Defining Leadership in Undergraduate Medical Education, Networks, and Instructors: A Scoping Review
Abstract
1. Introduction
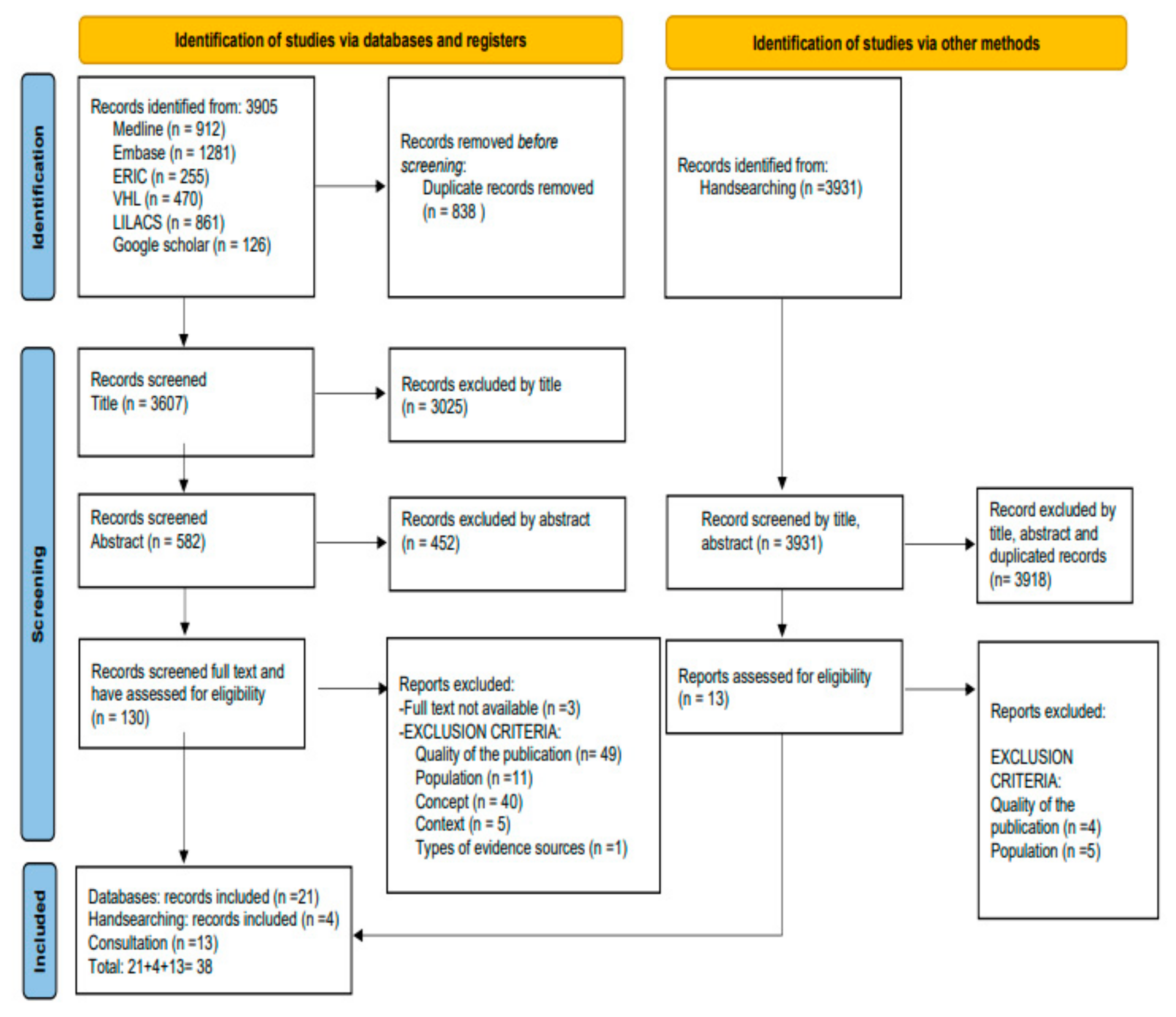
2. Methods
2.1. Research Model
2.2. Participants
2.3. Data Collection Tools
2.4. Data Collection Process
2.5. Data Analysis
3. Results
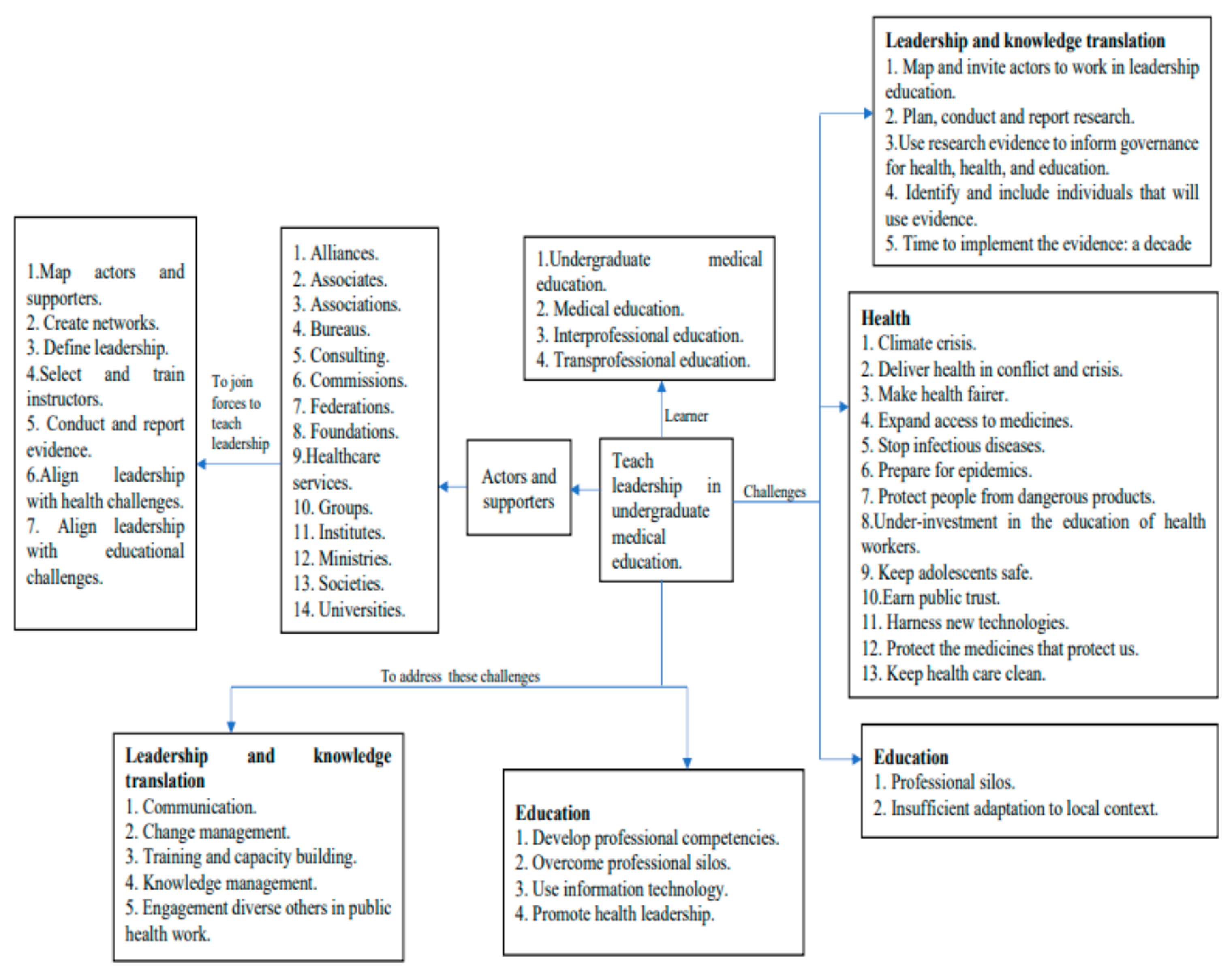
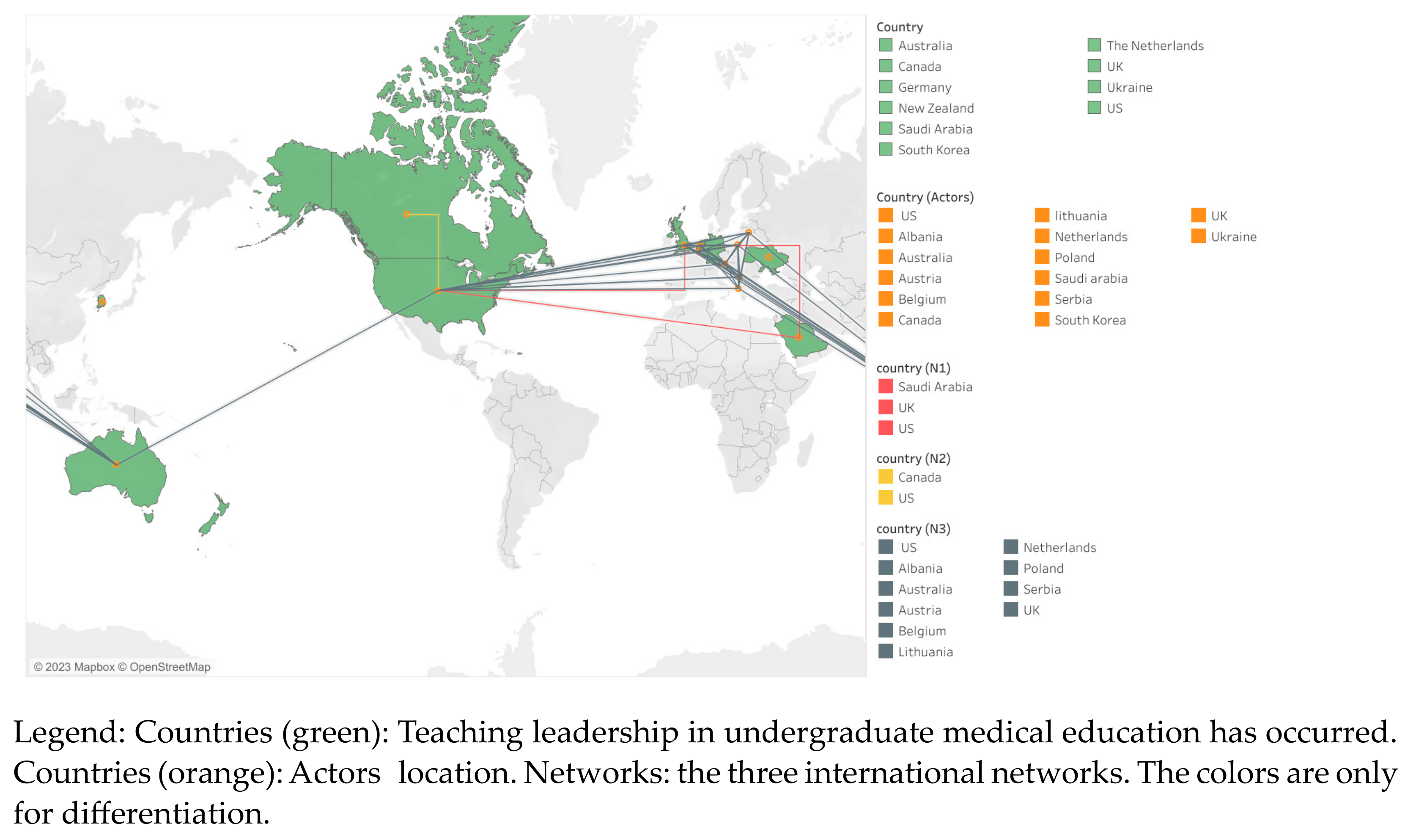
3.1. Mapping: Actors’ Networks and Their Supporters
3.2. Teaching Leadership: UME, IPE, and TPE
3.3. Defining Leadership and Learners’ Levels
3.4. Instructor
4. Discussion
- To map actors and supporters that have expertise in teaching leadership in UME nationally and internationally. Mapping actors can provide a roadmap to advance leadership education in their country by sharing information and resources, and capacitating trainers and learners.
- To define or conceptualize leadership in their context. This review provided more than 20 definitions that can guide actors and supporters. We invite them to include values in their definition.
- To target the learners that will have leadership competencies. It can be in UME, medical education, IPE and TPE. Ideally, breaking silos is desirable, and teaching leadership is about having competency to work with others.
- To establish instructors’ expertise and academic background to teach leadership and consider capacitating instructors with leadership and educational competencies.
- Actors, journals, and peer reviewers should enhance the use of GREET to provide relevant information to others about education in this field.
4.1. Areas of Future Research
- The best methods and practices to create or adapt leadership definitions, to target the students, and to select and train the trainers in a specific context.
- Identification of best practices sharing, including leadership definitions, and competency models to support leadership education and training in UME.
- Teaching leadership in UME and PhD candidates simultaneously by using CBE has not been retrieved in this review.
4.2. Limitations of This Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Frenk, J.; Chen, L.; Bhutta, Z.A.; Cohen, J.; Crisp, N.; Evans, T.; Fineberg, H.; Garcia, P.; Ke, Y.; Kelley, P.; et al. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet 2010, 376, 1923–1958. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, I.; Glasziou, P. Avoidable waste in the production and reporting of research evidence. Lancet 2009, 374, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Macleod, M.R.; Michie, S.; Roberts, I.; Dirnagl, U.; Chalmers, I.; Ioannidis, J.P.A.; Salman, R.A.-S.; Chan, A.-W.; Glasziou, P. Biomedical research: Increasing value, reducing waste. Lancet 2014, 383, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Visram, S.; Goodall, D.; Steven, A. Exploring conceptualizations of knowledge translation, transfer and exchange across public health in one UK region: A qualitative mapping study. Public Health 2014, 128, 497–503. [Google Scholar] [CrossRef] [PubMed]
- DeZee, K.J.; Artino, A.; Elnicki, D.M.; Hemmer, P.A.; Durning, S.J. Medical education in the United States of America. Med. Teach. 2012, 34, 521–525. [Google Scholar] [CrossRef]
- Matrix Insight. EU Level Collaboration on Forecasting Health Workforce Needs, Workforce Planning and Health Workforce Trends—A Feasibility Study; Commission Feasibility Study on EU Level Collaboration on Forecasting Health Workforce Needs, Workforce Planning and Health Workforce Trends; European Commission: Brussels, Belgium, 2012; Available online: https://european-union.europa.eu/select-language?destination=/node/1 (accessed on 31 January 2023).
- Talib, Z.; Narayan, M.L.; Harrod, M.T. Postgraduate Medical Education in Sub-Saharan Africa: A Scoping Review Spanning 26 Years and Lessons Learned. J. Grad. Med. Educ. 2019, 11, 34–46. [Google Scholar] [CrossRef]
- Luengo-Martínez, C.E.; Sanhueza-Alvarado, O. Formación del licenciado en Enfermería en América Latina. Aquichan 2016, 16, 240–255. [Google Scholar] [CrossRef]
- World Health Organization. Urgent Health Challenges for the Next Decade. 2020. Available online: https://www.who.int/news-room/photo-story/photo-story-detail/urgent-health-challenges-for-the-next-decade (accessed on 31 January 2023).
- Graham, I.D.; Logan, J.; Harrison, M.B.; Straus, S.E.; Tetroe, J.; Caswell, W.; Robinson, N. Lost in knowledge translation: Time for a map? J. Contin. Educ. Health Prof. 2006, 26, 13–24. [Google Scholar] [CrossRef]
- Shearer, J.C.; Dion, M.; Lavis, J.N. Exchanging and using research evidence in health policy networks: A statistical network analysis. Implement. Sci. 2014, 9, 126. [Google Scholar] [CrossRef]
- Campbell, C.; Pollock, K.; Briscoe, P.; Carr-Harris, S.; Tuters, S. Developing a knowledge network for applied education research to mobilise evidence in and for educational practice. Educ. Res. 2017, 59, 209–227. [Google Scholar] [CrossRef]
- Hoffman, S.J.; Cole, C.B. Defining the global health system and systematically mapping its network of actors. Glob. Health 2018, 14, 38. [Google Scholar] [CrossRef]
- Glegg, S.M.N.; Jenkins, E.; Kothari, A. How the study of networks informs knowledge translation and implementation: A scoping review. Implement. Sci. 2019, 14, 34. [Google Scholar] [CrossRef]
- Rodríguez-Feria, P.; Flórez, L.J.H.; Czabanowska, K. Leadership Competencies for Knowledge Translation in Public Health: A consensus study. J. Public Health 2021, 44, 926–935. [Google Scholar] [CrossRef]
- Warren, O.J.; Carnall, R. Medical leadership: Why it’s important, what is required, and how we develop it. Med. J. 2011, 87, 27–32. [Google Scholar] [CrossRef]
- Mintz, L.J.; Stoller, J.K. A Systematic Review of Physician Leadership and Emotional Intelligence. J. Grad. Med. Educ. 2014, 6, 21–31. [Google Scholar] [CrossRef]
- Frich, J.C.; Brewster, A.L.; Cherlin, E.J.; Bradley, E.H. Leadership Development Programs for Physicians: A Systematic Review. J. Gen. Intern. Med. 2015, 30, 656–674. [Google Scholar] [CrossRef]
- Czabanowska, K. Public health competencies: Prioritization and leadership. Eur. J. Public Health 2016, 26, 734–735. [Google Scholar] [CrossRef]
- Heinen, M.; Van Oostveen, C.; Peters, J.; Vermeulen, H.; Huis, A. An integrative review of leadership competencies and attributes in advanced nursing practice. J. Adv. Nurs. 2019, 75, 2378–2392. [Google Scholar] [CrossRef]
- Ross, S.J.; Gupta, T.S.; Johnson, P. Why we need to teach leadership skills to medical students: A call to action. BMJ Lead. 2019, 3, 6–10. [Google Scholar] [CrossRef]
- Cometto, G.; Buchan, J.; Dussault, G. Developing the health workforce for universal health coverage. Bull. World Health Organ. 2020, 98, 109–116. [Google Scholar] [CrossRef]
- Gershuni, O.; Czabanowska, K.; Burazeri, G.; Bjegovic-Mikanovic, V.; Juszczyk, G.; Myrup, A.C.; Kurpita, V. Aligning Best Practices: A Guiding Framework as a Valuable Tool for Public Health Workforce Development with the Example of Ukraine. Int. J. Environ. Res. Public Health 2021, 18, 9246. [Google Scholar] [CrossRef] [PubMed]
- Webb, A.M.; Tsipis, N.E.; McClellan, T.R.; McNeil, M.J.; Xu, M.; Doty, J.P.; Taylor, D.C. A First Step Toward Understanding Best Practices in Leadership Training in Undergraduate Medical Education: A Systematic Review. Acad. Med. 2014, 89, 1563–1570. [Google Scholar] [CrossRef] [PubMed]
- James, E.; Evans, M.; Mi, M. Leadership Training and Undergraduate Medical Education: A Scoping Review. Med. Sci. Educ. 2021, 31, 1501–1509. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.C.; Oliveira, F.R.A.; Delfino, B.M.; Pereira, T.M.; de Moraes, F.H.P.; Barbosa, G.V.; de Macedo, L.F.; Domingos, T.D.S.; Da Silva, D.P.; Menezes, C.C.R.; et al. How we enhanced medical academics skills and reduced social inequities using an academic teaching program. Med. Teach. 2015, 37, 1003–1007. [Google Scholar] [CrossRef] [PubMed]
- Gobierno de Colombia; Ministerio de Educación y Ministerio de Salud. Documento de Recomendaciones para la Transformación de la Educación Medica en Colombia. 2017. Available online: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/MET/recomendaciones-comision-para-la-transformacion.pdf (accessed on 31 January 2023).
- Flores-Domínguez, C. Feminización En Medicina: Liderazgo Y Academia Feminization of Medicine: Leadership and Academics. Educ. Méd. 2012, 15, 191–195. [Google Scholar] [CrossRef]
- Sánchez-Mendiola, M. Liderazgo en medicina: ¿debemos enseñarlo y evaluarlo? Investig. Educ. Méd. 2015, 4, 99–107. [Google Scholar] [CrossRef]
- Aguirre-Gas. H.G.; Mazón-González, B. Calidad y liderazgo en medicina. Rev. CONAMED 2013, 18, 172–182. [Google Scholar]
- Revista Colegio Médico CL. Liderazgo en el Equipo Sanitario. 2019. Available online: http://revista.colegiomedico.cl/liderazgo-en-el-equipo-sanitario/ (accessed on 31 January 2023).
- Llaque, D.W. Liderazgo-Ética Médica. Available online: http://anmperu.org.pe/anales/2011/liderazgo_etica_medica.pdf (accessed on 31 January 2023).
- Abreu Cervantes, A.; Téllez Cabrera, M.Y. Líderes Universitarios Y Protagonismo Estudiantil. Caso Universidad De Ciencias Médicas De Camagüey. Humanidades Méd. 2018, 18, 504–520. [Google Scholar]
- Bandeira, I.D.; Mendoza, J. Medical education and leadership: A call to action for Brazil’s mental health system. Int. J. Med. Educ. 2018, 9, 170–172. [Google Scholar] [CrossRef]
- Fennell, K.L. Conceptualisations of Leadership and Relevance to Health and Human Service Workforce Development: A Scoping Review. J. Multidiscip. Healthc. 2021, 14, 3035–3051. [Google Scholar] [CrossRef]
- Phillips, A.C.; Lewis, L.K.; McEvoy, M.P.; Galipeau, J.; Glasziou, P.; Hammick, M.; Moher, D.; Tilson, J.K.; Williams, M.T. A systematic review of how studies describe educational interventions for evidence-based practice: Stage 1 of the development of a reporting guideline. BMC Med. Educ. 2014, 14, 152. [Google Scholar] [CrossRef]
- Phillips, A.C.; Lewis, L.K.; McEvoy, M.P.; Galipeau, J.; Glasziou, P.; Moher, D.; Tilson, J.K.; Williams, M.T. Development and validation of the guideline for reporting evidence-based practice educational interventions and teaching (GREET). BMC Med. Educ. 2016, 16, 1–10. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic Review or Scoping Review? Guidance for Authors When Choosing between a Systematic or Scoping Review Approach. BMC Med. Res. Methodol. 2018, 18, 1–7. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Chapter 11: Scoping reviews. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: North Adelaide, SA, Australia, 2020. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K.; Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Canadian Health Care. The Effective Public Health Practice Project: Quality Assessment Tool for Quantitative Studies. Instructions for Completion: Please Circle Appropriate Response in Each Section. Available online: https://www.ephpp.ca/ (accessed on 31 January 2023).
- Critical Appraisal Skills Programme. CASP Qualitative Checklist. CASP-Qualitative-Checklist-2018_fillable_form.pdf. Available online: https://casp-uk.net/ (accessed on 31 January 2023).
- Tyndall, J. AACODS Checklist. Flinders University. 2010. Available online: http://dspace.flinders.edu.au/dspace/ (accessed on 31 January 2023).
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.P.; Griffiths, F.; Nicolau, B.; et al. Mixed Methods Appraisal Tool (MMAT), Registration of Copyright (#1148552), Canadian Intellectual Property Office, Industry Canada. Microsoft Word-MMAT_2018_criteria-manual_2018-07-26.docx. 2018. Available online: https://www.pbworks.com/ (accessed on 31 January 2023).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Gruner, D.; Feinberg, Y.; Venables, M.J.; Hashmi, S.S.; Saad, A.; Archibald, D.; Pottie, K. An undergraduate medical education framework for refugee and migrant health: Curriculum development and conceptual approaches. BMC Med. Educ. 2022, 22, 374. [Google Scholar] [CrossRef]
- Bernard, A.; Ortiz, S.C.; Jones, E.; Heung, M.; Guetterman, T.C.; Kirst, N. The Pandemic Leadership Model: A Study of Medical Student Values During COVID-19. Int. J. Med. Stud. 2021, 9, 274–281. [Google Scholar] [CrossRef]
- Ross, S.J.; Gupta, T.S.; Johnson, P. Leadership curricula and assessment in Australian and New Zealand medical schools. BMC Med. Educ. 2021, 21, 28. [Google Scholar] [CrossRef]
- Hashmi, S.S.; Saad, A.; Leps, C.; Gillies-Podgorecki, J.; Feeney, B.; Hardy, C.; Falzone, N.; Archibald, D.; Hoang, T.; Bond, A.; et al. A student-led curriculum framework for homeless and vulnerably housed populations. BMC Med. Educ. 2020, 20, 232. [Google Scholar] [CrossRef]
- Rajeh, N.; Grant, J.; Farsi, J.; Tekian, A. Contextual Analysis of Stakeholder Opinion on Management and Leadership Competencies for Undergraduate Medical Education: Informing Course Design. J. Med. Educ. Curric. Dev. 2020, 7, 2382120520948866. [Google Scholar] [CrossRef] [PubMed]
- Barry, E.S.; Dong, T.; Durning, S.J.; Schreiber-Gregory, D.; Torre, D.; Grunberg, N.E. Medical Student Leader Performance in an Applied Medical Field Practicum. Mil. Med. 2019, 184, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Hur, Y.; Lee, K. Identification and evaluation of the core elements of character education for medical students in Korea. J. Educ. Evaluation Health Prof. 2019, 16, 21. [Google Scholar] [CrossRef] [PubMed]
- Portney, D.S.; VonAchen, P.; Standiford, T.; Carey, M.R.; Vu, J.; Kirst, N.; Zink, B. Medical Student Consulting: Providing Students Leadership and Business Opportunities While Positively Impacting the Community. MedEdPORTAL 2019, 15, 10838. [Google Scholar] [CrossRef] [PubMed]
- Richard, K.; Noujaim, M.; Thorndyke, L.E.; Fischer, M.A. Preparing Medical Students to Be Physician Leaders: A Leadership Training Program for Students Designed and Led by Students. MedEdPORTAL 2019, 15, 10863. [Google Scholar] [CrossRef]
- Wagenschutz, H.; McKean, E.L.; Mangrulkar, R.; Zurales, K.; Santen, S. A first-year leadership programme for medical students. Clin. Teach. 2019, 16, 623–629. [Google Scholar] [CrossRef]
- Dickerman, J.; Sánchez, J.P.; Portela-Martinez, M.; Roldan, E. Leadership and Academic Medicine: Preparing Medical Students and Residents to Be Effective Leaders for the 21st Century. MedEdPORTAL 2018, 14, 10677. [Google Scholar] [CrossRef]
- Chen, H.C.; Wamsley, M.A.; Azzam, A.; Julian, K.; Irby, D.M.; O’Sullivan, P.S. The Health Professions Education Pathway: Preparing Students, Residents, and Fellows to Become Future Educators. Teach. Learn. Med. 2017, 29, 216–227. [Google Scholar] [CrossRef]
- Gonzalo, J.D.; Dekhtyar, M.; Starr, S.R.; Borkan, J.; Brunett, P.; Fancher, T.; Green, J.; Grethlein, S.J.; Lai, C.; Lawson, L.; et al. Health Systems Science Curricula in Undergraduate Medical Education. Acad. Med. 2017, 92, 123–131. [Google Scholar] [CrossRef]
- Schmidt-Huber, M.; Netzel, J.; Kiesewetter, J. On the road to becoming a responsible leader: A simulation-based training approach for final year medical students. GMS J. Med. Educ. 2017, 34, Doc34. [Google Scholar] [CrossRef]
- Jefferies, R.; Sheriff, I.H.; Matthews, J.H.; Jagger, O.; Curtis, S.; Lees, P.; Spurgeon, P.C.; Fountain, D.M.; Oldman, A.; Habib, A.; et al. Leadership and management in UK medical school curricula. J. Health Organ. Manag. 2016, 30, 1081–1104. [Google Scholar] [CrossRef]
- Sydorchuk, A.; Moskaliuk, V.D.; Randiuk, Y.O.; Sorokhan, V.D.; Golyar, O.I.; Sydorchuk, L.; Humenna, A.V. Aspects of development of leader creative thinking of medical student at the undergraduate level of medical education. Wiadomości Lek. 2016, 69, 809–812. [Google Scholar]
- Stringfellow, T.D.; Rohrer, R.M.; Loewenthal, L.; Gorrard-Smith, C.; Sheriff, I.H.; Armit, K.; Lees, P.D.; Spurgeon, P.C. Defining the structure of undergraduate medical leadership and management teaching and assessment in the UK. Med. Teach. 2015, 37, 747–754. [Google Scholar] [CrossRef]
- Czabanowska, K.; Smith, T.; Könings, K.; Sumskas, L.; Otok, R.; Bjegovic-Mikanovic, V.; Brand, H. In search for a public health leadership competency framework to support leadership curriculum-a consensus study. Eur. J. Public Health 2014, 24, 850–856. [Google Scholar] [CrossRef]
- Mullan, P.B.; Williams, J.; Malani, P.N.; Riba, M.; Haig, A.; Perry, J.; Kolars, J.C.; Mangrulkar, R.; Williams, B. Promoting medical students’ reflection on competencies to advance a global health equities curriculum. BMC Med. Educ. 2014, 14, 91. [Google Scholar] [CrossRef]
- Quince, T.; Abbas, M.; Murugesu, S.; Crawley, F.; Hyde, S.; Wood, D.; Benson, J. Leadership and management in the undergraduate medical curriculum: A qualitative study of students’ attitudes and opinions at one UK medical school. BMJ Open 2014, 4, e005353. [Google Scholar] [CrossRef]
- Warde, C.M.; Vermillion, M.; Uijtdehaage, S. A medical student leadership course led to teamwork, advocacy, and mindfulness. Fam. Med. 2014, 46, 459–462. [Google Scholar]
- Coleman, M.M.; Blatt, B.; Greenberg, L. Preparing Students to Be Academicians: A National Student-Led Summer Program in Teaching, Leadership, Scholarship, and Academic Medical Career-Building. Acad. Med. 2012, 87, 1734–1741. [Google Scholar] [CrossRef]
- Varkey, P.; Peloquin, J.; Reed, D.; Lindor, K.; Harris, I. Leadership curriculum in undergraduate medical education: A study of student and faculty perspectives. Med. Teach. 2009, 31, 244–250. [Google Scholar] [CrossRef]
- Perry, I.J. Commentary: ASPHER at age 50. Eur. J. Public Health 2017, 27, 3. [Google Scholar] [CrossRef] [PubMed]
- Equator Network. Development and Validation of the Guideline for Reporting Evidence-Based Practice Educational Interventions and Teaching (GREET)|The EQUATOR Network. 2021. Available online: https://www.equator-network.org/ (accessed on 31 January 2023).
- Könings, K.D.; De Jong, N.; Lohrmann, C.; Šumskas, L.; Smith, T.; O’Connor, S.J.; Spanjers, I.A.E.; Van Merriënboer, J.J.G.; Czabanowska, K. Is blended learning and problem-based learning course design suited to develop future public health leaders? An explorative European study. Public Health Rev. 2018, 39, 13. [Google Scholar] [CrossRef] [PubMed]
| # | Tittle | First author | Year | Location | Support | Co-authors | Learners’ level | Instructor selection 1 | Instructor training 2 | Leadership Definition |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | An Undergraduate Medical Education Framework for Refugee and Migrant Health: Curriculum Development and Conceptual Approaches | Douglas Gruner | 2022 | Y | Y | Y | Y | NA | NA | Y |
| 2 | Leadership curricula and assessment in Australian and New Zealand medical schools | Simone Jacquelyn Ross | 2021 | Y | Y | Y | Y | NA | NA | NA |
| 3 | The Pandemic Leadership Model: A Study of Medical Student Values During COVID-19 | Alec Bernard | 2021 | Y | Y | Y | Y | NA | NA | N |
| 4 | Contextual Analysis of Stakeholder Opinion on Management and Leadership Competencies for Undergraduate Medical Education: Informing Course Design. | Nisreen Rajeh | 2020 | Y | Y | Y | Y | NA | NA | Y |
| 5 | A student-led curriculum framework for homeless and vulnerably housed populations | Syeda Shanza Hashmi. | 2020 | Y | Y | Y | Y | NA | NA | N |
| 6 | A first-year leadership programme for medical students | Heather Wagenschutz | 2019 | Y | Y | Y | Y | Y | Y | Y |
| 7 | Medical Student Consulting: Providing Students Leadership and Business Opportunities While Positively Impacting the Community | David S. Portney | 2019 | Y | Y | Y | Y | N | Y | N |
| 8 | Medical Student Leader Performance in an Applied Medical Field Practicum. | Erin S. Barry | 2019 | Y | Y | Y | Y | Y | Y | Y |
| 9 | Preparing Medical Students to Be Physician Leaders: A Leadership Training Program for Students Designed and Led by Students | Kristen Richard | 2019 | Y | Y | Y | Y | Y | N | Y |
| 10 | Identification and evaluation of the core elements of character education for medical students in Korea. | Yera Hur | 2019 | Y | Y | Y | NA | NA | NA | Y |
| 11 | Leadership and Academic Medicine: Preparing Medical Students and Residents to Be Effective Leaders for the 21st Century. | Joel Dickerman | 2018 | Y | Y | Y | Y | Y | Y | Y |
| 12 | On the road to becoming a responsible leader: A simulation-based training approach for final year medical students | Marion Schmidt-Huber | 2017 | Y | Y | Y | Y | Y | N | Y |
| 13 | Health Systems Science Curricula in Undergraduate Medical Education: Identifying and Defining a Potential Curricular Framework | Jed D. Gonzalo | 2017 | Y | Y | Y | Y | NA | NA | Y |
| 14 | The Health Professions Education Pathway: Preparing Students, Residents, and Fellows to Become Future Educators | H. Carrie Chen | 2017 | Y | Y | Y | Y | Y | Y | Y |
| 15 | Leadership and management in UK medical school curricula | Richard Jefferies | 2016 | Y | N | Y | Y | NA | NA | NA |
| 16 | Aspects of development of leader creative thinking of medical student at the undergraduate level of medical education | Aniuta Sydorchuk | 2016 | Y | N | Y | Y | NA | NA | N |
| 17 | Defining the structure of undergraduate medical leadership and management teaching and assessment in the UK. | Thomas D Stringfellow | 2014 | Y | Y | Y | Y | NA | NA | NA |
| 18 | A medical student leadership course led to teamwork, advocacy, and mindfulness. | Carole M. Warde | 2014 | Y | Y | Y | Y | N | N | Y |
| 19 | Promoting medical students’ reflection on competencies to advance a global health equities curriculum. | Patricia B Mullan | 2014 | Y | Y | Y | Y | NA | NA | NA |
| 20 | Leadership and management in the undergraduate medical curriculum: a qualitative study of students’ attitudes and opinions at one UK medical school | Thelma Quince | 2014 | Y | Y | Y | Y | NA | NA | NA |
| 21 | In search for a public health leadership competency framework to support leadership curriculum-a consensus study | Katarzyna Czabanowska | 2013 | Y | Y | Y | Y | Y | Y | Y |
| 22 | Preparing students to be academicians: a national student-led summer program in teaching, leadership, scholarship, and academic medical career-building | Michelle M. Coleman | 2012 | Y | Y | Y | Y | Y | N | N |
| 23 | Leadership curriculum in undergraduate medical education: a study of student and faculty perspectives | Prathibha Varkey | 2009 | Y | N | Y | Y | NA | NA | NA |
| First author | UME | Residency -ME- | Fellow-Ship -ME- | Nursing -IPE- | Dentistry -IPE- | Pharmacy -IPE- | Physical Therapy -IPE- | Social Work -IPE- | Micro-Biology -IPE- | Master -IPE or TPE- | PhD -IPE or TPE- | Staff -IPE or TPE- |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gruner | X | |||||||||||
| Ross | X | |||||||||||
| Bernard | X | |||||||||||
| Rajeh | X | |||||||||||
| Hashmi | X | |||||||||||
| Wagenschutz | X | X | X | X | ||||||||
| Portney | X | |||||||||||
| Barry | X | X | ||||||||||
| Richard | X | |||||||||||
| Hur | X | X | ||||||||||
| Dickerman | X | X | X | X | ||||||||
| Schmidt-Huber | X | |||||||||||
| Gonzalo | X | |||||||||||
| Chen | X | X | X | X | X | X | X | |||||
| Jefferies | X | |||||||||||
| Sydorchuk | X | |||||||||||
| Stringfellow | X | |||||||||||
| Warde | X | |||||||||||
| Mullan | X | |||||||||||
| Quince | X | |||||||||||
| Czabanowska | X | X | X | X | X | |||||||
| Coleman | X | |||||||||||
| Varkey | X |
| # | Definition | Key Words | Learner |
|---|---|---|---|
| 1 | As Leaders, physicians engage with others to contribute to a vision of a high-quality health care system and take responsibility for the delivery of excellent patient care through their activities as clinicians, administrators, scholars, or teachers. | -Leader | UME |
| 2 | Leaders have a vision | -Leader | Medical education |
| 3 | The whole concept of personal leadership, all the traits of personal leadership, starting from having the insight, having the trait of how a person can contribute to an institutional vision, a country vision, and the traits of time management. | -Leadership | Medical education |
| 4 | A leader should inspire people to move on, to do the job well, to have a good practice, to become the best they can be as a group working together toward a common goal | -Leader | Medical education |
| 5 | develop humble, reflective leaders who identify problems, work collaboratively with teams to create solutions, and create a vision for positive change | -Leader. | Interprofessional education |
| 6 | Leadership is defined as influence on individuals and groups by enhancing behaviors (actions), cognitions (perceptions, thoughts, and beliefs), and motivations (why people act and think as they do) to achieve goals that benefit the individuals and groups. Leaders set the vision and inspire followers | -Leadership - Leader | Interprofessional education |
| 7 | Leadership, therefore, refers to social psychological processes, interpersonal and group dynamics, and influence on all aspects of psychology (behaviors, cognitions, and motivations) of others. Leaders are the drivers of these processes who adjust to goals, individuals, and context | -Leadership -Leader | Interprofessional education |
| 8 | Leadership is… inspiring others to work together to achieve a common vision | -Leadership | UME |
| 9 | Attitudes and ability to reflect on, examine, and endure in difficult situations, to view health care in its social context, and to reach agreement with other members of an organization | -Patience -Leadership | Medical education |
| 10 | Origin of words lead, leader, leadership is “laid”, alluding “path” or “road” | -Lead -Leader -Leadership | Medical education |
| 11 | verb læden = “to travel”. A leader is an individual who shows other travelers the path ahead | -Leader | Medical education |
| 12 | Leadership has been described as the behavior of an individual when directing the activities of a group toward a shared goal | -Leadership | Medical education |
| 13 | The new healthcare leader is not fearful or resistant in the face of change, but rather embraces change as a means to innovate. The leader is able to apply leadership skills to all aspects of health care, from education to delivery of care | -Leader | Medical education |
| 14 | leadership produces change and movement | -Leadership | Medical education |
| 15 1 | In this context, the concept of leadership comprises exerting conscious, goal-oriented social influence on people (subordinates, colleagues and teams) for the purpose of performing shared tasks in pursuit of common goals, and focuses on leading | -Leadership | UME |
| 16 | Lateral leadership (exerting influence without formal power) and disciplinary leadership functions as well | -Lateral Leadership | UME |
| 17 | Ethical leadership emphasizes the responsibility of leaders for human dignity and, at the same time, strives for excellent performance. | -Ethical Leadership | UME |
| 18 | All issues related to the ability to inspire motivation in others to create goals toward a desirable vision. In the context of undergraduate medical education, leadership pertains to team-based care, quality improvement projects, etc | -Leadership -Change Agency | UME |
| 19 | All issues related to ethical behavior and professionalism, including conduct, congruent with generally accepted moral principles and values and with professional guidelines based on those principles and values. This definition includes general leadership ethics, such as honesty and responsibility, as well as ethics and professionalism specific to the HSS domains | -Professionalism -ethics (Leadership) | UME |
| 20 | Educational Leadership as a domain that encompasses academic positions that encompass formal administrative responsibilities for educational programs (e.g., residency training directors, directors of medical student education in specific departments, etc.).] | -Educational Leadership | Medical Education |
| 21 | Leadership being a responsibility for all staff at every level through effective teamwork and the continuous development of personal MLM attributes and behaviours | -Shared Leadership | UME |
| 22 | A student’s capacity for leadership and resilience stems from the intrapersonal relationship one has with oneself; interpersonal relationships; and relationships within organizations that build partnership, respect, and change capacity. | -Leadership -Resilience stems | UME |
| 23 | We base the programme on the idea of influencing others to work together towards achieving a common goal, which is improved health and well-being of the population through transformation and change. The leadership training is competency-based supported by a framework and self-assessment including the following areas: system thinking, emotional intelligence, collaboration and teamwork, organisational learning and development, leading change, ethical and professional practice | Leadership | Trans-professional |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Feria, P.; Czabanowska, K.; Babich, S.; Rodríguez-Sánchez, D.; Carreño Hernández, F.L.; Hernández Flórez, L.J. Defining Leadership in Undergraduate Medical Education, Networks, and Instructors: A Scoping Review. Int. Med. Educ. 2023, 2, 49-70. https://doi.org/10.3390/ime2010006
Rodríguez-Feria P, Czabanowska K, Babich S, Rodríguez-Sánchez D, Carreño Hernández FL, Hernández Flórez LJ. Defining Leadership in Undergraduate Medical Education, Networks, and Instructors: A Scoping Review. International Medical Education. 2023; 2(1):49-70. https://doi.org/10.3390/ime2010006
Chicago/Turabian StyleRodríguez-Feria, Pablo, Katarzyna Czabanowska, Suzanne Babich, Daniela Rodríguez-Sánchez, Fredy Leonardo Carreño Hernández, and Luis Jorge Hernández Flórez. 2023. "Defining Leadership in Undergraduate Medical Education, Networks, and Instructors: A Scoping Review" International Medical Education 2, no. 1: 49-70. https://doi.org/10.3390/ime2010006
APA StyleRodríguez-Feria, P., Czabanowska, K., Babich, S., Rodríguez-Sánchez, D., Carreño Hernández, F. L., & Hernández Flórez, L. J. (2023). Defining Leadership in Undergraduate Medical Education, Networks, and Instructors: A Scoping Review. International Medical Education, 2(1), 49-70. https://doi.org/10.3390/ime2010006







