Neck Pain in Dental Education: A Cross-Sectional Analysis of Neck Strength Differences
Abstract
1. Introduction
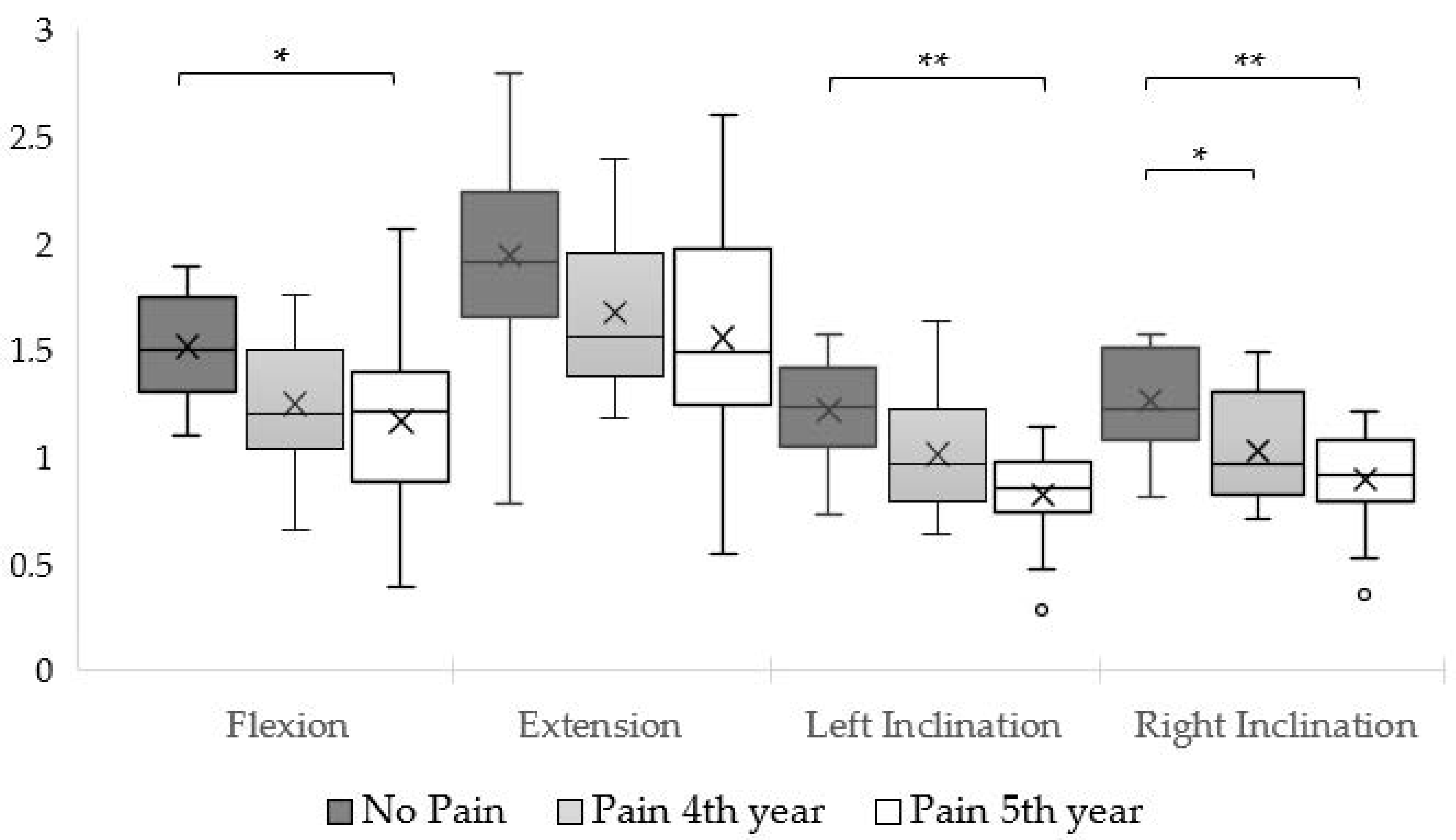
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Participants
4.3. Procedure
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ANOVA | Analysis of Variance |
| BMI | Body Mass Index |
| CEEM | Egas Moniz School of Health & Science Ethics Committee |
| F/E | Flexion/Extension ratio |
| HHD | Hand-Held Dynamometer |
| L/R | Left lateral flexion/Right lateral flexion ratio |
| MVIC | Maximal Voluntary Isometric Contraction |
| NMQ | Nordic Musculoskeletal Questionnaire |
| NP | No Pain (group) |
| P4 | Pain–4th year (group) |
| P5 | Pain–5th year (group) |
| SD | Standard Deviation |
| STROBE | Strengthening the Reporting of Observational Studies in Epidemiology |
| WMSDs | Work-Related Musculoskeletal Disorders |
References
- Lietz, J.; Kozak, A.; Nienhaus, A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: A systematic literature review and meta-analysis. PLoS ONE 2018, 13, e0208628. [Google Scholar] [CrossRef]
- Hayes, M.; Cockrell, D.; Smith, D. A systematic review of musculoskeletal disorders among dental professionals. Int. J. Dent. Hyg. 2009, 7, 159–165. [Google Scholar] [CrossRef]
- Ohlendorf, D.; Naser, A.; Haas, Y.; Haenel, J.; Fraeulin, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brueggmann, D. Prevalence of musculoskeletal disorders among dentists and dental students in Germany. Int. J. Environ. Res. Public Health 2020, 17, 8740. [Google Scholar] [CrossRef]
- Kapitán, M.; Pilbauerová, N.; Vavřičková, L.; Šustová, Z.; Machač, S. Prevalence of musculoskeletal disorders symptoms among Czech dental students. Part 1: A questionnaire survey. Acta Med. 2019, 61, 131–136. [Google Scholar] [CrossRef]
- Aboalshamat, K.T. Nordic assessment of occupational disorders among dental students and dentists in Saudi Arabia. J. Int. Soc. Prev. Community Dent. 2020, 10, 561. [Google Scholar] [CrossRef]
- Almeida, M.B.; Póvoa, R.; Tavares, D.; Alves, P.M.; Oliveira, R. Prevalence of musculoskeletal disorders among dental students: A systematic review and meta-analysis. Heliyon 2023, 9, e19956. [Google Scholar] [CrossRef]
- Suganthirababu, P.; Parveen, A.; Mohan Krishna, P.; Sivaram, B.; Kumaresan, A.; Srinivasan, V.; Vishnuram, S.; Alagesan, J.; Prathap, L. Prevalence of work-related musculoskeletal disorders among health care professionals: A systematic review. Work 2022, 74, 455–467. [Google Scholar] [CrossRef]
- Santos, R.R.; Garbin, C.A.S.; Batista, J.A.; Saliba, T.A.; Garbin, A.J.I. Prevalence of musculoskeletal pain in dental students and associated factors. Braz. J. Oral. Sci. 2019, 18, e191668. [Google Scholar] [CrossRef]
- Felemban, R.A.; Sofi, R.A.; Alhebshi, S.A.; Alharbi, S.G.; Farsi, N.J.; Abduljabbar, F.H.; Farsi, J.M. Prevalence and predictors of musculoskeletal pain among undergraduate students at a dental school in Saudi Arabia. Clin. Cosmet. Investig. Dent. 2021, 13, 39–46. [Google Scholar] [CrossRef]
- Peck, C.; Murray, G.; Gerzina, T. How does pain affect jaw muscle activity? The Integrated Pain Adaptation Model. Aust. Dent. J. 2008, 53, 201–207. [Google Scholar] [CrossRef]
- Murray, G.M.; Peck, C.C. Orofacial pain and jaw muscle activity: A new model. J. Orofac. Pain 2007, 21, 263–278; discussion 279–288. [Google Scholar]
- Wytrążek, M.; Huber, J.; Lisiński, P. Changes in muscle activity determine progression of clinical symptoms in patients with chronic spine-related muscle pain. A complex clinical and neurophysiological approach. Funct. Neurol. 2011, 26, 141. [Google Scholar] [PubMed]
- O’Leary, S.; Falla, D.; Jull, G. The relationship between superficial muscle activity during the cranio-cervical flexion test and clinical features in patients with chronic neck pain. Man. Ther. 2011, 16, 452–455. [Google Scholar] [CrossRef] [PubMed]
- Gilchrist, I.; Storr, M.; Chapman, E.; Pelland, L. Neck muscle strength training in the risk management of concussion in contact sports: Critical appraisal of application to practice. J. Athl. Enhanc. 2015, 19, 2. [Google Scholar] [CrossRef]
- Park, K.-N.; Jung, D.-Y.; Kim, S.-H. Trapezius and serratus anterior muscle strength in violinists with unilateral neck pain. J. Back Musculoskelet. Rehabil. 2020, 33, 631–636. [Google Scholar] [CrossRef]
- Kahlaee, A.H.; Ghamkhar, L.; Nourbakhsh, M.R.; Arab, A.M. Strength and Range of Motion in the Contralateral Side to Pain and Pain-Free Regions in Unilateral Chronic Nonspecific Neck Pain Patients. Am. J. Phys. Med. Rehabil. 2020, 99, 133–141. [Google Scholar] [CrossRef]
- Jull, G.A.; O’leary, S.P.; Falla, D.L. Clinical assessment of the deep cervical flexor muscles: The craniocervical flexion test. J. Manip. Physiol. Ther. 2008, 31, 525–533. [Google Scholar] [CrossRef]
- Ylinen, J.; Takala, E.-P.; Kautiainen, H.; Nykänen, M.; Häkkinen, A.; Pohjolainen, T.; Karppi, S.-L.; Airaksinen, O. Association of neck pain, disability and neck pain during maximal effort with neck muscle strength and range of movement in women with chronic non-specific neck pain. Eur. J. Pain 2004, 8, 473–478. [Google Scholar] [CrossRef]
- Wang, D.M.; Li, C.; Hatchard, N.; Chang Chien, G.C.; Alm, J. Lower trapezius muscle function in people with and without shoulder and neck pain: A systematic review. J. Osteopath. Med. 2023, 123, 73–89. [Google Scholar] [CrossRef]
- Almeida, M.B.; Moreira, M.; Moleirinho-Alves, P.; Oliveira, R. Neck Strength Variations in Dental Students with and without Neck Pain: A Longitudinal Study. Appl. Sci. 2024, 14, 8205. [Google Scholar] [CrossRef]
- Falla, D.; Jull, G.; Hodges, P. Training the cervical muscles with prescribed motor tasks does not change muscle activation during a functional activity. Man. Ther. 2008, 13, 507–512. [Google Scholar] [CrossRef]
- Tsang, S.M.; Szeto, G.P.; Lee, R.Y. Altered spinal kinematics and muscle recruitment pattern of the cervical and thoracic spine in people with chronic neck pain during functional task. J. Electromyogr. Kinesiol. 2014, 24, 104–113. [Google Scholar] [CrossRef]
- Almeida, M.B.D.; Moreira, M.; Miranda-Oliveira, P.; Moreira, J.; Família, C.; Vaz, J.R.; Moleirinho-Alves, P.; Oliveira, R. Evolving Dynamics of Neck Muscle Activation Patterns in Dental Students: A Longitudinal Study. Sensors 2024, 24, 5689. [Google Scholar] [CrossRef]
- Tudini, F.; Myers, B.; Bohannon, R. Reliability and validity of measurements of cervical retraction strength obtained with a hand-held dynamometer. J. Man. Manip. Ther. 2019, 27, 222–228. [Google Scholar] [CrossRef]
- Kim, I.H.; Geiger-Brown, J.; Trinkoff, A.; Muntaner, C. Physically demanding workloads and the risks of musculoskeletal disorders in homecare workers in the USA. Health Soc. Care Community 2010, 18, 445–455. [Google Scholar] [CrossRef]
- Mousavi, S.J.; Olyaei, G.R.; Talebian, S.; Sanjari, M.A.; Parnianpour, M. The effect of angle and level of exertion on trunk neuromuscular performance during multidirectional isometric activities. Spine 2009, 34, E170–E177. [Google Scholar] [CrossRef]
- Strimpakos, N. The assessment of the cervical spine. Part 2: Strength and endurance/fatigue. J. Bodyw. Mov. Ther. 2011, 15, 417–430. [Google Scholar] [CrossRef]
- Chamorro, C.; Arancibia, M.; Trigo, B.; Arias-Poblete, L.; Jerez-Mayorga, D. Absolute Reliability and Concurrent Validity of Hand-Held Dynamometry in Shoulder Rotator Strength Assessment: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 9293. [Google Scholar] [CrossRef]
- Mentiplay, B.F.; Perraton, L.G.; Bower, K.J.; Adair, B.; Pua, Y.-H.; Williams, G.P.; McGaw, R.; Clark, R.A. Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: A reliability and validity study. PLoS ONE 2015, 10, e0140822. [Google Scholar] [CrossRef]
- Almeida, M.B.; Oliveira, C.; Ornelas, G.; Soares, T.; Souto, J.; Póvoa, R.; Ferreira, L.M.A.; Ricci-Vitor, A.L. Intra-Rater and Inter-Rater Reliability of the Kinvent Hand-Held Dynamometer in Young Adults. Med. Sci. Forum 2023, 22, 12. [Google Scholar] [CrossRef]
- Vannebo, K.T.; Iversen, V.M.; Fimland, M.S.; Mork, P.J. Test-retest reliability of a handheld dynamometer for measurement of isometric cervical muscle strength. J. Back Musculoskelet. Rehabil. 2018, 31, 557–565. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Tudini, F. Magnitude, validity and responsiveness of dynamometer measured neck retraction strength in patients referred with neck pain to out-patient physical therapy. J. Phys. Ther. Sci. 2022, 34, 694–696. [Google Scholar] [CrossRef]
- Catenaccio, E.; Mu, W.; Kaplan, A.; Fleysher, R.; Kim, N.; Bachrach, T.; Zughaft Sears, M.; Jaspan, O.; Caccese, J.; Kim, M. Characterization of neck strength in healthy young adults. Pm&r 2017, 9, 884–891. [Google Scholar] [CrossRef]
- Faust, A.M.; Ahmed, S.N.; Johnston, L.B.; Harmon, J.B. Teaching methodologies for improving dental students’ implementation of ergonomic operator and patient positioning. J. Dent. Educ. 2021, 85, 370–378. [Google Scholar] [CrossRef]
- de Almeida, M.B.; Moleirinho-Alves, P.; Oliveira, R. Work-related musculoskeletal disorders among dental students: A cross-sectional study integrating the pain adaptation model. J. Public Health 2024. [Google Scholar] [CrossRef]
- Koni, A.; Kufersin, M.; Ronchese, F.; Travan, M.; Cadenaro, M.; Filon, F.L. Approach to prevention of musculoskeletal symptoms in dental students: An interventional study. Med. Lav. 2018, 109, 276. [Google Scholar] [CrossRef] [PubMed]
- Webb, R.; Brammah, T.; Lunt, M.; Urwin, M.; Allison, T.; Symmons, D. Prevalence and predictors of intense, chronic, and disabling neck and back pain in the UK general population. Spine 2003, 28, 1195–1202. [Google Scholar] [CrossRef]
- Moreira, J.; Miguel, S.; Delgado, B.; Boto, P. Patient-reported outcome measures in rehabilitation after knee surgery: A rapid systematic review. J. Public Health 2024. [Google Scholar] [CrossRef]
- Devecchi, V.; Rushton, A.B.; Gallina, A.; Heneghan, N.R.; Falla, D. Are neuromuscular adaptations present in people with recurrent spinal pain during a period of remission? A systematic review. PLoS ONE 2021, 16, e0249220. [Google Scholar] [CrossRef]
- Oka, Y.; Jiroumaru, T.; Wachi, M.; Kida, N. Prevalence and treatment of chronic musculoskeletal pain focused on service gaps: A comparative analysis by age group and body part. PeerJ 2024, 12, e18389. [Google Scholar] [CrossRef] [PubMed]
- Geneen, L.J.; Moore, R.A.; Clarke, C.; Martin, D.; Colvin, L.A.; Smith, B.H. Physical activity and exercise for chronic pain in adults: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2017, 4, Cd011279. [Google Scholar] [CrossRef]
- Moreira, J.; Mesquita, M.; Flamínio, J.; Almeida, M.; Delgado, B.; Boto, P. Patient-reported outcome measures in knee injuries rehabilitation: A protocol for intervention. Methods X 2024, 12, 102647. [Google Scholar] [CrossRef]
- Almeida, M.B.; Moreira, M.; Moleirinho-Alves, P.; Raul, O. Neck pain in dental education: Analysis of neck strength differences. Mendeley Data 2023. [Google Scholar] [CrossRef]
- Lindstroem, R.; Graven-Nielsen, T.; Falla, D. Current Pain and Fear of Pain Contribute to Reduced Maximum Voluntary Contraction of Neck Muscles in Patients With Chronic Neck Pain. Arch. Phys. Med. Rehabil. 2012, 93, 2042–2048. [Google Scholar] [CrossRef]
- Karaağaç, A.; Arslan, S.A.; Keskin, E.D. Assessment of pain, scapulothoracic muscle strength, endurance and scapular dyskinesis in individuals with and without nonspecific chronic neck pain: A cross-sectional study. J. Bodyw. Mov. Ther. 2023, 35, 261–267. [Google Scholar] [CrossRef]
- Almeida, M.B.; Moreira, M.; Moreira, J.; Vaz, J.R.; Moleirinho-Alves, P.; Oliveira, R. The time-course changes in postural control variability between neck pain and asymptomatic dental students. Sci. Rep. 2024, 14, 31004. [Google Scholar] [CrossRef]
- Hidalgo, B.; Hall, T.; Bossert, J.; Dugeny, A.; Cagnie, B.; Pitance, L. The efficacy of manual therapy and exercise for treating non-specific neck pain: A systematic review. J. Back Musculoskelet. Rehabil. 2017, 30, 1149–1169. [Google Scholar] [CrossRef]
- Lluch, E.; Nijs, J.; De Kooning, M.; Van Dyck, D.; Vanderstraeten, R.; Struyf, F.; Roussel, N.A. Prevalence, incidence, localization, and pathophysiology of myofascial trigger points in patients with spinal pain: A systematic literature review. J. Manip. Physiol. Ther. 2015, 38, 587–600. [Google Scholar] [CrossRef]
- Jull, G.; Sterling, M.; Falla, D.; Treleaven, J.; O’Leary, S. Whiplash, Headache, and Neck Pain: Research-Based Directions for Physical Therapies; Elsevier Health Sciences: London, UK; Oxford, UK, 2008. [Google Scholar]
- Madeleine, P. On functional motor adaptations: From the quantification of motor strategies to the prevention of musculoskeletal disorders in the neck–shoulder region. Acta Physiol. 2010, 199, 1–46. [Google Scholar] [CrossRef]
- Bonilla-Barba, L.; Florencio, L.L.; Rodríguez-Jiménez, J.; Falla, D.; Fernández-de-Las-Peñas, C.; Ortega-Santiago, R. Women with mechanical neck pain exhibit increased activation of their superficial neck extensors when performing the cranio-cervical flexion test. Musculoskelet. Sci. Pr. 2020, 49, 102222. [Google Scholar] [CrossRef]
- O’leary, S.; Falla, D.; Elliott, J.M.; Jull, G. Muscle dysfunction in cervical spine pain: Implications for assessment and management. J. Orthop. Sports Phys. Ther. 2009, 39, 324–333. [Google Scholar] [CrossRef]
- Folland, J.P.; Williams, A.G. Morphological and neurological contributions to increased strength. Sports Med. 2007, 37, 145–168. [Google Scholar] [CrossRef]
- Benatto, M.T.; Florencio, L.L.; Bragatto, M.M.; Lodovichi, S.S.; Dach, F.; Bevilaqua-Grossi, D. Extensor/flexor ratio of neck muscle strength and electromyographic activity of individuals with migraine: A cross-sectional study. Eur. Spine J. 2019, 28, 2311–2318. [Google Scholar] [CrossRef]
- Gabriel, D.A.; Kamen, G.; Frost, G. Neural adaptations to resistive exercise: Mechanisms and recommendations for training practices. Sports Med. 2006, 36, 133–149. [Google Scholar] [CrossRef]
- Yajima, H.; Nobe, R.; Takayama, M.; Takakura, N. The mode of activity of cervical extensors and flexors in healthy adults: A cross-sectional study. Medicina 2022, 58, 728. [Google Scholar] [CrossRef]
- Hanvold, T.N.; Wærsted, M.; Mengshoel, A.M.; Bjertness, E.; Stigum, H.; Twisk, J.; Veiersted, K.B. The effect of work-related sustained trapezius muscle activity on the development of neck and shoulder pain among young adults. Scand. J. Work. Environ. Health 2013, 39, 390–400. [Google Scholar] [CrossRef]
- Petersen, S.M.; Wyatt, S.N. Lower trapezius muscle strength in individuals with unilateral neck pain. J. Orthop. Sports Phys. Ther. 2011, 41, 260–265. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Krause, D.A.; Hansen, K.A.; Hastreiter, M.J.; Kuhn, T.N.; Peichel, M.L.; Hollman, J.H. A comparison of various cervical muscle strength testing methods using a handheld dynamometer. Sports Health 2019, 11, 59–63. [Google Scholar] [CrossRef]
- Mesquita, C.C.; Ribeiro, J.C.; Moreira, P. Portuguese version of the standardized Nordic musculoskeletal questionnaire: Cross cultural and reliability. J. Public Health 2010, 18, 461–466. [Google Scholar] [CrossRef]
- Peek, K. The measurement of neck strength: A guide for sports medicine clinicians. Phys. Ther. Sport 2022, 55, 282–288. [Google Scholar] [CrossRef]
- Jaric, S. Muscle strength testing: Use of normalisation for body size. Sports Med. 2002, 32, 615–631. [Google Scholar] [CrossRef] [PubMed]

| No Pain (n = 15) | Pain—4th Year (n = 14) | Pain—5th Year (n = 14) | |||||
|---|---|---|---|---|---|---|---|
| Mean (+SD) | [Range] | Mean (+SD) | [Range] | Mean (+SD) | [Range] | p | |
| Age (years) | 22.9 (±1.49) | [20–26] | 22.8 (±2.26) | [20–28] | 24.6 (±3.48) | [22–30] | 0.088 a |
| Height (cm) | 169.3 (±9.08) | [156–183] | 168.1 (±11.19) | [152–196] | 170.9 (±9.4) | [153–190] | 0.751 a |
| Body Mass (kg) | 63.7 (±3.44) | [46–88] | 61.7 (±13.1) | [46–96] | 58.2 (±10.12) | [43–83] | 0.338 a |
| BMI (kg/m2) | 22.0 (±3.01) | [18.1–26.9] | 21.6 (±2.33) | [17.1–25.0] | 19.8 (±1.96) | [17.4–23.0] | 0.103 a |
| Sex % (n) | Male 46.7% (7) Female 53.3% (8) | Male 21.4% (3) Female 78.6% (11) | Male 21.4% (3) Female 78.6% (11) | 0.229 b | |||
| Ratios | Reference [33] | No Pain | P4 | P5 | ||||
|---|---|---|---|---|---|---|---|---|
| F/E | L/R | F/E | L/R | F/E | L/R | F/E | L/R | |
| Male | 0.64 | 1.00 | 0.73 | 0.98 | 0.66 | 1.02 | 0.68 | 0.91 |
| Female | 0.64 | 0.98 | 0.81 | 0.99 | 0.78 | 0.97 | 0.78 | 0.92 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almeida, M.B.; Moreira, M.; Moleirinho-Alves, P.; Oliveira, R. Neck Pain in Dental Education: A Cross-Sectional Analysis of Neck Strength Differences. Muscles 2025, 4, 40. https://doi.org/10.3390/muscles4030040
Almeida MB, Moreira M, Moleirinho-Alves P, Oliveira R. Neck Pain in Dental Education: A Cross-Sectional Analysis of Neck Strength Differences. Muscles. 2025; 4(3):40. https://doi.org/10.3390/muscles4030040
Chicago/Turabian StyleAlmeida, Manuel B., Marion Moreira, Paula Moleirinho-Alves, and Raúl Oliveira. 2025. "Neck Pain in Dental Education: A Cross-Sectional Analysis of Neck Strength Differences" Muscles 4, no. 3: 40. https://doi.org/10.3390/muscles4030040
APA StyleAlmeida, M. B., Moreira, M., Moleirinho-Alves, P., & Oliveira, R. (2025). Neck Pain in Dental Education: A Cross-Sectional Analysis of Neck Strength Differences. Muscles, 4(3), 40. https://doi.org/10.3390/muscles4030040







