such empathic behavior by the healthcare providers may increase patients’ compliance and satisfaction. Guidi and Traversa detailed the importance of trust in therapeutic medicine, and how trust in the healthcare provider empowers patients to follow their medical treatment plan more actively [7]. In a study conducted on Mayo Clinic medical residents, higher levels of error were associated with lower levels of empathy [18]. It indicates that more empathetic physicians make fewer errors because they can gather more critical insight and develop deeper insights, improving healthcare quality with better disease outcomes. From a financial perspective, these outcomes are also advantageous as they lead to reduced costs of medical care. Empathic relationships contribute to improved physiological responses and shorter hospital stays, resulting in lower overall expenses [19]. Therefore, a decline in empathy among healthcare providers can adversely impact on patient care by reducing patient satisfaction, increasing medical errors, diminishing patient trust, and increasing healthcare costs [20,21].
5. Improving Empathy
As mentioned earlier, the declining empathy among medical students has been well-documented in the last few decades, partly driven by the sense of elitism, amalgamated with a lack of learning and training opportunities for the students to appreciate the value of empathy in clinical medicine. To improve empathy, healthcare professionals need periodic training. One strategy for fostering empathy is incorporating such training in the early years of medical, nursing, or healthcare-related educational curriculum. Such early training of care providers would help improve the professional relationship with the patients [22]. However, certain studies have shown that adopting courses stressing the importance of clinical empathy in the later years of medical education might yield better health outcomes [23]. Another strategy is mindfulness training among healthcare providers. Mindfulness boosts interpersonal relationships by enhancing empathy, compassion, and attentiveness, reflected in the improved patient-centeredness of mindful physicians conducting their clinical practice [24]. It, however, needs to be mentioned that a recent systematic review/meta-analysis by Cardoso Gomes da Silva and colleagues found that mindfulness training may improve psychological well-being and reduce stress, but evidence for empathy outcome was very marginal [25]. According to Gleichgerrcht and Decety, empathic concern strongly relates to compassion satisfaction, which may affect how empathy is practiced in clinical settings [26]. In terms of clinical empathy, Decety and Lamm proposed that empathy has three dimensions: emotion sharing, perspective taking, and emotional regulation [27]. The holistic conception of clinical empathy may include cognitive and affective empathy. Gleichgerrcht and Decety recommend that to promote clinical empathy, early-year medical training should focus on the cognitive components [26]. These components involve understanding another person’s experiences and perspectives, rather than solely focusing on the emotional component, which involves sharing their emotions and may contribute to emotional exhaustion. Reiss refers to this as attenuation, which enables individuals to empathize without becoming overwhelmed by the personal distress of others [1]. By avoiding excessive emotional distress, individuals can maintain their ability to be helpful and supportive.
To highlight, in order to improve the level of empathy, healthcare providers need to (1) practice active listening to understand the perspective and feelings of the patients; (2) avoid judgment and prejudices when interacting with patients; (3) show compassion towards the patients; provide reassurance, show understanding, and offer comfort when needed; (4) develop cultural competence to appreciate that different cultures have different ways of expressing and perceiving illness and pain; and finally, (5) practice self-reflection on own emotions and reactions during patient encounters with self-awareness training [11]. These practices would foster empathy, enhance patient’s emotional satisfaction, and improve health outcomes.
By documenting the lack of empathy amongst healthcare providers (Figure 1) and appreciating its importance in clinical medicine, the relevant institutes should adopt the necessary academic curriculum to train healthcare workers to foster a higher level of empathy for better clinical outcomes. Columbia University incorporated a course (Narrative Medicine) to teach physicians the importance of considering patients’ overall socioeconomic situations to design a comprehensive healthcare plan [28]. Duke University adopted a course to train oncology fellows on the importance of empathy in providing physical and emotional support to patients [29]. Medical students at Stanford University are assessed for social and cultural awareness with a level of empathy through a simulated clinical environment. By incorporating the Standardized Patients Program for student physicians as early as the first quarter of medical school, Stanford University students can appreciate the importance of empathy in dealing with patients early in their professional careers [30].
6. Conclusions
The decline of empathy in healthcare has significantly impacted both patients and healthcare providers (Figure 1). Medical students and residents have reported a decline in empathy due to distresses such as burnout, low sense of well-being, reduced quality of life, and depression, which have negatively impacted patient care. Fortunately, several interventions can be implemented to halt and reverse this decline, such as mindfulness-based stress reduction, self-awareness training, meaningful experiences, and reflective practice discussions on clinical empathy. Also, the hidden curriculum that prioritizes medical knowledge over patient care might lead to a lack of development in the empathetic behavior of the students and could impact patient care [31]. Finally, a relatively recent systematic review/meta-analysis highlighted the importance of using a mixture of pedagogical methods and adopting courses emphasizing clinical empathy’s importance in the later years of medical education to yield better health outcomes [23].
Author Contributions
Conceptualization, M.S.R.; writing—original draft preparation, M.O.R.; writing—review and editing, R.F. and M.S.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
We want to express our sincere gratitude to Nuraly Akimbekov (Al-Farabi Kazakh National University, Kazakhstan) for his help in drawing the illustrations. We also wish to thank Peace Uwambaye, and Margo Wolfe for providing useful suggestions. M.O.R. is an Osteopathic Medical Student (OMS III) at the Lake Erie College of Osteopathic Medicine, Erie (USA).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Riess, H. The Science of Empathy. J. Patient Exp. 2017, 4, 74–77. [Google Scholar] [CrossRef] [PubMed]
- Roff, S. Reconsidering the “decline” of medical student empathy as reported in studies using the Jefferson Scale of Physician Empathy-Student version (JSPE-S). Med. Teach. 2015, 37, 783–786. [Google Scholar] [CrossRef]
- Derksen, F.; Bensing, J.; Lagro-Janssen, A. Effectiveness of empathy in general practice: A systematic review. Br. J. Gen. Pract. 2013, 63, e76–e84. [Google Scholar] [CrossRef] [PubMed]
- Halpern, J. What is clinical empathy? J. Gen. Intern. Med. 2003, 18, 670–674. [Google Scholar] [CrossRef] [PubMed]
- Decety, J.; Fotopoulou, A. Why empathy has a beneficial impact on others in medicine: Unifying theories. Front. Behav. Neurosci. 2014, 8, 457. [Google Scholar] [CrossRef]
- Singer, T.; Klimecki, O.M. Empathy and compassion. Curr. Biol. 2014, 24, R875–R878. [Google Scholar] [CrossRef]
- Guidi, C.; Traversa, C. Empathy in patient care: From ‘Clinical Empathy’ to ‘Empathic Concern’. Med. Health Care Philos. 2021, 24, 573–585. [Google Scholar] [CrossRef]
- Dohrenwend, A.M. Defining Empathy to Better Teach, Measure, and Understand Its Impact. Acad. Med. 2018, 93, 1754–1756. [Google Scholar] [CrossRef]
- Mercer, S.W.; Reynolds, W.J. Empathy and quality of care. Br. J. Gen. Pract. 2020, 52, S9–S12. [Google Scholar]
- Blatt, B.; LeLacheur, S.F.; Galinsky, A.D.; Simmens, S.J.; Greenberg, L. Does perspective-taking increase patient satisfaction in medical encounters? Acad. Med. 2010, 85, 1445–1452. [Google Scholar] [CrossRef]
- Neumann, M.; Edelhauser, F.; Tauschel, D.; Fischer, M.R.; Wirtz, M.; Woopen, C.; Haramati, A.; Scheffer, C. Empathy decline and its reasons: A systematic review of studies with medical students and residents. Acad. Med. 2011, 86, 996–1009. [Google Scholar] [CrossRef] [PubMed]
- Decety, J.; Yang, C.Y.; Cheng, Y. Physicians down-regulate their pain empathy response: An event-related brain potential study. Neuroimage 2010, 50, 1676–1682. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.; Hu, W.; Griffin, B. Cultures of Success: How elite students develop and realise aspirations to study Medicine. Aust. Educ. Res. 2020, 50, 1127–1147. [Google Scholar] [CrossRef]
- Howick, J.; Dudko, M.; Feng, S.N.; Ahmed, A.A.; Alluri, N.; Nockels, K.; Winter, R.; Holland, R. Why might medical student empathy change throughout medical school? a systematic review and thematic synthesis of qualitative studies. BMC Med. Educ. 2023, 23, 270. [Google Scholar] [CrossRef]
- Kim, S.S.; Kaplowitz, S.; Johnston, M.V. The effects of physician empathy on patient satisfaction and compliance. Eval. Health Prof. 2004, 27, 237–251. [Google Scholar] [CrossRef]
- Moudatsou, M.; Stavropoulou, A.; Philalithis, A.; Koukouli, S. The Role of Empathy in Health and Social Care Professionals. Healthcare 2020, 8, 26. [Google Scholar] [CrossRef]
- Del Canale, S.; Louis, D.Z.; Maio, V.; Wang, X.; Rossi, G.; Hojat, M.; Gonnella, J.S. The relationship between physician empathy and disease complications: An empirical study of primary care physicians and their diabetic patients in Parma, Italy. Acad. Med. 2012, 87, 1243–1249. [Google Scholar] [CrossRef]
- West, C.P.; Huschka, M.M.; Novotny, P.J.; Sloan, J.A.; Kolars, J.C.; Habermann, T.M.; Shanafelt, T.D. Association of Perceived Medical Errors With Resident Distress and EmpathyA Prospective Longitudinal Study. JAMA 2016, 296, 1071–1078. [Google Scholar] [CrossRef] [PubMed]
- Howick, J.; Mittoo, S.; Abel, L.; Halpern, J.; Mercer, S.W. A price tag on clinical empathy? Factors influencing its cost-effectiveness. J. R. Soc. Med. 2020, 113, 389–393. [Google Scholar] [CrossRef]
- Wang, C.X.Y.; Pavlova, A.; Fernando, A.T., 3rd; Consedine, N.S. Beyond empathy decline: Do the barriers to compassion change across medical training? Adv. Health Sci. Educ. Theory Pract. 2022, 27, 521–536. [Google Scholar] [CrossRef]
- Yu, C.C.; Tan, L.; Le, M.K.; Tang, B.; Liaw, S.Y.; Tierney, T.; Ho, Y.Y.; Lim, B.E.E.; Lim, D.; Ng, R.; et al. The development of empathy in the healthcare setting: A qualitative approach. BMC Med. Educ. 2022, 22, 245. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Guo, H.; Xu, Z.; Xiao, H. Empathy variation of undergraduate medical students after early clinical contact: A cross-sectional study in China. BMJ Open 2020, 10, e035690. [Google Scholar] [CrossRef]
- Fragkos, K.C.; Crampton, P.E.S. The Effectiveness of Teaching Clinical Empathy to Medical Students: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Acad. Med. 2020, 95, 947–957. [Google Scholar] [CrossRef]
- Ardenghi, S.; Rampoldi, G.; Pepe, A.; Bani, M.; Salvarani, V.; Strepparava, M.G. An Exploratory Cross-Sectional Study on the Relationship between Dispositional Mindfulness and Empathy in Undergraduate Medical Students. Teach. Learn. Med. 2021, 33, 154–163. [Google Scholar] [CrossRef]
- da Silva, C.C.G.; Bolognani, C.V.; Amorim, F.F.; Imoto, A.M. Effectiveness of training programs based on mindfulness in reducing psychological distress and promoting well-being in medical students: A systematic review and meta-analysis. Syst. Rev. 2023, 12, 79. [Google Scholar] [CrossRef] [PubMed]
- Gleichgerrcht, E.; Decety, J. Empathy in clinical practice: How individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PLoS ONE 2013, 8, e61526. [Google Scholar] [CrossRef] [PubMed]
- Decety, J.; Lamm, C. Human empathy through the lens of social neuroscience. Sci. World J. 2006, 6, 1146–1163. [Google Scholar] [CrossRef]
- Miller, E.; Balmer, D.; Hermann, N.; Graham, G.; Charon, R. Sounding narrative medicine: Studying students’ professional identity development at Columbia University College of Physicians and Surgeons. Acad. Med. 2014, 89, 335–342. [Google Scholar] [CrossRef]
- Pollak, K.I.; Arnold, R.; Alexander, S.C.; Jeffreys, A.S.; Olsen, M.K.; Abernethy, A.P.; Rodriguez, K.L.; Tulsky, J.A. Do patient attributes predict oncologist empathic responses and patient perceptions of empathy? Support. Care Cancer 2010, 18, 1405–1411. [Google Scholar] [CrossRef][Green Version]
- Standford-Medicine. Standardized Patient Program. Available online: https://cisl.stanford.edu/standardized–patient–program.html (accessed on 13 September 2023).
- Weissman, S. Faculty empathy and the hidden curriculum. Acad. Med. 2012, 87, 389. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).