Clinical Consequences of Ankyloglossia from Childhood to Adulthood: Support for and Development of a Three-Dimensional Animated Video
Abstract
1. Introduction
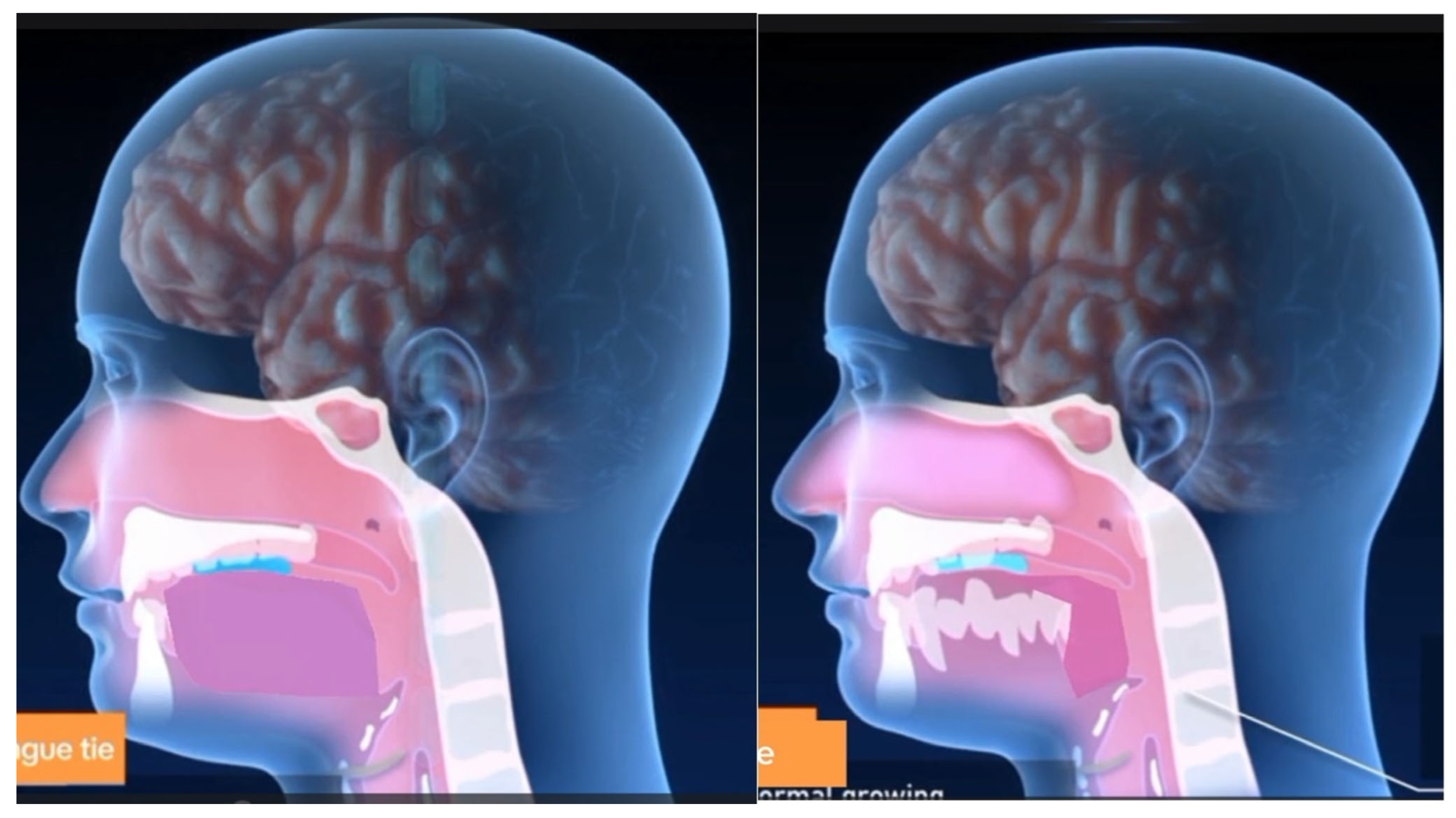
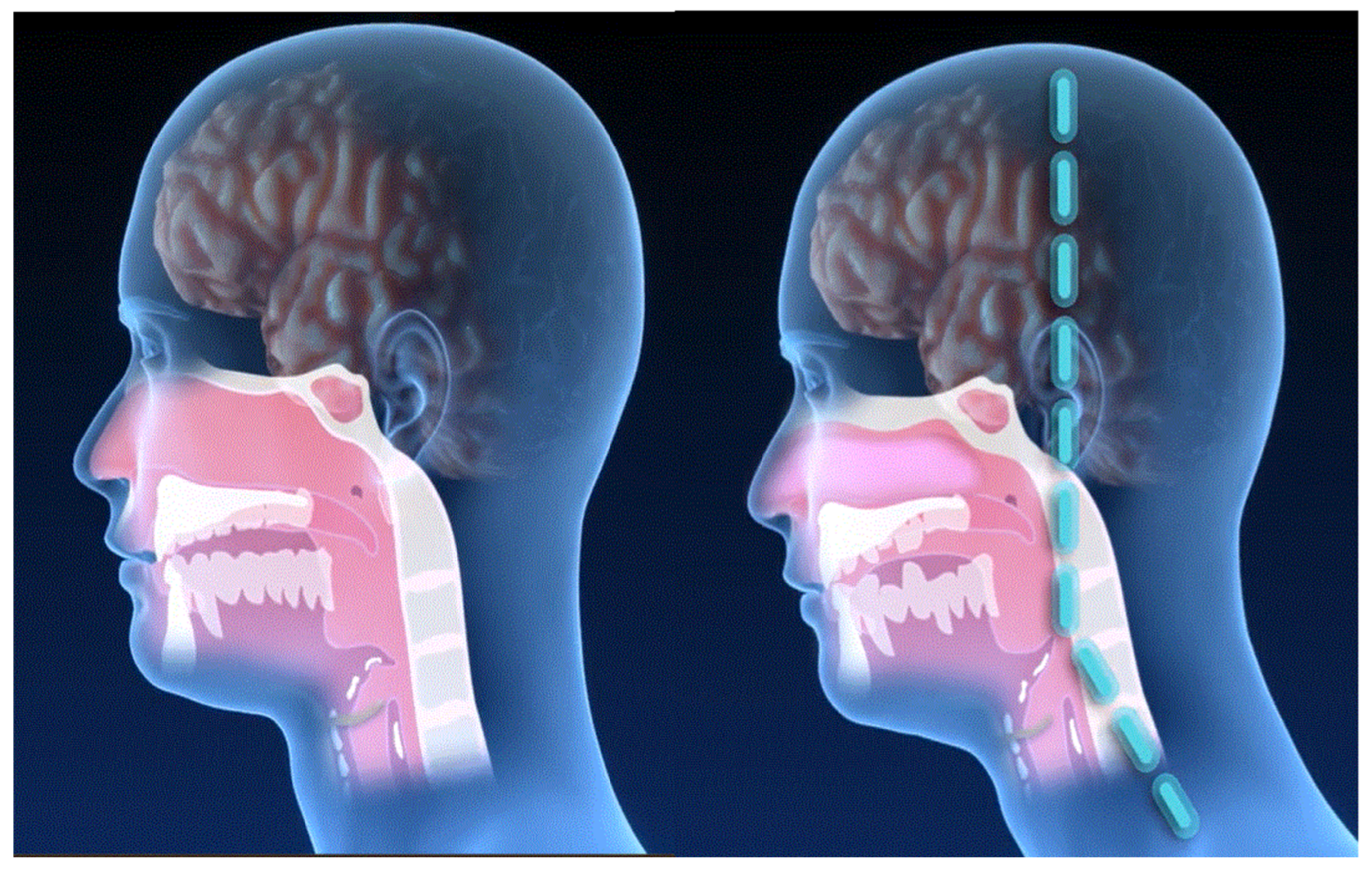
Sleep Apnea
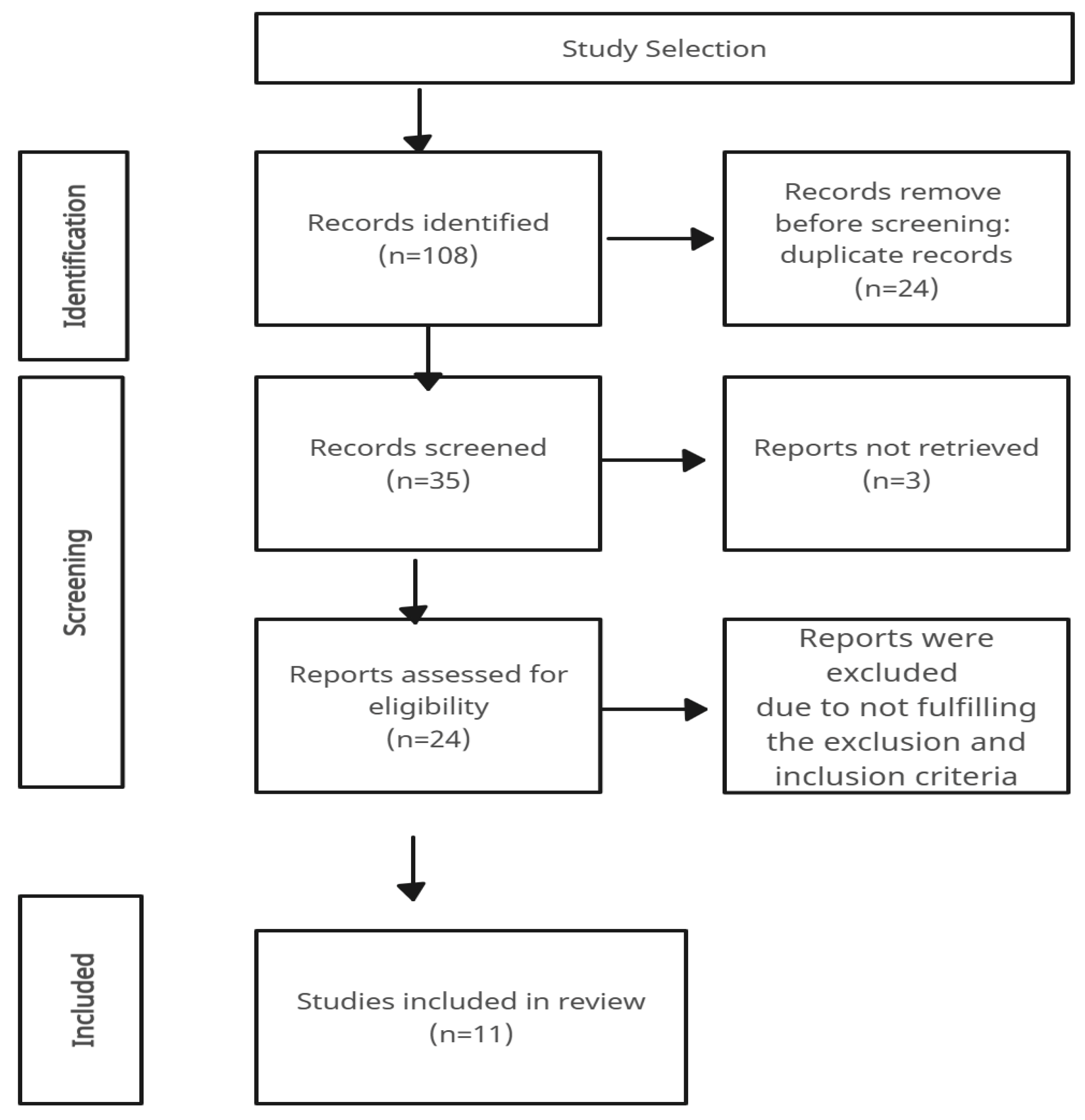
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mills, N.; Geddes, D.T.; Amirapu, S.; Mirjalili, S.A. Understanding the lingual frenulum: Histological structure, tissue composition, and implications for tongue tie surgery. Int. J. Otolaryngol. 2020, 2020, 1820978. [Google Scholar] [CrossRef] [PubMed]
- Wei, E.X.; Meister, K.D.; Balakrishnan, K.; Cheng, A.G.; Qian, Z.J. Ankyloglossia: Clinical and sociodemographic predictors of diagnosis and management in the United States, 2004 to 2019. Otolaryngol.–Head Neck Surg. 2023, 169, 1020–1027. [Google Scholar] [CrossRef] [PubMed]
- Smart, S.J.; Kittrell, A.; Merkel-Walsh, R.; Tseng, R.J. International Consortium of Oral Ankylofrenula Professionals (ICAP): Practice guidelines for ankylofrenula management. Int. J. Orofac. Myol. Myofunct. Ther. 2024, 50, 1–11. [Google Scholar] [CrossRef]
- Buryk, M.; Bloom, D.; Shope, T. Efficacy of neonatal release of ankyloglossia: A randomized trial. Pediatrics 2011, 128, 280–288. [Google Scholar] [CrossRef]
- González Jiménez, D.; Costa Romero, M.; Riaño Galán, I.; González Martínez, M.T.; Rodríguez Pando, M.C.; Lobete Prieto, C. Prevalencia de anquiloglosia en recién nacidos en Asturias (España). An. De Pediatr. 2014, 81, 115–119. (In Spanish) [Google Scholar] [CrossRef]
- O’Connor-Reina, C.; Rodríguez Alcala, L.; Moreno Sales, R. Terapia miofuncional en la apnea obstructiva del sueño. In Diagnóstico y Tratamiento de los Trastornos Respiratorios del Sueño: Actualización en Diagnóstico y Tratamiento Quirúrgico; Ibérica, A., Ed.; Editorial Autor-Editor: Boadilla del Monte, Madrid, Spain, 2022; pp. 509–538. ISBN 9788409443635. [Google Scholar]
- Garliner, D. Myofunctional therapy. ICD Sci. Educ. J. 1975, 8, 39–46. [Google Scholar]
- Jang, S.J.; Cha, B.K.; Ngan, P.; Choi, D.S.; Lee, S.K.; Jang, I. Relationship between the lingual frenulum and craniofacial morphology in 445 adults. Am. J. Orthod. Dentofac. Orthop. 2011, 139, e361–e367. [Google Scholar] [CrossRef]
- Saccomanno, S.; Di Tullio, A.; D’Alatri, L.; Grippaudo, C. Proposal for a myofunctional therapy protocol in case of altered lingual frenulum: A pilot study. Eur. J. Paediatr. Dent. 2019, 20, 67–72. [Google Scholar]
- Bhattad, M.S.; Baliga, M.S.; Kriplani, R. Clinical guidelines and management of ankyloglossia with 1-year follow-up: Report of 3 cases. Case Rep. Dent. 2013, 2013, 185803. [Google Scholar] [CrossRef]
- Pompeia, L.E.; Ilinsky, R.S.; Ortolani, C.L.F.; Faltin, K.J. Ankyloglossia and its influence on growth and development of the stomatognathic system. Rev. Paul. Pediatr. 2017, 35, 216–221. [Google Scholar] [CrossRef]
- Yoon, A.; Zaghi, S.; Weitzman, R.; Ha, S.; Law, C.S.; Guilleminault, C. Toward a functional definition of ankyloglossia: Validating current grading scales for lingual frenulum length and tongue mobility in 1052 subjects. Sleep Breath. 2017, 21, 767–775. [Google Scholar] [CrossRef]
- Srinivasan, B.; Chitharanjan, A.B. Skeletal and dental characteristics in subjects with ankyloglossia. Prog. Orthod. 2013, 14, 44. [Google Scholar] [CrossRef]
- Yoon, A.J.; Zaghi, S.; Ha, S.; Law, C.S.; Guilleminault, C.; Liu, S.Y. Ankyloglossia as a risk factor for maxillary hypoplasia and soft palate elongation: A functional–morphological study. Orthod. Craniofacial Res. 2017, 20, 237–244. [Google Scholar] [CrossRef]
- Vaz, A.C.; Bai, P.M. Lingual frenulum and malocclusion: An overlooked tissue or a minor issue. Indian J. Dent. Res. 2015, 26, 488–492. [Google Scholar] [CrossRef]
- Suzart, D.D.; Carvalho, A.R.R. Alterações de fala relacionadas às alterações do frênulo lingual em escolares. Rev. CEFAC 2016, 18, 1332–1339. [Google Scholar] [CrossRef]
- Guilleminault, C.; Huseni, S.; Lo, L. A frequent phenotype for paediatric sleep apnoea: Short lingual frenulum. ERJ Open Res. 2016, 2, 00043–02016. [Google Scholar] [CrossRef]
- Huang, Y.S.; Quo, S.B.J.; Guilleminault, C. Short lingual frenulum and obstructive sleep apnea in children. Int. J. Pediatr. Res. 2015, 1, 003. [Google Scholar] [CrossRef]
- Brożek-Mądry, E.; Burska, Z.; Steć, Z.; Burghard, M.; Krzeski, A. Short lingual frenulum and head-forward posture in children with the risk of obstructive sleep apnea. Int. J. Pediatr. Otorhinolaryngol. 2021, 144, 110699. [Google Scholar] [CrossRef]
- Correa, E.J.; O’Connor-Reina, C.; Rodríguez-Alcalá, L.; Conti, D.M.; Rabino, A.; Baptista, P.M.; Garcia-Iriarte, M.-T.; Plaza, G. What are we missing in adult obstructive sleep apnea clinical evaluation? Review of official guidelines. Int. J. Orofac. Myol. Myofunct. Ther. 2022, 49, 1–10. [Google Scholar] [CrossRef]
- Messner, A.H.; Walsh, J.; Rosenfeld, R.M.; Schwartz, S.R.; Ishman, S.L.; Baldassari, C.; Brietzke, S.E.; Darrow, D.H.; Goldstein, N.; Levi, J.; et al. Clinical consensus statement: Ankyloglossia in children. Otolaryngol.–Head Neck Surg. 2020, 162, 597–611. [Google Scholar] [CrossRef]
- Kezirian, E.J.; Hohenhorst, W.; de Vries, N. Drug-induced sleep endoscopy: The VOTE classification. Eur. Arch. Oto-Rhino-Laryngol. 2011, 268, 1233–1236. [Google Scholar] [CrossRef] [PubMed]
- Garaycochea, O.; Baptista, P.; Calvo-Imirizaldu, M.; Terrasa, D.; Moffa, A.; Casale, M.; Alcalde, H.; O’Connor-Reina, C.; Plaza, G.; Fernández, S. Surgical anatomy of the lingual nerve for palate surgery: Where is it located and how to avoid it? Eur. Arch. Oto-Rhino-Laryngol. 2022, 279, 5347–5353. [Google Scholar] [CrossRef] [PubMed]
- Rebelo Puccini, F.; Gatti, M.; de Castro Rodrigues, A.; Rondon-Melo, S.; Lung Wen, C.; Lopes de Castro Martinelli, R.; Berretin-Felix, G. Virtual Baby: 3D model of the anatomy and physiology of sucking and swallowing in infants as an educational tool. Int. J. Orofac. Myol. Myofunct. Ther. 2022, 48, 1–11. [Google Scholar] [CrossRef]
- O’Shea, J.E.; Foster, J.P.; O’Donnell, C.P.; Breathnach, D.; Jacobs, S.E.; Todd, D.A.; Davis, P.G. Frenotomy for tongue-tie in newborn infants. Cochrane Database Syst. Rev. 2017, 2021, CD011065. [Google Scholar] [CrossRef]
- Valderrama-Penagos, J.X.; Rodríguez Alcalá, L.; Plaza, G.; Baptista, P.; Garcia Iriarte, M.T.; Correa, E.J.; O’Connor-Reina, C. Ankyloglossia in children, a cause of obstructive sleep apnoea: Case report of paediatric ankyloglossia and sleep apnoea: DISE resolves the mystery. Children 2024, 11, 218. [Google Scholar] [CrossRef]
- Correa, E.J.; O’Connor-Reina, C.; Rodríguez-Alcalá, L.; Benjumea, F.; Casado-Morente, J.C.; Baptista, P.M.; Casale, M.; Moffa, A.; Plaza, G. Does frenotomy modify upper airway collapse in OSA adult patients? Case report and systematic review. J. Clin. Med. 2022, 12, 201. [Google Scholar] [CrossRef]
- Villa, M.P.; Evangelisti, M.; Barreto, M.; Cecili, M.; Kaditis, A. Short lingual frenulum as a risk factor for sleep-disordered breathing in school-age children. Sleep Med. 2020, 66, 119–122. [Google Scholar] [CrossRef]
- LeFort, Y.; Evans, A.; Livingstone, V. Academy of Breastfeeding Medicine position statement on ankyloglossia in breastfeeding dyads. Breastfeed. Med. 2021, 16, 278–281. [Google Scholar] [CrossRef]
- American Academy of Pediatric Dentistry. Policy on management of the frenulum in pediatric patients. In The Reference Manual of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2022; pp. 80–85. Available online: https://www.aapd.org/ (accessed on 1 January 2025).
- Australian Dental Association. Policy Statement 2.13: Ankyloglossia and Oral Frena. 2022. Available online: https://ada.org.au/policy-statement-2-13-ankyloglossia-and-oral-frena (accessed on 23 January 2025).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Hasan, N. Tongue tie as a cause of deformity of lower central incisor. J. Pediatr. Surg. 1973, 8, 985. [Google Scholar] [CrossRef]
- Defabianis, P. Ankyloglossia and its influence on maxillary and mandibular development: A seven-year follow-up case report. Funct. Orthod. 2000, 17, 25–33. [Google Scholar]
- Correa, E.J.; Conti, D.M.; Gozal, D.; O’Connor-Reina, C. Preventive medicine in obstructive sleep apnea: A systematic review and a call to action. Sleep 2024, 47, zsae164. [Google Scholar] [CrossRef]
- ISRCTN. Evaluation of the Effectiveness of a New Therapy for Chronic Back Pain. ISRCTN17260595. Available online: https://doi.org/10.1186/ISRCTN17260595 (accessed on 21 March 2025).
| Clinical Consequences | Reference | Type | Follow-Up Time | Number of Patients | Assessment Tools |
|---|---|---|---|---|---|
| Breastfeeding and swallowing | Saccomanno et al. [9] | Pilot study | 3 weeks | 6 children | Hazelbaker Assessment Tool for Lingual Frenulum Function (HATLFF) |
| Pompeia et al. [11] | Systematic review | N/A | N/A | Marchesan Lingual Frenulum Protocol | |
| Yoon et al. [12] | Prospective cohort case series | 3 months | 1052 | Kotlow Classification Tongue Range of Motion Ratio (TRMR) * | |
| Craniofacial growth | Pompeia et al. [11] | Systematic review | N/A | N/A | Marchesan Lingual Frenulum Protocol |
| Yoon et al. [14] | Prospective cohort case series | Occasional | 302 | TRMR | |
| Srinivasan et al. [13] | Prospective cohort case series and control | Occasional | 57 vs. 60 | Nonspecific standardized tool | |
| Dental occlusion | Bhattad et al. [10] | Prospective case series | 1 year | 3 | Kotlow Classification |
| Yoon et al. [12] | Prospective case series | 3 months | 1052 | Kotlow Classification TRMR | |
| Vaz et al. [15] | Prospective case series | Occasional | 700 | Nonspecific standardized tool | |
| Articulation | Bhattad et al. [10] | Prospective case series | 1 year | 3 | Kotlow Classification |
| Suzart et al. [16] | Case series and control | Occasional | 52 | Marchesan Lingual Frenulum Protocol | |
| Mouth breathing | Bhattad et al. [10] | Prospective case series | 1 year | 3 | Kotlow Classification |
| Pompeia et al. [11] | Systematic review | N/A | N/A | Marchesan Lingual Frenulum Protocol | |
| Yoon et al. [12] | Prospective case series | 3 months | 1052 | TRMR | |
| Social relationships | Bhattad et al. [10] | Case series | 1 year | 3 | Kotlow Classification |
| Sleep apnea | Guilleminault et al. [17] | Retrospective case series | Occasional | 150 | Nonspecific standardized tool |
| Huang et al. [18] | Retrospective case series | Occasional | 27 | Nonspecific standardized tool | |
| Head posture | Brożek-Mądry et al. [19] | Case series and control | Occasional | 128 | Nonspecific standardized tool |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the International Association of Orofacial Myology (IAOM). Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Connor-Reina, C.; Rodriguez Alcala, L.; Bosco, G.; Martínez-Ruiz de Apodaca, P.; Mackers, P.; Garcia-Iriarte, M.T.; Baptista, P.; Plaza, G. Clinical Consequences of Ankyloglossia from Childhood to Adulthood: Support for and Development of a Three-Dimensional Animated Video. Int. J. Orofac. Myol. Myofunct. Ther. 2025, 51, 5. https://doi.org/10.3390/ijom51010005
O’Connor-Reina C, Rodriguez Alcala L, Bosco G, Martínez-Ruiz de Apodaca P, Mackers P, Garcia-Iriarte MT, Baptista P, Plaza G. Clinical Consequences of Ankyloglossia from Childhood to Adulthood: Support for and Development of a Three-Dimensional Animated Video. International Journal of Orofacial Myology and Myofunctional Therapy. 2025; 51(1):5. https://doi.org/10.3390/ijom51010005
Chicago/Turabian StyleO’Connor-Reina, Carlos, Laura Rodriguez Alcala, Gabriela Bosco, Paula Martínez-Ruiz de Apodaca, Paula Mackers, Maria Teresa Garcia-Iriarte, Peter Baptista, and Guillermo Plaza. 2025. "Clinical Consequences of Ankyloglossia from Childhood to Adulthood: Support for and Development of a Three-Dimensional Animated Video" International Journal of Orofacial Myology and Myofunctional Therapy 51, no. 1: 5. https://doi.org/10.3390/ijom51010005
APA StyleO’Connor-Reina, C., Rodriguez Alcala, L., Bosco, G., Martínez-Ruiz de Apodaca, P., Mackers, P., Garcia-Iriarte, M. T., Baptista, P., & Plaza, G. (2025). Clinical Consequences of Ankyloglossia from Childhood to Adulthood: Support for and Development of a Three-Dimensional Animated Video. International Journal of Orofacial Myology and Myofunctional Therapy, 51(1), 5. https://doi.org/10.3390/ijom51010005








