Clinical Column: Inclusion of Orofacial Myofunctional Disorders Content for Communication Sciences and Disorders Students
Abstract
:INTRODUCTION
Need for Training in OMDs
OMDs in CSD Textbooks
OMDs in CSD Coursework
Potential Benefits
Future Research
CONCLUSION
Appendix A
SLP SURVEY
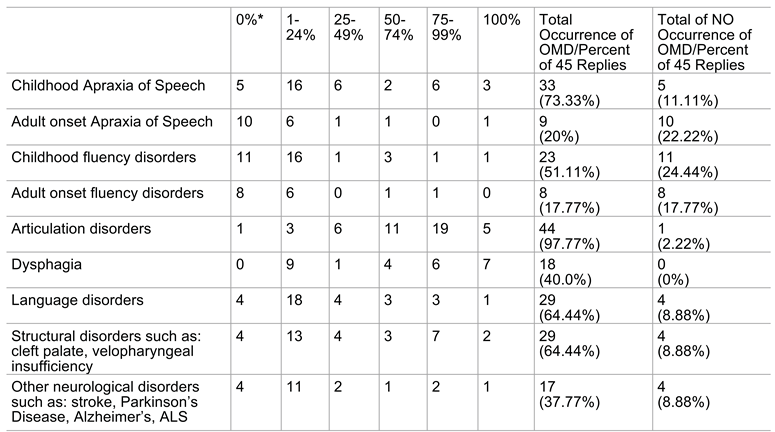
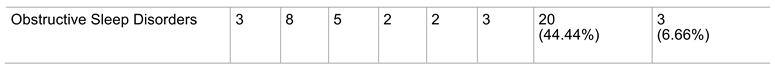
PART 2. OMDs and SPEECH DISORDERS
Appendix B
LECTURE/CONFERENCE PRESENTATION TOPICS
- I.
- Defining tongue thrust and other OMDs
- II.
- Correct versus incorrect swallowing patterns
- III.
- Incidence and prevalence
- IV.
- Etiologies
- V.
- OMDs
- VI.
- Anatomy and physiology
- VII.
- Dentition and eruption
- VIII.
- Force and pressure
- IX.
- Orthodontic and maxillofacial principles
- X.
- Occlusion and malocclusion
- XI.
- The relationship between OMDs, teeth, and speech sound disorders
- XII.
- Diagnosis
- XIII.
- Treatment
- XIV.
- Treatment: Patient variables
- XV.
- Insurance and documentation
- XVI.
- Thumb and digit sucking habits
- XVII.
- Before and after photographs
- XVIII.
- How and where to obtain more information
- XIX.
- Becoming a C.O.M.
- XX.
- Obtaining more information
- XXI.
- IAOM
- XXII.
- Continuing education and convention
- XXIII.
- IJOM and research
References
- Ackerman, R. L.; Klapper, L. Tongue Position and Openbite: The Key Roles for Growth and the Nasopharyngeal Cavity. Journal of Dentistry for Children 1981, 48, 339–345. [Google Scholar] [PubMed]
- American Speech-Language-Hearing Association. The role of the speech-language pathologist in assessment and management of oral myofunctional disorders. ASHA 1991, 33(Suppl 5), 7. [Google Scholar]
- American Speech-Language-Hearing Association; Ad Hoc Joint Committee with the International Association of Orofacial Myology. Orofacial myofunctional disorders: knowledge and skills. American Speech-Language-Hearing Association. ASHA Supply 1993, 35(3 Suppl 10), 21–23. [Google Scholar]
- American Speech-Language-Hearing Association. Preferred practice patterns for the profession of speech-language pathology [Preferred Practice Patterns]. 2004. Available online: www.asha.org/policy.
- American Speech-Language-Hearing Association. Scope of practice in speech-language pathology [Scope of Practice]. 2016. Available online: www.asha.org/policy/.
- Bahr, D.; Rosenfeld-Johnson, S. Treatment of children with speech oral placement disorders (OPDs): A paradigm emerges. Communication Disorders Quarterly 2010, 3(3), 131–138. [Google Scholar] [CrossRef]
- Bell, D.; Hale, A. Observations of tongue thrust swallow in preschool children. Journal of Speech and Hearing Disorders 1963, 28, 195–197. [Google Scholar] [CrossRef]
- Benkert, K. The effectiveness of orofacial myofunctional therapy in improving dental occlusion. International Journal of Orofacial Myology 1997, 23, 35–46. [Google Scholar]
- Bernthal, J. E.; Bankson, N. W. Articulation and phonological disorders, 4th ed.; Pearson, 1998. [Google Scholar]
- Bernthal, J. E.; Bankson, N. W.; Flipsen, P., Jr. Articulation and phonological disorders: Speech sound disorders in children, 7th ed.; Pearson, 2013. [Google Scholar]
- Bleile, K. M. Manual of articulation and phonological disorders: Infancy through adulthood, 2nd ed.; Thompson Delmar Learning, 2004. [Google Scholar]
- Blyth, P. The relationship between speech, tongue behavior, and occlusal abnormalities. The Dental Practitioner 1959, 10, 11–22. [Google Scholar]
- Bowen, C. What is the evidence for oral-motor therapy? Acquiring Knowledge in Speech, Language and Hearing, Speech Pathology 2005, 7, 144–147. [Google Scholar]
- Bowen, C. Controversial practices and intervention for children with speech sound disorders. 4 September 2016. Available online: http://www.speech-language-therapy.com/index.php?option=.com_content&view=article&id=28:controversy&catid=11:admin&Itemid=121.
- Bzoch, K. R. Bzoch, K. R., Ed.; Introduction to the study of communicative disorders in cleft palate and related craniofacial anomalies. In Communicative disorders related to cleft lip and palate, 4th ed.; Pro-Ed, 1997. [Google Scholar]
- Christensen, M.; Hanson, M. An investigation of the efficacy of oral myofunctional therapy as a precursor to articulation therapy for pre-first grade children. Journal of Speech and Hearing Disorders 1981, 46, 160–167. [Google Scholar] [CrossRef]
- Creaghead, N. A.; Newman, P. W.; Secord, W. A. Assessment and remediation of articulatory and phonological disorders; Charles E. Merrill Publishing Company, 1985. [Google Scholar]
- Creaghead, N. A.; Newman, P. W.; Secord, W. A. Assessment and remediation of articulatory and phonological disorders, 2nd ed.; Macmillan, 1989. [Google Scholar]
- D’Asaro, M.; Shapiro, S.; Baum, A.; Jacoby, M. Incidence and relationship of abnormal swallow, open bite, absence of gag reflex, lisping and lip posture in children from 8 to 10 years. ASHA 1961, 3, 369. [Google Scholar]
- Fletcher, S.; Casteel, R.; Bradley, D. Tongue thrust swallow, speech articulation, and age. Journal of Speech and Hearing Disorders 1961, 26, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Jann, G.; Ward, M.; Jann, H. A longitudinal study of articulation, deglutition, and malocclusion. Journal of Speech and Hearing Disorders 1964, 29, 424–435. [Google Scholar] [CrossRef] [PubMed]
- Kummer, A. W. Cleft palate and craniofacial anomalies: Effects on speech and resonance, 3rd ed.; Cengage Learning, 2014. [Google Scholar]
- Lof, G. L. Logic, theory and evidence against the use of non-speech oral-motor exercises to change speech sound productions. Paper presented at the American Speech-Language-Hearing Association Convention, Miami, FL, USA, November; 2006. [Google Scholar]
- Lof, G. L. Reasons why non-speech oral-motor exercises should not be used for speech sound disorders. Paper presented at the American Speech-Language-Hearing Association Convention, Boston, MA, USA, November; 2007. [Google Scholar]
- Lof, G. L. Nonspeech oral-motor exercises: an update on the controversy. Paper presented at the American Speech-Language-Hearing Association Convention, New Orleans, LA, USA, November; 2009. [Google Scholar]
- Marshalla, P. Oral-motor techniques are not new [Monograph]. Oral-motor Institute 2007, 1(1). [Google Scholar]
- Peña-Brooks, A.; Hegde, M. N. Assessment and treatment of articulation and phonological disorders in children, 2nd ed.; Pro-Ed, 2007. [Google Scholar]
- Peña-Brooks, A.; Hegde, M. N. Assessment and treatment of speech sound disorders in children: A dual-level text, 3rd ed.; Pro-Ed, 2015. [Google Scholar]
- Pierce, R. The role of myofunctional therapy in speech pathology. International Journal of Orofacial Myology 1980, 6, 11–13. [Google Scholar] [CrossRef]
- Pierce, R. Age and articulation characteristics: A survey of patient records on 100 patients referred for “tongue thrust therapy”. International Journal of Orofacial Myology 1996, 22, 32–33. [Google Scholar] [CrossRef]
- Pierce, R. B. Orofacial myofunctional therapy. ADVANCE for Speech-Language Pathologists. October 1999. Available online: http://speech-language-pathology-audiologyadvanceweb.com/Article/Orofacial-Myofunctional-Therapy.aspx#AnchorComment.
- Pierce, R. B.; Taylor, P. Rationale for including orofacial myofunctional therapy in university training programs. International Journal of Orofacial Myology 2001, 27, 24–31. [Google Scholar] [CrossRef]
- Ray, J. Orofacial myofunctional therapy in dysarthria: A study on speech intelligibility. International Journal of Orofacial Myology 2002, 28, 39–48. [Google Scholar] [CrossRef]
- Ray, J. Effects of orofacial myofunctional therapy on speech intelligibility in individuals with persistent articulatory impairments. International Journal of Orofacial Myology 2003, 29, 5–14. [Google Scholar] [CrossRef]
- Rogers, G. When to start tongue thrust treatment? [Web log post]. 28 April 2015. Available online: https://www.speechbuddy.com/blog/speech-therapy-techniques/when-to-start-tongue-thrust-treatment/.
- Ronson, I. Incidence of visceral swallowing among lispers. Journal of Speech and Hearing Disorders 1965, 30, 318–324. [Google Scholar] [CrossRef]
- Smit, A. B. Articulation and phonology resource guide for school-age children and adults; Thompson Delmar Learning, 2004. [Google Scholar]
- Straub, W. Malfunction of the tongue. Part I. The abnormal swallowing habit: Its cause, effects, and results in relation to orthodontic treatment and speech therapy. American Journal of Orthodontics 1960, 46, 404–424. [Google Scholar] [CrossRef]
- Subtelney, J. Daniel; Subtelney, Joanne D. Malocclusion, speech, and deglutition. American Journal of Orthodontics. 48 1962, 685–697. [Google Scholar] [CrossRef]
- Tilakraj, T. N. Essential of pedodontics; Jaypee Brothers Medical Publishers, 2003. [Google Scholar]
- Umberger, F. G.; Johnston, R. The efficacy of oral myofunctional and coarticulation therapy. International Journal of Orofacial Myology 1997, 23, 3–9. [Google Scholar] [CrossRef]
- Wadsworth, S. D.; Maul, C. A.; Stevens, E. J. The prevalence of orofacial myofunctional disorders among children identified with speech and language disorders in grades kindergarten through six. International Journal of Orofacial Myology 1998, 24, 1–19. [Google Scholar] [CrossRef]
- Ward, M.; Malone, H.; Jann, G.; Jann, H. Articulation variations associated with visceral swallowing and malocclusion. Journal of Speech and Hearing Disorders 1961, 26, 334–341. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the author. 2016 Hope C. Reed
Share and Cite
Reed, H.C. Clinical Column: Inclusion of Orofacial Myofunctional Disorders Content for Communication Sciences and Disorders Students. Int. J. Orofac. Myol. Myofunct. Ther. 2016, 42, 35-42. https://doi.org/10.52010/ijom.2016.42.1.4
Reed HC. Clinical Column: Inclusion of Orofacial Myofunctional Disorders Content for Communication Sciences and Disorders Students. International Journal of Orofacial Myology and Myofunctional Therapy. 2016; 42(1):35-42. https://doi.org/10.52010/ijom.2016.42.1.4
Chicago/Turabian StyleReed, Hope C. 2016. "Clinical Column: Inclusion of Orofacial Myofunctional Disorders Content for Communication Sciences and Disorders Students" International Journal of Orofacial Myology and Myofunctional Therapy 42, no. 1: 35-42. https://doi.org/10.52010/ijom.2016.42.1.4
APA StyleReed, H. C. (2016). Clinical Column: Inclusion of Orofacial Myofunctional Disorders Content for Communication Sciences and Disorders Students. International Journal of Orofacial Myology and Myofunctional Therapy, 42(1), 35-42. https://doi.org/10.52010/ijom.2016.42.1.4



