What Are We Missing in Adult Obstructive Sleep Apnea Clinical Evaluation? Review of Official Guidelines
Abstract
INTRODUCTION
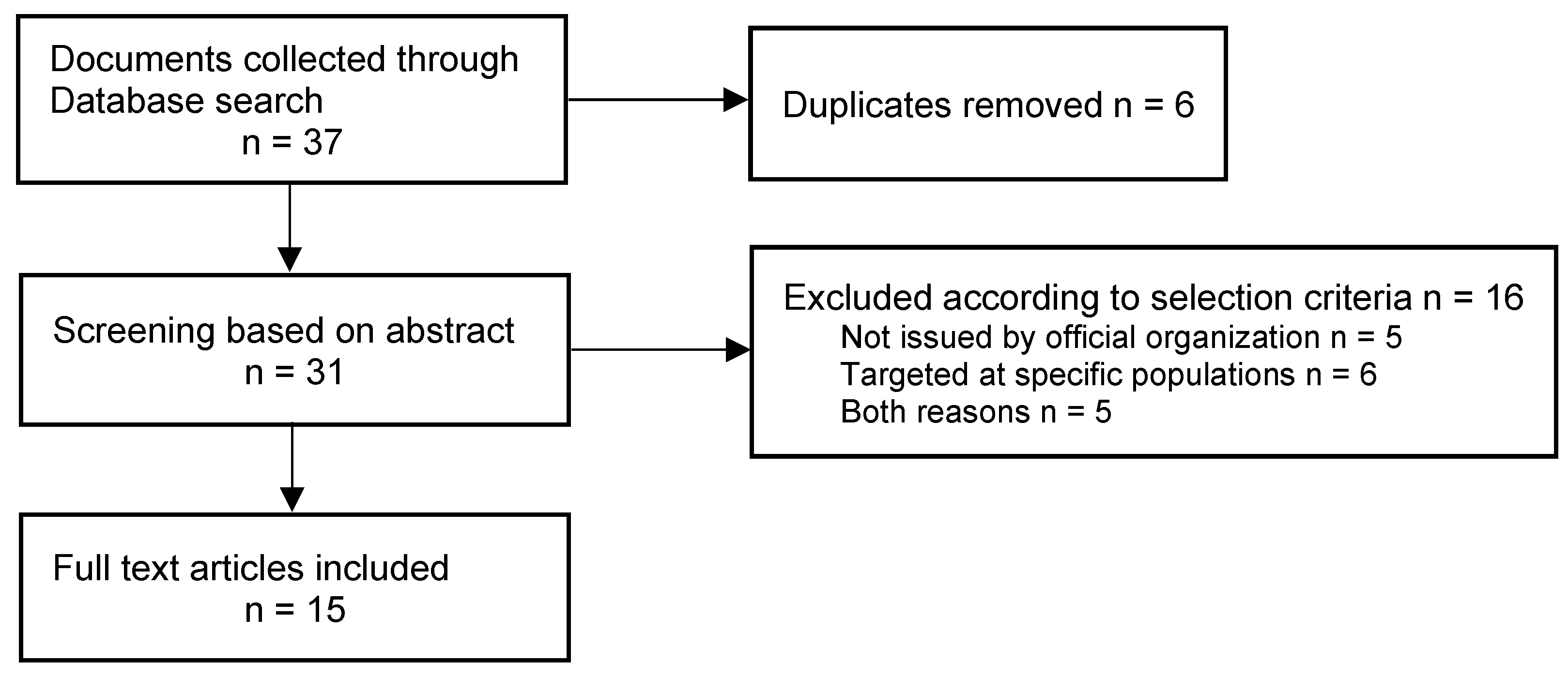
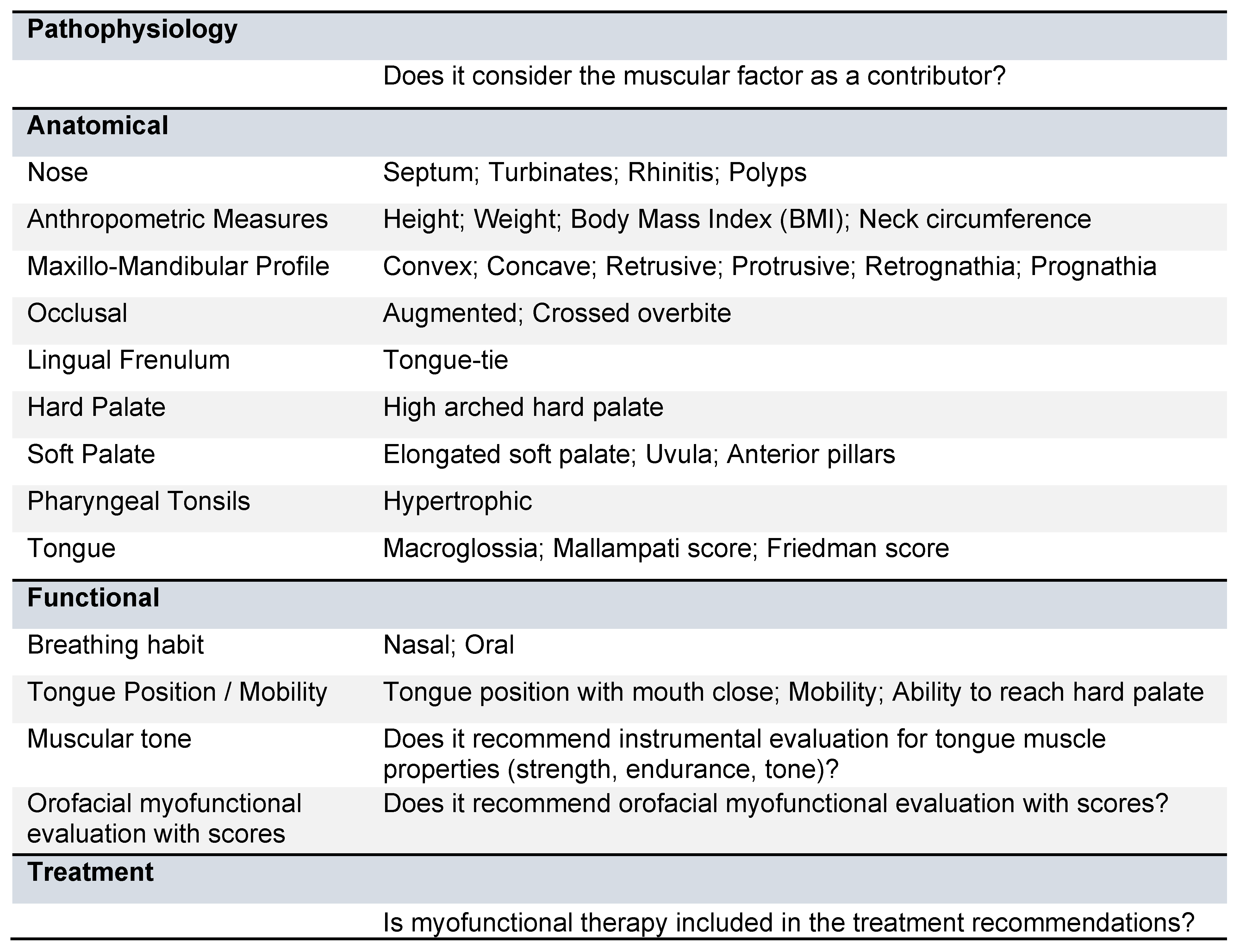
METHODS
RESULTS
DISCUSSION
CONCLUSION
Author Contributions
Data Availability Statement
References
- AAOHNS. 2021. Position Statement: Treatment of Obstructive Sleep Apnea. Available online: https://www.entnet.org/resource/position-statement-treatment-of-obstructive-sleep-apnea/.
- Adams, V., B. Mathisen, S. Baines, C. Lazarus, and R. Callister. 2013. A systematic review and meta-analysis of measurements of tongue and hand strength and endurance using the Iowa Oral Performance Instrument (IOPI). Dysphagia 28, 3: 350–369. [Google Scholar] [CrossRef] [PubMed]
- Aiello, K. D., W. G. Caughey, B. Nelluri, A. Sharma, F. Mookadam, and M. Mookadam. 2016. Effect of exercise training on sleep apnea: A systematic review and meta-analysis. Respiratory Medicine 116: 85–92. [Google Scholar] [CrossRef] [PubMed]
- Baethge, C., S. Goldbeck-Wood, and S. Mertens. 2019. SANRA-a scale for the quality assessment of narrative review articles. Research Integrity and Peer Review 4: 5. [Google Scholar] [CrossRef]
- Bamagoos, A. A., P. A. Cistulli, K. Sutherland, M. Madronio, D. J. Eckert, L. Hess, B. A. Edwards, A. Wellman, and S. A. Sands. 2019. Polysomnographic endotyping to select patients with obstructive sleep apnea for oral appliances. Annals of the American Thoracic Society 16, 11: 1422–1431. [Google Scholar] [CrossRef]
- Bassetti, C. L. A., W. Randerath, L. Vignatelli, L. Ferini-Strambi, A. K. Brill, M. R. Bonsignore, L. Grote, P. Jennum, D. Leys, J. Minnerup, L. Nobili, T. Tonia, R. Morgan, J. Kerry, R. Riha, W. T. McNicholas, and V. Papavasileiou. 2020. EAN/ERS/ESO/ESRS statement on the impact of sleep disorders on risk and outcome of stroke. European Respiratory Journal 55, 4. [Google Scholar] [CrossRef]
- Benjafield, A. V., N. T. Ayas, P. R. Eastwood, R. Heinzer, M. S. M. Ip, M. J. Morrell, C. M. Nunez, S. R. Patel, T. Penzel, J.-L. Pépin, P. E. Peppard, S. Sinha, S. Tufik, K. Valentine, and A. Malhotra. 2019. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. The Lancet. Respiratory Medicine 7, 8: 687–698. [Google Scholar] [CrossRef] [PubMed]
- Beydoun, H. A., M. A. Beydoun, H. Cheng, A. Khan, S. M. Eid, C. Alvarez-Garriga, C. Anderson-Smits, A. B. Zonderman, and D. Marinac-Dabic. 2018. Complications associated with surgical treatment of sleep-disordered breathing among hospitalized U.S. adults. Journal of Cranio-Maxillo-Facial Surgery: Official Publication of the European Association for Cranio-Maxillo-Facial Surgery 46, 8: 1303–1312. [Google Scholar] [CrossRef]
- Camacho, M., V. Certal, J. Abdullatif, S. Zaghi, C. M. Ruoff, R. Capasso, and C. A. Kushida. 2015. Myofunctional Therapy to Treat Obstructive Sleep Apnea: A Systematic Review and Meta-analysis. Sleep 38, 5: 669–675. [Google Scholar] [CrossRef]
- de Castro Corrêa, C., S. A. T. Weber, M. Evangelisti, and M. P. Villa. 2020. The short evaluation of orofacial myofunctional protocol (ShOM) and the sleep clinical record in pediatric obstructive sleep apnea. International Journal of Pediatric Otorhinolaryngology 137. [Google Scholar] [CrossRef]
- Cuesta, F. J. P., G. P. Arboledas, J. S. M. Cano, J. Durán-Cantolla, and G. E.. de Sueño. 2005. Consenso Nacional Sobre El Síndrome De Apneas-Hipopneas Del Sueño Grupo Español De Sueño (SAHS). Archivos de Bronconeumología 41: 3–110. Available online: http://www.sen.es/pdf/2005/consenso_sahs_completo.pdf.
- de Felício, C. M., F. V. da S. Dias, and L. V. V. Trawitzki. 2018. Obstructive sleep apnea: Focus on myofunctional therapy. Nature and Science of Sleep 10: 271–286. [Google Scholar] [CrossRef] [PubMed]
- de Felício, C. M., and C. L. P. Ferreira. 2008. Protocol of orofacial myofunctional evaluation with scores. International Journal of Pediatric Otorhinolaryngology 72, 3: 367–375. [Google Scholar] [CrossRef] [PubMed]
- Drazin, P. 1994. The Assessment Tool for Lingual Frenulum Function (ATLFF): Use in a Lactation Consultant Private Practice. Journal of Human Lactation 10, 1: 54. [Google Scholar] [CrossRef]
- Dutta, R., G. Delaney, B. Toson, A. S. Jordan, D. P. White, A. Wellman, and D. J. Eckert. 2021. A novel model to estimate key obstructive sleep apnea endotypes from standard polysomnography and clinical data and their contribution to obstructive sleep apnea severity. Annals of the American Thoracic Society 18, 4: 656–667. [Google Scholar] [CrossRef]
- Eckert, D. J., D. P. White, A. S. Jordan, A. Malhotra, and A. Wellman. 2013. Defining phenotypic causes of obstructive sleep apnea: Identification of novel therapeutic targets. American Journal of Respiratory and Critical Care Medicine 188, 8: 996–1004. [Google Scholar] [CrossRef]
- Epstein, L. J., D. Kristo, P. J. J. Strollo, N. Friedman, A. Malhotra, S. P. Patil, K. Ramar, R. Rogers, R. J. Schwab, E. M. Weaver, and M. D. Weinstein. 2009. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine 5, 3: 263–276. [Google Scholar]
- Esteller Moré, E., J. Vila Martín, I. Vilaseca González, M. Á. Díaz Herrera, M. Carrasco Llatas, A. Ferré Masó, J. Juvanteny Gorgals, G. Sampol Rubio, and R. Sieira Gil. 2018. Guía de práctica clínica sobre la exploración física de la vía aérea superior en el síndrome de apnea-hipoapnea obstructiva del sueño del adulto. 134. Available online: https://seorl.net/wp-content/uploads/2018/04/20180410_GUIA-PRACTICA-CLINICA-VAS-SAHOS.pdf.
- Folha, G. A., F. C. P. Valera, and C. M. de Felício. 2015. Validity and reliability of a protocol of orofacial myofunctional evaluation for patients with obstructive sleep apnea. European Journal of Oral Sciences 123, 3: 165–172. [Google Scholar] [CrossRef] [PubMed]
- Fraga, W. S., V. M. Seixas, J. C. Santos, L. R. Paranhos, and C. P. César. 2018. Mouth breathing in children and its impact in dental malocclusion: A systematic review of observational studies. Minerva Stomatologica 67, 3: 129–138. [Google Scholar] [CrossRef]
- Friedman, M. 2009. Edited by Elsevier. Friedman tongue position and the staging of obstructive sleep apnea/hypopnea syndrome. In Sleep Apnea and Snoring: Surgical and Non-Surgical Therapy. Elsevier Ltd. [Google Scholar]
- Gottlieb, D. J., and N. M. Punjabi. 2020. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA 323, 14: 1389–1400. [Google Scholar] [CrossRef]
- Guimarães, K. C., L. F. Drager, P. R. Genta, B. F. Marcondes, and G. Lorenzi-Filhoy. 2009. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. American Journal of Respiratory and Critical Care Medicine 179, 10: 962–966. [Google Scholar] [CrossRef]
- Haddad, F. L. M., L. R. A. Bittencourt, M. da C. Bagnato, R. Skomro, C. D. Fabbro, P. R. Genta, V. M. S. de Bruin, E. Zancanela, and B. N. Gomes. 2013. Diretrizes Recomendações para o Diagnóstico e Tratamento da Síndrome da Apneia Obstrutiva do Sono no Adulto, 1st ed. Edited by A. B. do Sono. Associacao Brasileira do Sono. [Google Scholar]
- Harari, D., M. Redlich, S. Miri, T. Hamud, and M. Gross. 2010. The effect of mouth breathing versus nasal breathing on dentofacial and craniofacial development in orthodontic patients. Laryngoscope 120, 10: 2089–2093. [Google Scholar] [CrossRef]
- Ieto, V., F. Kayamori, M. I. Montes, R. P. Hirata, M. G. Gregório, A. M. Alencar, L. F. Drager, P. R. Genta, and G. Lorenzi-Filho. 2015. Effects of Oropharyngeal Exercises on Snoring: A Randomized Trial. Chest 148, 3: 683–691. [Google Scholar] [CrossRef] [PubMed]
- Irish Sleep Society. 2015. Practice Management Support Document. Available online: https://irishsleepsociety.ie/wp-content/uploads/2022/03/Practice-Management-Support-Document.pdf.
- Isono, S., A. Tanaka, Y. Tagaito, T. Ishikawa, and T. Nishino. 2004. Influences of head positions and bite opening on collapsibility of the passive pharynx. Journal of Applied Physiology 97, 1: 339–346. [Google Scholar] [CrossRef] [PubMed]
- Javaheri, S., F. Barbe, F. Campos-Rodriguez, J. A. Dempsey, R. Khayat, S. Javaheri, A. Malhotra, M. A. Martinez-Garcia, R. Mehra, A. I. Pack, V. Y. Polotsky, S. Redline, and V. K. Somers. 2017. Sleep Apnea: Types, Mechanisms, and Clinical Cardiovascular Consequences. Journal of the American College of Cardiology 69, 7: 841–858. [Google Scholar] [CrossRef]
- Knösel, M., S. Klein, A. Bleckmann, and W. Engelke. 2012. Coordination of tongue activity during swallowing in mouth-breathing children. Dysphagia 27, 3: 401–407. [Google Scholar] [CrossRef]
- Koka, V., A. De Vito, G. Roisman, M. Petitjean, G. R. F. Pignatelli, D. Padovani, and W. Randerath. 2021. Orofacial myofunctional therapy in obstructive sleep apnea syndrome: A pathophysiological perspective. Medicina (Lithuania) 57, 4: 1–10. [Google Scholar] [CrossRef]
- Levine, M., K. M. Bennett, M. K. Cantwell, K. Postol, and D. B. Schwartz. 2018. Dental Sleep Medicine Standards for Screening, Treating, and Managing Adults with Sleep-Related Breathing Disorders Standards of Practice Committee of the American Academy of Dental Sleep Medicine. Journal of Dental Sleep Medicine 5, 3: 61–68. [Google Scholar] [CrossRef]
- Li, M., X. Li, and Y. Lu. 2018. Obstructive sleep apnea syndrome and metabolic diseases. Endocrinology 159, 7: 2670–2675. [Google Scholar] [CrossRef]
- Light, M., R. L. Owens, C. N. Schmickl, and A. Malhotra. 2019. Precision Medicine for Obstructive Sleep Apnea. Sleep Medicine Clinics 14, 3: 391–398. [Google Scholar] [CrossRef]
- Lloberes, P., J. Durán-Cantolla, M. Á. Martínez-García, J. M. Marín, A. Ferrer, J. Corral, J. F. Masa, O. Parra, M. L. Alonso-Álvarez, and J. Terán-Santos. 2011. Diagnóstico y tratamiento del síndrome de apneas-hipopneas del sueño. Archivos de Bronconeumologia 47, 3: 143–156. [Google Scholar] [CrossRef] [PubMed]
- Lorenzi-Filho, G., F. R. Almeida, and P. J. Strollo. 2017. Treating OSA: Current and emerging therapies beyond CPAP. Respirology (Carlton, Vic.) 22, 8: 1500–1507. [Google Scholar] [CrossRef]
- Mackay, S. G., R. Lewis, D. Mcevoy, S. Joosten, and N. R. Holt. 2020. Surgical management of obstructive sleep apnoea: A position statement of the Australasian Sleep Association. Respirology 25: 1292–1308. [Google Scholar] [CrossRef]
- Malhotra, A., O. Mesarwi, J.-L. Pepin, and R. L. Owens. 2020. Endotypes and phenotypes in obstructive sleep apnea. Current Opinion in Pulmonary Medicine 26, 6: 609–614. [Google Scholar] [CrossRef] [PubMed]
- Marchesan, I. Q. 2012. Lingual frenulum protocol. International Journal of Orofacial Myology and Myofunctional Therapy 38: 89–103. [Google Scholar] [PubMed]
- Marín Trigo, J., X. A. Corbella Ferran, and Ó. Biurrum Unzué. 1993. Diagnóstico y tratamiento del síndrome de apnea obstructiva del sueño (SAOS). Normativa SEPAR. [Google Scholar]
- Mayer, G., M. Arzt, B. Braumann, J. H. Ficker, I. Fietze, H. Frohnhofen, W. Galetke, J. T. Maurer, M. Orth, T. Penzel, H. Pistner, W. Randerath, M. Rösslein, H. Sitter, and B. A. Stuck. 2017. German S3 Guideline Nonrestorative Sleep/Sleep Disorders, chapter “Sleep-Related Breathing Disorders in Adults,” short version: German Sleep Society (Deutsche Gesellschaft für Schlafforschung und Schlafmedizin, DGSM). Somnologie 21, 4: 290–301. [Google Scholar] [CrossRef]
- Mediano, O., N. González, M. L. Alonso-álvarez, I. Almendros, A. Alonso-fernández, F. Barbé, E. Borsini, C. Caballero-eraso, I. Cano-pumarega, F. De Carlos, C. Carmona-bernal, J. Luis, C. Alduenda, E. Chiner, J. Aurelio, C. Guevara, L. De Manuel, J. Durán-cantolla, R. Farré, and S. Network. 2022. Documento internacional de consenso sobre apnea obstructiva del sueño. Archivos de Bronconeumologia 58: 52–68. [Google Scholar]
- Mediano, O., S. Romero-Peralta, P. Resano, I. Cano-Pumarega, M. Sánchez-De-la-torre, M. Castillo-García, A. B. Martínez-Sánchez, A. Ortigado, and F. García-Río. 2019. Obstructive sleep apnea: Emerging treatments targeting the genioglossus muscle. Journal of Clinical Medicine 8, 10: 1–18. [Google Scholar] [CrossRef]
- Moeller, M., S. Anna, T. Weber, L. Paskay, P. Amat, E. Gonçalves, E. Bianchini, E. Botzer, K. Boyd, O. Bruni, C. M. de Felício, H. Hrubos-Strøm, T. Jagomägi, S. Keenan, J. Moeller, D. Kwok-Keung, Ng, C. O’Connor, C. Reina, and E. Botzer. 2021. Consensus statement on the orofacial myofunctional assessment and therapy in patients with OSA: proposal of an international Delphi Method process, 513–520. [CrossRef]
- National Institute for Health and Care Excellence. 2021. Obstructive sleep apnoea/hypopnoea syndrome and obesity hypoventilation syndrome in over 16s. Evidence Review G: Oral Devices NG202. NICE. March. Available online: https://www.nice.org.uk/guidance/ng202/evidence/g-oral-devices-pdf-9204444691.
- O’Connor-Reina, C., J. M. Ignacio Garcia, L. R. Alcala, E. R. Ruiz, M. T. G. Iriarte, J. C. C. Morente, P. Baptista, and G. Plaza. 2021. Improving adherence to myofunctional therapy in the treatment of sleep-disordered breathing. Journal of Clinical Medicine 10, 24: 5772. [Google Scholar] [CrossRef]
- O’Connor-Reina, C., J. M. Ignacio Garcia, E. R. Ruiz, M. Del Carmen Morillo Dominguez, V. I. Barrios, P. B. Jardin, J. C. Casado Morente, M. T. Garcia Iriarte, and G. Plaza. 2020. Myofunctional therapy app for severe apnea–hypopnea sleep obstructive syndrome: Pilot randomized controlled trial. JMIR MHealth and UHealth 8, 11: 1–14. [Google Scholar] [CrossRef]
- Owens, R. L., D. J. Eckert, S. Y. Yeh, and A. Malhotra. 2008. Upper airway function in the pathogenesis of obstructive sleep apnea: a review of the current literature. Current Opinion in Pulmonary Medicine 14, 6: 519–524. [Google Scholar] [CrossRef]
- Patil, S. P., I. A. Ayappa, S. M. Caples, R. J. Kimoff, S. R. Patel, and C. G. Harrod. 2019. Treatment of Adult Obstructive Sleep Apnea with Positive Airway Pressure: An American Academy of Sleep Medicine Clinical Practice Guideline. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine 15, 2: 335–343. [Google Scholar] [CrossRef] [PubMed]
- Rabie, A. N., O. Mady, A. N. El-Shazly, and A. Abouzeid. 2021. Systematic Review and Meta-Analysis of the Palatal Surgeries in the Treatment of Obstructive Sleep Apnea. International Journal of Otolaryngology and Head & Neck Surgery 10, 02: 61–74. [Google Scholar] [CrossRef]
- Randerath, W., J. Verbraecken, C. A. L. De Raaff, J. Hedner, S. Herkenrath, W. Hohenhorst, T. Jakob, O. Marrone, M. Marklund, W. T. McNicholas, R. L. Morgan, J. L. Pepin, S. Schiza, N. Skoetz, D. Smyth, J. Steier, T. Tonia, W. Trzepizur, P. H. Van Mechelen, and P. Wijkstra. 2021. European Respiratory Society guideline on non-CPAP therapies for obstructive sleep apnoea. European Respiratory Review 30, 162: 210200. [Google Scholar] [CrossRef]
- Reutrakul, S., and B. Mokhlesi. 2017. Obstructive Sleep Apnea and Diabetes: A State of the Art Review. Chest 152, 5: 1070–1086. [Google Scholar] [CrossRef] [PubMed]
- Rizzatti, F. G., D. R. Mazzotti, J. Mindel, G. Maislin, B. T. Keenan, L. Bittencourt, N. H. Chen, P. A. Cistulli, N. McArdle, F. M. Pack, B. Singh, K. Sutherland, B. Benediktsdottir, I. Fietze, T. Gislason, D. C. Lim, T. Penzel, B. Sanner, F. Han, and U. J. Magalang. 2020. Defining Extreme Phenotypes of OSA Across International Sleep Centers. Chest 158, 3: 1187–1197. [Google Scholar] [CrossRef]
- Rodriguez-Alcalá, L., J. Ignacio-García, M. S. Serrano Angulo, J. C. Casado Morente, F. Benjumea Flores, and C. O’Connor-Reina. 2022. Tongue+ protocol for the diagnosis of obstructive sleep apnoea in Quirónsalud Marbella hospital. F1000Research 11(May): 322. [Google Scholar] [CrossRef]
- Rodríguez-Alcalá, L., J. M. L. Martínez, P. Baptista, R. Ríos Fernández, F. Javier Gómez, J. Parejo Santaella, and G. Plaza. 2021. Sensorimotor tongue evaluation and rehabilitation in patients with sleep-disordered breathing: a novel approach. Journal of Oral Rehabilitation 48, 12: 1363–1372. [Google Scholar] [CrossRef]
- Rodríguez-Alcalá, L., J. M. L. Martínez, C. O’Connor-Reina, and G. Plaza. 2021. Assessment of muscular tone of the tongue using a digital measure spoon in a healthy population: A pilot study. PLoS ONE 16, 2: e0245901. [Google Scholar] [CrossRef]
- Rueda, J. R., I. Mugueta-Aguinaga, J. Vilaró, and M. Rueda-Etxebarria. 2020. Myofunctional therapy (oropharyngeal exercises) for obstructive sleep apnoea. The Cochrane Database of Systematic Reviews 11, 11. [Google Scholar] [CrossRef]
- Salman, L. A., R. Shulman, and J. B. Cohen. 2020. Obstructive Sleep Apnea, Hypertension, and Cardiovascular Risk: Epidemiology, Pathophysiology, and Management. Current Cardiology Reports 22, 2. [Google Scholar] [CrossRef]
- Sawyer, A. M., N. S. Gooneratne, C. L. Marcus, D. Ofer, K. C. Richards, and T. E. Weaver. 2011. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Medicine Reviews 15, 6: 343–356. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, M., L. Acosta, Y. L. Hung, M. Padilla, and R. Enciso. 2018. Effects of CPAP and mandibular advancement device treatment in obstructive sleep apnea patients: a systematic review and meta-analysis. Sleep & Breathing=Schlaf & Atmung 22, 3: 555–568. [Google Scholar] [CrossRef]
- Sharma, S. K., V. M. oha Katoch, A. Mohan, T. Kadhiravan, A. Elavarasi, R. Ragesh, N. Nischal, P. Sethi, D. Behera, M. Bhatia, A. G. Ghoshal, D. Gothi, J. Joshi, M. S. Kanwar, O. P. Kharbanda, S. Kumar, P. R. Mohapatra, B. N. Mallick, and R. Mehta. Indian Initiative on Obstructive Sleep Apnoea Guidelines Working Group. (2014). Consensus & evidence-based INOSA Guidelines 2014 (first edition). The Indian Journal of Medical Research 140, 3: 451–468. [PubMed]
- Subramani, Y., M. Singh, J. Wong, C. A. Kushida, A. Malhotra, and F. Chung. 2017. Understanding Phenotypes of Obstructive Sleep Apnea: Applications in Anesthesia, Surgery, and Perioperative Medicine. Anesthesia and Analgesia 124, 1: 179–191. [Google Scholar] [CrossRef]
- Venema, J. A. M. U., B. R. A. M. Rosenmöller, N. de Vries, J. de Lange, G. Aarab, F. Lobbezoo, and A. Hoekema. 2021. Mandibular advancement device design: A systematic review on outcomes in obstructive sleep apnea treatment. Sleep Medicine Reviews 60: 101557. [Google Scholar] [CrossRef]
- Wong, A., S. A. Landry, S. A. Joosten, L. D. J. Thomson, A. Turton, J. Stonehouse, D. R. Mansfield, G. Burgess, A. Hays, S. A. Sands, C. Andara, C. J. Beatty, G. S. Hamilton, and B. A. Edwards. 2022. Examining the impact of multilevel upper airway surgery on the obstructive sleep apnoea endotypes and their utility in predicting surgical outcomes. Respirology. [Google Scholar] [CrossRef]
 |
 |
© 2023 by the authors. 2023 Eduardo J. Correa, Carlos O’Connor-Reina, Laura Rodríguez-Alcalá, Diego M. Conti, Alberto Rabino, Peter M. Baptista, María-Teresa García-Iriarte, Guillermo Plaza.
Share and Cite
Correa, E.J.; O'Connor-Reina, C.; Rodriguez-Alcalá, L.; Conti, D.M.; Rabino, A.; Baptista, P.M.; Garcia-Iriarte, M.-T.; Plaza, G. What Are We Missing in Adult Obstructive Sleep Apnea Clinical Evaluation? Review of Official Guidelines. Int. J. Orofac. Myol. Myofunct. Ther. 2023, 49, 1-10. https://doi.org/10.52010/ijom.2023.49.2.1
Correa EJ, O'Connor-Reina C, Rodriguez-Alcalá L, Conti DM, Rabino A, Baptista PM, Garcia-Iriarte M-T, Plaza G. What Are We Missing in Adult Obstructive Sleep Apnea Clinical Evaluation? Review of Official Guidelines. International Journal of Orofacial Myology and Myofunctional Therapy. 2023; 49(2):1-10. https://doi.org/10.52010/ijom.2023.49.2.1
Chicago/Turabian StyleCorrea, Eduardo J., Carlos O'Connor-Reina, Laura Rodriguez-Alcalá, Diego M. Conti, Alberto Rabino, Peter M. Baptista, Maria-Teresa Garcia-Iriarte, and Guillermo Plaza. 2023. "What Are We Missing in Adult Obstructive Sleep Apnea Clinical Evaluation? Review of Official Guidelines" International Journal of Orofacial Myology and Myofunctional Therapy 49, no. 2: 1-10. https://doi.org/10.52010/ijom.2023.49.2.1
APA StyleCorrea, E. J., O'Connor-Reina, C., Rodriguez-Alcalá, L., Conti, D. M., Rabino, A., Baptista, P. M., Garcia-Iriarte, M.-T., & Plaza, G. (2023). What Are We Missing in Adult Obstructive Sleep Apnea Clinical Evaluation? Review of Official Guidelines. International Journal of Orofacial Myology and Myofunctional Therapy, 49(2), 1-10. https://doi.org/10.52010/ijom.2023.49.2.1







