Poster 1: Rest Position of the Tongue in Infants with and Without Lingual Frenulum Alteration
Abstract
INTRODUCTION
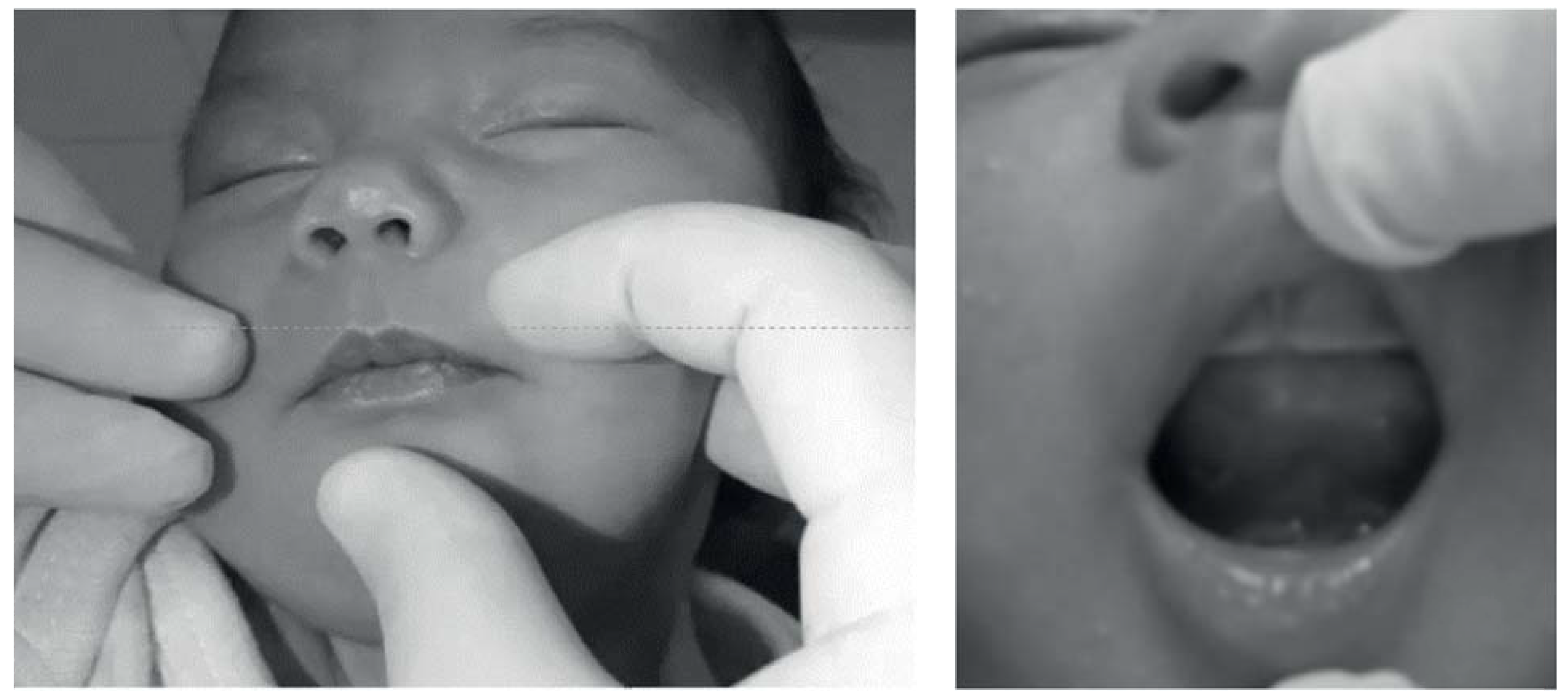
MATERIALS AND METHODS

RESULTS
DISCUSSION
CONCLUSION
References
- American Speech-Language-Hearing Association. Evidence-based practice in communication disorders [Position Statement]. 15 October 2005. Available online: http://www.asha.org/policy.
- Burton, P.; Deng, J.; McDonald, D.; Fewtrell, M.S. Real-time 3D ultrasound imaging of infant tongue movements during breastfeeding. Early Human Development 2013, 89(9), 635–641. [Google Scholar] [CrossRef] [PubMed]
- Camargo, Z. A.; Marchesan, I. Q.; Oliveira, L. R.; Svicero, M. A. F.; Pereira, L. C. K.; Madureira, S. Lingual frenectomy and alveolar tap production: An acoustic and perceptual study. Logopedics Phoniatrics Vocology 2013, 38(4), 157–166. [Google Scholar] [CrossRef] [PubMed]
- Correa, M. S. N. Odontopediatria na primeira infância, 3 ed.; São Paulo: Santos, 2010; p. 923. [Google Scholar]
- Derrick, K.; Stavness, I.; Gick, B. Three speech sounds, one motor action: Evidence for speech-motor disparity from English flap production. The Journal of the Acoustical Society of America 2015, 137(3), 1493–1502. [Google Scholar]
- Elad, D.; Koslovsky, P.; Blum, O.; Laine, A. F.; Po, M. J.; Botzer, E.; Dollberg, S.; Zelicovich, M.; Ben Sira, L. Biomechanics of milk extraction during breastfeeding. Proceedings of the National Academy of Sciences of the USA 2014, 111(14), 5230–5235. [Google Scholar]
- Garbin, C. P.; Sakalidis, V. S.; Chadwick, L. M.; Whan, E.; Hartmann, P. E.; Geddes, D. T. Evidence of improved milk intake after frenotomy: A case report. Pediatrics 2013, 132(5), 1413–1417. [Google Scholar]
- Geddes, D. T.; Langton, D. B.; Gollow, I.; Jacobs, L. A.; Hartmann, P. E.; Simmer, K. Frenulotomy for breastfeeding infants with ankyloglossia: Effect on milk removal and sucking mechanism as imaged by ultrasound. Pediatrics 2008, 122(1), 188–194. [Google Scholar] [CrossRef]
- Geddes, D. T.; Kent, J. C.; Mitoulas, L. R.; Hartmann, P. E. Tongue movement and intra-oral vacuum in breastfeeding infants. Early Human Development 2008, 84(7), 471–477. [Google Scholar]
- Guedes-Pinto, A. C.; Bönecker, M.; Rodrigues, C. R. M. D. Odontopediatria—Fundamentos de odontologia, 1st ed.; Santos-GEN, 2009. [Google Scholar]
- Guilleminault, C.; Huseni, S.; Lo, L. A frequent phenotype for paediatric sleep apnoea: Short lingual frenulum. ERJ Open Research 2016, 00043-2016. [Google Scholar]
- Henry, L.; Hayman, R. Ankyloglossia its impact breastfeeding. Nursing for Women’s Health 2014, 18(2), 122–129. [Google Scholar]
- Horton, C. E.; Crawford, H. H.; Adamson, J. E.; Ashbell, T. S. Tongue-tie. Cleft Palate Journal 1969, 6, 8–23. [Google Scholar]
- Huang, Y.; Quo, S.; Berkowski, J. A.; Guilleminault, C. Short lingual frenulum and Obstructive Sleep Apnea in Children. International Journal of Pediatric Research 2015, 1, 1. [Google Scholar] [CrossRef]
- Knox, I. Tongue Tie and Frenotomy in the Breastfeeding Newborn. NeoReviews 2010, 11(9), 513–519. [Google Scholar]
- Ito, Y. Does frenotomy improve breast-feeding difficulties in infants with ankyloglossia? Pediatrics International 2014, 56(4), 497–505. [Google Scholar] [CrossRef] [PubMed]
- Marchesan, I. Q. Lingual Frenulum: Classification and speech interference. International Journal of Orofacial Myology 2004, 30, 31–38. [Google Scholar] [CrossRef]
- Marchesan, I. Q. Protocolo de Avaliação do frênulo da língua. Revista CEFAC 2010, 12(6), 977–989. [Google Scholar] [CrossRef]
- Martinelli, R. L. C.; Marchesan, I. Q.; Berretin-Felix, G. Protocolo de avaliação do frênulo lingual para bebês: relação entre aspectos anatômicos e funcionais. Revista CEFAC 2013, 15(3), 599–610. [Google Scholar]
- Martinelli, R. L. C.; Marchesan, I. Q.; Gusmão, R. J.; Honório, H. M.; Berretin-Felix, G. The effects of frenotomy on breastfeeding. Journal of Applied Oral Science 2015, 23(2), 153–157. [Google Scholar] [CrossRef]
- Martinelli, R. L. C.; Marchesan, I. Q.; Lauris, J. R.; Honório, H. M.; Gusmão, R. J.; Berretin-Felix, G. Validity and reliability of the neonatal tongue screening test. Revista CEFAC 2016, 18(6), 1323–1331. [Google Scholar]
- Neiva, F. C.; Cattoni, D. M.; Ramos, J. L.; Issler, H. Desmame precoce: Implicações para o desenvolvimento motor-oral. Jornal de Pediatria 2003, 79, 7–12. [Google Scholar] [CrossRef]
- Paskay, L. C. Instrumentation and measurement procedures in orofacial myology. International Journal of Orofacial Myology 2006, 32, 37–57. [Google Scholar]
- Serra-Negra, J. M. C.; Pordeus, I. A.; Rocha, J. F., Jr. Estudo da associação entre aleitamento, hábitos bucais e maloclusões. Revista de Odontologia da Universidade de São Paulo 1997, 11, 79–86. [Google Scholar] [CrossRef]
- Sethi, N.; Smith, D.; Kortequee, S.; Ward, V. M.; Clarke, S. Benefits of frenulotomy in infants with ankyloglossia. International Journal of Pediatric Otorhinolaryngoly 2013, 77(5), 762–765. [Google Scholar] [CrossRef] [PubMed]
- Silva, M. C.; Costa, M. L. V. C. M.; Nemr, K.; Marchesan, I. Q. Frênulo de língua alterado e interferência na mastigação. Revista CEFAC 2009, 11(Suppl 3), 363–369. [Google Scholar] [CrossRef]
- Singh, S.; Kent, R. D. Dictionary of Speech-Language Pathology; Singular’s, 2000. [Google Scholar]
- Wallace, H.; Clarke, S. Tongue tie division in infants with breastfeeding difficulties. International Journal of Pediatric Otorhinolaryngology 2006, 70(7), 1257–1261. [Google Scholar] [CrossRef] [PubMed]
 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2016 by the authors. 2016 Roberta Lopes De Castro Martinelli, Irene Queiroz Marchesan, Giédre Berretin-Felix
Share and Cite
Martinelli, R.L.d.C.; Marchesan, I.Q.; Berretin-Felix, G. Poster 1: Rest Position of the Tongue in Infants with and Without Lingual Frenulum Alteration. Int. J. Orofac. Myol. Myofunct. Ther. 2016, 42, 43-48. https://doi.org/10.52010/ijom.2016.42.1.5
Martinelli RLdC, Marchesan IQ, Berretin-Felix G. Poster 1: Rest Position of the Tongue in Infants with and Without Lingual Frenulum Alteration. International Journal of Orofacial Myology and Myofunctional Therapy. 2016; 42(1):43-48. https://doi.org/10.52010/ijom.2016.42.1.5
Chicago/Turabian StyleMartinelli, Roberta Lopes de Castro, Irene Queiroz Marchesan, and Giédre Berretin-Felix. 2016. "Poster 1: Rest Position of the Tongue in Infants with and Without Lingual Frenulum Alteration" International Journal of Orofacial Myology and Myofunctional Therapy 42, no. 1: 43-48. https://doi.org/10.52010/ijom.2016.42.1.5
APA StyleMartinelli, R. L. d. C., Marchesan, I. Q., & Berretin-Felix, G. (2016). Poster 1: Rest Position of the Tongue in Infants with and Without Lingual Frenulum Alteration. International Journal of Orofacial Myology and Myofunctional Therapy, 42(1), 43-48. https://doi.org/10.52010/ijom.2016.42.1.5




