The Use of a Myofunctional Device in an Aged Care Population for Oral Care and Swallowing: A Feasibility Study †
Abstract
:INTRODUCTION
METHOD
Setting and Participants
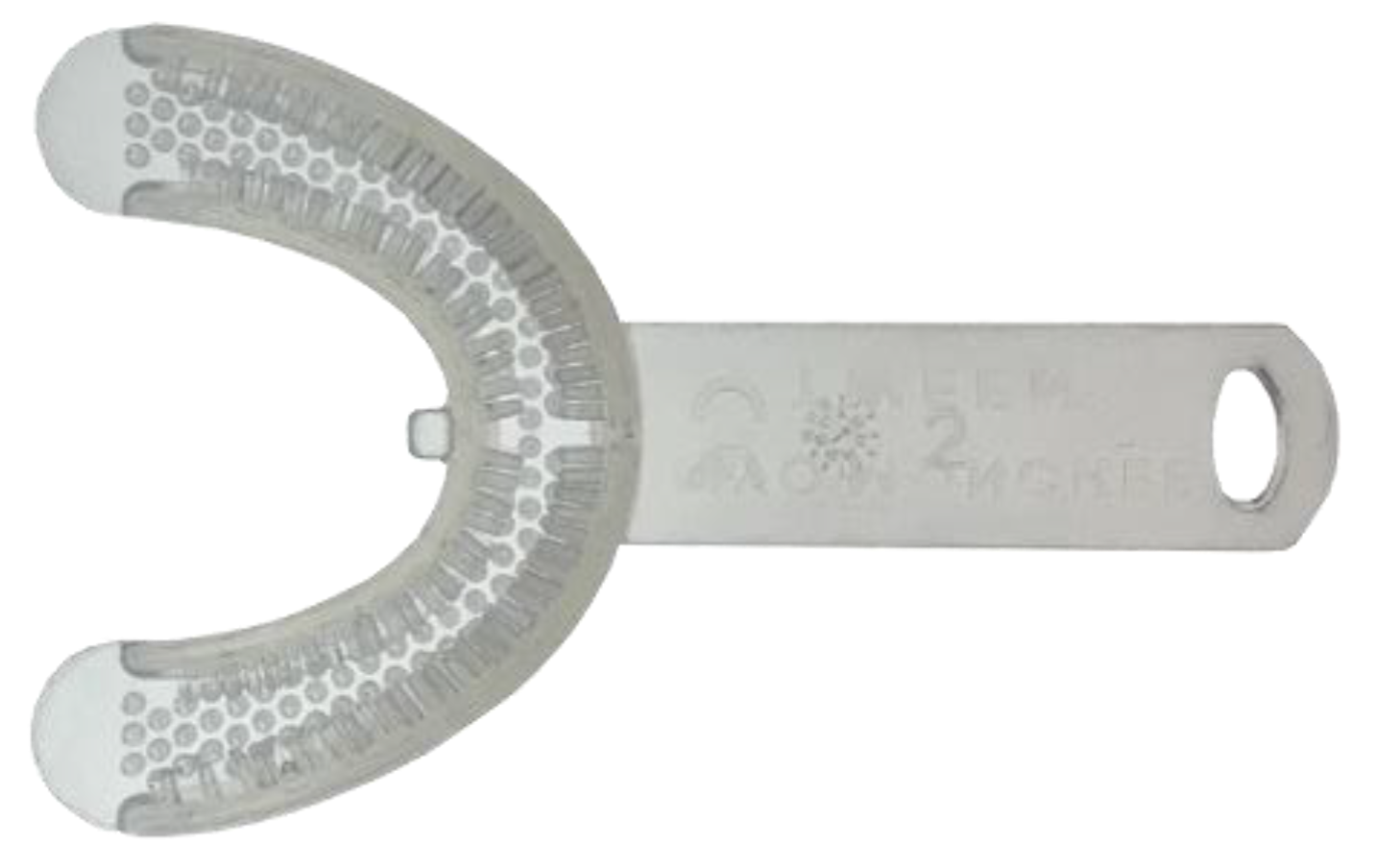
Intervention
Data Collection
Recruitment and retention
Adherence
Acceptability
Clinical Outcome Measures
Data Analysis
RESULTS
Inter-assessor Reliability
Feasibility Outcomes
Recruitment and Retention
Adherence
Acceptability
“chewing meals was easier after device use, 5 mins too long of time to do, 3 minutes easier to do” (Participant 3).
“comfortable at 2–3 minutes of use. The longer used the more uncomfortable after 2–3 minutes” (Participant 8).
Collection of Outcome Measures
DISCUSSION
Limitations
Future Directions
CONCLUSION
Author Contributions
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Outcome Measure | Area of Evaluation | Description |
| Oral Health Assessment Tool (OHAT) (Chalmers et al., 2004) | Oral health | Reliable and valid screening tool for use in aged care and with cognitive impairment. Approximately 7–8 minutes to administer; 8 items. Rating scale 0 = healthy, 1 = changes, 2 = unhealthy; Total score possible = 16. The higher the score, the worse the oral health. Items that score 1 indicate intervention is required, and items scoring 2 indicate referral to a dental professional is required. |
| Test of Mastication and Swallowing Solids (TOMASS) (Huckabee et al., 2018) | Mastication ability | Quantitative assessment of solid bolus ingestion. Sensitive in detecting changes in performance ability of mastication; high interrater and test-retest reliability. Count number of bites, number of masticatory cycles per bite, and number of swallows per bite. More likely to identify patients with subtle oral phase impairment or bolus transition issues. Normative ranges in older adults: number of bites (male = 1.47; female = 1.87), time (male = 32.61s; female = 41.85s), total number of swallows (male = 3.61/female = 3.5), masticatory cycle (male = 37.6; female = 41.65). |
| Timed Water Swallow Test (TWST) (Hughes & Wiles, 1996) | Aspiration risk | Swallow speed is a sensitive indicator for identifying patients at risk of swallow dysfunction. Choking on 100ml TWST may be a potential indicator for follow-up aspiration. Measures swallow time, number of swallows and observes for signs of choking. Abnormal swallow is defined as a speed below 10ml/s (amount of water divided by elapsed time); count the number of swallows taken to consume 100ml of water and time taken to consume 100ml of water. |
| Mann Assessment of Swallowing Ability (MASA) (Mann, 2002) | Identify swallowing disorders | Screening bedside tool to identify eating and swallowing disorders in stroke and other diseases. Used to quantify aspiration risk; 24 clinical items; 4 components of the assessment include general patient examination, oral preparation, oral phase, and pharyngeal phase; 5–10 point rating scale. Total score possible = 200; >178 = normal, 168–177 = mild, 139–167 = moderate, <138 = severe. Risk of aspiration is defined by a sum of the 4 scores/categories, >170 = normal, 149–169 = mild, 141–148 = moderate, <140 = severe. |
| Functional Oral Intake Scale (FOIS) (Crary et al., 2005) | Functionality | Functional level of oral intake of food and liquid; interrater reliability high and sensitive to changes. 7-point ordinal scale: Levels 1–3 relate to non-oral feeding; Levels 4–7 relate to varying degrees of oral feeding; all levels focus on what is/not consumed orally. |
| Eating Assessment Tool (EAT-10) (Belafsky et al., 2008) | Self-perceived symptoms | Screen self-perceived symptoms of oropharyngeal dysphagia. Scores range from 0–40; Scores >3 indicates dysphagia. 10 questions rated on a 5-point scale, 0 = no problem, 4 = severe problem. Scores >15 indicate aspiration risk. An elevated score indicates a higher self-perception of dysphagia. |
References
- Affoo, R., and S. Hachey. 2022. Integrating oral health in speech-language pathology practice: A viewpoint. Perspectives of the ASHA Special Interest Groups, 1–11. [Google Scholar] [CrossRef]
- Ajwani, S., S. Jayanti, N. Burkolter, C. Anderson, S. Bhole, R. Itaoui, and A. George. 2017. Integrated oral health care for stroke patients—A scoping review. Journal of Clinical Nursing 26, 7–8: 891–901. [Google Scholar] [CrossRef] [PubMed]
- American Speech & Hearing Association (ASHA). 2022. Dysphagia. Available online: https://www.asha.org/practice-portal/clinical-topics/late-language-emergence/assessment-tools-techniques-and-data-sources/ (accessed on 1 October 2022).
- Aquilanti, L., S. Alia, S. Pugnaloni, E. Coccia, M. Mascitti, A. Santarelli, L. Limongelli, G. Favia, M. Mancini, A. Vignini, and G. Rappelli. 2020. Impact of elderly masticatory performance on nutritional status: An observational study. Medicina 56, 130. [Google Scholar] [CrossRef]
- Australian Government Department of Health. 2019. Dental health. Available online: https://www.health.gov.au/health-topics/dental-health (accessed on 1 October 2022).
- Australian Health Ministers Advisory Council (AHMAC). 2017. Aboriginal and Torres Strait Islander health performance framework 2017 report. Canberra. [Google Scholar]
- Australian Institute of Health & Welfare (AIHW). 2021. Oral health and dental care in Australia. Available online: https://www.aihw.gov.au/reports/dental-oral-health/oral-health-and-dental-care-in-australia/contents/introduction (accessed on 19 August 2022).
- Badiah, B., P. Kang, W. Hor, M. Razali, and T. Mohd Dom. 2013. Exploring factors influencing adherence to oral hygiene care among periodontal patients: A pilot study. Sains Malaysiana 42: 13–17. [Google Scholar]
- Belafsky, P.C., D.A. Mouadeb, C.J. Rees, J.C. Pryor, G.N. Postma, J. Allen, and R.J. Leonard. 2008. Validity and reliability of the eating assessment tool (EAT-10). Annals of Otology, Rhinology & Laryngology 117, 12: 919–24. [Google Scholar] [CrossRef]
- Bourke, K. n.d.9th Asian Pacific Conference. The chewing brush. Oral Physiotherapy Lecture 12. Available online: https://static1.squarespace.com/static/57ba3862893fc01e071991d8/t/5912949f2e69cf5fef74e9fb/1494389920781/The+Chewing+Brush.pdf (accessed on 28 June 2022).
- Bourke, M., and C. Clayton. 2018. Myo munchee: A practitioner user guide.
- Bulgareli, J.V., K.L. Cortellazzi, L.M. Guerra, G.M. Bovi Ambrosano, A.K. Kaieda, I.P. da Cunha, F. de Lima Vazquez, and A.C. Pereira. 2021. Determinants of adherence to dental treatment of socially vulnerable adolescents: A cohort study. BMC Res Notes 14: 116. [Google Scholar] [CrossRef]
- Chalmers, J., V. Johnson, J.H. Tang, and M.G. Titler. 2004. Evidence-based protocol: Oral hygiene care for functionally dependent and cognitively impaired older adults. Journal Gerontology Nursing 30, 11: 5–12. [Google Scholar]
- Colgate. 2022. Brushing and flossing. Available online: https://www.colgate.com.au/oral-health/brushing-and-flossing/3-tooth-brushing-techniques-that-get-the-job-done (accessed on 1 October 2022).
- Council of Australian Governments Health Council. 2017. Healthy mouths, healthy lives: Australia’s national oral health plan 2015–2024. Performance Monitoring Report: Baseline Report. Victoria: Dental Health Services Victoria. [Google Scholar]
- Crary, M.A., G.D. Carnaby-Mann, and M.E. Groher. 2005. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Archives of Physical Medicine and Rehabilitation 86: 1516–1520. [Google Scholar] [CrossRef]
- Danckert, R., A. Ryan, V. Plummer, and C. Williams. 2016. Hospitalisation impacts on oral hygiene: An audit of oral hygiene in a metropolitan health service. Scandinavian Journal of Caring Sciences 30, 1: 129–134. [Google Scholar] [CrossRef]
- de Felício, C.M., M. Melchior, O. de, and M.A.M.R. da Silva. 2010. Effects of orofacial myofunctional therapy on temporomandibular disorders. CRANIO® 28, 4: 249–259. [Google Scholar] [CrossRef] [PubMed]
- Dodd, S., I.R. White, and P. Williamson. 2012. Nonadherence to treatment protocol in published randomised controlled trials: a review. Trials Journal 13: 84. [Google Scholar] [CrossRef]
- Drapal, C.S. 2015. Oral care practice guidelines for the care-dependent hospitalized adult outside of the intensive care unit setting. Available online: https://scholarworks.waldenu.edu/cgi/viewcontent.cgi?article=1408&context=dissertations&httpsredir=1&referer= (accessed on 1 October 2022).
- Eldridge, S.M., C.L. Chan, M.J. Campbell, C.M. Bond, S. Hopewell, and L. Thabane. 2010. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ 355: i5239. [Google Scholar] [CrossRef]
- Farrell, D.C., and M. Darcy. 2018. The history of myofunctional orthodontics: Part 1. The beginning & the separation. Australian Dental Practice, Special Report May/June: 74–76. Available online: https://myoresearch.com/storage/app/media/history-of-myofunctional-orthodontics-part-I-0518.pdf (accessed on 1 August 2022).
- Fricker, A., and A. Lewis. 2009. Better oral health in residential care–final report; Central Northern Adelaide Health Service, South Australian Dental Service, Adelaide. Available online: https://www.sahealth.sa.gov.au/wps/wcm/connect/32902a8043506b6a91bef32835153af6/SADS-BOHP-Fin-Report-Nov-09.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-32902a8043506b6a91bef32835153af6-nKKIejJ (accessed on 1 October 2022).
- Hägglund, P., M. Hägg, P. Wester, and E. Levring Jäghagen. 2019. Effects of oral neuromuscular training on swallowing dysfunction among older people in intermediate care: A cluster randomised, controlled trial. Age and Ageing 48, 4: 533–540. [Google Scholar] [CrossRef]
- Huckabee, M.L., T. McIntosh, L. Fuller, M. Curry, P. Thomas, M. Walshe, E. McCague, I. Battel, D. Nogueira, U. Frank, L. van den Engel-Hoek, and O. Sella-Weiss. 2018. The test of masticating and swallowing solids (TOMASS): Reliability, validity and international normative data. International Journal of Language and Communication Disorders 53, 1: 144–156. [Google Scholar] [CrossRef] [PubMed]
- Hughes, T.A., and C.M. Wiles. 1996. Clinical measurement of swallowing in health and in neurogenic dysphagia. Quarterly Journal of Medicine 89: 109–16. [Google Scholar] [CrossRef]
- In, J. 2017. Introduction of a pilot study. Korean Journal of Anesthesiology 70, 6: 601–605. [Google Scholar] [CrossRef] [PubMed]
- International dysphagia diet standardisation initiative (IDDSI). 2019. Complete IDDSI framework detailed definitions. Available online: https://iddsi.org/IDDSI/media/images/Complete_IDDSI_Framework_Final_31July2019.pdf (accessed on 19 August 2022).
- Kenny, C., J. Regan, L. Balding, S. Higgins, N. O'Leary, F. Kelleher, R. McDermott, J. Armstrong, A. Mihai, E. Tiernan, J. Westrup, P. Thirion, and D. Walsh. 2019. Dysphagia prevalence and predictors in cancers outside the head, neck, and upper gastrointestinal tract. Journal of Pain and Symptom Management 58, 6: 949–958.E2. [Google Scholar] [CrossRef]
- Krekeler, B.N., C.K. Broadfoot, S. Johnson, N.P. Connor, and N. Rogus-Pulia. 2018. Patient adherence to dysphagia recommendations: A systematic review. Dysphagia 33, 2: 173–184. [Google Scholar] [CrossRef]
- Langmore, S.E., M.S. Terpenning, A. Schork, Y. Chen, J.T. Murray, D. Lopatin, and W.J. Loesche. 1998. Predictors of aspiration pneumonia: How important is dysphagia? Dysphagia 13, 2: 69–81. [Google Scholar] [CrossRef]
- Lombardo, L., C. Ferguson, A. George, A.R. Villarosa, B.J. Villarosa, A.C. Kong, R. Wynne, and Y. Salamonson. 2022. Interventions to promote oral care regimen adherence in the critical care setting: A systematic review. Australian Critical Care: Official Journal of the Confederation of Australian Critical Care Nurses 35, 5: 583–594. [Google Scholar] [CrossRef] [PubMed]
- Luong, E., P. Drysdale, E. Campbell, J. deClifford, S.H. Lam, J. Coutsouvelis, and R. Danckert. 2018. Implementation of standardised oral care treatment and referral guidelines for older sub-acute patients: A multidisciplinary approach. Journal of Pharmacy Practice and Research 48, 1: 10–17. [Google Scholar] [CrossRef]
- Mann, G. 2002. MASA, The Mann Assessment of Swallowing Ability. New York, NY: Cengage Learning, Vol. 1. [Google Scholar]
- Molloy, D.W., and T.I. Standish. 1997. A guide to the standardized Mini-Mental State Examination. International Psychogeriatrics 9 Suppl. 1: 87–94, discussion 143–50. [Google Scholar] [CrossRef]
- Murray, J., and I. Scholten. 2018. An oral hygiene protocol improves oral health for patients in inpatient stroke rehabilitation. Gerodontology 35: 18–24. [Google Scholar] [CrossRef] [PubMed]
- National Research Council (US) Committee on the Role of Human Factors in Home Health Care. 2010. The role of human factors in home health care: Workshop summary; Washington, DC: National Academies Press (US): 8, Medical Devices in Home Health Care. Available online: https://www.ncbi.nlm.nih.gov/books/NBK210047 (accessed on 2 August 2022).
- Patel, J., J. Wallace, M. Doshi, M. Gadanya, B. Yahya, J. Roseman, and P. Srisilapanan. 2021. Personal view oral health for healthy ageing challenges for oral health in ageing populations. The Lancet 2: E521–E527. [Google Scholar] [CrossRef]
- Patterson Norrie, T., A.R. Villarosa, A.C. Kong, S. Clark, S. Macdonald, R. Srinivas, J. Anlezark, and A. George. 2020. Oral health in residential aged care: Perceptions of nurses and management staff. Nursing Open 7: 536–546. [Google Scholar] [CrossRef]
- Powell-Cope, G., A.L. Nelson, and E.S. Patterson. 2008. Patient care technology and safety (Chapter 50). Edited by R. G. Hughes. In Patient safety and quality: An evidence-based handbook for nurses. Rockville (MD): Agency for Healthcare Research and Quality (US). Available online: https://www.ncbi.nlm.nih.gov/books/NBK2686/ (accessed on 1 October 2022).
- Santoro, P., I.L. de Silva, F. Cardoso, E. Dias, and H. Beresford. 2011. Evaluation of the effectiveness of a phonoaudiology program for the rehabilitation of dysphagia in the elderly. Archives of Gerontology and Geriatrics 53, 1: e61–e66. [Google Scholar] [CrossRef]
- Shortland, H.L., S. Hewat, A. Vertigan, and G. Webb. 2021. Orofacial myofunctional therapy and myofunctional devices used in speech pathology treatment: A systematic quantitative review of the literature. American Journal of Speech-Language Pathology 30, 1: 301–317. [Google Scholar] [CrossRef] [PubMed]
- Shortland, H.A.L., G. Webb, A.E. Vertigan, and S. Hewat. 2022a. Speech-language pathologists' use of myofunctional devices in therapy programs. Perspectives of the ASHA Special Interest Groups 7, 6: 2012–2026. [Google Scholar] [CrossRef]
- Shortland, H.A.L., S. Hewat, G. Webb., and A. Vertigan. 2022b. Myofunctional device use in oral care and swallowing: A protocol for a feasibility study in an aged care population. Pilot Feasibility Studies 8: 187. [Google Scholar] [CrossRef]
- Tang, A., J.J. Eng, and D. Rand. 2012. Relationship between perceived and measured changes in walking after stroke. Journal of Neurologic Physical Therapy: JNPT 36, 3: 115–121. [Google Scholar] [CrossRef] [PubMed]
- Thabane, L., and G.A. Lancaster. 2019. Guide to the reporting of protocols of pilot and feasibility trials. Pilot Feasibility Studies. [Google Scholar] [CrossRef]
- Tkatch, R., S. Musich, S. MacLeod, K. Alsgaard, K. Hawkins, and C.S. Yeh. 2016. Population health management for older adults: Review of interventions for promoting successful aging across the health continuum. Gerontology Geriatric Medicine 2: 2333721416667877. [Google Scholar] [CrossRef]
- Wagner, S., I. Rosian-Schikuta, and J. Cabral. 2022. Oral-care adherence. Service design for nursing homes-initial caregiver reactions and socio-economic analysis. German Medical Science: GMS e-journal 20: Doc04. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.F., C.M. Huang, C. Chou, and S. Yu. 2015. Effect of oral health education programs for caregivers on oral hygiene of the elderly: A systemic review and meta-analysis. International Journal of Nursing Studies 52, 6: 1090–1096. [Google Scholar] [CrossRef]
- World Health Organization (WHO). 2003. Edited by T. Tan-Torres, T. Edejer, R. Baltussen, T. Adam, R. Hutbessy, A. Acharya, D.B. Evans and C.J.L. Murray. Making choices in health: WHO guide to cost-effectiveness analysis. Available online: https://apps.who.int/iris/handle/10665/42699 (accessed on 2 August 2022).
- World Health Organisation (WHO). 2022. Ageing & Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 1 October 2022).
- Ziebolz, D., C. Werner., G. Schmalz, I. Nitschke, R. Haak, R.F. Mausberg, and J.F. Chenot. 2017. Oral Health and nutritional status in nursing home residents-results of an explorative cross-sectional pilot study. BMC Geriatrics 17, 1: 39. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Age ≥ 65 years | On an end of life/palliative care pathway |
| Ability to understand English and follow instructions for timed water swallow test and use of the myofunctional device | Inability to provide informed consent including diminished understanding or comprehension, or inadequate English proficiency to follow directions for the intervention |
| Residents receiving texture modified diets (including normal cut up, easy chew, minced moist, and puree diets) and/or fluids | Conditions that interfere with a patient's ability to comply with all treatment(s) and procedure(s) and to follow study guidelines |
| Residents with natural teeth, dentures (partial and full), or edentulous | Identified by the visiting oral health professional to have tooth mobility |
| Identified Temporomandibular Dysfunction by dental practitioner |
| Demographics | Age in years; Mean, (Range) | 87.1 (74-99) |
| Gender, N (%) | 10 females (76.9%) | |
| 3 males (23.1%) | ||
| Functional Status | Level of Care | *Low level 7 (53.8%) |
| **Moderate level 6 (46.1%) | ||
| Feeding ability | 13 could self-feed (100%) 3 required set-up of meals (23%) | |
| Dentition | Natural teeth (15.4%) | |
| Partial denture (23.1%) | ||
| Upper denture (7.7%) | ||
| Upper and lower denture (53.8%) | ||
| Diet (IDDSI level) | Food | 13 IDDSI level 7 (easy to chew) (100%) |
| 3 Extra sauces required (23.1%) | ||
| Drinks | 13 IDDSI level 0 (thin) (100%) | |
| Medical Background (grouped by the number of residents presenting with each medical diagnosis) | Hypertension | 8 (61.5%) |
| Depression | 6 (46.1%) | |
| Cognitive Decline, Thyroid, | 3 (23%) | |
| Arthritis | ||
| Vision impairment, hearing impairment, cardiovascular disease, asthma, bladder cancer, Parkinson disease | 2 (15.3%) | |
| Polio, transient ischemic attack, osteoporosis, prostate cancer, amputation, traumatic brain injury, diabetes, post-traumatic stress disorder | 1 (7.6%) |
| Participant | Week 3 Adherence (%) | Week 5 Adherence (%) |
|---|---|---|
| 1 | 100.0 | 100.0 |
| 2 | 71.4 | 51.4 |
| 3 | 100.0 | 91.4 |
| 4 | 90.4 | 94.2 |
| 5 | 88.0 | 67.1 |
| 6 | 97.6 | 92.8 |
| 7 | 83.3 | 87.1 |
| 8 | 100.0 | 100.0 |
| 9 | 100.0 | 100.0 |
| 10 | 83.3 | 90.0 |
| 11 | 100.0 | 100.0 |
| 12 | 97.6 | 98.5 |
| Average | 92.6 | 89.3 |
| Targeted Outcome | No Change Number (%) | Unsure Number (%) | Positive Change Number (%) |
|---|---|---|---|
| Oral hygiene | 5 (45.4%) | 1 (9.0%) | 5 (45.4%) |
| Saliva | 6 (54.5%) | 1 (9.0%) | 4 (36.3%) |
| Swallowing | 9 (81.8%) | 2 (18.1%) | 0 |
| Chewing | 7 (63.6%) | 2 (18.1%) | 2 (18.1%) |
| Targeted Outcome | Unsure of Change Number (%) | Positive Change Number (%) |
|---|---|---|
| Oral hygiene | 4 (40%) | 6 (60%) |
| Saliva | 8 (80%) | 2 (20%) |
| Swallowing | 8 (80%) | 2 (20%) |
| Chewing | 8 (80%) | 2 (20% |
| Outcomes | Measurement | Criteria | Average Percentage for all Participants |
|---|---|---|---|
| Study Recruitment and Retention | |||
| Recruitment consent rate | Proportion of eligible residents consented | >30% | 61.9 |
| Recruitment retention rate | Proportion of residents who completed the 5-week intervention | >70% | 92.3 |
| Adherence to the intervention protocol | |||
| Occasions of use after 3 weeks | Total number of device usage from 42 possible occasions | >85% | 92.6 |
| Occasions of use after 5 weeks | Total number of device usage from 70 possible occasions | >70% | 89.3 |
| Acceptability | |||
| Resident ease of use | Five-point Likert scale Very Easy – Very Difficult | 70% rate as easy or very easy | 100.0 |
| Resident oral comfort | Five-point Likert scale Very Comfortable – Very Uncomfortable | 70% rate as comfortable or very comfortable | 90.9 |
| Care staff perception of resident’s ease of device use | Five-point Likert scale Very Easy – Very Difficult | 70% rate as easy or very easy | 70.0 |
| No impact on care staff workload (time) | Yes/Unsure/No | 70% respond Yes/Unsure | 70.0 |
© 2023 by the authors. 2023 Hollie-Ann L. Shortland, Gwendalyn Webb, Anne E. Vertigan, Sally Hewat.
Share and Cite
Shortland, H.-A.L.; Webb, G.; Vertigan, A.E.; Hewat, S. The Use of a Myofunctional Device in an Aged Care Population for Oral Care and Swallowing: A Feasibility Study. Int. J. Orofac. Myol. Myofunct. Ther. 2023, 49, 1-13. https://doi.org/10.52010/ijom.2023.49.1.2
Shortland H-AL, Webb G, Vertigan AE, Hewat S. The Use of a Myofunctional Device in an Aged Care Population for Oral Care and Swallowing: A Feasibility Study. International Journal of Orofacial Myology and Myofunctional Therapy. 2023; 49(1):1-13. https://doi.org/10.52010/ijom.2023.49.1.2
Chicago/Turabian StyleShortland, Hollie-Ann L., Gwendalyn Webb, Anne E. Vertigan, and Sally Hewat. 2023. "The Use of a Myofunctional Device in an Aged Care Population for Oral Care and Swallowing: A Feasibility Study" International Journal of Orofacial Myology and Myofunctional Therapy 49, no. 1: 1-13. https://doi.org/10.52010/ijom.2023.49.1.2
APA StyleShortland, H.-A. L., Webb, G., Vertigan, A. E., & Hewat, S. (2023). The Use of a Myofunctional Device in an Aged Care Population for Oral Care and Swallowing: A Feasibility Study. International Journal of Orofacial Myology and Myofunctional Therapy, 49(1), 1-13. https://doi.org/10.52010/ijom.2023.49.1.2





