INTRODUCTION
Frenum attachments of the tongue, lip or cheeks if restrictive may be described as ties or restrictive tethered oral tissues (RTOTs). Ankyloglossia, more commonly known as tongue tie is an oral anomaly in which an abnormally short lingual frenum affects the tongue mobility by tethering it to the floor of the mouth. It is present in approximately 8% of infants [
1].
Numerous studies in the literature have quoted that neonatal ankyloglossia and/or shortened maxillary frenum (upper lip tie) are identified as an established cause of breastfeeding difficulties in the mother- child dyad. [
2,
3,
4] Mothers of infants with ankyloglossia often develop painful, bleeding nipples, flattened, compressed and injured nipples, plugged ducts, mastitis, extended feeding times, frequent breastfeeding with reduced milk transfer, reduced milk supply, and post-partum depression [
5].
Aerophagia, from the Greek word
aerophagein meaning to “eat air,” is a poorly studied phenomenon. Major studies in the literature indicate that “post-feed aerophagia” is observed with higher rates in infants with ankyloglossia or possible lip tie [
6].
During feeding, when the infant attempts to latch and has an ineffective seal with limited tongue mobility, this eventually leads to an increase in swallowing of air followed by a cascade of post- feeding gastrointestinal (GI) distress, irritability, pain, sudden or constant crying, loud clicking noises due to tongue recoil, poor infant weight gain, gagging, coughing, curd chewing, hiccupping, colic, and possible reflux [
7].
Prescription of anti-reflux drugs or acid-blocking drugs like an H-2 blocker or proton pump inhibitor have been in routine practice as the medical/scientific community is still evolving to accept the concept of aerophagia/air- induced reflux [
18]. Crying and irritability is distressing to families, and often results in the use of medications [
7], particularly proton pump inhibitors (PPIs). In a systemic review, Gieruszczak-Bialek et al. [
8] found that there was no effect of PPIs on crying and irritability in infants.
Studies do suggest significant improvement in the infants’ gastrointestinal symptoms after frenotomy irrespective of the method used almost immediately with continued improvements noted up to six months post- procedure. However, to date, an exclusive systematic review highlighting this topic has not been conducted.
Therefore, in this systematic review, we aim to systematically explore improvements in gastrointestinal symptoms 1 week and 1 month after frenotomy procedure as compared to before the procedure for infants younger than 12 months of age using meta-analysis calculations. The review includes severity of tongue tie and lip tie classified by various authors, combinations of surgeries and the tools used.
Objective
To investigate the evidence of gastrointestinal symptom improvement in infants after RTOTs release.
METHOD
Protocol Registration and Review Reporting
This systematic review protocol was registered under the PROSPERO with the registration number CRD42023423702.
The present systematic review was reported in accordance to Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) 2020 checklist from, Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews.
Eligibility Criteria
Inclusion Criteria. Studies were selected according to these defined criteria:
Population (P)
Infants currently breastfeeding
Infants under 12 months of age
Infants with functional restriction of movement of tongue and/or upper lip or cheeks
Infants with gastrointestinal symptoms, reflux
Infants who underwent surgical correction for restrictive (tethered) maxillary labial frenum (upper lip tie) and/or ankyloglossia/tongue tie or maxillary buccal frena.
Comparator (C)
There is no control group. Rather, improvement in gastrointestinal symptoms before and after the release were evaluated.
Main Outcome (O)
Improvement in the gastrointestinal symptom after the RTOTs release.
Additional Outcomes
Gastrointestinal improvement 1 week after release. Gastrointestinal improvement 1 month after release,
Study Design (S)
Randomized controlled trials, non-randomized controlled trials, Observational studies and Interventional studies, grey literature with this study design.
Articles on improvement in gastrointestinal symptoms after tongue tie or lip tie release in infants.
Articles published from April 2016 to March 2023
Articles published only in English.
Exclusion Criteria. The following exclusion criteria were applied:
Case reports, Case series, Book chapters, Letters to editors, Previous systematic reviews, In vitro studies, Animal studies.
Articles reporting medically compromised patients or patients with disorders of the tongue with etiologies other than ankyloglossia.
Only Abstracts.
Search Strategy
The search terms included the key concepts, Mesh terms, controlled vocabulary terms as well as free text terms. The search strategy followed the syntax rules adapted for each database based on the PICO question. Additional keywords related to the aim of this review were used through Boolean operators (OR, AND) to combine search words. A complementary search was also conducted by screening the references of the selected articles, previously published reviews of this topic and journals to find any that did not appear in the database search, one article was found in reference lists that was included in the review.
The following search strategies with corresponding keywords were used:
PubMed
“Ankyloglossia” OR “lip tie” OR “infant” OR “breastfeeding” OR “Tongue tie” OR “Lip tie” OR “Lingual frenum” OR “Lingual frenulum” OR “Shortened lingual frenum” OR “Tethered Oral Tissues” (All Fields) AND “Frenotomy” OR “Frenectomy” OR “Tongue tie release” OR “Lip tie release” (All Fields) AND “gastroesophageal reflux” OR “gastrointestinal distress” OR “aerophagia” OR “colic” OR “air ingestion” OR “reflux” (All Fields)
Web of Science
“Ankyloglossia” OR “lip tie” OR “infant” OR “breastfeeding” OR “Tongue tie” OR “Lip tie” OR “Lingual frenum” OR “Lingual frenulum” OR “Shortened lingual frenum” OR “Tethered Oral Tissues” (All Fields) AND “Frenotomy” OR “Frenectomy” OR “Tongue tie release” OR “Lip tie release” (All Fields) AND “gastroesophageal reflux” OR “gastrointestinal distress” OR “aerophagia” OR “colic” OR “air ingestion” OR “reflux” (All Fields)
Scopus
(TITLE-ABS-KEY (“Ankyloglossia”) AND TITLE-ABS-KEY (“reflux”) AND TITLE-ABS-KEY (infant)
Embase
TITLE-ABS-KEY (“Ankyloglossia”) AND TITLE- ABS-KEY (“reflux”) AND TITLE-ABS-KEY (infant)
Cochrane Library
TITLE-ABS-KEY (“Ankyloglossia”) AND TITLE- ABS-KEY (“reflux”) AND TITLE-ABS-KEY (infant)
EBSCOhost
Ankyloglossia” OR “lip tie” OR “infant” OR “breastfeeding” OR “Tongue tie” OR “Lip tie” OR “Lingual frenum” OR “Lingual frenulum” OR “Shortened lingual frenum” OR “Tethered Oral Tissues” (All Fields) AND “Frenotomy” OR “Frenectomy” OR “Tongue tie release” OR “Lip tie release” (All Fields) AND “gastroesophageal reflux” OR “gastrointestinal distress” OR “aerophagia” OR “colic” OR “air ingestion” OR “reflux” (All Fields)
Study Selection Process and Data Extraction
The identified articles were exported to Endnote Web and, where the first phase was carried out, titles and abstracts were screened independently by both authors (IM and HK) using the inclusion and exclusion criteria. Both authors then reviewed the full-text articles for inclusion/exclusion independently. If necessary, any unresolved differences were resolved by a consensus agreement by all the authors.
This review was conducted in July 2023. The included studies were then exported to RevMan Software 5.4 for further analysis. Relevant study characteristics extracted from each study included authors, type of study, number of samples, interventions, outcome measures, measurement instrument and results obtained.
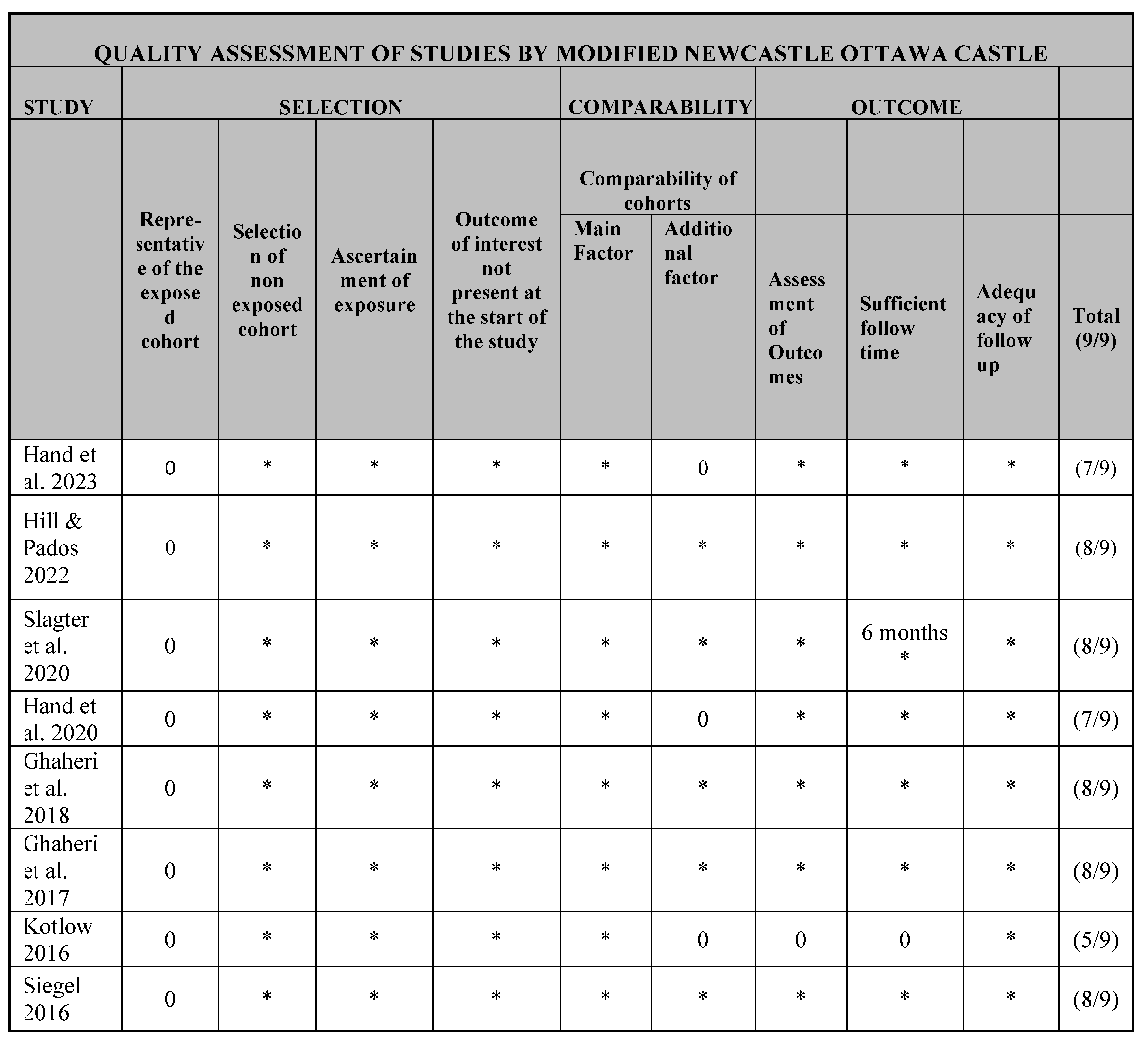
Risk of Bias and Quality Assessment
The risk of bias was evaluated using the Modified Newcastle-Ottawa Scale for Risk of Bias criteria. Studies were categorized as having low, moderate, and high methodological quality, according to Modified NOS scores under five, from five to seven, and above seven, respectively. This quality assessment was used only for the descriptive part and not for statistical evaluation. The evaluation of study quality was independently carried out by the identical investigators. Disagreements among the investigators were resolved through consensus, seeking the input of a third investigator in cases of uncertainty.
Assessment criteria, including study design, risk of bias, result consistency, indirect evidence, imprecision, and publication bias, were utilized to evaluate the overall strength of evidence through the grading of recommendations, assessment, development, and evaluations tool (GRADE Handbook).
RESULTS
Study Selection
A total of 90 articles were identified, relevant to the PICO Question: 10 in PubMed, 11 in Web of Science, 23 in Scopus, 27 in Embase, 6 in Cochrane Library, and 11 in EBSCOhost.
After evaluating duplicates, 38 articles were excluded. Thus, the reviewers read 52 titles and abstracts in the first phase. Of these, 22 were sought for retrieval, 30 were excluded by the authors for not meeting the inclusion criteria or for having a study design that met the exclusion criteria. Two articles could not be retrieved, 20 articles were then read with full texts. Of the 20, 11 articles were excluded since they were systematic reviews [
1], not research [
7] and case report [
1] and had different outcome variables of interest [
2].
Thus, nine articles were included in the systematic review. The selection process in the different phases is detailed in the PRISMA flow chart (
Figure 1).
Study Characteristics
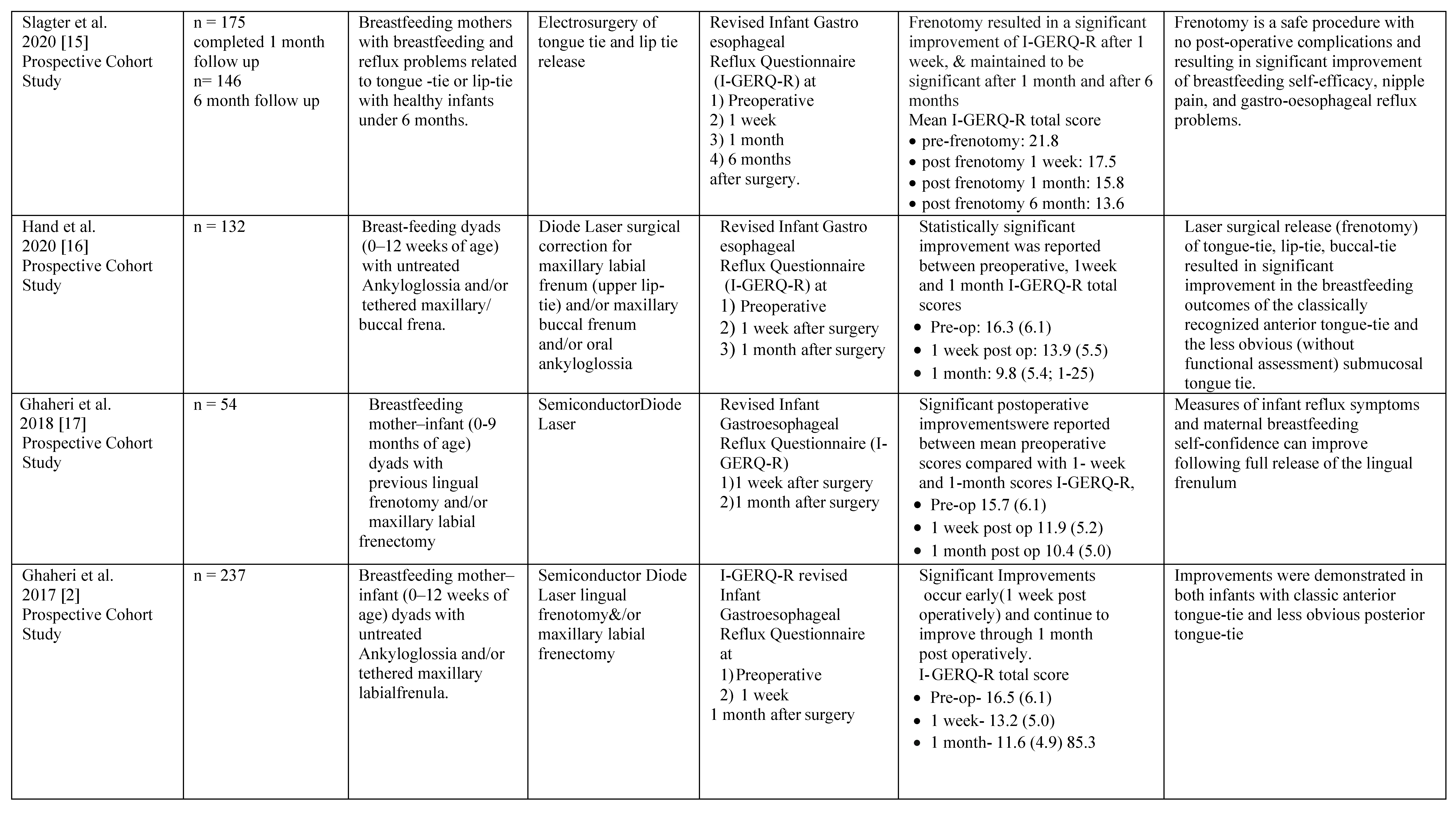
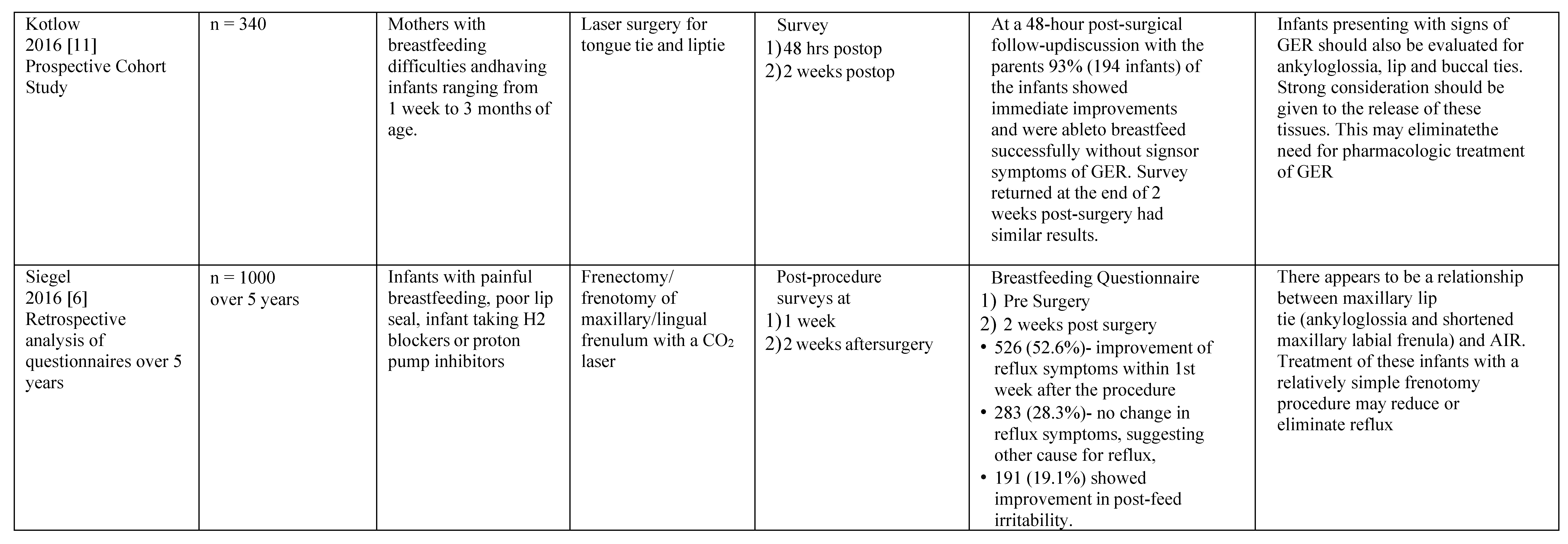
The characteristics of the nine eligible studies [
2,
6,
10,
11,
13,
14,
15,
16,
17] are presented in
Table 1. Out of these studies, seven were prospective cohort studies, one was a prospective randomized trial, and one was a retrospective analysis. The number of patients included in the studies varied from 40 to 1000 infants under 12 months of age. Siegel et al. [
6] and Kotlow [
11] presented the largest sample populations among the included studies, 1000 and 340, respectively. Slagter et al. [
15], had the highest follow- up time of 6 months.
Risk of Bias and Quality Assessment
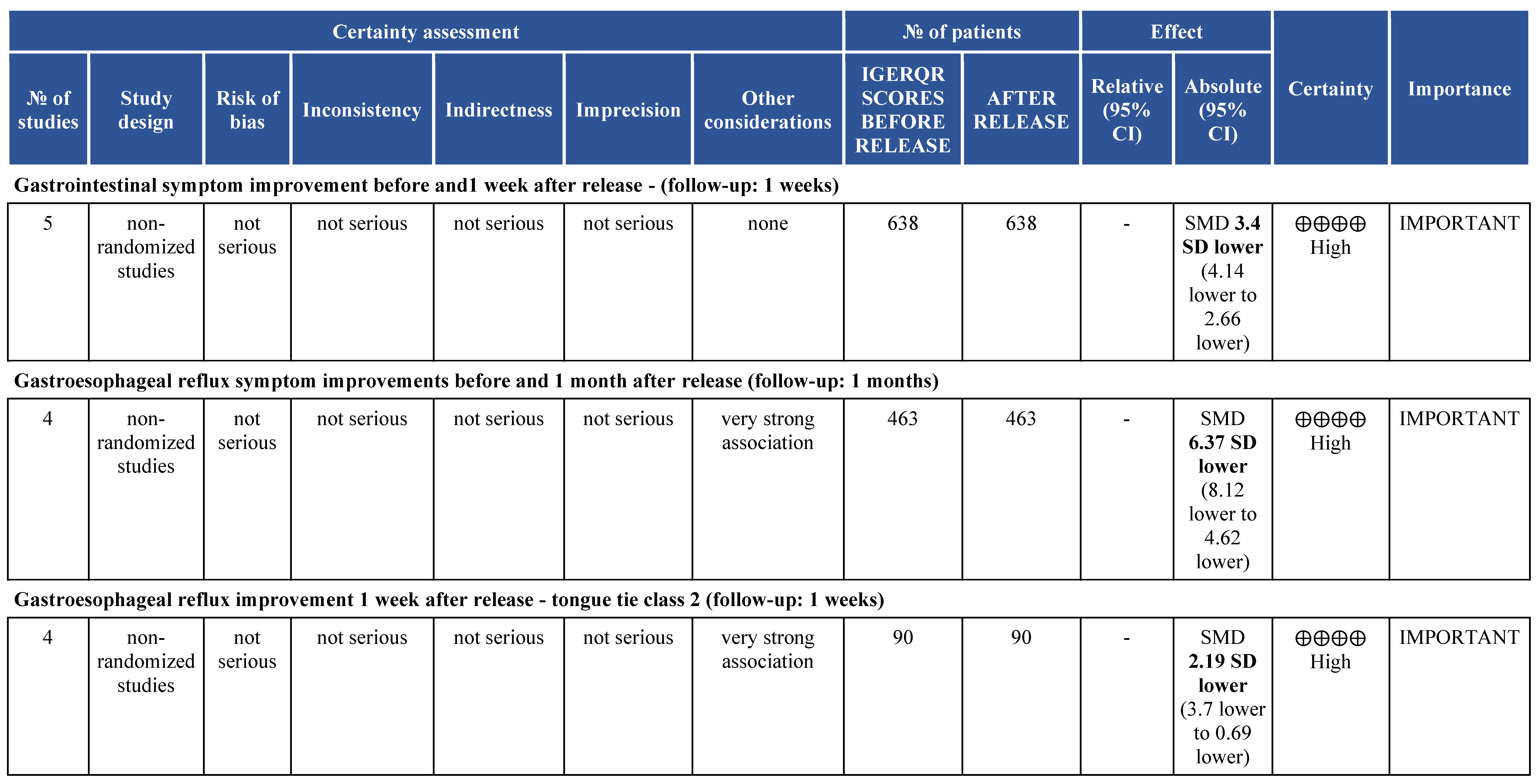
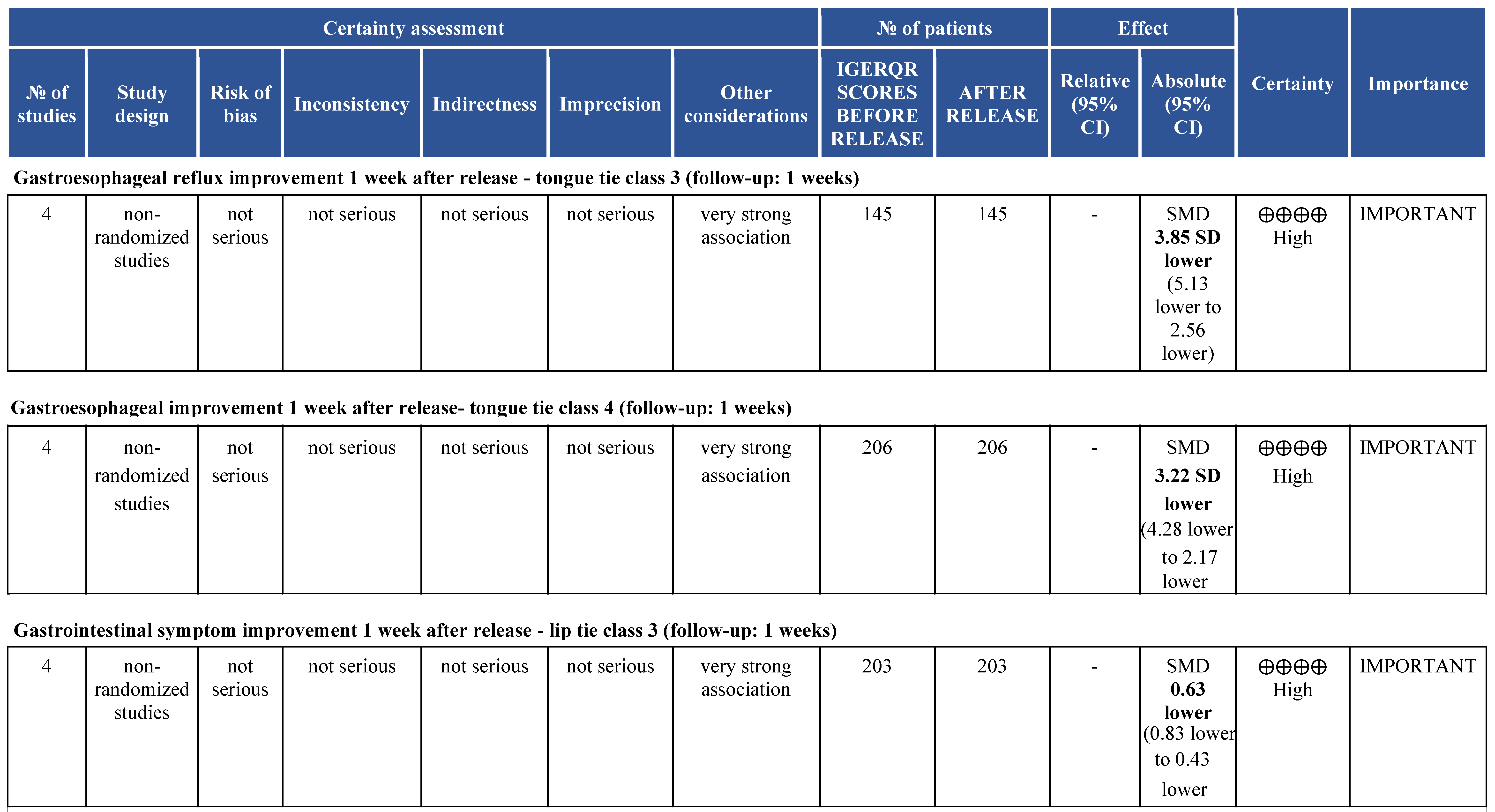
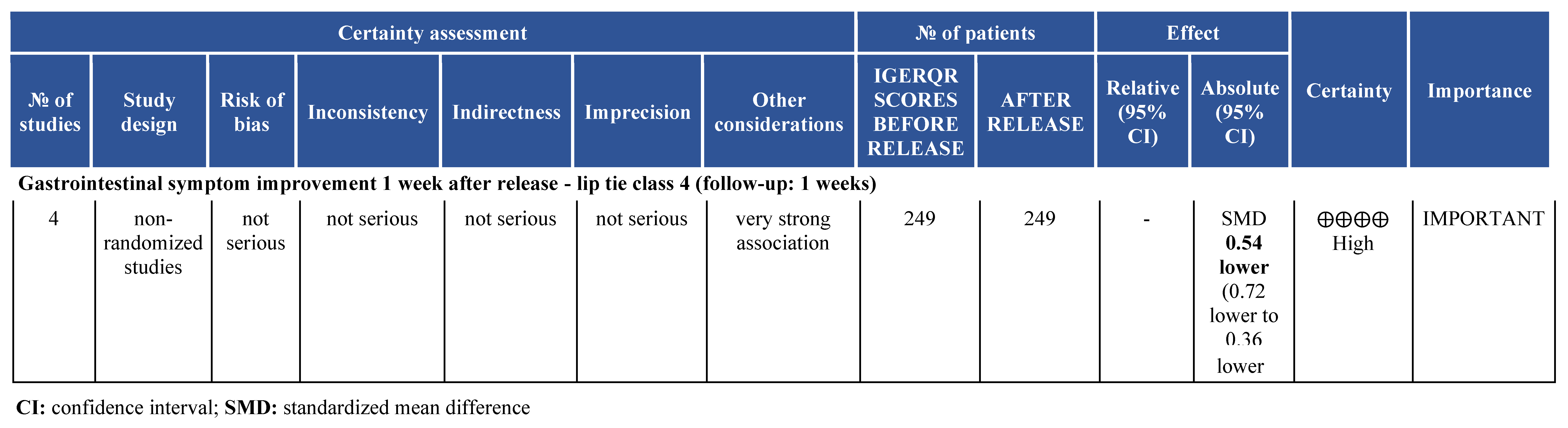
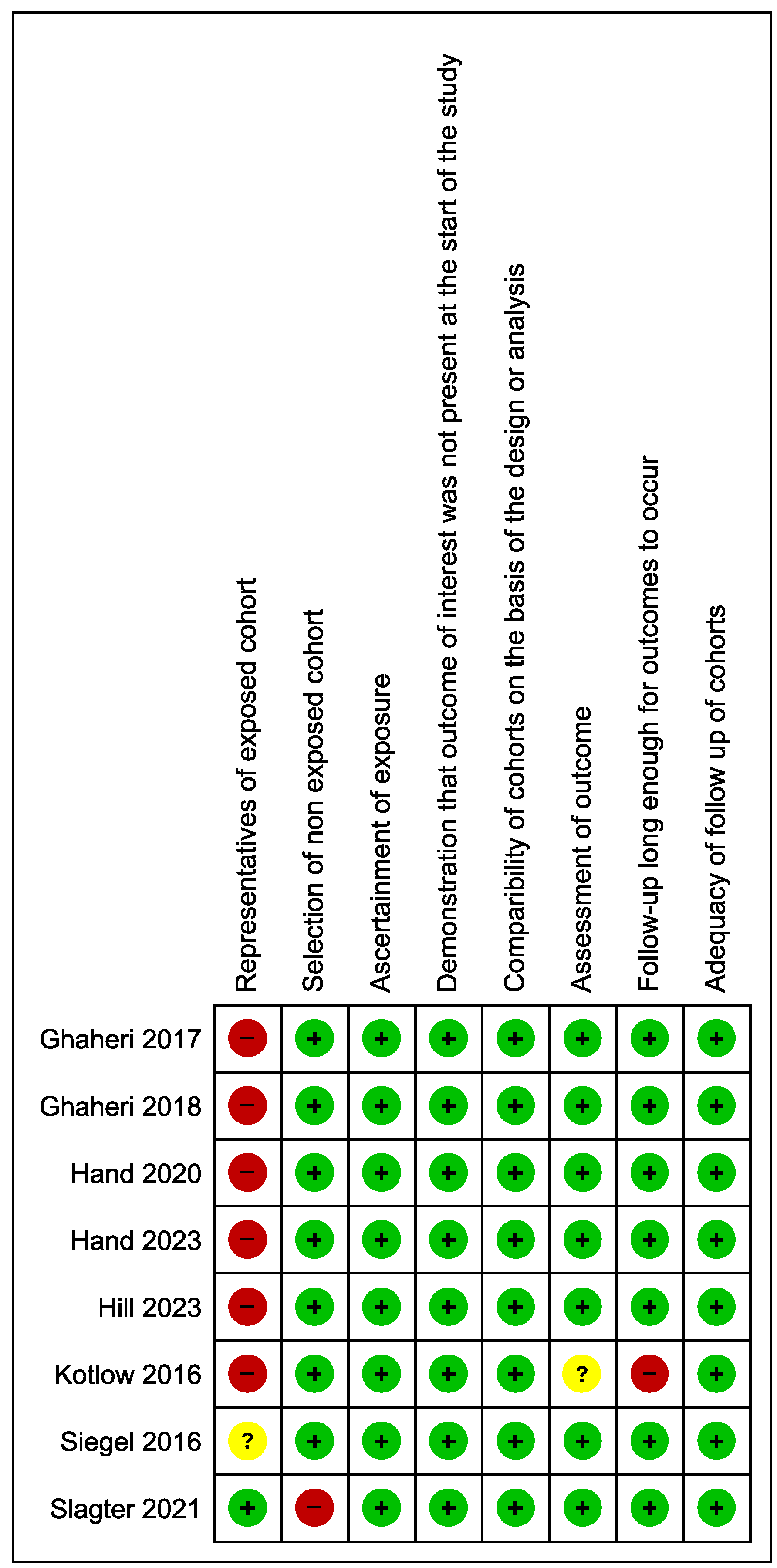
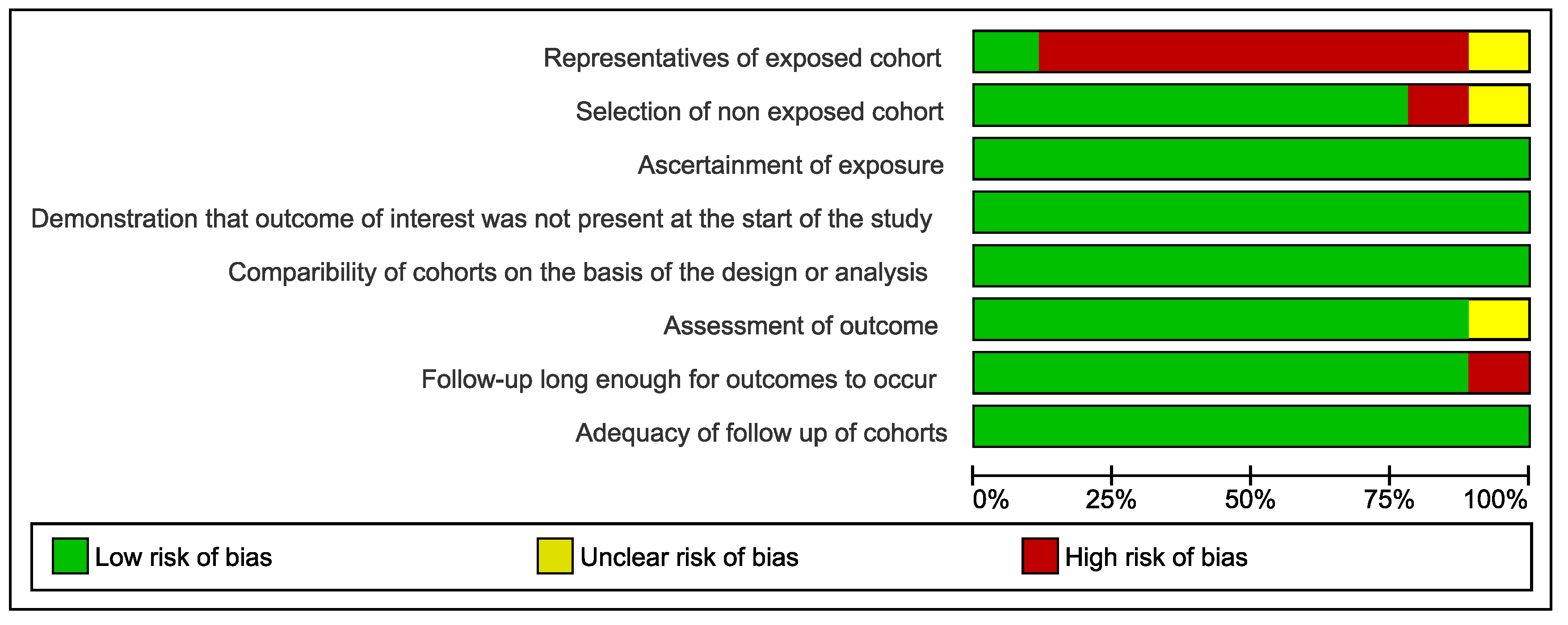
To exclude the risk of bias, the eight eligible studies were independently analyzed using a modified Newcastle – Ottawa appraisal checklist, a tool designed to appraise the included studies on three main areas: the selection of the study groups, the comparability of these groups, and the ascertainment outcome measures. Results are displayed in
Appendix A.
Figure 2a,b show that seven [
2,
6,
10,
13,
15,
16,
17] studies scored 7 or higher in the risk of bias assessment, indicating low risk of bias, and only one [
11] study presented moderate risk of bias with a score of 5.
GRADE profiler (GRADEpro) was used to rate the quality of evidence and to create a 'Summary of Findings' table of seven pre-specified outcomes. [
27]
In
Appendix B, we provide more detailed evaluation and reporting, including a full risk-of-bias assessment of individual studies as well as grading quality of evidence for each outcome measure, considering limitations in study design or execution, inconsistencies in the results, indirectness of the evidence, imprecision and publication bias. The quality of the body of evidence was rated high for all critical and important outcomes.
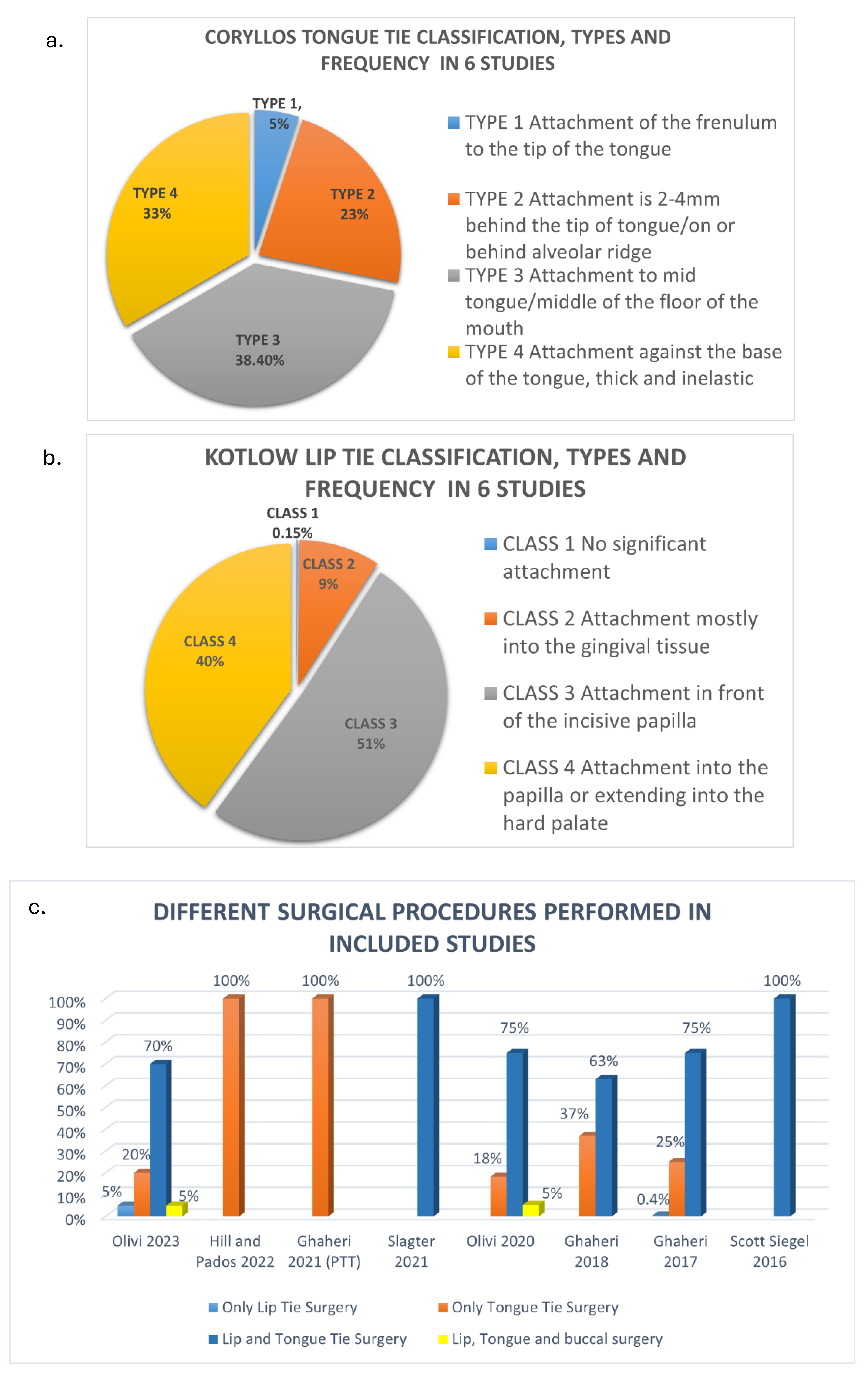
Lip Tie and Tongue Tie Classifications
Across the nine studies, different tools and classifications were used to assess the frenum attachment. Six studies used Kotlow’s upper lip-tie classification [
19] and Coryllos tongue-tie classification. [
20]
Siegel [
6] used the Kotlow’s classification for upper lip tie [
19] and Hazelbaker assessment tool for tongue tie classification. [
22] However, Hill [
13] did not take lip tie into consideration and only used Kotlow’s Tongue tie classification. [
21] Similarly, Ghaheri [
14] had excluded lip tie in his study and used Coryllos classification of tongue tie. [
20]
The diagnostic tools used assess different characteristics of tongue tie. The Coryllos Grading System [
20] classifies tongue tie based on severity of restriction to the floor of the mouth. Kotlow's diagnostic criteria [
19] involves measurement of free tongue (portion not attached to the frenulum) in millimeters.
Since the Kotlow Lip tie Classification and Coryllos tongue tie classification were used more commonly, due to the ease of reproducibility and apprehensibility, the data from these six studies are collectively depicted in pie diagrams.
Data presented in
Figure 3a,b confirm the total sample population of 638 in six studies. Kotlow Class 3 (325/638) and class 4 (255/638) lip tie were the highest. Coryllos Type 3 (244/638) and Type 4 (210/638) tongue tie were the highest.
Different combinations of surgeries were carried out in the included studies, as shown in
Figure 3c. The distribution of surgeries performed were:
Lip tie surgery alone: 1%
Tongue tie surgery alone: 33%
Combined lip and tongue tie surgeries: 66%
Lip, tongue, and buccal surgeries: 1%
Surgical Interventions
Out of the nine studies, eight [
2,
6,
10,
11,
13,
14,
16,
17] used laser for the correction of lip tie, tongue tie or buccal tie, whereas one study [
15] mentioned the use of electrosurgery. Of the eight studies that used laser, three [
13,
14,
16] mentioned the use of CO2 laser, whereas four [
2,
10,
16,
17] mentioned the use of diode laser and one study [
11] did not mentioned the type of laser used.
Infant Gastroesophageal Reflux
Infant gastroesophageal reflux was measured in five studies [
2,
10,
15,
16,
17] using the validated Infant Gastroesophageal Reflux Questionnaire Revised (I-GERQ-R) Questionnaire (University of Pittsburgh, Pittsburgh, PA). I-GERQ-R is a 12-item survey with strong internal consistency designed to evaluate the severity of gastroesophageal reflux symptomatology. [
26]
One study [
13] used the 36-item Gastrointestinal and Gastroesophageal Reflux (GIGER) Scale for Infants and Toddlers. The GIGER has evidence of adequate psychometric properties, including acceptable internal consistency reliability (Cronbach α = .78-.94), convergent validity, and known-groups validity. [
23]
One study used the Gastroesophageal Symptom Questionnaire for Infants (GSQ-I; 2004, Pfizer). The GSQ-I quantifies the duration and severity of 6 to 8 symptoms associated with infant reflux. [
14] Two studies [
6,
11] did not mention the post-op surveys or questionnaires used.
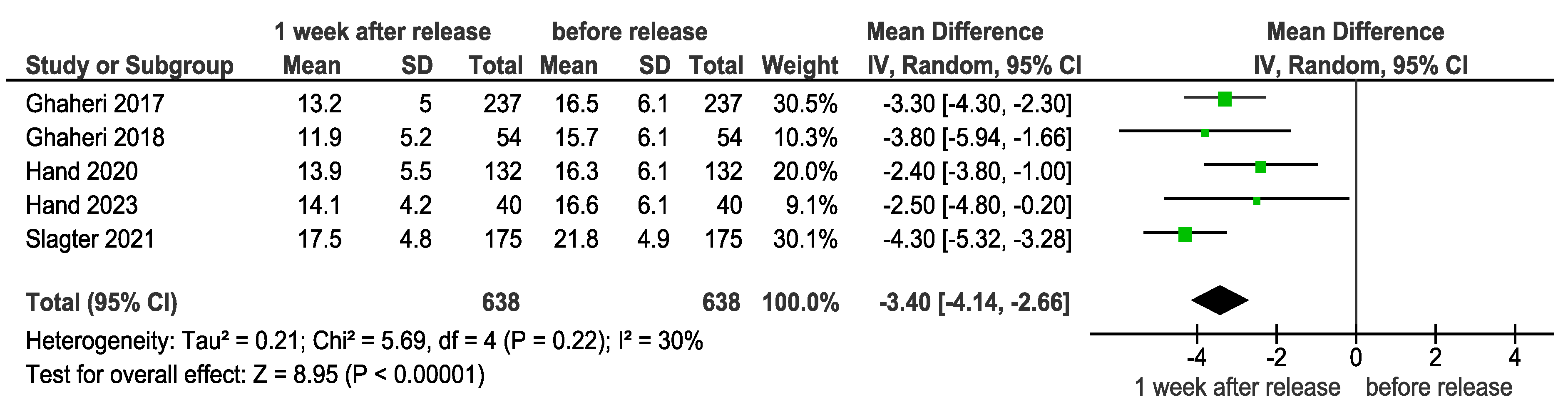
I-GERQ-R Scores Improvement 1 Week After Release
Five studies [
15,
10,
16,
17,
2] compared the I-GERQ-R scores before and 1 week after release (
Figure 4a). Meta-analysis of these five studies [
15,
10,
16,
17,
2] demonstrated a statistically significant improvement in gastrointestinal symptoms, with a large effect size [SMD = 3.40 (4.14, 2.66), p < 0.00001] one week after RTOT release. The low heterogeneity (I² = 30%) indicates consistent results across studies.
Clinical Significance
The large effect size reflects a marked reduction in gastrointestinal symptoms like reflux.
Using a validated, patient-based instrument, all five studies were able to demonstrate a reduction in reflux symptoms scores after frenotomy, suggesting that lingual restriction with or without labial restriction may be associated with infant reflux symptoms, and that correction of latch abnormalities attributed to ankyloglossia significantly improves reflux scores at 1 week post procedure.
Whereas infant reflux is multifactorial in nature, the reflux improvement seen in the cohort soon after the procedure points more to a decrease in aerophagia from a poor latch than it does spontaneous resolution of other factors contributing to reflux.
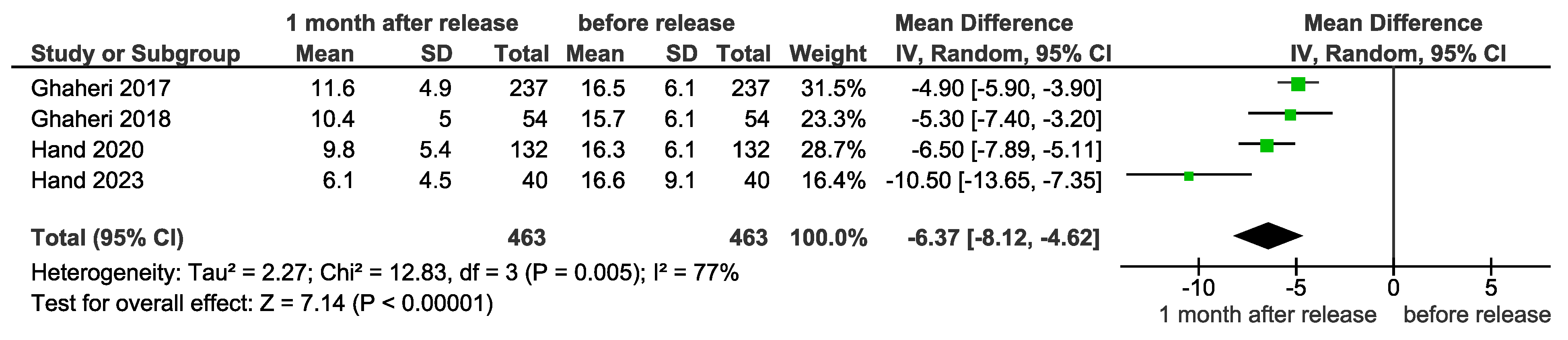
I-GERQ-R scores improvement 1 month after release
Four studies [
10,
16,
17,
2] compared the I-GERQ-R scores before release and 1 month after release (
Figure 4b). The meta-analysis showed a statistically significant improvement in gastrointestinal symptoms, with a standard mean difference (SMD) of 6.37 [8.12, 4.62] (p < 0.00001), indicating a large effect size favoring improvement.
Clinical Significance
Substantial symptom relief
An effect size of 6.37 represents a dramatic improvement in gastrointestinal symptoms, suggesting clinically meaningful benefits for infants experiencing reflux and related issues. This level of improvement is likely to significantly enhance feeding efficiency, comfort, and overall health.
Practical impact
Significant improvement in breastfeeding outcomes that impact dyad quality of life, and therefore are likely to improve breast feeding quality and duration. Maternal self-efficacy, pain, infant reflux symptoms, and the rate of milk transfer all significantly improved with lingual frenotomy with or without maxillary labial frenectomy, indicating a strong consistency of treatment effect.
Heterogeneity
While heterogeneity was substantial (I² = 77%), this may reflect variability in study designs or patient populations rather than undermining the observed clinical relevance.
In summary, both the statistical significance and large effect size strongly suggest that RTOT release offers significant clinical benefits for gastrointestinal health in affected infants.
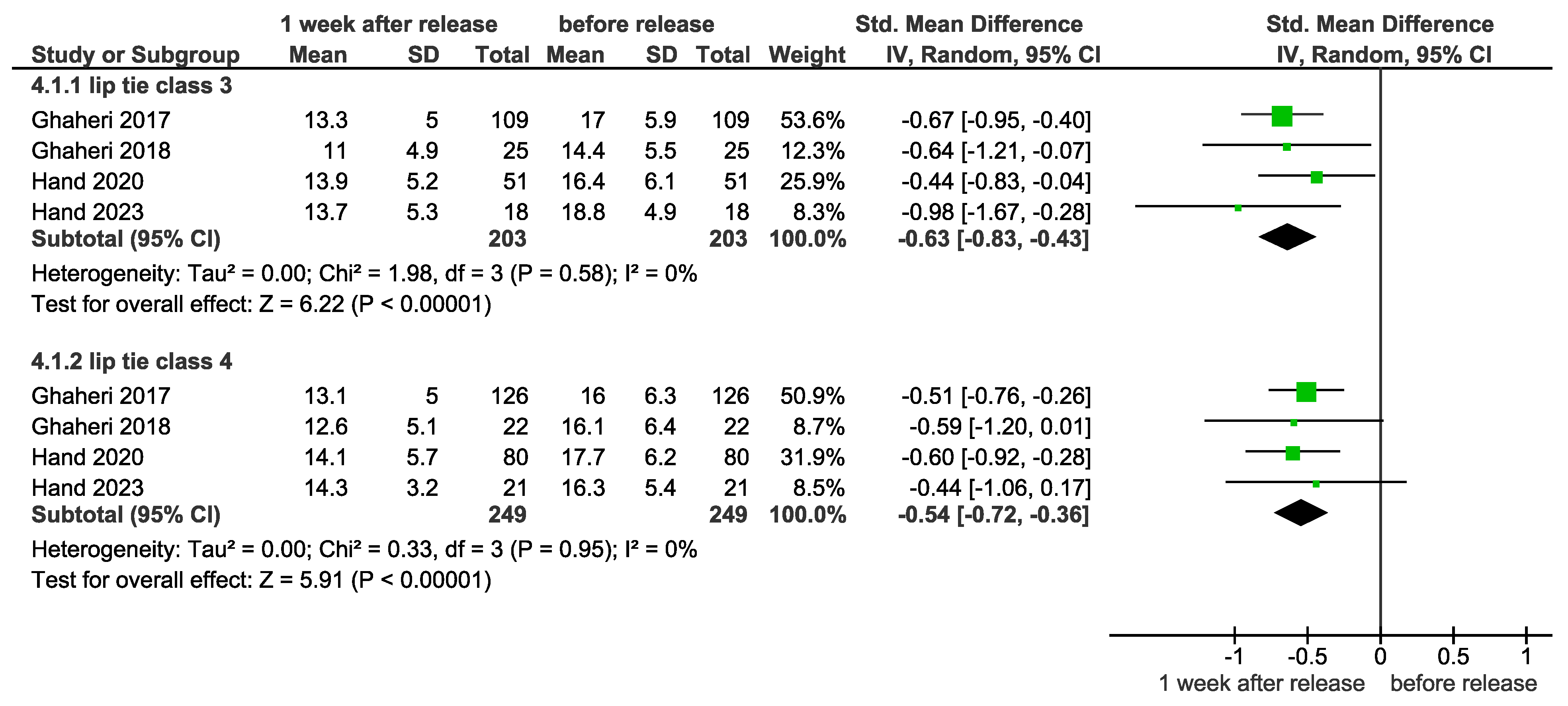
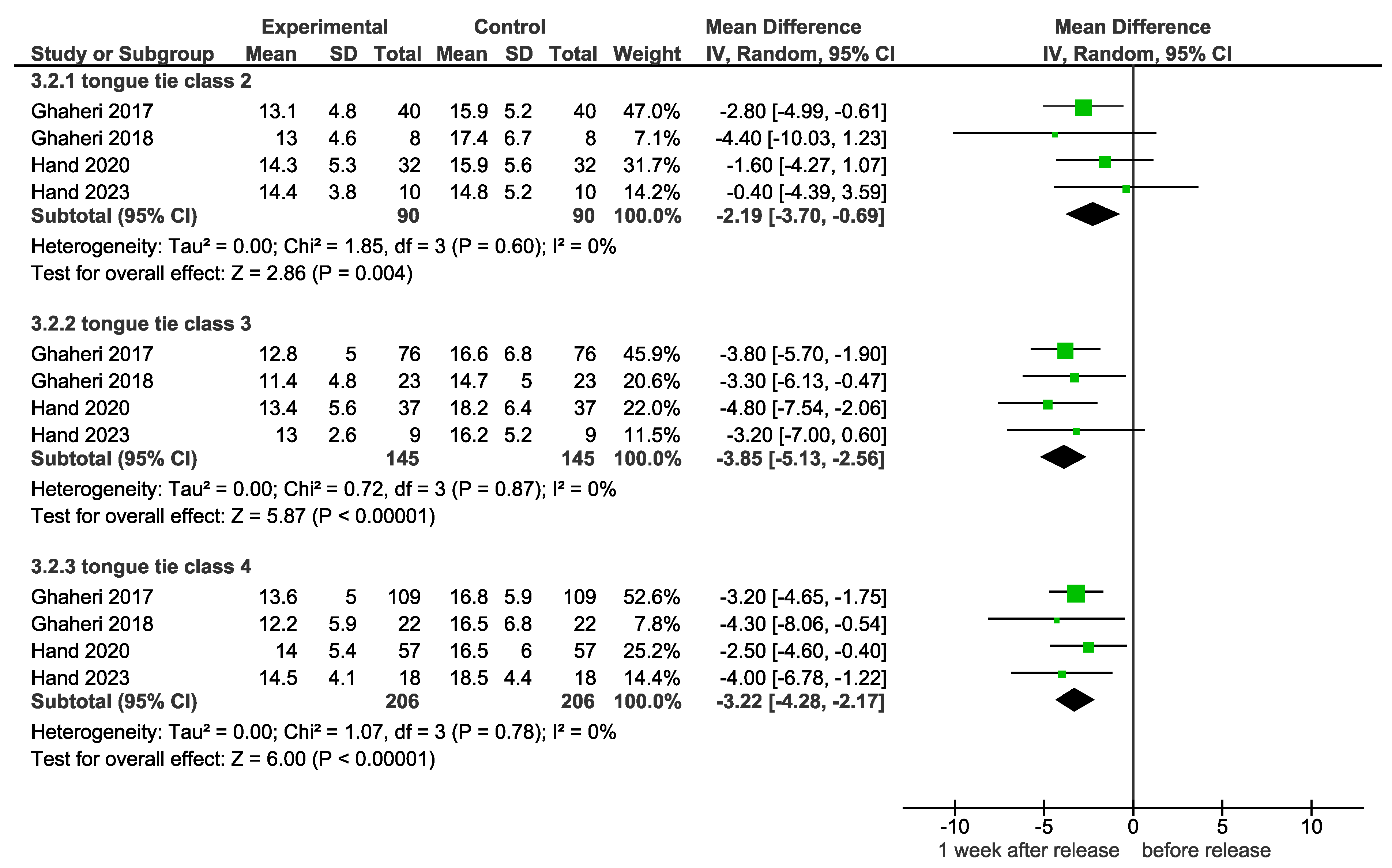
Tongue Tie
A subgroup meta-analysis was conducted comparing infants with tongue tie Type 2, tongue tie Type 3, and tongue tie Type 4 to assess the outcomes before and 1 week after release (
Figure 4d).
Tongue Tie Type 2
Four studies studies [
2,
10,
16,
17] compared the I-GERQ- R scores of infants with tongue tie Type 2 before release and 1 week after release. The subgroup meta- analysis showed a significant improvement in gastrointestinal symptoms, with SMD = 2.19 [3.70,0.69] (p = 0.004).
Tongue Tie Type 3
Four studies [
2,
10,
16,
17] compared the I-GERQ-R scores of infants with tongue tie Type 3 before release and 1 week after release. The subgroup meta-analysis showed a statistically significant improvement in gastrointestinal symptoms, with SMD = 3.85 [5.13,2.56] (p < 0.00001).
Tongue Tie Type 4
Four studies [
2,
10,
16,
17] compared the I-GERQ-R scores of infants with tongue tie Type 4 before release and 1 week after release. The subgroup meta-analysis showed a statistically significant improvement in gastrointestinal symptoms, with SMD = 3.22 [4.28,2.17] (p < 0.00001).
Clinical Significance
Overall, a statistically significant relationship between gastrointestinal improvement before and 1 week after release was found in infants presenting with Type 3 and Type 4 tongue tie.
Type 3 tongue tie exhibited a larger improvement, with an effect size of 3.85 (p < 0.00001).
Type 4 tongue tie showed a slightly smaller but still significant improvement, with an effect size of 3.22 (p < 0.00001).
Summary of Clinical Significance
The large number of posterior tongue-ties (Types 3 and 4) within the referred (and successfully treated) infants in the five studies indicates that the still widely disregarded submucosal (posterior) tongue- tie demonstrates a population of infants who are having considerable feeding problems.
The tongue must be palpated to feel the restriction. A coated dorsum of the tongue (not thrush but milk residue), poor lift and/or lateral movement of the tongue, may indicate the need for intervention.
Without the knowledge to diagnose RTOTs, this cohort of infants and their mothers struggling to feed is being ignored.
Maxillary labial restriction due to a restrictive lip- tie can affect the quality of the latch. Where indicated by poor shallow latch an upper labial frenotomy was also performed and the results from these studies suggest that this was also beneficial.
Infants requiring tongue-tie and lip-tie releases can open their mouths wider immediately after release. This increased opening allows a deeper latch to the nipple.
DISCUSSION
This is the first known systematic review to conduct meta-analysis and subgroup analyses highlighting gastrointestinal symptom improvement in infants after tongue tie and/or lip tie release with extensive research on the correlation of the classification of tongue and lip ties and their corresponding improvement.
Breastfeeding Difficulties
Efficient breastfeeding relies on the complex interplay between the physiology and behavior of both the mother and the infant. Although the reflexes required for breastfeeding are already established at birth, the extraction of milk from the breast is an acquired skill that requires the baby to adequately latch and adjust his or her oral anatomical structures to facilitate adequate feeding. [
9]
Despite the World Health Organization (WHO) recommendations for exclusive breastfeeding (EBF) for the first 6 months of life (
www.who.int), the U.S. Center for Disease Control (CDC)’s most recent report states only 24.9% of mothers reach this goal. [
10]
Numerous factors, one of them being reflux symptoms, contribute to early cessation of breastfeeding. It is of vital importance to identify and treat the causes of dysfunctional breastfeeding and associated symptoms that may result in premature cessation. [
5]
When women experience breastfeeding difficulties, frenotomy of restrictive tongue or lip ties could be an option if non-interventional professional support does not help. A frenotomy could help women with breastfeeding difficulties improve maternal functioning in early parenthood. [
15]
Infants with tongue tie and possible lip tie often have a poor latch in which there is often an inadequate seal around the breast and disorganized swallowing. As a result, many of these infants swallow air during breastfeeding and may display symptoms of reflux that is not acid induced, but rather air induced. A new term has been created to describe this entity: aerophagia induced reflux (AIR). [
6]
The tethered tongue should be considered as part of any medical differential diagnosis when infant reflux is present before invasive surgical procedures such as stomach feeding tubes, or endoscopies under a general anesthetic, placement of nasal tubes for feeding, hospitalization for failure to thrive, or placement on adult anti-reflux medication. [
11] However, the idea that the restricted tethered tongue may be a factor in developing difficulties other than preventing an infant to achieve a secure latch is often misdiagnosed or ignored completely.
Most studies evaluating the outcomes of surgical management of ankyloglossia have used objective assessment tools to gauge the degree of ankyloglossia and to evaluate breastfeeding difficulties. It is suggested that severity of these complications is determined by the degree of ankyloglossia.
Hong et al. [
24] described posterior ankyloglossia as a condition in which the lingual frenulum is not very prominent on inspection but thought to be tight on manual palpation or found to be abnormally prominent, short, thick, or fibrous cord-like when exposed with a grooved director for identification. The large number of posterior tongue-ties (71.4%) (Coryllos Type 3 and 4) within the referred (and successfully treated) infants in the six studies, indicate that the still widely disregarded submucosal (posterior) tongue-tie demonstrates a population of infants who are having considerable feeding problems. It remains a major paradigm shift within the lactation and medical community for acceptance of what we have shown is a significant issue.
Kotlow’s clinical classification described lip-ties based on the position and attachment of the frenum along the maxillary ridge. It has been postulated that a tightly attached maxillary labial frenum may interfere with lip flanging resulting in a poorer latch. However, there is a paucity of high-quality evidence that explores the relationship between the maxillary labial frenum and breastfeeding outcome. [
10]
In the six studies, 100% of the infants had a low insertion of the maxillary labial frenum, out of which Kotlow Class 3 lip tie were 51% and Class 4 lip tie were 40%.
Infants who undergo tongue-tie and lip-tie releases open their mouths wider and latch deeper to the nipple and breast or bottle, which reduces symptoms affecting the mother and infant. [
9] This has been reflected in our systematic review wherein lip and tongue tie surgery were the highest, that is 66%, in all nine included studies.
I-GERQ-R Questionnaire
Using a validated, patient-based instrument tool, most of the studies demonstrated a reduction in GERD symptom scores after frenotomy, suggesting that RTOTs may be associated with infant reflux symptoms, and that correction of latch abnormalities significantly improves reflux scores at 1 week and 1 month post-procedure. Overall, the quality of life had improved for the mother-infant dyad.
The 12 item I-GERQ-R survey [
25,
26] was used to evaluate the severity of symptoms associated with infant gastroesophageal reflux disease in five studies. It is a reliable and validated measure of infant GERD symptoms to monitor treatment outcomes in clinical practice and to serve as an evaluative tool in clinical trials.
Smith et al. (2020), in their review of 42 papers on the I-GERQ-R, which ranges in score from 0–40, identified a clinically important difference (CID) threshold of around 6. They also noted that the lower limit of the 95% confidence interval suggested a minimally important difference of 3 to 4. [
29]
Surgical Intervention
The use of electrosurgery or laser technology for frenotomies has demonstrated shorter operative working time, improved hemostasis, reduced intra- and postoperative pain and discomfort, fewer postoperative complications (e.g., swelling, infection), and increased patient acceptance. These procedures require extensive training as well as skillful technique and patient management, especially in the neonate, and should be performed by well-trained, experienced and proficient clinicians.
One of the surgeons routinely performed the tethered oral tissue release using tenotomy scissors prior to the adoption of, and transition to, laser frenotomy. The surgeon noticed no change in the success of the procedure during that transition period. [
17]
Of the eight studies that used laser, three studies [
6,
13,
14] used CO2 laser, whereas four [
2,
10,
16,
17] used diode laser; one study [
11] did specify the type of laser used.
Outcomes
Most of the studies included in this review demonstrated reduced frequency of reported reflux symptoms in the RTOTs intervention groups. Those studies demonstrated that reports of vomiting, irritability or fussiness, infant refusal to feed, choking or gagging, back arching, and severity of hiccups were all statistically better in the intervention group than controls.
Recent evidence suggests detrimental effects of indiscriminate use of adult anti-reflux medications to infants with reflux symptomology. Infants are placed on oral medication such as Acid-blocking drugs like an H-2 blocker such as ranitidine, a PPI such as omeprazole or lansoprazole. USFDA has not approved these drugs for children under 1 year of age. Studies show they are not effective, yet their use has skyrocketed. [
6,
11,
18]
If RTOTs are the cause of breastfeeding difficulties and a nonsurgical approach is uneventful, a frenotomy can be a safe procedure resulting in significant improvement of breastfeeding self- efficacy and gastroesophageal reflux problems if done cautiously by an experienced surgeon. Our results suggest evaluation of restriction of upper lip and tongue function as a treatment paradigm in infant reflux.
This is in accordance with the systematic review by Hill and Pados [
28] which stated that prior to initiation of acid-reducing medications, an oral assessment to rule out tongue tie as a potential cause of GERD is reasonable.
Limitations and Future Directions
Although the I-GERQ-R Questionnaire is subjective, until and unless there is any difficulty, the mother would not report. The ordeal of going through a surgical procedure is difficult for the mother, baby and the family at that very young age. Only if there was a genuine improvement in the symptoms would a mother happily take the second follow up. We believe the measurement tools are appropriate and have clinical relevance.
There is substantial heterogeneity in how outcomes are measured across studies. The implications of this heterogeneity on the meta-analysis findings and the ability to draw firm conclusions could be further explored.
Follow-up studies are needed for long-term follow- up to understand the persistence of gastrointestinal symptom improvements. In addition, research is needed to address comparative effectiveness, such as those that would
compare different surgical techniques or compare surgical intervention with non-surgical management strategies;
prospectively compare tongue, lip, and combined (simultaneous and staged) releases;
prospectively compare different surgical techniques (i.e., “anterior” vs. “posterior”); and
prospectively compare different surgical instruments (i.e., various lasers and scissors).