Myofunctional Therapy in Atypical Swallowing: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol
2.2. Eligibility Criteria
2.3. Search Strategy and Information Sources
2.4. Study Selection and Data Extraction
3. Results
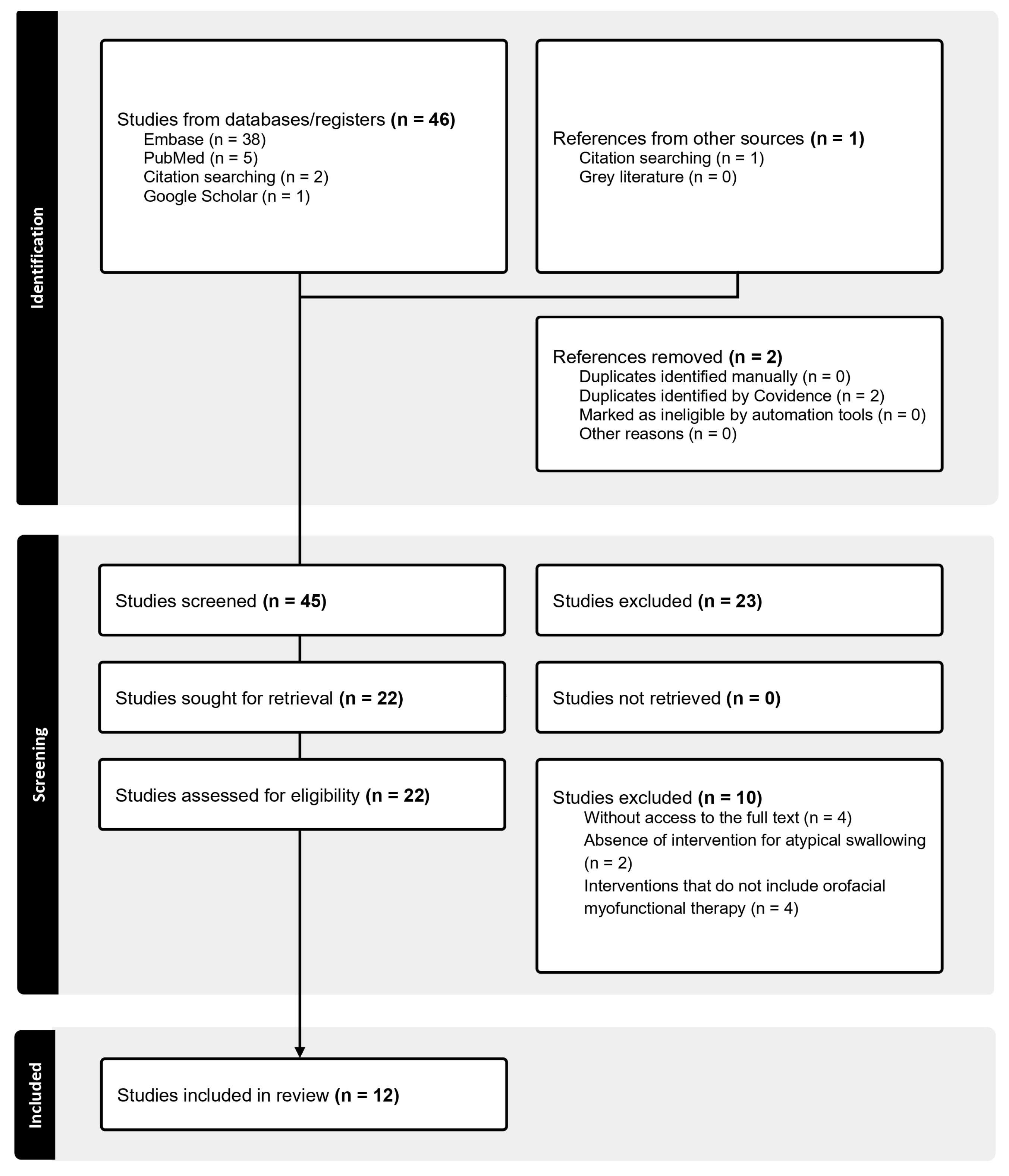
3.1. Selection of Evidence Sources
3.2. Characteristics of the Evidence Sources
3.3. Results of Individual Evidence Sources
3.4. Synthesis of Results
| Origin | Participants | General Description of the Study | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First Author | Year | Country | Institution of Origin | N° | Age (Years) | M | F | Swallowing Diagnosis | Dental Diagnosis | Objective | Study Type | Methodological Design | Main Findings |
| Zimmerman, J.B. [15] | 1989 | United States | NR | 1 | 13 | 0 | 1 | Bilateral tongue thrust with an anterior component | Open Bite | To describe the coordination between OMT and orthodontics in a case of AOB | Descriptive case report | Longitudinal single-case design with follow-ups at 1, 3, 6, and 12 months | OMT helped improve tongue posture and swallowing pattern, reducing tongue thrust and stabilizing orthodontic treatment |
| Gommerman, S.L. [23] | 1995 | Canada | Capital Health Authority, University of Alberta | 1 | 16 | 0 | 1 | Tongue thrust swallowing pattern | NR | To investigate the effects of OMT on tongue thrust swallowing and interdental sibilant distortion | Descriptive case report | Single-case pre-post design with 6-month follow-up | Significant improvements in swallowing, but not in the production of sibilant sounds after OMT |
| Cayley, A.S [24] | 2000 | Australia | Orthodontic Department, Perth Dental Hospital | 8 | 9.08–11.75 | 8 | 0 | Tongue thrust swallowing pattern | AOB | To assess the effect of tongue re-education therapy on tongue function and dentofacial form in patients with AOB | Quasi-experimental | Prospective single-group pre-post design | OMT showed partial effectiveness in enhancing swallowing function and contributing to the reduction in anterior open bite |
| Saccomanno, S. [18] | 2012 | Italy | Catholic University A. Gemelli | 23 | 5–17 | 10 | 13 | AS | NR | To analyze the causal relationship between malocclusion and oral muscle dysfunction, and the impact of OMT | Quasi-experimental | Prospective pre-post design | Patients who received OMT showed increased orbicularis strength. sEMG analysis indicated muscle activity imbalances related to bite type in skeletal Class I and II cases |
| Saccomanno, S. [19] | 2014 | Italy | Catholic University A. Gemelli | 3 | 8–13 | 2 | 1 | AS (lateral tongue); AS (anterior tongue); AS (anterior tongue) | Class II, lateral open bite AOB; Class II, AOB and maxillary contraction | To evaluate the effectiveness of OMT combined with orthodontics in patients with oral bad habits (thumb sucking, OB, AS and labial interposition) | Descriptive case report | Multiple single-case pre-post design with 1-year follow-up | The combination of orthodontics and OMT was effective in correcting oral habits and malocclusions |
| Van Dyck, C. [25] | 2016 | Belgium | University Hospitals Leuven | 22 | 7.1–10.6 | 11 | 11 | Visceral swallowing pattern | AOB | To investigate the effects of OMT on tongue behavior in children with AOB and a visceral swallowing pattern | Randomized pilot study | RCT pilot with 6-month follow-up | OMT produced significant changes in tongue elevation strength, resting tongue posture, and tongue position during solid food swallowing, but further research is needed |
| Begnoni, G. [20] | 2020 | Italy | University of Milan | 15 | 17.72 ± 5.21 | 4 | 11 | AS | NR | To analyze the effects of OMT on muscular function and orofacial behavior in a group of patients with AS and second dentition completed | Quasi-experimental | Prospective single-group pre-post design | OMT allows the shortening of the muscular activation pattern and increases submental muscle activity |
| Mozzanica, F. [21] | 2020 | Italy | Department of Clinical Sciences and Community Health, University of Milan | 22 | 8.8 ± 1.1; 19.8 ± 4.7 | 9 | 13 | Tongue thrust | AOB, Overjet | To evaluate the effects of OMT using a validated instrument and to explore the influence of dentition on its efficacy | Quasi-experimental | Prospective single-group pre-post design | OMT improves swallowing and tongue strength in patients with tongue thrust, regardless of dentition type |
| Saccomanno, S. [22] | 2022 | Italy | Department of Health, Life and Environmental Science, University of L’Aquila | 1 | 9 | 0 | 1 | AS | AOB | To verify the advantages of OMT through the description of a clinical case treated only with this kind of therapy | Descriptive case report | Single-case pre-post design with 1-year follow-up | In one clinical case, OMT alone resolved AS and improved malocclusion, helping to stabilize the treatment |
| Debucean, D. [26] | 2023 | Romania | Faculty of Medicine and Pharmacy, University of Oradea | 61 | 12–26 | 25 | 36 | AS | NR | To explore whether OMT combined with a physiotherapeutic rehabilitation program for postural problems adds benefits to swallowing rehabilitation in healthy young population | Analytical observational | Prospective two-group pre-post design | The OMT combined with physiotherapy (manual therapy and Global Postural Re-education) proved to be more effective than single OMT |
| Noh, H. [16] | 2024 | South Korea | Department of Orthodontics, School of Dentistry, Kyungpook National University | 1 | 8 (follow-up until 23) | 0 | 1 | Infantile swallowing pattern | AOB, Class II (right side) | To correct AOB and tongue thrust through OMT and orthodontics | Descriptive case report | Single-case pre-post design with follow-up two months after bite stabilization | Controlling infantile swallowing is crucial for AOB treatment stability. The smile-clenching-swallowing exercise was key to long-term stability |
| Saccomanno, S. [17] | 2024 | Italy | University of L’Aquila | 6 | 7–14 | 5 | 1 | AS | NR | To explore the use of edible spread cream and small candies as tools to enhance motivation and compliance in children undergoing OMT for optimizing oral functions, including AS | Observational, retrospective | Retrospective single-group pre-post design | Young patients’ compliance limits OMT effectiveness in AS. Creative solutions like edible tools could improve cooperation and outcomes |
| First Author (Year) | In Situ Dental Treatment | Other Functional Disorders | Specific Activities for the Treatment | Total Therapy Duration | Therapy Session Duration | Therapy Frequency | Home Practice | Home Training Time | Therapist in Charge | Outcome Measures |
|---|---|---|---|---|---|---|---|---|---|---|
| Zimmerman (1989) [15] | Orthodontic retainer with lingual spurs after palatal expansion and headgear | SSD | 1. Increase awareness of the orofacial musculature to establish an appropriate resting posture of the tongue and lips, as well as functional movements during speech and swallowing. 2. Develop neuromuscular movement patterns to support conscious and coordinated swallowing of food, liquids, and saliva. 3. Assign therapeutic activities to promote the automatization of these motor skills, including speech therapy tasks to correct the interdental lisp. | 16 weeks | NR | Once a week for 5 weeks and then every 15 days | Yes | NR | Orofacial myologist | Clinical evaluation of oral rest posture, speech and swallowing function, and occlusion at follow-up. |
| Gommerman (1995) [23] | NR | OB, SSD | 1. Phase of OMT: 14 sessions included patient education on normal swallowing physiology, tongue strengthening exercises, and structured practice of correct swallows. Therapy incorporated modified versions of Garliner’s elastic swallowing exercises. 2. Phase of Articulation Treatment: 4 structured sessions followed a hierarchical model from isolated sounds to connected speech. Techniques included direct feedback, mental imagery, and structured self-monitoring with clinician-patient agreement on performance ratings. | 18 sessions | NR | NR | NR | NR | SLT | Swallowing measures: frequency of tongue thrust swallowing, duration of swallows and ease of swallowing. Tongue strength and endurance measured with IOPI. Sibilant distortion and labial diadochokinetic rate. |
| Cayley (2000) [24] | No treatment | NR | 1. Development of new muscle patterns needed as a foundation for proper swallowing and appropriate lip and tongue posture. 2. Swallowing training with liquids and semi-solids. | 8 weeks | 20 min | Every 15 days | NR | NR | SLT | Cephalometric analysis. Electropalatography to assess tongue-palate contact during speech and tongue position during the propulsive phase of saliva and water swallowing. |
| Saccomanno (2012) [18] | Rapid palatal expansion | OB | Therapeutic approach varied by malocclusion. For overbite ≤2 mm, a fixed grid/tongue crib was used to partially close the bite before starting speech therapy. For overbite >1 mm, speech therapy was applied. In overjet ≥4 mm, Class I patients received OMT only; Class II patients combined OMT with orthodontics. For overjet ≤0 mm, 20 speech therapy sessions plus daily home exercises preceded orthodontics. Exercises not specified. | 20 weeks | NR | Once a week | Yes | NR | SLT | Strength of the orbicularis muscle measured with a dynamometer; sEMG used to assess masseter and temporalis muscle activity. |
| Saccomanno (2014) [19] | The 2nd case was treated with a palatal crib and Fränkel III appliance. The third case was treated with rapid palatal expander, and with a removable orthodontic appliance. | OB, thumb sucking | Functional rehabilitation of the orofacial musculature. No specific exercises were described. Emphasis was placed on patient and family compliance with home therapy and interdisciplinary collaboration among professionals involved. | 20–30 sessions | NR | NR | NR | NR | SLT | Extraoral and intraoral photographs, plaster models, cephalometric analysis (lateral cephalogram), labial orbicular muscle contraction measurement, and tongue posture analysis. |
| Van Dyck (2016) [25] | Removable maxillary expansion device | SSD | Session 1. Explanation of treatment process and motivation; Sessions 2–3. Strengthen tongue and lip musculature; Sessions 4–5. Basis of the swallowing process; Session 6. Strengthen the anterior part of the tongue; Sessions 7–9. Strengthen the mid part of the tongue; Sessions 10–11. Strengthen the posterior part of the tongue; Sessions 13–14. Coordination of the total swallow movement; Sessions 15–16. Practice on conscious habit formation; Sessions 17–18. Practice on unconscious habit formation; Session 19. Control of physiological swallowing act; Session 20. Control of physiological swallowing act and follow-up. | 4–6 months | 30 or 60 min | Weekly or every 2 weeks | Yes | NR | OMT therapist | Maximum tongue elevation strength measured with IOPI. Functional characteristics such as resting tongue posture, swallowing pattern, and articulation were assessed through clinical evaluation performed by a speech pathologist. |
| Begnoni (2020) [20] | NR | NR | Myofunctional exercises based on the Garliner method. | 10 weeks | 45 min | Once a week | Yes | NR | SLT | Duration and intensity of electrical activation (sEMG) of masseter, temporal, and sublingual muscles. OMES protocol score. |
| Mozzanica (2020) [21] | No treatment | NR | Myofunctional exercises based on the Garliner method: Session 1: Education on physiology and dysfunctional habits, initial training on tongue posture. Session 2: Maintaining tongue posture for 5–10 min, practicing swallowing with 1–2 elastic bands, start strengthening. Session 3: Extending posture to 20 min, swallowing practice with bands and water retention, strengthening lips and masseter. Session 4: Maintaining posture for 30 min, swallowing with water and crackers, alternating chewing, strengthening exercises. Session 5: Maintaining posture for 45 min, correct swallowing during meals, reinforcement of tongue, lips, and masseter exercises. Session 6: Maintaining posture for 50 min with lip closure, swallowing during meals, strengthening continued. Session 7: Maintaining posture for 60 min, swallowing without bands, lip and masseter strengthening during meals. Session 8: Maintaining posture for 60 min, checking swallowing at two meals, establishing daily self-monitoring. Session 9: Maintaining posture twice daily for 15 min, monitoring swallowing at all meals, continuing self-recording. Session 10: Consolidating correct posture and swallowing habits with daily exercises and ongoing monitoring | 10 weeks | 45 min | Once a week | Yes | NR | SLT | OMES protocol scores. Tongue strength measured with IOPI. |
| Saccomanno (2022) [22] | No treatment | OB, difficulties chewing | 1. Teach the child the correct resting position of the tongue, ensuring that the tongue remains lightly in contact with the alveolar ridge (incisive papilla) at rest, with the teeth apart and the lips gently closed. 2. Stimulate the anterior, middle, and posterior parts of the tongue through targeted exercises to promote balanced activation and correct tongue posture against the palate. 3. Instruct the child to place the tip of the tongue on the incisive papilla and the rest of the tongue pressed flatly against the hard palate, maintaining this posture both at rest and during swallowing. 4. Perform an exercise in which the child holds an elastic band with the tip of the tongue on the retroincisal papilla, initially for 10 min per day with lips open and teeth apart, progressively increasing the time and advancing to perform the exercise with teeth slightly in contact and lips closed. | 3.5 months | NR | Once a week | Yes | 30 min, 3 times a day | SLT | Clinical evaluation, through the Rosenthal test, observation of swallowing patterns, assessment of masticatory function, and caregiver interviews. |
| Debucean (2023) [26] | NR | OB | 1. Nasal breathing. 2. Tongue training with a new resting position. Exercises stimulate the anterior tongue first, then the lateral parts, and finally the posterior tongue. 3. Restoration of lip seal. 4. Increase in facial muscle tone. 5. Restoration of soft palate tone. 6. Restructuring of proper swallowing. | 20 weeks | 40 min | Once a week | Yes | 15 min daily | SLT | OMES-Expanded protocol scores. |
| Noh (2024) [16] | Habit control devices (tongue cribs) and fixed orthodontic treatment with microimplants | NR | OMT includes smiling to naturally move the tongue backward, positioning the tongue against the hard palate, and swallowing by clenching the molars and pushing the tongue toward the palatal rugae without lip seal, aiming to establish a mature swallowing pattern and correct resting tongue posture. | NR | NR | NR | Yes | 10–20 min twice each day | Orthodontist | Closure of AOB, changes in tongue posture, post-treatment stability. |
| Saccomanno (2024) [17] | NR | OB | 1. Development of oral awareness. 2. Correction of resting tongue posture. 3. Specific exercises to strengthen the anterior, middle, and posterior parts of the tongue, as well as the lip muscles. 4. Swallowing training: patients practice swallowing with liquids, semi-solids, and finally solids to ensure physiological swallowing function. 5. Automation of the swallowing function. | 12 sessions over a 6-month period | 30 min | Every 15 days | Yes | 15 min daily | SLT | Increased strength of lip muscles measured with a dynamometer, appropriate tongue posture verified with fluorescein and photogrammetry. Level of cooperation assessed by the therapist. |
4. Discussion
4.1. Clinical Implications and Future Research Directions
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OMT | Orofacial myofunctional therapy |
| JBI | Joanna Briggs Institute |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Scoping Reviews |
| PCC | Population, concept, and context |
| AS | Atypical swallowing |
| OMES | Orofacial Myofunctional Evaluation Protocol With Scores |
| sEMG | Electromyography |
| SBFa | Brazilian Society of Speech-Language Pathology |
References
- Kumar, A.; Munirji, L.; Nayif, S.; Almotairy, N.; Grigoriadis, J.; Grigoriadis, A.; Trulsson, M. Motor performance and skill acquisition in oral motor training with exergames: A pilot study. Front. Aging Neurosci. 2022, 14, 730072. [Google Scholar] [CrossRef] [PubMed]
- Ambrocio, K.R.; Garand, K.L.; Roy, B.; Bhutada, A.M.; Malandraki, G.A. Diagnosing and managing dysphagia in inclusion body myositis: A systematic review. Rheumatology 2023, 62, 3227–3244. [Google Scholar] [CrossRef]
- Wei, K.C.; Wang, T.G.; Hsiao, M.Y. The cortical and subcortical neural control of swallowing: A narrative review. Dysphagia 2024, 39, 177–197. [Google Scholar] [CrossRef]
- Kletzien, H.; Cullins, M.J.; Connor, N.P. Age-related alterations in swallowing biomechanics. Exp. Gerontol. 2019, 118, 45–50. [Google Scholar] [CrossRef]
- Sayahpour, B.; Eslami, S.; Usherenko, R.; Jamilian, A.; Gonzalez, M.; Plein, N.; Grassia, V.; Nucci, L. Impact of dental midline shift on the perception of facial attractiveness in young adults. J. Clin. Med. 2024, 13, 3944. [Google Scholar] [CrossRef]
- Maspero, C.; Prevedello, C.; Giannini, L.; Galbiati, G.; Farronato, G. Atypical swallowing: A review. Minerva Stomatol. 2014, 63, 217–227. [Google Scholar] [PubMed]
- Bocquet, E.; Moreau, A.; Honoré, J.; Doual, A. La déglutition dysfonctionnelle a-t-elle une influence sur la posture? Orthod. Fr. 2008, 79, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Cenzato, N.; Iannotti, L.; Maspero, C. Open bite and atypical swallowing: Orthodontic treatment, speech therapy or both? A literature review. Eur. J. Paediatr. Dent. 2021, 22, 286–290. [Google Scholar] [CrossRef]
- Álvarez-Cervantes, J.E.; de Santiago-Tovar, J.R.; Monjaras-Ávila, A.J. Maloclusiones. Problema de salud bucodental. Revisión narrativa. Educ. Salud Bol. Cient. Inst. Cienc. Salud Univ. Autón Estado Hidalgo. 2023, 12, 79–86. [Google Scholar] [CrossRef]
- Gómez-González, C.; González-Mosquera, A.; Alkhraisat, M.H.; Anitua, E. Mouth breathing and its impact on atypical swallowing: A systematic review and meta-analysis. Dent. J. 2024, 12, 21. [Google Scholar] [CrossRef] [PubMed]
- Zaghi, S.; Shamtoob, S.; Peterson, C.; Christianson, L.; Valcu-Pinkerton, S.; Peeran, Z.; Fung, B.; Ng, D.K.; Jagomagi, T.; Archambault, N.; et al. Assessment of posterior tongue mobility using lingual-palatal suction: Progress towards a functional definition of ankyloglossia. J. Oral Rehabil. 2021, 48, 692–700. [Google Scholar] [CrossRef]
- Kilinc, D.D.; Mansiz, D. Myofunctional orofacial examination tests: A literature review. BMC Oral Health. 2023, 23, 350. [Google Scholar] [CrossRef]
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid.-Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, J.B. Orofacial myofunctional therapy for bilateral tongue posture and tongue thrust associated with open bite: A case report. Int. J. Orofac. Myol. Myofunct. Ther. 1989, 15, 5–9. [Google Scholar] [CrossRef]
- Noh, H.K.; Kim, H.J.; Park, H.S. A 17-year case report: Smile-clenching-swallowing exercise treatment to control tongue behavior and posture of anterior open bite. AJO-DO Clin. Companion 2024, 1, 51–63. [Google Scholar] [CrossRef]
- Saccomanno, S.; Quinzi, V.; Santori, F.; Pisaneschi, A.; Salvati, S.E.; Paskay, L.C.; Marci, M.C.; Marzo, G. Use of Edibles as Effective Tools in Myofunctional Therapy: A Pilot Study. Diagnostics 2024, 14, 251. [Google Scholar] [CrossRef]
- Saccomanno, S.; Antonini, G.L.; D’Alatri, L.; D’Angelantonio, M.; Fiorita, A.; Deli, R. Causal relationship between malocclusion and oral muscle dysfunction: A model of approach. Eur. J. Paediatr. Dent. 2012, 13, 321–323. [Google Scholar] [PubMed]
- Saccomanno, S.; Antonini, G.; D’Alatri, L.; D’Angeloantonio, M.; Fiorita, A.; Deli, R. Case report of patients treated with an orthodontic and myofunctional protocol. Eur. J. Paediatr. Dent. 2014, 15, 184–186. [Google Scholar] [PubMed]
- Begnoni, G.; Dellavia, C.; Pellegrini, G.; Scarponi, L.; Schindler, A.; Pizzorni, N. The efficacy of myofunctional therapy in patients with atypical swallowing. Eur. Arch. Otorhinolaryngol. 2020, 277, 2501–2511. [Google Scholar] [CrossRef]
- Mozzanica, F.; Pizzorni, N.; Scarponi, L.; Crimi, G.; Schindler, A. Impact of oral myofunctional therapy on orofacial myofunctional status and tongue strength in patients with tongue thrust. Folia Phoniatr. Logop. 2021, 73, 413–421. [Google Scholar] [CrossRef]
- Saccomanno, S.; Bovicelli, L.; Saran, S.; Vanella, V.; De Luca, M.; Capogreco, M.; Pirino, A.; Scoppa, F. The role of myofunctional therapy in the treatment of malocclusions: A clinical case The importance of differential diagnosis. J. Biol. Regul. Homeost. Agents 2022, 36, 157–164. [Google Scholar] [CrossRef]
- Gommerman, S.L.; Hodge, M.M. Effects of oral myofunctional therapy on swallowing and sibilant production. Int. J. Orofacial Myol. 1995, 21, 9–22. [Google Scholar] [CrossRef]
- Cayley, A.S.; Tindall, A.P.; Sampson, W.J.; Butcher, A.R. Electropalatographic and cephalometric assessment of myofunctional therapy in open-bite subjects. Australas. Orthod. J. 2000, 16, 23–33. [Google Scholar] [CrossRef]
- Van Dyck, C.; Dekeyser, A.; Vantricht, E.; Manders, E.; Goeleven, A.; Fieuws, S.; Willems, G. The effect of orofacial myofunctional treatment in children with anterior open bite and tongue dysfunction: A pilot study. Eur. J. Orthod. 2016, 38, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Debucean, D.; Mihaiu, J.; Maghiar, A.M.; Marcu, F.; Marcu, O.A. A multidisciplinary approach to swallowing rehabilitation in patients with forward head posture. Medicina 2023, 59, 1580. [Google Scholar] [CrossRef]
- de Oliveira, L.C.; Barbosa, L.N.; de Santana, I.H.; Sousa, C.F.; Dantas, M.A.; do Amaral, A.K.; Mélo, C.B.; Piagge, C.S.L.D. Intervenção com terapia miofuncional orofacial em idosos: Um estudo bibliométrico. Contrib. Cienc. Soc. 2023, 16, 8664–8677. [Google Scholar] [CrossRef]
- Kasparaviciene, K.; Sidlauskas, A.; Zasciurinskiene, E.; Vasiliauskas, A.; Juodzbalys, G.; Sidlauskas, M.; Marmaite, U. The prevalence of malocclusion and oral habits among 5–7-year-old children. Med. Sci. Monit. 2014, 20, 2036. [Google Scholar] [CrossRef]
- Sasigornwong, U.; Samnieng, P.; Puwanun, S.; Piyapattamin, T.; Tansalarak, R.; Nunthayanon, K.; Sirichom, S. Prevalence of abnormal oral habits and its relation to malocclusion in dental patients of the lower northern part of Thailand. Med. Dent. J. DFCT 2016, 36, 113–119. [Google Scholar]
- Simôes, W.A. Ortopedia Funcional de los Maxilares. A Través de la Rehabilitación Neuro-Oclusal; Artes Médicas: São Paulo, Brazil, 2004; Volume 1. [Google Scholar]
- Webster, M.J.; Elashoff, M.; Weickert, C.S. Molecular evidence that cortical synaptic growth predominates during the first decade of life in humans. Int. J. Dev. Neurosci. 2011, 29, 225–236. [Google Scholar] [CrossRef]
- Qaisar, R.; Bhaskaran, S.; Van Remmen, H. Muscle fiber type diversification during exercise and regeneration. Free Radic. Biol. Med. 2016, 98, 56–67. [Google Scholar] [CrossRef]
- Pabón, A.M.; Aristizábal, L.M.; Hernández, J.A. Tratamiento de la maloclusión clase III en el paciente pediátrico. reporte de caso. Rev. Odontopediatr. Latinoam. 2011, 1, 214–225. [Google Scholar] [CrossRef]
- Sandoval, P.; Bizcar, B. Beneficios de la implementación de ortodoncia interceptiva en la clínica infantil. Int. J. Odontostomatol. 2013, 7, 253–265. [Google Scholar] [CrossRef]
- Homem, M.A.; Vieira-Andrade, R.G.; Falci, S.G.; Ramos-Jorge, M.L.; Marques, L.S. Effectiveness of orofacial myofunctional therapy in orthodontic patients: A systematic review. Dent. Press J. Orthod. 2014, 19, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Sugawara, Y.; Ishihara, Y.; Takano-Yamamoto, T.; Yamashiro, T.; Kamioka, H. Orthodontic treatment of a patient with unilateral orofacial muscle dysfunction: The efficacy of myofunctional therapy on the treatment outcome. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 167–180. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Lai, G.; Wang, J. Effect of orofacial myofunctional therapy along with preformed appliances on patients with mixed dentition and lip incompetence. BMC Oral Health 2022, 22, 586. [Google Scholar] [CrossRef]
- AlQhtani; Abbooud, F.A.B. Evaluating the Impact of Myofunctional Therapy on Orthodontic Treatment Outcomes. J. Pharm. Bioallied Sci. 2024, 16, S2667–S2669. [Google Scholar] [CrossRef]
- Calisgan, E.; Talu, B.; Altun, O.; Dedeoglu, N.; Duman, B. The effects of proprioceptive neuromuscular facilitation, myofascial releasing maneuvers and home exercises on pain and jaw function in patients with bruxism. Med. Sci. 2018, 7, 617–621. [Google Scholar] [CrossRef]
- Paolucci, T.; Ferrillo, M.; Pezzi, L.; Agostini, F.; Di Matteo, A.; Prosperi, P.; Mangone, M.; Bernetti, A.; Spacone, A.; de Sire, A. Efficacy of orofacial myofunctional therapy combined with myofascial release in patients with mild obstructive sleep apnoea: A randomized controlled trial. J. Oral Rehabil. 2023, 50, 555–565. [Google Scholar] [CrossRef] [PubMed]
- Guilleminault, C.; Huang, Y.S.; Monteyrol, P.J.; Sato, R.; Quo, S.; Lin, C.H. Critical role of myofascial reeducation in pediatric sleep-disordered breathing. Sleep Med. 2013, 14, 518–525. [Google Scholar] [CrossRef]
- Knösel, M.; Klein, S.; Bleckman, A.; Engelke, W. Coordination of tongue activity during swallowing in mouth-breathing children. Dysphagia 2012, 27, 401–407. [Google Scholar] [CrossRef]
- Thijs, Z.; Bruneel, L.; De Pauw, G.; Van Lierde, K.M. Oral myofunctional and articulation disorders in children with malocclusions: A systematic review. Folia Phoniatr. Logop. 2022, 74, 1–16. [Google Scholar] [CrossRef]
- Garliner, D. Myofunctional Therapy in Dental Practice Abnormal Swallowing Habits: Diagnosis-treatment. A Course of Study for the Dental Practitioner and Speech Pathologist; Bartel: Brooklyn, NY, USA, 1974; Volume 2. [Google Scholar]
- Clark, H.M. Specificity of Training in the Lingual Musculature. J. Speech Lang. Hear. Res. 2012, 55, 657–667. [Google Scholar] [CrossRef]
- Rahal, A. Exercícios Miofuncionais Orofaciais. In Motricidade Orofacial: A Atuação nos Diferentes Níveis de Atenção à Saúde; Motta, A.R., Cunha, D.A., Mattos, F., Berretin-Felix, G., Eds.; Pulso: São José dos Campos, Brazil, 2017; pp. 71–76. [Google Scholar]
- Krekeler, B.N.; Yee, J.; Daggett, S.; Leverson, G.; Rogus-Pulia, N. Lingual exercise in older veterans with dysphagia: A pilot investigation of patient adherence. J. Speech Lang. Hear. Res. 2021, 64, 1526–1538. [Google Scholar] [CrossRef] [PubMed]
- Korfage, J.A.; Koolstra, J.H.; Langenbach, G.E.; van Eijden, T.M. Fiber-type Composition of the Human Jaw Muscles—(Part 1) Origin and Functional Significance of Fiber-type Diversity. J. Dent. Res. 2005, 84, 774–783. [Google Scholar] [CrossRef]
- Inostroza, F. Muscle plasticity and hybrid fibers in the masticatory musculature. Literature review. Int. J. Med. Surg. Sci. 2020, 7, 1–11. [Google Scholar] [CrossRef]
- Maas, E.; Robin, D.A.; Hula, S.N.; Freedman, S.E.; Wulf, G.; Ballard, K.J.; Schmidt, R.A. Principles of motor learning in treatment of motor speech disorders. Am. J. Speech Lang. Pathol. 2008, 17, 398–415. [Google Scholar] [CrossRef]
- Madill, C.; McIlwaine, A.; Russell, R.; Hodges, N.J.; McCabe, P. Classifying and identifying motor learning behaviors in voice-therapy clinician-client interactions: A proposed motor learning classification framework. J. Voice 2020, 34, 806.e19–806.e31. [Google Scholar] [CrossRef]
- Guimarães, K.C.; Drager, L.F.; Genta, P.R.; Marcondes, B.F.; Lorenzi-Filho, G. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am. J. Respir. Crit. Care Med. 2009, 179, 962–966. [Google Scholar] [CrossRef]
- de Felício, C.M.; Melchior, M.D.; da Silva, M.A. Effects of orofacial myofunctional therapy on temporomandibular disorders. CRANIO® 2010, 28, 249–259. [Google Scholar] [CrossRef]
- Migliorucci, R.R.; Abramides, D.V.; Rosa, R.R.; Bresaola, M.D.; Nary, H.; Berretin-Felix, G. Effect of myofunctional therapy on orofacial functions and quality of life in individuals undergoing orthognathic surgery. Int. J. Orofac. Myol. 2017, 43, 60–76. [Google Scholar] [CrossRef]
- Dhawale, A.K.; Smith, M.A.; Ölveczky, B.P. The role of variability in motor learning. Annu. Rev. Neurosci. 2017, 40, 479–498. [Google Scholar] [CrossRef] [PubMed]
- Rondon-Melo, S.; Andrade, C.R. Computer-assisted instruction in Speech-Language and Hearing Sciences: Impact on motivation for learning about the Orofacial Myofunctional System. CoDAS 2016, 28, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Sociedade Brasileira de Fonoaudiologia. Departamento de Motricidade Orofacial—Definición y Atribuciones Profesionales. Available online: https://www.sbfa.org.br/portal2017/departamentos/6_motricidade-orofacial (accessed on 25 June 2024).
- American Speech-Language-Hearing Association (ASHA). Roles and Responsibilities of Speech-Language Pathologists with Respect to Orofacial Myofunctional Disorders. Available online: https://www.asha.org/policy/pp2004-00191/ (accessed on 25 June 2024).
- American Speech-Language-Hearing Association (ASHA). Orofacial Myofunctional Disorders: Practice Portal. Available online: https://www.asha.org/practice-portal/clinical-topics/orofacial-myofunctional-disorders/#collapse_0 (accessed on 25 June 2024).
- Felício, C.M.; Ferreira, C.L. Protocol of orofacial myofunctional evaluation with scores. Int. J. Pediatr. Otorhinolaryngol. 2008, 72, 367–375. [Google Scholar] [CrossRef] [PubMed]
| # | Search Strategy |
|---|---|
| 1 | Myofunctional therapy.mp. or muscle training/ |
| 2 | Atypical swallowing.mp. |
| 3 | Tongue interposition.mp. |
| 4 | Tongue thrust.mp. or tongue thrusting/ |
| 5 | 2 or 3 or 4 |
| 6 | 1 and 5 |
| 7 | remove duplicates from 6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the International Association of Orofacial Myology (IAOM). Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salinas, P.C.; Inostroza-Allende, F.; Caviedes-Ulloa, C.; Soto-Fernández, P.; Berretin-Felix, G. Myofunctional Therapy in Atypical Swallowing: A Scoping Review. Int. J. Orofac. Myol. Myofunct. Ther. 2025, 51, 10. https://doi.org/10.3390/ijom51020010
Salinas PC, Inostroza-Allende F, Caviedes-Ulloa C, Soto-Fernández P, Berretin-Felix G. Myofunctional Therapy in Atypical Swallowing: A Scoping Review. International Journal of Orofacial Myology and Myofunctional Therapy. 2025; 51(2):10. https://doi.org/10.3390/ijom51020010
Chicago/Turabian StyleSalinas, Pedro Contreras, Felipe Inostroza-Allende, Cristóbal Caviedes-Ulloa, Patricio Soto-Fernández, and Giédre Berretin-Felix. 2025. "Myofunctional Therapy in Atypical Swallowing: A Scoping Review" International Journal of Orofacial Myology and Myofunctional Therapy 51, no. 2: 10. https://doi.org/10.3390/ijom51020010
APA StyleSalinas, P. C., Inostroza-Allende, F., Caviedes-Ulloa, C., Soto-Fernández, P., & Berretin-Felix, G. (2025). Myofunctional Therapy in Atypical Swallowing: A Scoping Review. International Journal of Orofacial Myology and Myofunctional Therapy, 51(2), 10. https://doi.org/10.3390/ijom51020010







