Abstract
Purpose: Poor oral health is a known predictor of aspiration pneumonia in vulnerable populations such as the elderly and chronically ill. This study examined the feasibility of using myofunctional devices during a 5-week intervention for the management of oral care and dysphagia for residents in a residential aged-care facility. Method: Feasibility was determined through evaluation of study recruitment and retention rates, adherence to intervention, and resident and staff acceptability of the intervention. Thirteen residents, ages 74–99, participated in the intervention and 10 care staff completed feedback on post-intervention questionnaires. Results: Enrolment and retention rates were 61.9% and 92.3%, respectively. Adherence rates for use of the device were 92.6% at 3 weeks, and 89.3% at 5 weeks for the 12 participants who completed the protocol. The device was considered acceptable for ease of use, comfort, and amount of support required. Conclusion: Results indicate that further research exploring device use in an aged care population for the management of dysphagia and oral hygiene is feasible.
INTRODUCTION
Globally, there is an increase in older persons in the population, with a predicted rise of those over the age of 60 years from 12% to 22% between the years of 2015 to 2050 (World Health Organization (WHO), 2022). The increase in life expectancy is due to improvements in health, wellbeing, and access to health care (Aquilanti et al., 2020; Australian Institute of Health & Welfare (AIHW), 2021). Further factors that influence healthy aging include physical activity, adequate nutrition, and both psychological and social wellbeing (Tkatch et al., 2016). With the global aging population expected to continue to increase, there is a need to ensure healthy aging to prevent disability and disease (Aquilanti et al., 2020).
Poor oral health is a strong predictor of adverse health outcomes, especially in the elderly (Aquilanti et al., 2020). The link between poor oral health with systemic disease, morbidity and mortality has been demonstrated extensively throughout the literature (Danckert et al., 2016; Wang et al., 2015). Oral health is important across the lifespan; however, it deteriorates with age (Council of Australian Governments Health Council, 2017). On average, adults 75 years and older have 24.4 decayed, missing, or filled teeth (AIHW, 2021; Council of Australian Governments Health Council, 2017). The Australian Health Ministers Advisory Council (AHMAC) (2017) identified that one of the four population groups that are at greater risk of poor oral health are people with additional and/or specialized health care needs such as those with mental illness or the frail older population.
Reduced oral health and the ability to manage oral health independently are known predictors of aspiration pneumonia in vulnerable populations such as the elderly and chronically unwell (Langmore et al., 1998). Poor oral health may also result in changes to dentition and pain, with impacts on mastication for swallowing, the potential for malnutrition, reduced quality of life, and poorer health outcomes (Luong et al., 2018). Quality of life and health outcomes are linked to nutrition especially among the elderly, with morbidity and mortality influenced by oral intake (Ziebolz et al., 2017). The Age Care Commission in Australia highlights that a healthy mouth is essential for oral health and well-being and is important for healthy aging (Fricker & Lewis, 2009).
Currently, oral care protocols with measurable outcomes used in hospitals and care facilities in Australia and the United Kingdom are inconsistent and lack standardised implementation by staff (Affoo & Hachey, 2022; Drapal, 2015). The impact of poor oral health on mastication, swallowing function and the increased risk of aspiration is of particular concern to speech-language pathologists (SLPs). Approaches by SLPs in the management of dysphagia have predominantly been compensatory and restorative (American Speech, Language, and Hearing Association (ASHA), 2022). However, preventative measures such as simple oral-care protocols may have a role in minimising oral health deterioration and aspiration pneumonia for those at increased risk of swallowing difficulties in populations such as those in aged care. Relatedly, a recent review has highlighted the use of orofacial myofunctional therapy (OMT) and myofunctional devices (MD) as potential interventions for the management of oral hygiene and swallowing function (Shortland et al., 2021).
The use of oral devices for the correction of malocclusion and dental-related disorders is well supported in the dental and orthodontic literature (Farrell & Darcy, 2018; de Felício et al., 2010). However, some SLPs are providing services that incorporate MDs as part of their therapy programs in communication and swallowing (Shortland et al., 2022a). Positive and rapid outcomes in therapy have been reported by some SLPs with the use of MDs in several areas including swallowing, habit correction, breathing, speech, and oral health (Shortland et al., 2022a). However, there are currently still limited studies available with evidence to support the use of MDs in SLP practice and very few that specifically consider the aged care population (Shortland et al., 2021). It would be relevant to further explore the use of MDs in a population such as the elderly who make up a large proportion of those with oral health and swallowing difficulties, for whom function may be impacted (Santoro et al., 2011).
The aim of this study was to determine the feasibility of the use of a MD in improving oral health and dysphagia in an aged care population. Thabane and Lancaster (2019), In (2017), and Eldridge and colleagues (2010) highlighted the importance of feasibility studies to further guide, inform, conduct, and design a larger clinical trial or future research. The published protocol reported by Shortland and colleagues (2022b) provides criteria for trialling an MD to determine the feasibility of their use with an aged care population for the management of oral hygiene, swallowing function, and dysphagia.
METHOD
This feasibility study was registered with the Australian New Zealand Clinical Trials Registry and was conducted according to the published protocol for MD use in oral care and swallowing aged care population (Shortland et al., 2022b). This study obtained ethical approval by the University of Newcastle Human Research Ethics Committee (HREC) H-2021-0250 (18 August 2021). All participants provided written informed consent.
Setting and Participants
This was a single-arm feasibility study conducted at a residential aged care facility (RACF) in Newcastle, Australia. A multilevel care facility was chosen as the study site due to the range of residents’ level of independence. Further, as the study was conducted during the COVID-19 pandemic, a single site was appropriate to reduce the possibility of cross- contamination across multiple sites.
Fifty RACF care staff attended training for supervision of residents involved in the study and all were invited to complete a post-intervention questionnaire. The questionnaire was designed to collect care staff’s perception of resident’s acceptance of the device, changes in oral care, and swallowing, as well as the impact on staff workload during the intervention period.
Intervention
An MD (Myo MuncheeTM), pictured in Figure 1, was used as the intervention tool, and the intervention protocol was developed based on information reported in previous studies (Hägglund et al., 2019; Shortland et al., 2021; Shortland et al., 2022a). The Myo MuncheeTM is shaped like a mouthguard with silicone prongs to massage the gums and teeth (Bourke & Clayton, 2018). The original development of the device was by the late Dr Kevin Bourke, an Australian dentist, with the purpose of improving oral hygiene and gum health (Bourke, n.d.).
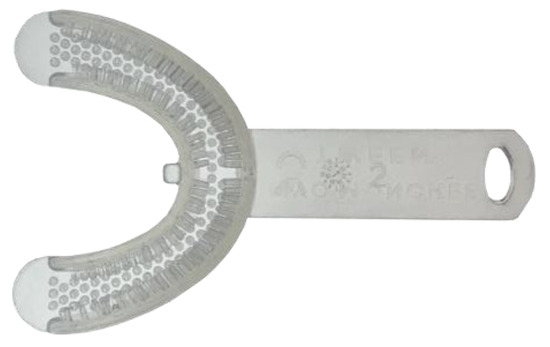
Figure 1.
Myofunctional device, the Myo MuncheeTM (photograph reprinted with permission).
The Myo MuncheeTM has been approved by the Australian Government Department of Health (2019), Therapeutic Goods Administration as a Class 1 (low risk) medical device. The intended purpose of the MD is to exercise the jaw and surrounding muscles, as well as improve gum health and other conditions treated by oral motor therapy such as improving nasal breathing, aiding in jaw health development, correcting oral posture and tongue positioning, and improving jaw balance (Bourke & Clayton, 2018). The device is ISO 13485 certified by the Standard for Quality Management System for design and manufacturing of medical devices and is made of non-toxic medical grade silicone.
The device was used for a 5-week intervention period, with participants required to use the device twice daily (recommended use in the morning and evening, at the time of participants’ usual oral care routine). The Myo MuncheeTM was placed in the oral cavity by the patient, with the lips around the device and gently masticated. The device was used for 1 minute twice daily in the first week and increased by 1 minute each week until the fifth week of intervention when the device was used twice daily for 5 minutes.
All participants received the treatment intervention. There was no alteration to their usual intervention for oral care or swallowing treatment unless this was deemed appropriate by the usual treating SLPs at the RACF, or the treating medical/nursing team. Care staff (nursing/allied health) assisted in providing intervention as part of their routine care for residents.
Care staff members (nursing/allied health) were provided with education and training on the MD and study protocol prior to the commencement of the intervention with residents. Training in the supervision of the intervention was attended by care staff as part of their normal work duties. Explanation regarding cleaning procedures, cleaning schedule and storage of the MD was provided during the training session.
Data Collection
Recruitment and retention
Nursing Unit Managers/care staff at the RACF screened residents’ medical notes for study eligibility (listed in Table 1). The number of eligible residents who were screened, determined to be eligible, approached for recruitment, agreed to participate, and completed the 5-week intervention and post-intervention assessment was recorded.

Table 1.
Inclusion and exclusion criteria for resident participants.
Adherence
There were 70 potential occasions of device use during the intervention period (2 times per day for 5 weeks). A twice daily checklist was used by participants or care staff to record use of the device. Checklists were collected at the end of each week and collated. The number of recorded occasions of device use was compared to the total expected number of occasions at the 3-week (3 minutes twice per day) and 5-week (5 minutes twice per day) timepoints of the intervention. The criteria for the current study to progress to a larger trial will consider both timepoint measurements of 85% adherence at 3 weeks, and 70% adherence at 5 weeks of intervention.
Acceptability
Care staff and residents completed a post- intervention questionnaire. Questionnaires included questions regarding ease of device use and cleaning, assistance required with the device, and perceived changes to oral hygiene and swallowing. Residents’ questionnaires also addressed device comfort and the likelihood of continuing to use the device after completion of the study. Care staff questionnaires included additional items related to adherence to using the device and the increased burden of assisting residents with the intervention.
The acceptability of the intervention was measured in relation to an average positive rating greater than 70% across all parameters of acceptability as set and described in the published protocol (Shortland et al., 2022b).
Clinical Outcome Measures
To gain insight into appropriate outcome measures that would be sensitive enough to detect change in oral health and swallowing function for future studies, clinical outcome measures were collected pre- and 5-weeks post-intervention using validated instruments. These outcomes are not explored in this current paper, as its aim is to determine the feasibility of the use of an MD in an aged care population rather than to explore the oral health and swallowing outcomes. The outcome measures collected included the Oral Health Assessment Tool (Chalmers et al., 2004), Test of Mastication and Swallowing Solids (Huckabee et al., 2018), Timed Water Swallow Test (Hughes & Wiles, 1996), Mann Assessment of Swallowing Ability (Mann, 2002), Functional Oral Intake Scale (Crary et al., 2005), and the Eating Assessment Tool (Belafsky et al., 2008). A brief description of these outcome measures is provided in the Appendix A.
Pre-intervention assessments were planned to be conducted within the week prior to commencement of intervention. The 5 weeks of intervention occurred at the same time for all participants. Post- assessment data collected was planned within 2 weeks of completion of the intervention period. Pre- and post-intervention data collection was completed by a qualified clinical SLP with over 18 years of clinical experience who was also the principal investigator of this study (SLH). A second qualified SLP with over 20 years of experience conducted reliability checking of 10% of residents onsite at the RACF.
Data Analysis
Descriptive statistics were used to analyse and describe data related to study recruitment and retention rates, adherence to the intervention protocol, and the acceptability of the device by staff and residents.
Participants’ free text responses on post-intervention surveys were collated, analysed using content analysis and included in the reporting of the results.
RESULTS
Inter-assessor Reliability
Agreement rate was 100% between the principal investigator and the second qualified SLP of participant severity for each of the pre- and post- assessment measures collected on 10% of participants (2 residents).
Feasibility Outcomes
Recruitment and Retention
RACF staff screened 140 residents’ medical notes and identified 43 eligible candidates for this study. Due to quarantine restrictions related to the COVID-19 pandemic in the facility at the time of recruitment, 21 of the candidates were approached to participate in the study, resulting in a recruitment rate of 48.8%. Of these 21 residents, 13 consented to participate, for an enrolment rate of 61.9%. Twelve residents completed the entire 5-weeks of intervention; the remaining resident withdrew from the research study during the first week of treatment, for a retention rate of 92.3%.
Participants’ demographic data are listed in Table 2. The mean age of resident participants was 87 years (range = 74 – 99 years) and the majority (76.9%) were female. Of the 13 residents, 12 were independent with oral care. Most participants had partial or full dentures. Based on the International Dysphagia Diet Standardization Initiative (IDDSI, 2019), all participants were currently receiving an easy-to-chew (IDDSI Level 7) diet with three residents requiring the use of extra sauce or gravy to moisten foods. All residents received normal fluids (IDDSI Level 0). Of the 13 residents, three were identified as having mild oropharyngeal dysphagia according to clinical swallowing assessments.

Table 2.
Demographics and background of the residents participating in the study taken from medical files.
Participants’ Mini Mental State Examination (MMSE) (Molloy & Standish, 1997) scores averaged 25.2 (range = 22–30). While scores between 21–24 indicate mild cognitive change (Molloy & Standish, 1997), all participating residents were considered (by documentation in the medical file) to be competent to provide consent and follow instructions adequately to complete assessment tasks and participate in the study. Participants presented with a range of diagnoses in their medical background and required low to moderate levels of care.
Of the 50 staff members who undertook pre- intervention education and participated in the study, 10 (20%) completed the questionnaire.
Adherence
One resident (Participant 13) withdrew from the study after one day of intervention. For the remaining 12 participants, the average adherence rates were 99.8% for Week 1, 92.6% at Week 3, and 89.3% at Week 5 (Table 3). Table 3 provides individual and average adherence rates for Weeks 3 and 5.

Table 3.
Individual participant adherence at 3 weeks and 5 weeks of intervention.
On average, overall adherence to the intervention across all of the participants for 70 potential occasions of device use during the intervention period at the 3-week and 5-week timepoint was 92.6% and 89.3%, respectively. There was individual variation in adherence across the 5 weeks of intervention. Four participants had decreased adherence between the 3 and 5-week timepoints, four participants had 100% adherence at both timepoints, and four participants had increased adherence from the 3-week to 5-week timepoints.
Acceptability
Eleven participants (84.6%) responded to the post- intervention survey regarding their experience using the MD. All rated the device as very easy to use. Ten of the 11 participants rated the device as very comfortable. Table 4 provides a summary of the residents’ perceived changes of swallowing, oral health and speech post intervention. Whilst no changes were reported for swallowing, 5 participants who responded to the survey reported an improvement in oral hygiene, 4 for saliva production, and 2 for chewing.

Table 4.
Perceived changes by residents post myofunctional device use.
Seven participants provided free-text written feedback on the post-intervention survey. One resident reported chewing meals was easier after intervention, another reported their teeth looked brighter, and a further resident reported an increase in saliva production. Four of the residents commented that using the MD for 5 minutes was “boring,” with one participant commenting on discomfort when using the device more than 3 minutes at a time. Three participants suggested 2–3 minutes would be the preferred dosage for device use.
“chewing meals was easier after device use, 5 mins too long of time to do, 3 minutes easier to do” (Participant 3).
“comfortable at 2–3 minutes of use. The longer used the more uncomfortable after 2–3 minutes” (Participant 8).
Care staff who completed the post intervention questionnaire mostly reported they were unsure of changes related to saliva production, swallowing, and chewing; however, 6 of the 10 care staff observed improvements in oral hygiene (Table 5).

Table 5.
Care staff perceived improvement of residents post intervention.
Four care staff provided additional comments; one participant commented “Good in theory, but residents not all cognitive enough” (Care staff participant 4), and another commented "I feel that the concept for the device is amazing. And if residents can benefit in any way it is worth it.”
Seven of the 10 care staff indicated that the device was easy or very easy to clean (Table 6). The remaining three care staff rated cleaning as neither easy nor hard. Care staff reported 50% of the residents used the MD without prompting, 40% required encouragement to use the device, and the remaining 10% rarely used the device which is reflected in participants’ adherence for device use. Seven care staff reported no increase in workload supervising residents using the device, one gave a neutral response, and the remaining two indicated the supervision was time-consuming on their usual workload.

Table 6.
Feasibility Outcome Results for Trial Progression.
As per the published protocol (Shortland et al., 2022b), a criterion to assess feasibility was determined and applied to the results of the current study. As indicated in Table 6, the criteria for recruitment and retention, adherence, and acceptability of the use of the device were achieved.
Collection of Outcome Measures
All outcome measures were able to be collected from all participants within a single 8-hour workday. Pre-intervention measures were collected 1 week prior to the intervention, and post-intervention measures were collected 2 weeks following the intervention.
DISCUSSION
This study aimed to determine the feasibility of using a MD for management of oral health and swallowing function in an aged care population. Key findings indicate high recruitment and retention rates, and excellent overall participant adherence with device use across the 5-week intervention. Additionally, the MD was usually reported to be easy to use, clean, and comfortable for residents to use.
Previous research exploring oral health in those with dysphagia have utilized shorter timeframes for study length (Murray & Scholton, 2018); however, longer timeframes and good adherence to therapy are needed when considering changes to swallowing function (Bulgareli et al., 2021; Hägglund et al., 2019; Patterson et al., 2020). While there was variable adherence across the individual participants in this study, overall adherence across the 5-week intervention remained above 89%. Factors that can influence individuals’ adherence to oral health regimens include education of the benefits of oral hygiene, and the affordability to maintain good oral health (Bulgareli et al., 2021; Patterson et al., 2020). However, adherence to oral health regimens in care facilities falls predominantly to care staff and may be impacted by the level of training and education in oral health care, the available guidelines around performing oral care (Lombardo et al., 2022; Wagner et al., 2022) and be further impacted by the identification of those who require assistance with oral care (Colgate, 2022). It is suggested that simple instructions for care staff are needed to ensure adherence with completing oral cares for those in care facilities (Lombardo et al., 2022).
Usual oral care practices and recommendations should also be considered when discussing adherence in relation to this study, especially the timepoint in the reduction of adherence, which was observed with 7 of the 12 participants in Week 3 of the intervention. Week 3 required residents to chew on the MD for 3 minutes twice a day. In Australia, the Department of Health recommends that people brush their teeth twice daily for 2 minutes with a 45° angle on the gumline and brushing both inside and outside of the chewing surface, including brushing of the tongue (Krekeler et al., 2018). While the intended purpose of the study was not to replace typical oral care practices, the timepoint in the reduction of adherence and feedback reported by participants in this study is longer than the usual recommended oral care regimen. However, appropriate usual daily oral care (such as teeth brushing) may not be achieved or take longer to complete for those who experience upper limb weakness secondary to age, surgery, or because of a medical event including hemiparesis (Affoo & Hachey, 2022).
In general practice and therapy in all health professions, the success of any intervention is related to the adherence to therapy recommendations by the patient (WHO, 2003). Reduced adherence and commitment to long-term therapy not only may result in poorer health outcomes and quality of life, but also further financial implications for the healthcare system (Dodd et al., 2012; WHO, 2003). However, a study by Dodds and colleagues (2012) discusses that in a clinical trial setting where a specific protocol is required, there is an increased demand on participants for adherence to trial conditions and the intensiveness of follow-up assessments post-trial intervention. Dodds and colleagues (2012) suggested that there may be multiple layers of nonadherence by participants including a complete withdrawal from a study, permanent or temporary discontinuation of the intervention, or failure to follow intervention protocols for timing and dosage of the intervention (Dodds et al., 2012). Given that only one participant withdrew from this study and only two others reported adherence below 70% at 5 weeks, the assessment and intervention protocol was highly successful.
Most residents in the study reported the MD was both comfortable and easy to use and did not require assistance from staff in using the device. The importance of ease of use and care for products was highlighted in a review of home healthcare with an increase in medical devices that are being produced as consumer products for convenient and independent care at home/outside of hospitals (National Research Council, 2010). Devices to manage healthcare need to be safe, and easily used by individuals or care staff that may be assisting them (National Research Council, 2010). Patient care technologies and devices can range from relatively simple (such as the Myo MuncheeTM used in this trial), to those that are more complex but can assist nursing staff in delivering care (Powell-Cope et al., 2008). The use of devices may allow for improvement in care staff productivity, efficiency, safety, and improved health outcomes for the patient (Powell-Cope et al., 2008). The current study was completed in a general healthy aged-care population with adequate cognition such that most residents were able to use the MD independently, without the assistance of staff, and therefore not increasing the burden of care. This is of importance when considering time constraints for care staff and highlights the importance of implementing simple oral care regimens which may reduce care staff workload and have a positive impact on residents’ oral health.
Given the ease of MD use and comfort level that was reported by residents in this study, along with feedback from staff supervising the intervention, justification for further research in other vulnerable groups such as those with cognitive impairment who are at high risk of oral hygiene deficits and malnutrition should be considered. It is important to consider, however, that modifications to the intervention and dosage of MD use may be required for the acceptability of the device in more vulnerable populations who are not independent with oral hygiene practices.
There is a complex and multifactorial nature to the relationship between oral health, general well-being, and oral intake (Affoo & Hachy, 2022; Patel et al., 2021). This is demonstrated by links between poor oral health with systemic disease, morbidity and mortality demonstrated extensively throughout allied health, nursing, and dental literature (Ajwani et al., 2017; Danckert et al., 2016; Wang et al., 2015). Oral health is crucial to health and wellbeing [Council of Australian Government Health Council (COAG), 2019] and is important for adequate function of speech, mastication, swallowing, and conveying emotion (Kenny et al., 2019; Patel et al., 2021). However, the burden of oral disease is growing with an increase in the aging population (Kenny et al., 2019). A reduction in dentition and the presence of pain may impact mastication and swallowing, with potential for malnutrition, poorer health outcomes and reduced quality of life (Luong et al., 2018).
Both residents and staff reported on perceived changes to swallowing and oral hygiene in post- intervention questionnaires. Just under half of the residents and over half of care staff reported improvement with oral hygiene following the 5- week intervention. It is possible that the length of intervention may not have been sufficient for residents and staff to experience or detect change. However, although the participants’ perspectives of change following an intervention are important as indicators of meaningfulness of the intervention, they may not always align with the results on assessment measures (Tang et al., 2012).
Limitations
Appropriate to a feasibility study, the sample size was small, residents and investigators were not blinded to the conditions, and there was no experimental control; therefore, results should be interpreted with caution. The study recruited participants from a heterogenous aged care population with minimal dysphagic symptoms and adequate cognition. Further studies would need to be considered to assess the use of MDs in those with cognitive impairment. In addition, post-intervention questionnaires used with both residents and staff to gain an understanding of the perceived change of speech, oral health, and swallowing did not include a scale or questions addressing deterioration. Future studies may benefit from the inclusion of questioning around perceived deterioration to provide greater perceived effectiveness of the use of MDs.
Future Directions
The results of this study support the feasibility of a larger clinical trial using an MD for management of oral health and swallowing in an aged care population. Consideration of expansion on the eligibility criteria and recruitment across multiple sites may be beneficial. Given positive results of feasibility for device use in this study with a general aged care population, the link between dysphagia and aspiration pneumonia, and the known predictor of aspiration pneumonia being an inability to manage oral health independently, future research should consider inclusion of people at increased risk of or diagnosed with dysphagia. Further consideration for inclusion should also be given to people with reduced oral health independence such as those with cognitive impairments. Future studies should also investigate optimal dosage for device use.
CONCLUSION
The use of an MD in an aged care population for managing oral health and swallowing function was determined to be feasible. There were both high retention rates and overall participant adherence with MD use across the 5-week intervention. Further, the MD was reported to be easy to use, clean, and was comfortable for residents to use. Results from this study indicate the feasibility of further clinical trials to determine the efficacy of MD use in the management of oral health and dysphagia in an aged care population.
Author Contributions
Conceptualization: H.S., S.H., G.W., A.V.; Study design: H.S., S.H., G.W., A.V.; Data collection: H.S., S.H.; Data analysis and interpretation: H.S., S.H., G.W., A.V.; Writing/manuscript preparation: H.S., S.H., G.W.; Critical revision: H.S., S.H., G.W., A.V.
Data Availability Statement
The data sets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
Thank you to the residents and staff at Maroba Aged Care for participating in this research. The research team appreciates the support of the organization Maroba Aged Care to enable the study to be conducted during the peak of the COVID-19 Pandemic.
Conflicts of Interest
Funding for a Higher Degree of Research (HDR) scholarship has been provided by the industry partner grant from Myo Munchee to A/Prof. Sally Hewat and Dr. Gwendalyn Webb, University of Newcastle. A PhD scholarship was awarded to Hollie-Ann Shortland and this study was conducted as part of Shortlands’ program of research. The authors alone are responsible for the recruitment of participants, collection and analysis of data, and the content and writing of this paper.
Appendix A
Outcome measures for collection pre and post intervention
| Outcome Measure | Area of Evaluation | Description |
| Oral Health Assessment Tool (OHAT) (Chalmers et al., 2004) | Oral health | Reliable and valid screening tool for use in aged care and with cognitive impairment. Approximately 7–8 minutes to administer; 8 items. Rating scale 0 = healthy, 1 = changes, 2 = unhealthy; Total score possible = 16. The higher the score, the worse the oral health. Items that score 1 indicate intervention is required, and items scoring 2 indicate referral to a dental professional is required. |
| Test of Mastication and Swallowing Solids (TOMASS) (Huckabee et al., 2018) | Mastication ability | Quantitative assessment of solid bolus ingestion. Sensitive in detecting changes in performance ability of mastication; high interrater and test-retest reliability. Count number of bites, number of masticatory cycles per bite, and number of swallows per bite. More likely to identify patients with subtle oral phase impairment or bolus transition issues. Normative ranges in older adults: number of bites (male = 1.47; female = 1.87), time (male = 32.61s; female = 41.85s), total number of swallows (male = 3.61/female = 3.5), masticatory cycle (male = 37.6; female = 41.65). |
| Timed Water Swallow Test (TWST) (Hughes & Wiles, 1996) | Aspiration risk | Swallow speed is a sensitive indicator for identifying patients at risk of swallow dysfunction. Choking on 100ml TWST may be a potential indicator for follow-up aspiration. Measures swallow time, number of swallows and observes for signs of choking. Abnormal swallow is defined as a speed below 10ml/s (amount of water divided by elapsed time); count the number of swallows taken to consume 100ml of water and time taken to consume 100ml of water. |
| Mann Assessment of Swallowing Ability (MASA) (Mann, 2002) | Identify swallowing disorders | Screening bedside tool to identify eating and swallowing disorders in stroke and other diseases. Used to quantify aspiration risk; 24 clinical items; 4 components of the assessment include general patient examination, oral preparation, oral phase, and pharyngeal phase; 5–10 point rating scale. Total score possible = 200; >178 = normal, 168–177 = mild, 139–167 = moderate, <138 = severe. Risk of aspiration is defined by a sum of the 4 scores/categories, >170 = normal, 149–169 = mild, 141–148 = moderate, <140 = severe. |
| Functional Oral Intake Scale (FOIS) (Crary et al., 2005) | Functionality | Functional level of oral intake of food and liquid; interrater reliability high and sensitive to changes. 7-point ordinal scale: Levels 1–3 relate to non-oral feeding; Levels 4–7 relate to varying degrees of oral feeding; all levels focus on what is/not consumed orally. |
| Eating Assessment Tool (EAT-10) (Belafsky et al., 2008) | Self-perceived symptoms | Screen self-perceived symptoms of oropharyngeal dysphagia. Scores range from 0–40; Scores >3 indicates dysphagia. 10 questions rated on a 5-point scale, 0 = no problem, 4 = severe problem. Scores >15 indicate aspiration risk. An elevated score indicates a higher self-perception of dysphagia. |
References
- Affoo, R., and S. Hachey. 2022. Integrating oral health in speech-language pathology practice: A viewpoint. Perspectives of the ASHA Special Interest Groups, 1–11. [Google Scholar] [CrossRef]
- Ajwani, S., S. Jayanti, N. Burkolter, C. Anderson, S. Bhole, R. Itaoui, and A. George. 2017. Integrated oral health care for stroke patients—A scoping review. Journal of Clinical Nursing 26, 7–8: 891–901. [Google Scholar] [CrossRef] [PubMed]
- American Speech & Hearing Association (ASHA). 2022. Dysphagia. Available online: https://www.asha.org/practice-portal/clinical-topics/late-language-emergence/assessment-tools-techniques-and-data-sources/ (accessed on 1 October 2022).
- Aquilanti, L., S. Alia, S. Pugnaloni, E. Coccia, M. Mascitti, A. Santarelli, L. Limongelli, G. Favia, M. Mancini, A. Vignini, and G. Rappelli. 2020. Impact of elderly masticatory performance on nutritional status: An observational study. Medicina 56, 130. [Google Scholar] [CrossRef]
- Australian Government Department of Health. 2019. Dental health. Available online: https://www.health.gov.au/health-topics/dental-health (accessed on 1 October 2022).
- Australian Health Ministers Advisory Council (AHMAC). 2017. Aboriginal and Torres Strait Islander health performance framework 2017 report. Canberra. [Google Scholar]
- Australian Institute of Health & Welfare (AIHW). 2021. Oral health and dental care in Australia. Available online: https://www.aihw.gov.au/reports/dental-oral-health/oral-health-and-dental-care-in-australia/contents/introduction (accessed on 19 August 2022).
- Badiah, B., P. Kang, W. Hor, M. Razali, and T. Mohd Dom. 2013. Exploring factors influencing adherence to oral hygiene care among periodontal patients: A pilot study. Sains Malaysiana 42: 13–17. [Google Scholar]
- Belafsky, P.C., D.A. Mouadeb, C.J. Rees, J.C. Pryor, G.N. Postma, J. Allen, and R.J. Leonard. 2008. Validity and reliability of the eating assessment tool (EAT-10). Annals of Otology, Rhinology & Laryngology 117, 12: 919–24. [Google Scholar] [CrossRef]
- Bourke, K. n.d.9th Asian Pacific Conference. The chewing brush. Oral Physiotherapy Lecture 12. Available online: https://static1.squarespace.com/static/57ba3862893fc01e071991d8/t/5912949f2e69cf5fef74e9fb/1494389920781/The+Chewing+Brush.pdf (accessed on 28 June 2022).
- Bourke, M., and C. Clayton. 2018. Myo munchee: A practitioner user guide.
- Bulgareli, J.V., K.L. Cortellazzi, L.M. Guerra, G.M. Bovi Ambrosano, A.K. Kaieda, I.P. da Cunha, F. de Lima Vazquez, and A.C. Pereira. 2021. Determinants of adherence to dental treatment of socially vulnerable adolescents: A cohort study. BMC Res Notes 14: 116. [Google Scholar] [CrossRef]
- Chalmers, J., V. Johnson, J.H. Tang, and M.G. Titler. 2004. Evidence-based protocol: Oral hygiene care for functionally dependent and cognitively impaired older adults. Journal Gerontology Nursing 30, 11: 5–12. [Google Scholar]
- Colgate. 2022. Brushing and flossing. Available online: https://www.colgate.com.au/oral-health/brushing-and-flossing/3-tooth-brushing-techniques-that-get-the-job-done (accessed on 1 October 2022).
- Council of Australian Governments Health Council. 2017. Healthy mouths, healthy lives: Australia’s national oral health plan 2015–2024. Performance Monitoring Report: Baseline Report. Victoria: Dental Health Services Victoria. [Google Scholar]
- Crary, M.A., G.D. Carnaby-Mann, and M.E. Groher. 2005. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Archives of Physical Medicine and Rehabilitation 86: 1516–1520. [Google Scholar] [CrossRef]
- Danckert, R., A. Ryan, V. Plummer, and C. Williams. 2016. Hospitalisation impacts on oral hygiene: An audit of oral hygiene in a metropolitan health service. Scandinavian Journal of Caring Sciences 30, 1: 129–134. [Google Scholar] [CrossRef]
- de Felício, C.M., M. Melchior, O. de, and M.A.M.R. da Silva. 2010. Effects of orofacial myofunctional therapy on temporomandibular disorders. CRANIO® 28, 4: 249–259. [Google Scholar] [CrossRef] [PubMed]
- Dodd, S., I.R. White, and P. Williamson. 2012. Nonadherence to treatment protocol in published randomised controlled trials: a review. Trials Journal 13: 84. [Google Scholar] [CrossRef]
- Drapal, C.S. 2015. Oral care practice guidelines for the care-dependent hospitalized adult outside of the intensive care unit setting. Available online: https://scholarworks.waldenu.edu/cgi/viewcontent.cgi?article=1408&context=dissertations&httpsredir=1&referer= (accessed on 1 October 2022).
- Eldridge, S.M., C.L. Chan, M.J. Campbell, C.M. Bond, S. Hopewell, and L. Thabane. 2010. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ 355: i5239. [Google Scholar] [CrossRef]
- Farrell, D.C., and M. Darcy. 2018. The history of myofunctional orthodontics: Part 1. The beginning & the separation. Australian Dental Practice, Special Report May/June: 74–76. Available online: https://myoresearch.com/storage/app/media/history-of-myofunctional-orthodontics-part-I-0518.pdf (accessed on 1 August 2022).
- Fricker, A., and A. Lewis. 2009. Better oral health in residential care–final report; Central Northern Adelaide Health Service, South Australian Dental Service, Adelaide. Available online: https://www.sahealth.sa.gov.au/wps/wcm/connect/32902a8043506b6a91bef32835153af6/SADS-BOHP-Fin-Report-Nov-09.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-32902a8043506b6a91bef32835153af6-nKKIejJ (accessed on 1 October 2022).
- Hägglund, P., M. Hägg, P. Wester, and E. Levring Jäghagen. 2019. Effects of oral neuromuscular training on swallowing dysfunction among older people in intermediate care: A cluster randomised, controlled trial. Age and Ageing 48, 4: 533–540. [Google Scholar] [CrossRef]
- Huckabee, M.L., T. McIntosh, L. Fuller, M. Curry, P. Thomas, M. Walshe, E. McCague, I. Battel, D. Nogueira, U. Frank, L. van den Engel-Hoek, and O. Sella-Weiss. 2018. The test of masticating and swallowing solids (TOMASS): Reliability, validity and international normative data. International Journal of Language and Communication Disorders 53, 1: 144–156. [Google Scholar] [CrossRef] [PubMed]
- Hughes, T.A., and C.M. Wiles. 1996. Clinical measurement of swallowing in health and in neurogenic dysphagia. Quarterly Journal of Medicine 89: 109–16. [Google Scholar] [CrossRef]
- In, J. 2017. Introduction of a pilot study. Korean Journal of Anesthesiology 70, 6: 601–605. [Google Scholar] [CrossRef] [PubMed]
- International dysphagia diet standardisation initiative (IDDSI). 2019. Complete IDDSI framework detailed definitions. Available online: https://iddsi.org/IDDSI/media/images/Complete_IDDSI_Framework_Final_31July2019.pdf (accessed on 19 August 2022).
- Kenny, C., J. Regan, L. Balding, S. Higgins, N. O'Leary, F. Kelleher, R. McDermott, J. Armstrong, A. Mihai, E. Tiernan, J. Westrup, P. Thirion, and D. Walsh. 2019. Dysphagia prevalence and predictors in cancers outside the head, neck, and upper gastrointestinal tract. Journal of Pain and Symptom Management 58, 6: 949–958.E2. [Google Scholar] [CrossRef]
- Krekeler, B.N., C.K. Broadfoot, S. Johnson, N.P. Connor, and N. Rogus-Pulia. 2018. Patient adherence to dysphagia recommendations: A systematic review. Dysphagia 33, 2: 173–184. [Google Scholar] [CrossRef]
- Langmore, S.E., M.S. Terpenning, A. Schork, Y. Chen, J.T. Murray, D. Lopatin, and W.J. Loesche. 1998. Predictors of aspiration pneumonia: How important is dysphagia? Dysphagia 13, 2: 69–81. [Google Scholar] [CrossRef]
- Lombardo, L., C. Ferguson, A. George, A.R. Villarosa, B.J. Villarosa, A.C. Kong, R. Wynne, and Y. Salamonson. 2022. Interventions to promote oral care regimen adherence in the critical care setting: A systematic review. Australian Critical Care: Official Journal of the Confederation of Australian Critical Care Nurses 35, 5: 583–594. [Google Scholar] [CrossRef] [PubMed]
- Luong, E., P. Drysdale, E. Campbell, J. deClifford, S.H. Lam, J. Coutsouvelis, and R. Danckert. 2018. Implementation of standardised oral care treatment and referral guidelines for older sub-acute patients: A multidisciplinary approach. Journal of Pharmacy Practice and Research 48, 1: 10–17. [Google Scholar] [CrossRef]
- Mann, G. 2002. MASA, The Mann Assessment of Swallowing Ability. New York, NY: Cengage Learning, Vol. 1. [Google Scholar]
- Molloy, D.W., and T.I. Standish. 1997. A guide to the standardized Mini-Mental State Examination. International Psychogeriatrics 9 Suppl. 1: 87–94, discussion 143–50. [Google Scholar] [CrossRef]
- Murray, J., and I. Scholten. 2018. An oral hygiene protocol improves oral health for patients in inpatient stroke rehabilitation. Gerodontology 35: 18–24. [Google Scholar] [CrossRef] [PubMed]
- National Research Council (US) Committee on the Role of Human Factors in Home Health Care. 2010. The role of human factors in home health care: Workshop summary; Washington, DC: National Academies Press (US): 8, Medical Devices in Home Health Care. Available online: https://www.ncbi.nlm.nih.gov/books/NBK210047 (accessed on 2 August 2022).
- Patel, J., J. Wallace, M. Doshi, M. Gadanya, B. Yahya, J. Roseman, and P. Srisilapanan. 2021. Personal view oral health for healthy ageing challenges for oral health in ageing populations. The Lancet 2: E521–E527. [Google Scholar] [CrossRef]
- Patterson Norrie, T., A.R. Villarosa, A.C. Kong, S. Clark, S. Macdonald, R. Srinivas, J. Anlezark, and A. George. 2020. Oral health in residential aged care: Perceptions of nurses and management staff. Nursing Open 7: 536–546. [Google Scholar] [CrossRef]
- Powell-Cope, G., A.L. Nelson, and E.S. Patterson. 2008. Patient care technology and safety (Chapter 50). Edited by R. G. Hughes. In Patient safety and quality: An evidence-based handbook for nurses. Rockville (MD): Agency for Healthcare Research and Quality (US). Available online: https://www.ncbi.nlm.nih.gov/books/NBK2686/ (accessed on 1 October 2022).
- Santoro, P., I.L. de Silva, F. Cardoso, E. Dias, and H. Beresford. 2011. Evaluation of the effectiveness of a phonoaudiology program for the rehabilitation of dysphagia in the elderly. Archives of Gerontology and Geriatrics 53, 1: e61–e66. [Google Scholar] [CrossRef]
- Shortland, H.L., S. Hewat, A. Vertigan, and G. Webb. 2021. Orofacial myofunctional therapy and myofunctional devices used in speech pathology treatment: A systematic quantitative review of the literature. American Journal of Speech-Language Pathology 30, 1: 301–317. [Google Scholar] [CrossRef] [PubMed]
- Shortland, H.A.L., G. Webb, A.E. Vertigan, and S. Hewat. 2022a. Speech-language pathologists' use of myofunctional devices in therapy programs. Perspectives of the ASHA Special Interest Groups 7, 6: 2012–2026. [Google Scholar] [CrossRef]
- Shortland, H.A.L., S. Hewat, G. Webb., and A. Vertigan. 2022b. Myofunctional device use in oral care and swallowing: A protocol for a feasibility study in an aged care population. Pilot Feasibility Studies 8: 187. [Google Scholar] [CrossRef]
- Tang, A., J.J. Eng, and D. Rand. 2012. Relationship between perceived and measured changes in walking after stroke. Journal of Neurologic Physical Therapy: JNPT 36, 3: 115–121. [Google Scholar] [CrossRef] [PubMed]
- Thabane, L., and G.A. Lancaster. 2019. Guide to the reporting of protocols of pilot and feasibility trials. Pilot Feasibility Studies. [Google Scholar] [CrossRef]
- Tkatch, R., S. Musich, S. MacLeod, K. Alsgaard, K. Hawkins, and C.S. Yeh. 2016. Population health management for older adults: Review of interventions for promoting successful aging across the health continuum. Gerontology Geriatric Medicine 2: 2333721416667877. [Google Scholar] [CrossRef]
- Wagner, S., I. Rosian-Schikuta, and J. Cabral. 2022. Oral-care adherence. Service design for nursing homes-initial caregiver reactions and socio-economic analysis. German Medical Science: GMS e-journal 20: Doc04. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.F., C.M. Huang, C. Chou, and S. Yu. 2015. Effect of oral health education programs for caregivers on oral hygiene of the elderly: A systemic review and meta-analysis. International Journal of Nursing Studies 52, 6: 1090–1096. [Google Scholar] [CrossRef]
- World Health Organization (WHO). 2003. Edited by T. Tan-Torres, T. Edejer, R. Baltussen, T. Adam, R. Hutbessy, A. Acharya, D.B. Evans and C.J.L. Murray. Making choices in health: WHO guide to cost-effectiveness analysis. Available online: https://apps.who.int/iris/handle/10665/42699 (accessed on 2 August 2022).
- World Health Organisation (WHO). 2022. Ageing & Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 1 October 2022).
- Ziebolz, D., C. Werner., G. Schmalz, I. Nitschke, R. Haak, R.F. Mausberg, and J.F. Chenot. 2017. Oral Health and nutritional status in nursing home residents-results of an explorative cross-sectional pilot study. BMC Geriatrics 17, 1: 39. [Google Scholar] [CrossRef]
© 2023 by the authors. 2023 Hollie-Ann L. Shortland, Gwendalyn Webb, Anne E. Vertigan, Sally Hewat.